On 22 March 2020, a total lockdown was applied in Greece due to COVID‐19. In this unprecedented situation, the psychological impact on the population, and especially on pregnant women, is largely unknown. Research at the time of previous similar epidemics (SARS and MERS) showed that pregnant women were more likely to be psychologically affected. 1 , 2
Anxiety is prevalent in pregnancy; in a recent meta‐analysis, the prevalence of self‐reported anxiety symptoms was 18.2% in the first trimester, 19.1% in the second trimester, and 24.6% in the third trimester, and the overall prevalence for a clinical diagnosis of any anxiety disorder was 15.2%. 3 Antenatal depression also affects up to 16% of the general pregnant population 4 while epidemiological studies consistently demonstrate high rates of comorbidity between anxiety and depressive disorders. 5 Studying antenatal mental health is of particular importance because of the potential negative consequences on perinatal outcomes, 6 so we sought to assess anxiety and depressive symptoms in pregnant women living in the current quarantine conditions in Greece by applying the most commonly used instruments for antenatal anxiety and depression: the State–Trait Anxiety Inventory (STAI) and the Edinburg Postnatal Depression Scale (EPDS). 7 , 8 , 9
All pregnant women who received routine antenatal care in a university clinic during the 6‐week period of total lockdown were asked to complete the STAI and the EPDS. State (S)‐ and Trait (T)‐anxiety scores are categorized as <36 (no anxiety), 36–45 (mild anxiety), 46–55 (moderate anxiety), 56–65 (high anxiety), and >65 (very high anxiety). 7 A cut‐off score of ≥46 was used to identify women with anxiety (moderate anxiety cut‐off), while the EPDS cut‐off score was ≥13; these were the dependent variables of interest. 7 Associated risk factors with maternal anxiety and depression were also investigated in a multivariable logistic regression. The study protocol complied with all the relevant national regulations, conformed to the provisions of the Declaration of Helsinki, and was approved by the bioethics committee of the Aristotle University of Thessaloniki.
Overall, 269 women consented to participate in the survey; 27.5% (n = 74) were ≥ 35 years old, 55.8% (n = 150) were nulliparous, 94.4% (n = 254) reported spontaneous conception, 27.9% (n = 75) had been overweight before pregnancy, and 12.3% (n = 33) reported themselves as current smokers. Anxiety in pregnancy affected 37.5% of the participants (S‐Anxiety), whereas 13.0% exhibited lifetime anxiety (T‐Anxiety; P < 0.001). The median S‐Anxiety value (transient, situational feelings at the moment; 42 [range: 24–67]) was higher than the median T‐Anxiety value (general, ongoing feelings; 35 [range: 22–67]; P < 0.001), indicating a significant increase in anxiety levels during the lockdown.
For S‐Anxiety, 21.6% of the women were classified as non‐anxious, 40.9% had mild anxiety, 27.5% had moderate, 9.7% had high, and 0.3% had very high anxiety. Accordingly, for T‐Anxiety, 52.4% were identified as non‐anxious, 34.6% had mild anxiety, 10.8% had moderate, 1.9% had high, and 0.3% had very high anxiety. There were significant differences between the corresponding S‐ and T‐Anxiety categories (P < 0.001). A moderate association was identified between the S‐ and T‐Anxiety scores (r = 0.549; P < 0.001).
Based on the multivariable analysis, the first week following the lockdown was identified as an independent risk factor for S‐Anxiety (odds ratio [OR]: 2.425; 95% confidence interval [CI]: 1.299–4.529). Moreover, the median S‐Anxiety was significantly different among the study weeks (P = 0.003; Fig. 1). When assessing the individual STAI questions during Weeks 1, 3, and 6, we found that women had similar feelings of tension, strain, and confusion during the whole period. Moreover, during Week 6, they started feeling more frightened than before; accordingly, in Week 3 they felt more comfortable and relaxed than in Week 1, but this was reversed in Week 6 (Table S1). Finally, the third trimester of pregnancy was identified as an independent risk factor for anxiety in pregnancy in the multivariable analysis (OR: 1.913; 95%CI: 1.037–3.529).
Fig. 1.
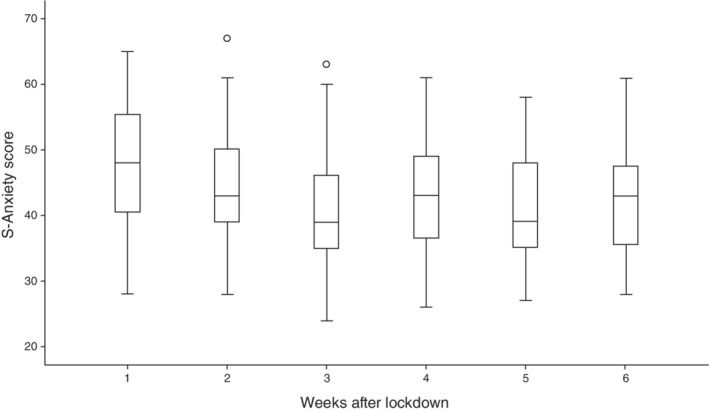
Boxplots of S‐Anxiety scores each week after lockdown. The top of the box represents the 75th centile, the bottom the 25th centile, and the horizontal line in the box represents the median. The T‐bars represent the maximum and minimum values, excluding outliers; the latter are shown as separate circles.
Regarding antenatal depression, 215 women completed the EPDS and 14.9% (n = 32) were identified as depressed. Antenatal depression was associated with S‐Anxiety (P = 0.015; OR: 2.570; 95%CI: 1.199–5.508) while, according to multivariable logistic regression, smoking was identified as an independent risk factor for antenatal depression during the lockdown (OR: 2.889; 95%CI: 1.028–8.118).
Concluding, the mass quarantine has negatively affected the anxiety levels of a large proportion of pregnant women (>50% at the first week of lockdown) in Greece, as they exhibited a significant increase in anxiety during the early stages of the lockdown. However, an encouraging aspect was that after the initial peak of anxiety levels during the first week, they then decreased, possibly due to the effective control of the disease in Greece. Similar studies may shed more light on the impact of the disease and the associated measures under less favorable conditions and hopefully serve as a guide for similar situations in the future.
Disclosure statement
The authors declare no conflicts of interest.
Supporting information
Table S1. Associations of S‐Anxiety scores on Weeks 1 versus 3 and 3 versus 6. The Mann–Whitney U‐test was used for the analyses.
References
- 1. Brooks SK, Webster RK, Smith LE et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020; 395: 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schwartz DA, Graham AL. Potential maternal and infant outcomes from coronavirus 2019‐nCoV (SARS‐CoV‐2) infecting pregnant women: Lessons from SARS, MERS, and other human coronavirus infections. Viruses 2020; 12: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dennis CL, Falah‐Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta‐analysis. Br. J. Psychiatry 2017; 210: 315–323. [DOI] [PubMed] [Google Scholar]
- 4. Koutra K, Vassilaki M, Georgiou V et al. Antenatal maternal mental health as determinant of postpartum depression in a population based mother‐child cohort (Rhea study) in Crete, Greece. Soc. Psychiatry Psychiatr. Epidemiol. 2014; 49: 711–721. [DOI] [PubMed] [Google Scholar]
- 5. Falah‐Hassani K, Shiri R, Dennis CL. The prevalence of antenatal and postnatal co‐morbid anxiety and depression: A meta‐analysis. Psychol. Med. 2017; 47: 2041–2053. [DOI] [PubMed] [Google Scholar]
- 6. Grigoriadis S, Graves L, Peer M et al. Maternal anxiety during pregnancy and the association with adverse perinatal outcomes: Systematic review and meta‐analysis. J. Clin. Psychiatry 2018; 79: 17r12011. [DOI] [PubMed] [Google Scholar]
- 7. Spielberger CD, Gorsuch RL, Lushene R. State‐Trait Anxiety Inventory for Adults: Sampler Set, Manual, Instrument and Scoring Guide. Consulting Psychologists Press, Palo Alto, CA, 1983. [Google Scholar]
- 8. Fountoulakis KN, Papadopoulou M, Kleanthous S et al. Reliability and psychometric properties of the Greek translation of the State‐Trait Anxiety Inventory form Y: Preliminary data. Ann. Gen. Psychiatry 2006; 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EPDS). J. Reprod. Infant Psychol. 1990; 8: 99–107. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Associations of S‐Anxiety scores on Weeks 1 versus 3 and 3 versus 6. The Mann–Whitney U‐test was used for the analyses.


