1.
Dear Editor,
Telemedicine has been available for several years, but the pandemic of coronavirus disease 2019 (COVID‐19) has highlighted its importance as an immediate, safe, and high standard of care. 1 Dermatology is among the most suited specialties for teleassistance, as its visual nature allows for an expert opinion without the need for an in‐person referral. 2 Here, we present two cases of crusted scabies that were successfully diagnosed and treated with the help of teledermatology.
2. CASE 1
Two cohabitant patients with typical scabies were referred to our department and reported that six other family members had similar complaints after visiting a constrained to bed, elderly relative in a nursing home. At consultation, they showed smartphone pictures of their relative. The photographs had reasonable quality and allowed identification of widespread large hyperkeratotic fissured plaques covered with white‐yellowish‐silvery scales on the upper limbs and hands (Figure 1). We suggested one of the relatives to collect skin scrapings in a sterilized urine sample container with the help of a clean spoon. The specimen was sent to a clinical analysis laboratory where a microscopic potassium hydroxide preparation revealed the presence of large numbers of Sarcoptes ectoparasites (Figure 2). The nursing home personnel was notified and the patient was initiated with oral ivermectin along with topical application of 5% permethrin lotion, resulting in rapid and complete resolution of the lesions (Figure 3).
FIGURE 1.

Hyperkeratotic fissured plaques covered with white‐yellowish‐silvery scales over the upper limbs
FIGURE 2.
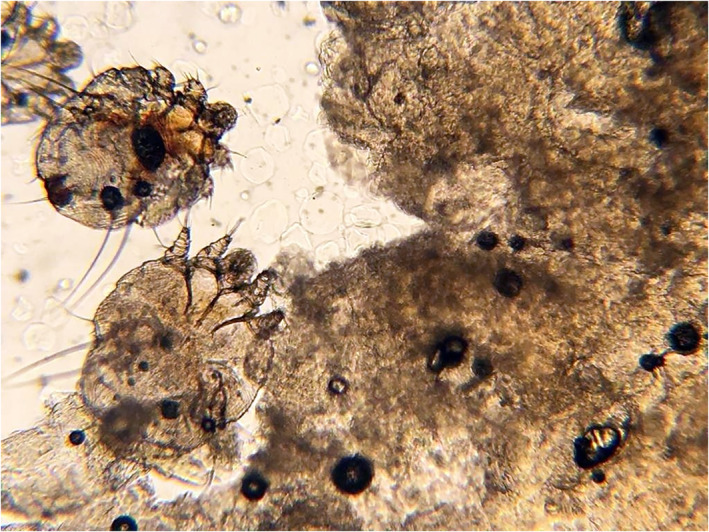
The diagnosis of crusted scabies was confirmed by the identification of the mites as well as fecal matter (scybala) (black or brown football‐shaped masses of feces) through microscopic examination of skin scrapings treated with 10% potassium hydroxide at ×10 magnification
FIGURE 3.

Image of the patient, 9 days after treatment initiation
3. CASE 2
A medical student living in Europe e‐mailed photographs of her 62‐year‐old mother to one of the authors. The photographs showed an alopecic squamous plaque on the scalp, reported to be intensely pruritic, which persisted for several months despite the application of emollients and topical steroids. The plaque bore fractured hair strands, was eroded by scratching, and covered with crusts (Figure 4). The daughter decided to contact us after identifying a paper on crusted scabies published by one of the authors 3 with pictures similar to her mother's. The diagnosis of crusted scabies was considered. Due to lack of access to a local doctor or laboratory, empiric treatment with oral ivermectin and topical 5% permethrin lotion was started and resulted in resolution of the pruritus and significant clinical improvement (Figure 5).
FIGURE 4.

A large, well‐defined, eroded, alopecic squamous plaque, on the scalp of the second patient
FIGURE 5.

Significant clinical improvement noticed within 10 days after treatment initiation, with resolution of the squamous and crusted component of the lesion
4. DISCUSSION
Crusted scabies is a rare form of scabies, caused by Sarcoptes scabiei. It occurs in patients with impaired immunological function such as on the basis of malignancies, autoimmune diseases, and neurological disorders. In institutional settings, scabies is a significant source of morbidity for both residents and health care workers. 4 , 5 Age, reduced mobility, and residency in a nursing home were considered the major risk factors in our patients.
The objective of this presentation is to highlight the importance of teledermatology as an effective tool for diagnosing dermatological ailments. The initial disbelief about the quality of care and the possible negative impact on the patient‐health provider relationship has been confronted by medical literature. 6 , 7 , 8 The COVID‐19 pandemic recognizably was a major stimulus to implement teledermatology in many countries. 1 , 9 Platforms were promptly available and, even, legislation and reimbursement systems were rapidly put into place. The care we provided was given using basic and inexpensive technology of cryptographed stored‐and‐forwarded images, which is available even in resource‐restrained settings.
The interesting characteristic that our cases bring to light is the inverse path taken in order to obtain telecare. Instead of searching for a distant health service, both patients obtained care departing from a visit of relatives (first patient) and a relevant literature research (second patient). We strongly believe that the availability of open access to this kind of care will offer solutions for a myriad of painful health problems. Patients deserve optimum access to it.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
All authors have made substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data, and have been involved in drafting the manuscript and revising it critically for important intellectual content. In addition, all authors have given final approval of the version to be published. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content and each author has agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Gupta R, Ibraheim MK, Doan HQ. Teledermatology in the wake of COVID‐19: advantages and challenges to continued care in a time of disarray. J Am Acad Dermatol. 2020;83(1):168‐169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McKoy K, Antoniotti NM, Armstrong A, et al. Practice guidelines for teledermatology. Telemed J E Health. 2016;22(12):981‐990. [DOI] [PubMed] [Google Scholar]
- 3. Bimbi C, Brzezinski P, Sokolowska‐Wojdylo M. Crusted (Norwegian) scabies as a strong marker of adult T‐cell leukemia/lymphoma in HTLV‐1 infection. Clin Case Rep. 2019;7(3):474‐476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chandler DJ, Fuller LC. A review of scabies: an infestation more than skin deep. Dermatology. 2019;235(2):79‐90. [DOI] [PubMed] [Google Scholar]
- 5. Sánchez‐Borges M, González‐Aveledo L, Capriles‐Hulett A, Caballero‐Fonseca F. Scabies, crusted (Norwegian) scabies and the diagnosis of mite sensitisation. Allergol Immunopathol (Madr). 2018;46(3):276‐280. [DOI] [PubMed] [Google Scholar]
- 6. Lee JJ, English JC 3rd. Teledermatology: a review and update. Am J Clin Dermatol. 2018;19(2):253‐260. [DOI] [PubMed] [Google Scholar]
- 7. Kanthraj GR. A longitudinal study of consistency in diagnostic accuracy of teledermatology tools. Indian J Dermatol Venereol Leprol. 2013;79(5):668‐678. [DOI] [PubMed] [Google Scholar]
- 8. Mounessa JS, Chapman S, Braunberger T, et al. A systematic review of satisfaction with teledermatology. J Telemed Telecare. 2018;24(4):263‐270. [DOI] [PubMed] [Google Scholar]
- 9. Skayem C, Cassius C, Ben Kahla M, et al. Teledermatology for COVID‐19 cutaneous lesions: substitute or supplement? J Eur Acad Dermatol Venereol. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


