Abstract
Objectives
To assess the level of deterioration in functioning of ED patients during confinement, due to COVID‐19, and examine potential contributing factors (coping strategies, anxiety‐depressive symptomatology and personality traits).
Methods
A total of 74 ED patients in treatment before the COVID‐19 outbreak, contributed to this study. Baseline pre‐treatment evaluation included the SCL‐90R, TCI‐R, EDI‐2 and Y‐FAS 2.0 questionnaires for general psychopathology, personality and ED severity indexes. ED symptoms, coping strategies, socio‐demographic data and COVID‐19 concerns were collected by clinicians through a semi‐structured telephone survey during lockdown.
Results
A deterioration in ED symptoms and general psychopathology (anxiety and depression), during lockdown, was associated with low self‐directedness. Higher ED symptomatology during confinement was associated with less‐adaptive coping strategies to deal with lockdown situation leading to an increase in weight.
Conclusions
These specific vulnerability factors to further confinement or stressful situations may help design personalized preventive and therapeutic approaches.
Keywords: confinement, COVID‐19, eating disorders, mental health, personality
Highlights.
For the first time, associated factors were assessed as predictors of ED‐state during COVID‐19 lockdown.
Self‐directedness was associated with an aggravation of ED and general psychopathology during confinement.
ED worsening was linked to less‐adaptive coping strategies in confinement situation with a resulting weight increase.
1. INTRODUCTION
The COVID‐19 disease has caused major disruptions across the world, after being declared as a pandemic by the World Health Organization (WHO) on 31rst January 2020 (WHO, 2020). The pandemic has led to a break with ordinary routines and social contact for most of the world's population. People with prior mental health disorders have been found to relapse during the pandemic (González‐Sanguino et al., 2020; Moccia et al., 2020; Ozamiz‐Etxebarria, Dosil‐Santamaria, Picaza‐Gorrochategui, & Idoiaga‐Mondragon, 2020; Rajkumar, 2020; Temorshuizen et al., 2020; Weissman et al., 2020). Hao et al. (2020) found higher levels of concerns about their physical health, anger, anxiety, depression, impulsivity and intense suicidal ideation stress in psychiatric patients in comparison with healthy controls during COVID‐19 confinement. Moreover, evidence these effects may be long‐lasting (Shah et al., 2020).
Patients with eating disorders (ED) and/or obesity represent a vulnerable group (Cornejo‐Pareja, 2020;doi:10.1002/erv.2770 van Rensburg, 2020). Symptomatic deterioration such as purging, binging and exercise has been reported (Phillipou et al., 2020). Moreover the physical sequel of the disorders such as weight loss in anorexia nervosa (AN), electrolyte imbalance in bulimia nervosa (BN), or cardiovascular risk in binge eating disorder (BED) amplify the risk (Chew, Wei, Vasoo, Chua, & Sim, 2020; Fernández‐Aranda et al., 2020; Cornejo‐Pareja et al., 2020; Touyz, Lacey, & Hay, 2020). Also constraints in food supply chains may increase “food insecurity” (Temorshuizen et al., 2020; and increase food hoarding (Touyz et al., 2020) triggering bingeing (Fernández‐Aranda et al., 2020; Temorshuizen et al., 2020. Furthermore, emotional distress in the face of environmental changes is another triggering factor (Mediouni, Madiouni, & Kaczor‐Urbanowicz, 2020; Rodgers et al., 2020; Touyz et al., 2020; Clark‐Bryan et al., 2020;https://doi.org/10.1002/erv.2762 2020). Restrictions placed on movement may have limited adaptive strategies in the face of these difficulties (Rodgers et al., 2020) with reduced access to support (Weissmann, Bauer, & Thomas 2020; Fernandez‐Aranda et al., 2020). Graell et al., 2020; https://doi.org/10.1002/erv.2763).
In the general population, factors related to the psychological impact include as female sex (González‐Sanguino et al., 2020; Özdin & Bayrak Özdin, 2020; Wang, Di, Ye, & Wei, 2020), low educational level and lower perceived health status (Özdin & Bayrak Özdin, 2020; Wang et al., 2020), and high perceived vulnerability to infection and exposure to news (Olagoke, Olagoke, & Hughes, 2020; Yao, 2020). Personality factors associated with better adaptation include higher scores in the fight‐flight system (related to personal safety concerns) and lower scores in the behavioural inhibition system (related to anxiety) (Bacon & Corr, 2020); confidence (linked to secure attachment) and discomfort with closeness (associated with avoidant attachment) (Moccia et al., 2020) and conscientiousness (Carvalho, Pianowski, & Gonçalves, 2020).
To the best of our knowledge, ours is the first study that examines the factors that might contribute to a poorer adaptation to the COVID‐19 pandemic.
1.1. Aims
The main aim of this study is to assess the factors that impact on the adjustment of people with ED to the COVID‐19 confinement. We hypothesized that that poorer social support and non‐adaptive coping strategies would be associated with a greater adverse reaction.
2. METHOD
2.1. Participants
The sample was constituted of 74 adults, with female predominance (71 patients, 95.9%) and a mean age of 32.12 (±12.84) years old. They all were diagnosed with an ED and presented for treatment to the ED Unit within the Department of Psychiatry at a University Hospital in Spain: 19 AN, 12 BN, 10 BED and 33 Other Specified Feeding or Eating Disorder (OSFED). Patients were diagnosed according to DSM‐5 criteria (APA, 2013).
2.2. Procedure
The present study was carried out in accordance with the latest version of the Declaration of Helsinki. The University Hospital Clinical Research Ethics Committee approved the study, and signed informed consent was obtained from all participants.
We used a semi‐structured telephone survey designed by a clinician team from our Unit, regarding five main thematic blocks to explore: (a) socio‐demographic information; (b) ED‐status; (c) COVID‐19 concerns; (d) pandemic stress (anxiety, depressive symptoms, other situations, and family conflicts) and, (e) coping strategies. This survey was administered as part of a prospective follow‐up coinciding with official COVID‐19 lockdown in the region of Catalonia (Spain) from 14th March to 11th May 2020 and was administered during April 2020.
2.3. Assessments
2.3.1. Eating disorders inventory‐2 (EDI‐2) (Garner, 1991)
It consists of 91 items self‐report questionnaire, answered on a 6‐point Likert scale, which assesses different cognitive and behavioural characteristics concerning ED: Drive for Thinness, Bulimia, Body Dissatisfaction, Ineffectiveness, Perfectionism, Interpersonal Distrust, Interoceptive Awareness, Maturity Fears, Asceticism, Impulse Regulation, and Social Insecurity. The EDI‐2 provides standardized subscale scores and a global measure of ED severity, which can be obtained based on the sum of all the items. The validated version for the Spanish population (Garner, 1998) had a mean internal consistency of 0.63 (coefficient alpha). Internal consistency for the total score in this study was between adequate (Cronbach‐alpha α = .70 for maturity fears) to excellent (α = .953 for total score).
2.3.2. Yale food addiction scale 2.0 (YFAS‐2) (Gearhardt, Corbin, & Brownell, 2016)
It is a 35‐item self‐report questionnaire for measuring Food Addiction (FA) during the previous 12 months. It was based on the Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV‐TR) (APA, 2000) criteria for substance dependence and was adapted to the context of food consumption. YFAS‐2, a newer version of the instrument, is based on DSM‐5 Criteria (APA, 2013) and evaluates 11 symptoms. Two measurements are shown: (a) a continuous symptom count score that reflects the number of fulfilled diagnostic criteria (ranging from 0 to 11), and (b) a FA food addiction threshold based on the number of symptoms (at least two) and self‐reported clinically significant impairment or distress. This final measurement allows for the binary classification of FA food addiction (present versus absent). Moreover, based on the revised DSM‐5 taxonomy, it is possible to establish severity cut‐offs: mild (between two and three symptoms), moderate (between four and five symptoms), and severe (between six and eleven symptoms). The Spanish validation of the YFAS‐2 (Granero et al., 2018) had an internal consistency of 0.94 (coefficient alpha). In this study, internal consistency for the total score was excellent (α = .949).
2.3.3. Symptom checklist‐90‐revised (SCL‐90‐R) (Derogatis, 1990)
It consists of a 90‐item questionnaire that evaluates a broad range of psychological problems and symptoms of psychopathology by measuring nine primary symptom dimensions: Somatization, Obsession‐Compulsion, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, and Psychoticism. It also includes three global indices: global severity index (overall psychological distress), positive symptom distress index (the intensity of symptoms), and a positive symptom total (self‐reported symptoms). The global severity index can be used as a summary of the test. The validation of the scale in a Spanish population (Derogatis, 2002), obtained a mean internal consistency of .75 (coefficient alpha). The internal consistency for this study was between adequate (α = .763 for paranoid ideation) to excellent (α = .980 for global indexes).
2.3.4. Temperament and character inventory‐revised (TCI‐R) (Cloninger, Svrakic, Przybeck, & Whitehead, 1999)
This questionnaire is composed of 240‐items scored on a 5‐point Likert scale and measures personality derived from three character dimensions (Self‐Directedness, Cooperativeness, and Self‐Transcendence) and four temperament scales (Harm Avoidance, Novelty Seeking, Reward Dependence and Persistence). Evaluation of the Spanish revised version (Gutiérrez‐Zotes et al., 2004) generated an internal consistency of 0.87 (coefficient alpha). The questionnaire obtained internal consistency in this study between moderate (α = .739 for cooperativeness) to excellent (α = .900 for harm avoidance).
2.3.5. Semi‐structured brief telephone survey during COVID‐19 confinement (Eating Disorders Unit, Psychiatry Department, University Hospital, Spain, 2020)
First, sociodemographic information was up‐dated regarding lockdown period in terms of employment status, confinement compliance, affected environment by COVID‐19 and presence of company during this situation using dichotomous response (yes/no). The second part of the survey was related to ED‐state (measured as remaining equal, worsening, or remaining in the background). COVID‐19 concerns were classified as related to (a) own or family infection's risk and, (b) uncertain future, (c) employment status, (d) supply and access to treatments and, (e) other concerns. A yes /no evaluation of anxiety (psychical, emotional, motor, and cognitive dimensions), depressive symptoms (such as low mood, pessimism, or insomnia), other consequences (boredom or social conflicts) and familial conflicts were made. Finally, coping strategies during confinement were evaluated in two ways: (a) as presence or absence of both adaptive and non‐adaptive mechanisms and, (b) as well as the kind of strategies carried out by categorizing the coping mechanisms in dimensions (five for adaptive strategies: social contact; leisure; sports activities; daily routines; and academic/work activity and three dimensions for non‐adaptive ones: COVID‐19 over‐information; ED behaviours and other non‐adaptive behaviours. An extended version of this scale has been published in the current issue (Fernández‐Aranda et al., 2020).
2.4. Statistical analyses
Statistical analysis was carried out with Stata16 for windows (Stata Press, 2019). The comparison between the groups of the study was done through chi‐square tests (χ 2) for categorical variables and t test for quantitative measures. Effect size for the proportion and the mean differences was estimated with Cohen's‐d coefficient, considering null effect for |d| < 0.20, low‐poor for |d| > 0.20, mild‐medium for |d| > 0.50 and large‐high for |d| > 0.80) (Cohen, 1988; Kelley & Preacher, 2012).
Path analysis procedure assessed the underlying relationships between the variables of the study (direct and indirect links, including mediational associations). This analysis was carried out as a case of structural equation modelling (SEM), with the maximum‐likelihood estimation method of parameter estimation. Due the large number of contextual and personal variables characterizing the COVID‐19 confinement, a latent variable was defined (labelled as “COVID” in the model, defined by the presence of concerns, adaptive reactions, non‐adaptive reactions, anxiety, depression, other problems and familiar conflicts). The goodness‐of‐fit was tested with standard statistical measures: χ 2 test, the root mean square error of approximation (RMSEA), Bentler's Comparative Fit Index (CFI), the Tucker‐Lewis Index (TLI), and the standardized root mean square residual (SRMR). Adequate fit was considered for (Barrett, 2007) non‐significant result in the χ 2 test, RMSEA<0.08, TLI > 0.90, CFI > 0.90 and SRMR<0.10.
3. RESULTS
3.1. Characteristics of the participants previous and during the confinement
Coinciding with the lockdown, most patients were undergoing outpatient treatment (73 patients, 98.6%). Almost 27% (20 patients) of the sample were actively working, almost 95% (70 patients, 94.6%) had social support and only 17.6% (13 patients) had close people affected by COVID‐19.
The presence of concerns related with the confinement for COVID‐19 was reported by 52 patients (70.3%), a high prevalence of patients used adaptive reactions (n = 70, 94.6%), 19 patients (25.7%) also reported non‐adaptive reactions. The presence of anxiety symptoms was reported by 31 participants (41.9%) and depression by 22 (29.7%). Familial conflicts were noted by 15 individuals (20.3%) and other difficulties 34 patients (45.9%).
Symptom evolution during the confinement due to the COVID‐19, worsened in n = 19 patients (25.7%), and became less dominant in n = 38 (51.4). For this study, the participants were re‐classified in two groups based on the ED state during the confinement: symptom deterioration (n = 19) or not (n = 55).
3.2. Comparison of groups based on the ED progression during COVID‐19 lockdown
No differences between these two groups were found for the marital status (p = .845), education levels (p = .796), social index (p = .555), and diagnostic subtype (p = .294) (see Table S1, supplementary material).
Table 1 displays the comparisons between the groups of the study for the variables registered during the COVID‐19 lockdown. Patients who noticed an ED worsening reported higher prevalence of future concerns, such as access to medical treatment, non‐adaptive reactions, symptoms of anxiety and depression, adverse situations and familiar conflict.
TABLE 1.
Association between the ED‐state during the confinement with the measures registered during the COVID‐19
| Worse n = 19 | Non‐worse n = 55 | |||||
|---|---|---|---|---|---|---|
| n | % | n | % | p | |d| | |
| COVID‐related concerns | 16 | 84.2 | 36 | 65.5 | .123 | 0.44 |
| Concerns: Infection risk | 7 | 36.8 | 14 | 25.5 | .343 | 0.25 |
| Concerns: Uncertain future | 10 | 52.6 | 16 | 29.1 | .046 * | 0.51 a |
| Concerns: Employment | 4 | 21.1 | 11 | 20.0 | .922 | 0.03 |
| Concerns: Medical treatments | 4 | 21.1 | 1 | 1.8 | .004 * | 0.68 a |
| Concerns: Other | 4 | 21.1 | 6 | 10.9 | .265 | 0.28 |
| Adaptive reactions | 17 | 89.5 | 53 | 96.4 | .252 | 0.28 |
| Adaptive reactions: Social | 1 | 5.3 | 13 | 23.6 | .078 | 0.55 a |
| Adaptive reactions: Leisure | 8 | 42.1 | 34 | 61.8 | .135 | 0.40 |
| Adaptive reactions: Sport | 2 | 10.5 | 15 | 27.3 | .135 | 0.44 |
| Adaptive reactions: Routine | 8 | 42.1 | 34 | 61.8 | .135 | 0.40 |
| Adaptive reactions: Work/studies | 8 | 42.1 | 14 | 25.5 | .171 | 0.35 |
| Non‐adaptive reactions | 10 | 52.6 | 9 | 16.4 | .002 * | 0.79 a |
| Non‐adaptive reactions: COVID | 1 | 5.3 | 0 | 0.0 | .575 | 0.46 |
| Non‐adaptive reactions: ED | 5 | 26.3 | 6 | 10.9 | .104 | 0.40 |
| Non‐adaptive reactions: Other | 4 | 21.2 | 2 | 3.6 | .016 * | 0.57 a |
| Anxiety | 14 | 73.7 | 17 | 30.9 | .001 * | 0.89 a |
| Anxiety: Physic | 6 | 31.6 | 10 | 18.2 | .221 | 0.31 |
| Anxiety: Emotional | 13 | 68.4 | 14 | 25.5 | .001 * | 0.89 a |
| Anxiety: Motor | 6 | 31.6 | 4 | 7.3 | .008 * | 0.65 a |
| Anxiety: Cognitive | 13 | 68.4 | 11 | 20.0 | .001 * | 1.02 a |
| Depression | 12 | 63.2 | 10 | 18.2 | .001 * | 0.96 a |
| Other situations | 13 | 68.4 | 21 | 38.2 | .023 * | 0.62 a |
| Familiar conflicts | 8 | 42.1 | 7 | 12.7 | .006 * | 0.68 a |
Bold: significant comparison.
Bold: effect size into the range mild–moderate (|d| > 0.50) to high‐large (|d| > 0.80).
Table 2 compares the baseline assessment between the groups. Self‐directedness was lower in the group with deterioration in their ED symptoms: 117.4 versus 127.6; p = .048, |d| = 0.51).
TABLE 2.
Association between the ED‐state during the confinement with the clinical measures prior to the COVID‐19
| Worse n = 19 | Non‐worse n = 55 | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p | |d| | |
| Age (yrs‐old) | 32.53 | 13.60 | 31.98 | 12.69 | .875 | 0.04 |
| Onset of the ED (yrs‐old) | 16.42 | 4.22 | 16.62 | 5.80 | .892 | 0.04 |
| Duration of the ED (yrs) | 14.49 | 11.56 | 14.60 | 11.32 | .971 | 0.01 |
| EDI‐2: Drive for thinness | 13.16 | 4.65 | 12.42 | 6.68 | .657 | 0.13 |
| EDI‐2: Body dissatisfaction | 17.63 | 7.03 | 14.80 | 8.24 | .185 | 0.37 |
| EDI‐2: Interoceptive awareness | 12.47 | 7.80 | 10.44 | 6.72 | .278 | 0.28 |
| EDI‐2: Bulimia | 6.26 | 4.63 | 5.55 | 5.46 | .610 | 0.14 |
| EDI‐2: Interpersonal distrust | 6.16 | 4.82 | 5.58 | 5.09 | .668 | 0.12 |
| EDI‐2: Ineffectiveness | 11.63 | 5.89 | 9.98 | 7.36 | .380 | 0.25 |
| EDI‐2: Maturity fears | 7.42 | 5.49 | 8.07 | 5.06 | .637 | 0.12 |
| EDI‐2: Perfectionism | 4.84 | 3.47 | 6.04 | 4.84 | .326 | 0.28 |
| EDI‐2: Impulse regulation | 6.89 | 4.48 | 5.20 | 5.98 | .263 | 0.32 |
| EDI‐2: Ascetic | 7.95 | 4.39 | 6.89 | 4.93 | .411 | 0.23 |
| EDI‐2: Social insecurity | 7.68 | 4.99 | 6.89 | 5.11 | .559 | 0.16 |
| EDI‐2: Total score | 102.11 | 38.99 | 91.87 | 45.33 | .383 | 0.24 |
| SCL‐90R: Somatization | 1.49 | 0.98 | 1.83 | 0.94 | .189 | 0.35 |
| SCL‐90R: Obsess./compulsive | 1.93 | 0.80 | 1.87 | 0.82 | .779 | 0.08 |
| SCL‐90R: Interpersonal sensitivity | 2.03 | 0.95 | 1.95 | 1.03 | .757 | 0.08 |
| SCL‐90R: Depressive | 2.32 | 0.85 | 2.15 | 1.01 | .512 | 0.18 |
| SCL‐90R: Anxiety | 1.55 | 0.91 | 1.59 | 0.97 | .899 | 0.03 |
| SCL‐90R: Hostility | 1.65 | 1.21 | 1.25 | 1.03 | .167 | 0.36 |
| SCL‐90R: Phobic anxiety | 0.86 | 0.86 | 1.14 | 1.00 | .281 | 0.30 |
| SCL‐90R: Paranoid ideation | 1.34 | 0.65 | 1.39 | 0.91 | .837 | 0.06 |
| SCL‐90R: Psychotic | 1.29 | 0.87 | 1.27 | 0.76 | .909 | 0.03 |
| SCL‐90R: PST score | 1.70 | 0.77 | 1.70 | 0.81 | .997 | 0.00 |
| SCL‐90R: GSI score | 60.00 | 19.17 | 63.15 | 17.67 | .515 | 0.17 |
| SCL‐90R: PSDI score | 2.42 | 0.57 | 2.28 | 0.61 | .373 | 0.24 |
| YFAS: Total score | 5.74 | 3.65 | 5.58 | 3.69 | .875 | 0.04 |
| TCI‐R: Novelty seeking | 97.11 | 13.35 | 97.24 | 17.07 | .976 | 0.01 |
| TCI‐R: Harm avoidance | 117.53 | 18.34 | 115.51 | 21.90 | .720 | 0.10 |
| TCI‐R: Reward dependence | 103.53 | 14.30 | 101.33 | 17.95 | .631 | 0.14 |
| TCI‐R: Persistence | 114.05 | 22.51 | 115.27 | 19.02 | .819 | 0.06 |
| TCI‐R: Self‐directedness | 117.37 | 20.96 | 127.56 | 18.70 | .048 * | 0.51 a |
| TCI‐R: Cooperativeness | 133.89 | 9.69 | 137.85 | 13.19 | .234 | 0.34 |
| TCI‐R: Self‐transcendence | 64.37 | 14.86 | 65.82 | 16.71 | .739 | 0.09 |
Bold: significant comparison.
Bold: effect size into the range mild–moderate (|d| > 0.50) to high‐large (|d| > 0.80).
Table S2 (supplementary material) contains the point‐serial correlation matrix with the associations between the variables measuring during the confinement with the clinical state registered previous to the COVID‐19 lockdown. The presence of concerns during the confinement was related to older age and lower EDI‐2 drive for thinness score. Non‐adaptive reactions were reported by patients with higher score in the YFAS‐2 scale, and depression symptoms were related to worse psychopathological state.
3.3. Path analysis
Figure 1 contains the path‐diagram with the standardized coefficients obtained in the SEM. Adequate fitting was obtained: χ 2 = 67.84 (p = .201), RMSEA = 0.045, CFI = 0.958, TLI = 0.945 and SRMR = 0.087.
FIGURE 1.
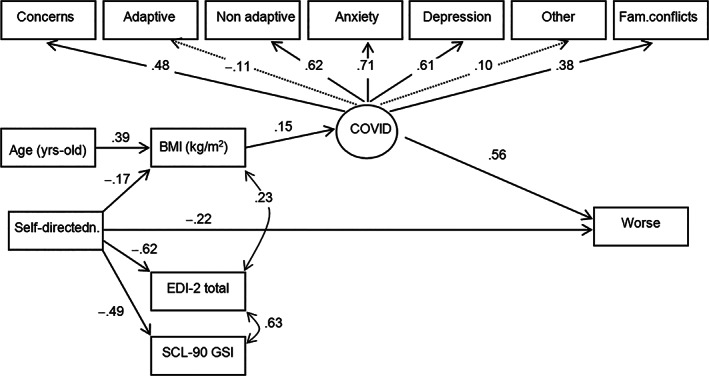
Path‐diagram with the standardized coefficients. Note. Continuous line: significant coefficient. Dash line: non‐significant coefficient
The latent variable measuring the contextual and personal features during the COVID‐19 lockdown was associated with concerns related to the confinement, non‐adaptive reactions, anxiety, depression and familial conflicts. Results from the SEM suggest that a poorer state during the COVID‐19 lockdown and lower TCI‐R self‐directedness score increase the likelihood of deteriorating ED symptoms during the confinement (direct effects). The COVID‐19 latent variable was also a mediational variable in the model: indicating that age, self‐directedness and BMI, contributed indirectly to the deterioration in ED symptoms.
4. DISCUSSION
The present study explored the factors associated with symptomatic deterioration in people with ED. A quarter of patients became more symptomatic during lockdown a similar proportion to that found during the first weeks of confinement (Fernández‐Aranda et al., 2020). The deterioration was higher in people with AN followed by those with OSFED. This differential pattern aligns with other studies (Temorshuizen et al., 2020).
A novel feature of the present work was the association of symptom deterioration with low levels of self‐directedness. This aligns with other work in confinement Moccia et al. (2020) and to the extensive literature associating in ED lower self‐directedness to poorer prognosis (Duffy et al., 2019; Krug et al., 2011). Age and ED severity, named drive for thinness (EDI‐2), were also related with COVID‐19 concerns. Patients with FA food addiction at baseline (Y‐FAS 2.0) had more non‐adaptive responses during COVID‐19 lockdown.
Finally, some strengths of this study should be highlighted. For instance, as the sample was comprised of patients who were linked to our unit before COVID‐19 outbreak, the baseline assessment was thorough. The use of a telephone interview rather than self‐report post COVID may have increased reliability. However, the sample size was modest and was without a control comparison.
5. CONCLUSIONS
In conclusion, the present findings suggest that an about a quarter of patient with an ED showed a deterioration in symptomatology, post COVID and this was mainly associated with lower self‐directedness. These results suggest the relevance of identifying specific vulnerability factors among ED patients in a confinement situation in order to develop preventive strategies and personalized treatment approaches.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Table S1 Association between the ED‐state during the confinement with sociodemographics, diagnosis subtype and treatment type
Table S2 Point‐biserial correlation matrix between the clinical measures prior to the COVID‐19 with the measures registered during the confinement
ACKNOWLEDGEMENTS
We thank CERCA Programme/Generalitat de Catalunya for institutional support. This work was partially supported by Instituto de Salud Carlos III (PI17/01167) and Generalitat de Catalunya (PERIS/SLT006/17/00246). CIBERObn is an initiative of ISCIII Spain. IB was partially supported by a Post‐Residency Grant from Research Committee of the University Hospital of Bellvitge (HUB; Barcelona, Spain) 2019‐2020. CVA is supported by a FPU grant (FPU16/01453) from Ministerio de Educación, Cultura y Deporte (Spain). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Baenas I, Caravaca‐Sanz E, Granero R, et al. COVID‐19 and eating disorders during confinement: Analysis of factors associated with resilience and aggravation of symptoms. Eur Eat Disorders Rev. 2020;28:855–863. 10.1002/erv.2771
Funding information Centro de Investigación Biomédica en Red‐Fisiopatología de la Obesidad y Nutrición; Generalitat de Catalunya ‐ PERIS, Grant/Award Number: SLT006/17/00246; Instituto de Salud Carlos III, Grant/Award Number: PI17/01167; Ministerio de Educación, Cultura y Deporte (Spain)‐ FPU, Grant/Award Number: FPU16/01453; Post‐Residency Grant from Research Committee of the University Hospital of Bellvitge (HUB; Barcelona, Spain) 2019‐2020
REFERENCES
- APA . (2000). Diagnostic and statistical manual of mental disorders (4th text revision ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- APA . (2013). Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association. [Google Scholar]
- Bacon, A. M. , & Corr, P. J. (2020). Coronavirus (COVID‐19) in the United Kingdom: A personality‐based perspective on concerns and intention to self‐isolate. British Journal of Health Psychology, 1–10. 10.1111/bjhp.12423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett, P. (2007). Structural equation modelling: Adjudging model fit. Personality and Individual Differences, 42(5), 815–824. 10.1016/j.paid.2006.09.018 [DOI] [Google Scholar]
- Carvalho, L. D. F. , Pianowski, G. , & Gonçalves, A. P. (2020). Personality differences and COVID‐19: Are extroversion and conscientiousness personality traits associated with engagement with containment measures? Trends in Psychiatry and Psychotherapy, 0, 1–6. 10.1590/2237-6089-2020 [DOI] [PubMed] [Google Scholar]
- Chew, Q. H. , Wei, K. C. , Vasoo, S. , Chua, H. C. , & Sim, K. (2020). Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID‐19 pandemic. Singapore Medical Journal, 1–31. 10.11622/smedj.2020046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloninger, C. R. , & (1999). In The Temperament and Character Inventory–Revised. St Louis: MO: Center for Psychobiology of Personality, Washington University. [Google Scholar]
- Cohen, J. (1988). Statistical power for the behavioral sciences (2nd ed.). Hillsdale, NJ: Laurence Erlbaum and Associates. [Google Scholar]
- Derogatis, L. (1990). SCL‐90‐R. Administration, scoring and procedures manual—II for the revised version. Baltimore, MD: Clinical Psychometric Research. [Google Scholar]
- Derogatis, L. (2002). SCL‐90‐R. Cuestionario de 90 Síntomas‐Manual. Madrid, Spain: TEA, Ed. [Google Scholar]
- Duffy, M. E. , Rogers, M. L. , Joiner, T. E. , Bergen, A. W. , Berrettini, W. , Bulik, C. M. , … Keel, P. K. (2019). An investigation of indirect effects of personality features on anorexia nervosa severity through interoceptive dysfunction in individuals with lifetime anorexia nervosa diagnoses. International Journal of Eating Disorders, 52, 200–205. 10.1002/eat.23008 [DOI] [PubMed] [Google Scholar]
- Fernández‐Aranda, F. , Casas, M. , Claes, L. , Bryan, D. C. , Favaro, A. , Granero, R. , … Treasure, J. (2020). COVID‐19 and implications for eating disorders. European Eating Disorders Review: The Journal of the Eating Disorders Association, 28(3), 239–245. 10.1002/erv.2738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner, D. (1991). Eating disorder inventory‐2, Odena: Psychological Assessment Resources. [Google Scholar]
- Garner, D. M. (1998). Inventario de Trastornos de la Conducta Alimentaria (EDI‐2)‐Manual. Madrid, Spain: TEA ediciones. [Google Scholar]
- Gearhardt, A. N. , Corbin, W. R. , & Brownell, K. D. (2016). Development of the Yale food addiction scale version 2.0. Psychology of Addictive Behaviors, 30(1), 113–121. 10.1037/adb0000136 [DOI] [PubMed] [Google Scholar]
- González‐Sanguino, C. , Ausín, B. , Castellanos, M. Á. , Saiz, J. , López‐Gómez, A. , Ugidos, C. , & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID‐19) in Spain. Brain, Behavior, and Immunity, 87, 172–176. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granero, R. , Jiménez‐Murcia, S. , Gerhardt, A. N. , Agüera, Z. , Aymamí, N. , Gómez‐Peña, M. , … Fernández‐Aranda, F. (2018). Validation of the Spanish version of the Yale Food Addiction Scale 2.0 (YFAS 2.0) and clinical correlates in a sample of eating disorder, gambling disorder, and healthy control participants. Frontiers in Psychiatry, 9, 208. 10.3389/fpsyt.2018.00208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutiérrez‐Zotes, J. A. , Bayón, C. , Montserrat, C. , Valero, J. , Labad, A. , Cloninger, C. R. , & Fernández‐Aranda, F. (2004). Inventario del Temperamento y el Carácter‐Revisado (TCI‐R). Baremación y datos normativos en una muestra de población general. Actas Espanolas de Psiquiatria, 32(1), 8–15. [PubMed] [Google Scholar]
- Hao, F. , Tan, W. , Jiang, L. , Zhang, L. , Zhao, X. , Zou, Y. , … Tam, W. (2020). Do psychiatric patients experience more psychiatric symptoms during COVID‐19 pandemic and lockdown? A case‐control study with service and research implications for immunopsychiatry. Brain, Behavior, and Immunity, 87, 100–106. 10.1016/j.bbi.2020.04.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley, K. , & Preacher, K. J. (2012). On effect size. Psychological Methods, 17(2), 137–152. 10.1037/a0028086 [DOI] [PubMed] [Google Scholar]
- Krug, I. , Root, T. , Bulik, C. , Granero, R. , Penelo, E. , Jiménez‐Murcia, S. , & Fernández‐Aranda, F. (2011). Redefining phenotypes in eating disorders based on personality: A latent profile analysis. Psychiatry Research, 188, 439–445. 10.1016/j.psychres.2011.05.026 [DOI] [PubMed] [Google Scholar]
- Mediouni, M. , Madiouni, R. , & Kaczor‐Urbanowicz, K. E. (2020). COVID‐19: How the quarantine could lead to the depreobesity. Obesity Medicine, 19, 100255. 10.1016/j.obmed.2020.100255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia, L. , Janiri, D. , Pepe, M. , Dattoli, L. , Molinaro, M. , De Martin, V. , … Di Nicola, M. (2020). Affective temperament, attachment style, and the psychological impact of the COVID‐19 outbreak: An early report on the Italian general population. Brain, Behavior, and Immunity, 87, 75–79. 10.1016/j.bbi.2020.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olagoke, A. A. , Olagoke, O. O. , & Hughes, A. M. (2020). Exposure to coronavirus news on mainstream media: The role of risk perceptions and depression. British Journal of Health Psychology, e12427. 10.1111/bjhp.12427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozamiz‐Etxebarria, N. , Dosil‐Santamaria, M. , Picaza‐Gorrochategui, M. , & Idoiaga‐Mondragon, N. (2020). Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID‐19 en una muestra recogida en el norte de España. Cadernos De Saude Publica, 36(4), e00054020. 10.1590/0102-311X00054020 [DOI] [PubMed] [Google Scholar]
- Özdin, S. , & Bayrak Özdin, Ş. (2020). Levels and predictors of anxiety, depression and health anxiety during COVID‐19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry, 002076402092705. 10.1177/0020764020927051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipou, A. , Meyer, D. , Neill, E. , Tan, E. J. , Toh, W. L. , Van Rheenen, T. E. , & Rossell, S. L. (2020). Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: Initial results from the COLLATE project. The International Journal of Eating Disorders, 53(7), 1158–1165. 10.1002/eat.23317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar, R. P. (2020). COVID‐19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, R. F. , Lombardo, C. , Cerolini, S. , Franko, D. L. , Omori, M. , Fuller‐Tyszkiewicz, M. , … Guillaume, S. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. The International Journal of Eating Disorders, 53(7), 1166–1170. 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah, K. , Kamrai, D. , Mekala, H. , Mann, B. , Desai, K. , & Patel, R. S. (2020). Focus on mental health during the coronavirus (COVID‐19) pandemic: Applying learnings from the past outbreaks. Cureus, 12, (3), e7405. 10.7759/cureus.7405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Press . (2019). Stata statistical software: Release 16. Statistical Software. College Station, Texas: StataCorp LLC. [Google Scholar]
- Temorshuizen, J. D. , Watson, H. J. , Thornton, L. M. , Borg, S. , Flatt, R. E. , MacDermod, C. M. , … Bulik, C. M. (2020). Early impact of COVID‐19 on individuals with eating disorders: A survey of ~1000 individuals in the United States and The Netherlands. medRxiv. 10.1101/2020.05.28.20116301 [DOI] [PubMed] [Google Scholar]
- Todisco, P. , & Donini, L. M. (2020). Coronavirus disease 2019 (COVID‐19) and obesity. Impact of obesity and its main comorbidities in the evolution of the disease. European Eating Disorders Review, (0123456789), 10–13. 10.1007/s40519-020-00938-z [DOI] [PubMed] [Google Scholar]
- Touyz, S. , Lacey, H. , & Hay, P. (2020). Eating disorders in the time of COVID‐19. Journal of Eating Disorders, 8(1), 8–10. 10.1186/s40337-020-00295-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rensburg, M. J. (2020). COVID19, the pandemic which may exemplify a need for harm‐reduction approaches to eating disorders: A reflection from a person living with an eating disorder. Journal of Eating Disorders, 31(8), 26. 10.1186/s40337-020-00306-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , Di, Y. , Ye, J. , & Wei, W. (2020). Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID‐19) in some regions of China. Psychology, Health and Medicine, 1–10. 10.1080/13548506.2020.1746817 [DOI] [PubMed] [Google Scholar]
- Weissman, R. S. , Bauer, S. , & Thomas, J. J. (2020). Access to evidence‐based care for eating disorders during the COVID‐19 crisis. International Journal of Eating Disorders, 53(5), 369–376. 10.1002/eat.23279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2020). WHO Director‐Generals opening remarks at the mission briefing on COVID‐19. https://doi.org/11 March 2020.
- Yao, H. (2020). The more exposure to media information about COVID‐19, the more distressed you will feel. Brain, Behavior, and Immunity, 87, 167–169. 10.1016/j.bbi.2020.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Association between the ED‐state during the confinement with sociodemographics, diagnosis subtype and treatment type
Table S2 Point‐biserial correlation matrix between the clinical measures prior to the COVID‐19 with the measures registered during the confinement


