A 61‐year‐old woman with type 2 diabetes mellitus presented to the emergency department with severe acute abdominal pain and vomiting. She was afebrile and had no other digestive or respiratory symptoms. She had no medical history of cardiovascular or rheumatic disease. On admission, laboratory results showed elevated transaminase levels (AST: 155 U/L, ALT: 313 U/L), increased C‐reactive protein (9.43 mg/L), low platelet count (46,000/μL) and high D‐dimer levels (43,998 μg/ml). A Computed tomography (CT) scan showed bibasal atelectasis, right hepatic vein thrombosis and a complete thrombosis of the splenoportal axis. Ileojejunal and right colon wall edema were also present as signs of tissue hypoperfusion changes (Fig. 1 a&b). Thrombophilia screening for both inherited and acquired causes was performed, and anticoagulation with Enoxaparin 1 mg/kg SC q12hr was started. Twelve hours after admission, the patient experienced rectal bleeding. Blood tests showed leukocytosis and a marked increase in serum transaminases levels (AST 2728 U/L, ALT 1065 U/L).
FIGURE 1.
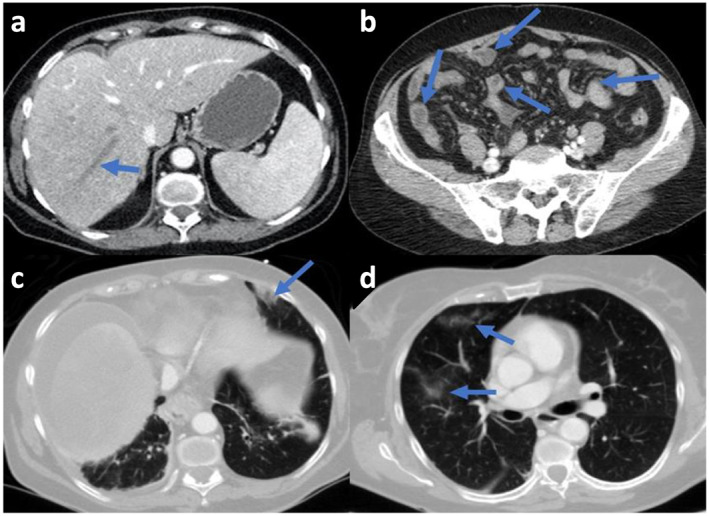
Abdominal CT scan (left) demonstrates thrombosis of the right hepatic vein and (right) thickening of the small bowel loops with absence of wall enhancement.
Both reverse‐transcriptase‐polymerase‐chain‐reaction (RT‐PCR) from nasopharyngeal swab and serologic testing were positive for SARS‐CoV2 infection, despite a negative RT‐PCR test in the other center 24 hours before. Lupus anticoagulant antibodies were detectable at low titer, but V617F Jak‐2, Factor V Leiden, prothrombin gene mutations anti‐cardiolipin IgG and anti–β2‐glycoprotein were negative. Due to deterioration in abdominal pain and clinical status, a second CT scan was performed. It showed worsening of liver, mesenteric and splenic ischemia and newly developed pulmonary opacities in left inferior and middle lobes (Fig. 1 c&d). Given the extent of the ischemia, the patient was not deemed a candidate for either surgery or radiological interventions. She died three days after onset of symptoms.
This case highlighted the fatal complication of hepatic vein thrombosis in the setting of SARS‐CoV2 infection. In addition, other unusual causes of venous thrombosis had been excluded. SARS‐CoV‐2 infection may predispose to both venous and arterial thromboembolism in critically ill patients. A 31% incidence of thrombotic complications in ICU patients with COVID‐19 has been reported, despite thromboprophylaxis. Severe inflammatory state, in conjunction with hypercoagulability and endothelial dysfunction, may explain this high incidence.
Splanchnic vein thrombosis, which includes both Budd‐Chiari syndrome (BCS) and non‐cirrhotic non‐tumoral portal vein thrombosis can lead to mesenteric ischemia, a severe condition with high mortality rate. At least one thrombotic risk factor has been identified in 60–80% of these patients. In the present case, apart from low‐titer lupus anticoagulant antibodies, no other predisposing risk factors were detected. However, it should be noted that these antibodies can arise transiently in patients with critical illness and various infections, including SARS‐CoV‐2, as well as in vascular liver diseases. Considering the negative results of other prothrombotic factors, COVID‐19 could explain this extensive splanchnic and hepatic vein thrombosis. This case suggests that COVID‐19 should be suspected in patients presenting with this syndrome, mainly during the pandemic context, in order to detect the infection promptly and to treat its thrombotic complications.
Del Hoyo, J. , López‐Muñoz, P. , Fernández‐de la Varga, M. , Garrido‐Marín, A. , Valero‐Pérez, E. , Prieto, M. , and Aguilera, V. (2020) Hepatobiliary and Pancreatic: A fatal case of extensive splanchnic vein thrombosis in a patient with Covid‐19. Journal of Gastroenterology and Hepatology, 35: 1853. 10.1111/jgh.15174.


