Editor's note: This special report highlights practices that were implemented by individual facilities in response to the COVID‐19 pandemic. Some practices may be inconsistent with evidence‐based practice and/or the AORN Guidelines and may be modified or obsolete by the time of publication. In addition, some practices (eg, N95 and other respirator reprocessing) have been approved by the US Food and Drug Administration for emergency use only in response to the pandemic.
Perioperative teams are no strangers to emergency response, but one of the differences of the Coronavirus Disease 2019 (COVID‐19) pandemic compared with other emergencies has been its longevity. No emergency in modern history has lasted as long, which has forced facilities to halt elective surgeries for months, required the conversion of hospital spaces to surge units for critically ill patients, and significantly diminished personal protective equipment (PPE) supplies. Perioperative leaders have shown agile responses, including quickly pulling together and mobilizing incident command centers, augmenting and modifying existing emergency management protocols, working together to agree on COVID‐19 clinical protocols, and enhancing communication efforts with their teams to keep everyone apprised of the rapidly changing situation. Perioperative team members also have excelled at innovation through the development and implementation of new practice tools to help manage the pandemic response.
EMERGENCY RESPONSE
Incident command centers have been central to pandemic response in many health care facilities. Their collaborative nature and inclusion of interdepartmental staff members have been keys to their success. Although the situation from state to state varied, one consistency among the COVID‐19 responses was the quick and efficient way that hospital teams mobilized their incident command centers to organize their pandemic response. Perioperative leaders were instrumental in their contributions to these efforts as they identified and filled gaps and regularly shared information with their colleagues and teams.
Like other health care facilities, OSF Saint Anthony's Health Center (SAHC) in Alton, Illinois, has emergency protocols in place. Because of their location in the Midwest near the convergence of three major rivers, personnel at this facility are prepared to respond to health emergencies occurring after extreme weather and accidents from nearby refineries, highways, and farming operations. The current crisis included new challenges, however, in that it also closed community resources and significantly increased PPE needs.
“The first indication we had issues was on a Friday afternoon when Governor Prisker announced that he's closing daycares, schools, all these kinds of things on the following Tuesday,” said Colleen Becker, RN, vice president and chief nursing officer at OSF SAHC. As a result, the leadership team met over the weekend to mobilize a command center that included staff members from human resources, occupational health, and infection prevention, among others. According to Becker, having the right voices at the table helped the leadership team to “be as nimble as possible.”
At St. Cloud Hospital, part of the CentraCare health care system in Minnesota, administrative leaders initiated the incident command center in late January. Since that time, “…it's been going full speed, nonstop, 24/7,” said Larry Asplin, MSN, RN, CNOR, CSSM, director of surgery at CentraCare. Having this team in place—which includes leaders from infection prevention and control and employee health services, in addition to senior nursing leaders and other senior leaders—has been critical for ensuring a consistent and coordinated response.
As of mid‐May, the incident command center at Beth Israel Deaconess Medical Center (BIDMC), Boston, Massachusetts, had been in place for 11 weeks, according to Elena Canacari, BSN, RN, associate chief nurse for perioperative services. Because of the prolonged nature of this crisis and the need for consistency, the BIDMC team adjusted the typical incident command structure—which would normally rotate the administrator‐on‐call role week by week—and appointed the chief nursing officer as the incident commander. For additional consistency, administrators communicated the policy changes and procedures to staff members across the Beth Israel Lahey Health system, so that regardless of where a patient entered the system—a clinic, the emergency room, or another area—staff members used standardized messaging.
“It's very comforting to patients to know that they're not hearing a different story from each one of us as we're going through trying to care for them,” Canacari said. “Standard patient pathways were developed. That standardization has helped ensure stability in a pretty unstable time.”
COVID‐19 PROTOCOLS
The COVID‐19 information (eg, transmissibility, PPE requirements) changed quickly and added to the feeling of instability for staff members and leaders. In perioperative services, leader responses to the changing recommendations required interdepartmental collaboration and a tenacious focus on patient and team member safety. The incident command structure and the various teams that administrators created to address crisis issues helped leaders reach consensus on new protocols so they could roll out changes as a unified group, whether to a single community hospital or a large health system. Protocol changes included new requirements for staff member, patient, and visitor screening; conversions of physical spaces; careful consideration when determining which surgeries are urgent or emergent and must proceed; and updated PPE requirements.
At many health care facilities, leaders required visitor and patient screenings upon entry to the building in an effort to minimize the spread of COVID‐19. During the pandemic response, staff members manning the doors to health care facilities have relied on screening tools and questionnaires—such as the one developed at Roper St. Francis Hospital in Charleston, South Carolina (Sidebar 1)—to help determine whether visitors might be infected.
Sidebar 1. COVID‐19 Patient Screening and Rescreening Questions at Roper St. Francis Healthcare System, Charleston, South Carolina.
Do you have
a fever (100.4° F [38° C] or higher according to the Centers for Disease Control and Prevention),
a cough (dry or productive),
shortness of breath,
difficulty breathing,
a sore throat,
laryngitis,
a headache,
fatigue,
myalgias,
diarrhea,
nausea, or
a sudden loss of taste or smell?
As perioperative department leaders canceled scheduled elective surgeries, leaders and staff members converted perioperative spaces to accommodate a potential influx of critically ill patients. At OSF SAHC, staff members completely changed the perioperative services area: they added negative airflow rooms and updated the patient flow to use preoperative and postoperative areas as a COVID‐19 cohort unit. These changes required perioperative and other nursing leaders to collaborate with the information technology team members to convert rooms and ensure nursing staff members could document patient care in the electronic health record. In addition, these changes required input and approval from the facilities department leaders, anesthesia professionals, and intensive care unit (ICU) physicians before implementation.
Facility personnel converted two postanesthesia care units at BIDMC into alternate care sites that became COVID‐19 units. The switch took time because of social distancing guidelines, air balancing, and erecting walls, according to Canacari. Realizing the need to repeat this conversion process multiple times, the team created a procedure for how to convert a postanesthesia care unit into an ICU (Figure 1).
Figure 1.
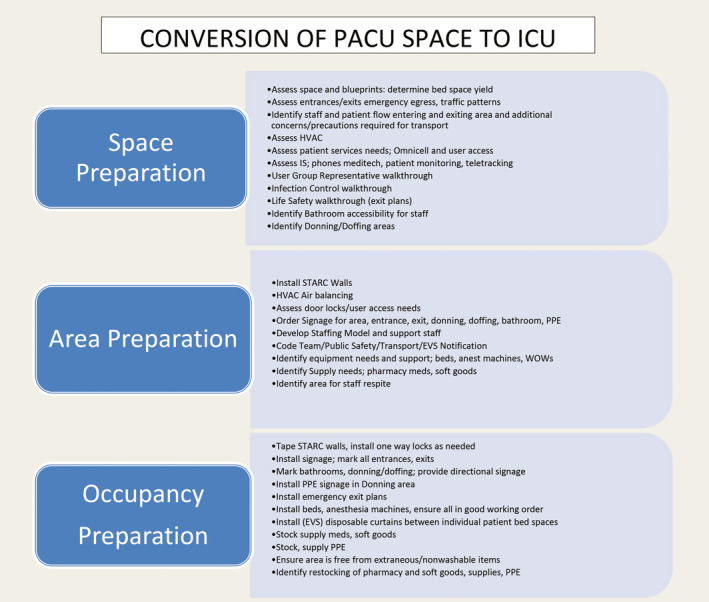
Converting a postanesthesia care unit to an intensive care unit. PACU = postanesthesia care unit; ICU = intensive care unit; HVAC = heating, ventilation, and air conditioning; IS = information services; PPE = personal protective equipment; EVS = environmental services; anest = anesthesia; WOWs = workstations on wheels. Copyright © 2020, Beth Israel Deaconess Medical Center, Boston, MA. Editor's notes: Omnicell is a registered trademark of Omnicell, Inc, Mountain View, CA. STARC is a registered trademark of STARC Systems, LLC, Brunswick, ME.
Leaders at Baylor University Medical Center, Dallas, Texas, developed visual management tools to assist team members with donning and folding masks correctly, transporting patients according to newly established routes, and managing their masks properly for resterilization (Figure 2). These tools were especially helpful for employees who came in from other teams to help and may not have been familiar with the protocols, said Patricia M. DeFrehn, DNP, MBA, RN, NEA‐BC, vice president, surgery and neuroscience.
Figure 2.
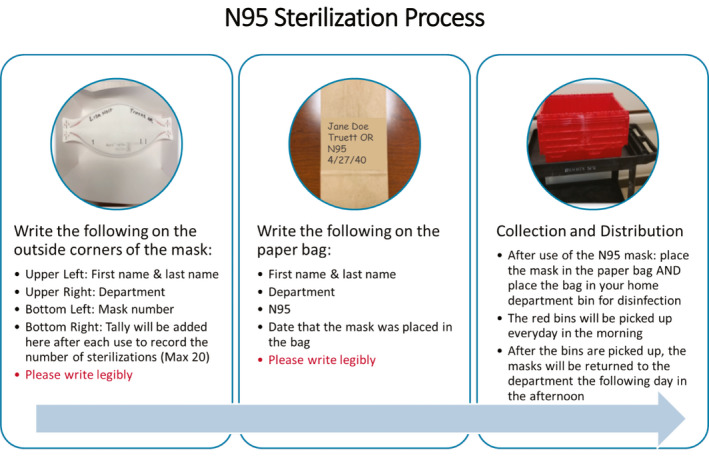
Sterilization process for an N95 respirator used by personnel at Baylor University Medical Center, Dallas, Texas. Max = maximum. Copyright © 2020, Baylor University Medical Center, Dallas, TX.
Although leaders did not discontinue all surgeries during the pandemic response, all planned surgeries required a careful review for medical necessity. “To determine which cases would proceed, the team at Roper St. Francis Healthcare developed an elective surgery algorithm based on patient acuity,” said Stephanie McKoin, RN, director of perioperative services and the surgery integrated practice network (Figure 3). The tool also helped providers identify urgent or emergent procedures, the need for intraoperative or postoperative blood administration, and patients who would require an ICU bed postoperatively. For nonemergent procedures, a team including McKoin, the medical director of the surgery integrated practice network, and two anesthesiologists reviewed the planned procedure together and determined whether to proceed or not. For urgent procedures, the team used a preoperative workflow screening process (Figure 4).
Figure 3.
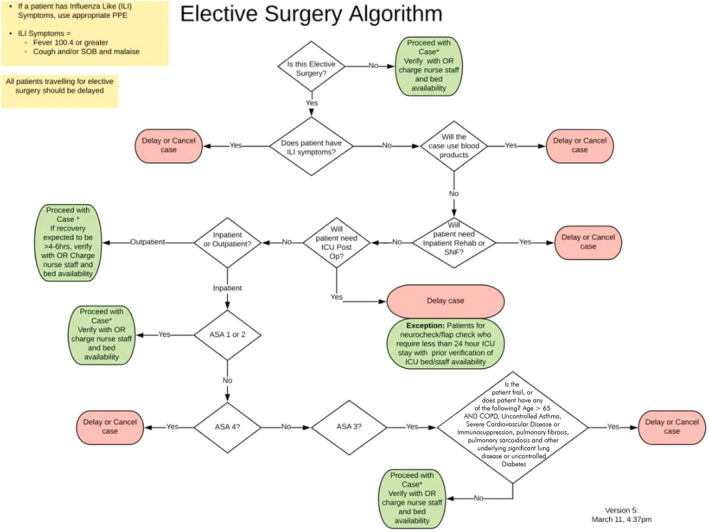
Elective surgery algorithm. ILI = influenza‐like illness; PPE = personal protective equipment; SOB = shortness of breath; ICU = intensive care unit; Post Op = postoperatively; Rehab = rehabilitation; SNF = skilled nursing facility; ASA = American Society of Anesthesiologists; COPD = chronic obstructive pulmonary disease. Copyright © 2020, Roper St. Francis Hospital, Charleston, SC.
Figure 4.
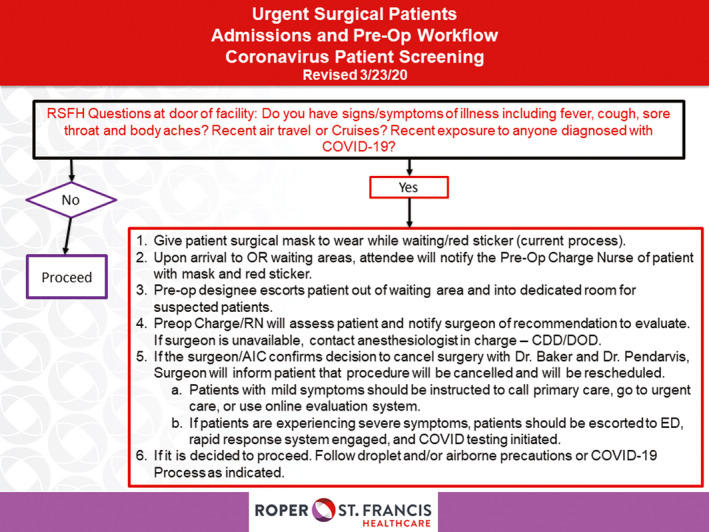
Urgent surgical patient admission and preoperative workflow for Coronavirus Disease 2019 patient screening. Pre‐Op = preoperative; RSFH = Roper St. Francis Hospital; ED = emergency department; COVID‐19 = Coronavirus Disease 2019; CDD = clinical doctor of the day; DOD = doctor of the day. Copyright © 2020, Roper St. Francis Hospital, Charleston, SC.
The nursing and infection prevention teams at Vanderbilt University Medical Center in Nashville, Tennessee, created a color‐coded system to identify risk levels for various patients and help guide protocols for perioperative treatment. Green indicated regular PPE was warranted; orange indicated a need to wear an N95 respirator for intubation and extubation; and red indicated a patient who had tested positive for COVID‐19, in which case droplet precautions were required, explained Cynthia Kildgore, RN, director of perioperative services.
Before rapid testing was available, anesthesia professionals took precautions for all intubations and extubations. At the time of this writing, the Vanderbilt health care team members have access to rapid turnaround COVID‐19 tests that provide results in approximately two hours. The laboratory personnel can complete 30 tests each day, so surgical patients must undergo testing 48 hours in advance (or 72 hours in advance for patients who live farther than 100 miles from the facility) and then self‐quarantine. Then the perioperative and anesthesia personnel review the surgery schedule the day before the scheduled procedures to verify the test results. They flag some patients for a rapid test before surgery—which, as of early May, was approximately 3% of the scheduled patients per day. “I'm amazed at how fast they put that process together and we were able to pretty much resume normal operational cases,” Kildgore said.
COMMUNICATION
With the rapidly changing protocols and evolving information on COVID‐19 best practices, leaders found great value in effective communication; and the incident command structure helped to facilitate enhanced communication. To share the same information with all health care personnel, nurse leaders and other health care providers used and contributed to various modes of communication, including in‐person and virtual meetings, e‐mail, newsletters, physical information boards, online resources, and smartphone applications.
Regular meetings of the different teams, including the incident command center teams, was a ubiquitous aspect of the pandemic response. Meetings included various groups of personnel—some were for leaders only, some included subteams, and others included all staff members—and often, meetings were interdepartmental. Some meetings occurred in person, but frequently, teams transitioned to online platforms to maintain social distancing. The goal was to share information and provide regular updates on the pandemic response, including new information from entities such as the Centers for Disease Control and Prevention and state departments of health. This information often included positive COVID‐19 test statistics from the international, national, state, and local communities, as well as the current situation at the health care facility.
Resources.
Clayton JL, Miller KJ. Professional and regulatory infection control guidelines: collaboration to promote patient safety. AORN J. 2017;106(3):201‐210.
COVID‐19 (Coronavirus) AORN Tool Kit. AORN. https://www.aorn.org/about-aorn/aorn-newsroom/covid-19-coronavirus. Updated July 1, 2020. Accessed July 24, 2020.
COVID‐19 FAQs. AORN. https://www.aorn.org/guidelines/aorn-support/covid19-faqs [member access only]. Updated April 20, 2020. Accessed May 22, 2020.
Link T. Guideline implementation: transmission‐based precautions. AORN J. 2019;110(6):637‐649.
Re‐entry guidance for health care facilities and medical device representatives. AORN. https://www.aorn.org/guidelines/aorn-support/re-entry-guidance-for-health-care-facilities. Accessed May 22, 2020.
Because COVID‐19 information was changing so quickly, CentraCare stationed multiple representatives, including two physicians and the hospital attorney, in St Paul to serve as subject matter experts to the governor and receive twice‐daily updates from state leaders. They then reported this information to hospital leaders. The goal was “getting that information then down to the staff level,” Asplin said.
Perioperative leaders set up a specific COVID‐19 information board outside the staff member locker rooms to share information in lieu of in‐person huddles. The leaders posted information every day about the effect of COVID‐19 on perioperative services. The clinical resource nurse also condensed the hospital's daily communication to provide updates specific to perioperative services. Another aspect of the response at CentraCare was to allow all staff members to contact the incident command center leaders directly with questions. The leaders answered these questions quickly and provided the most up‐to‐date information.
During daily leadership meetings at OSF SAHC, one focal point was PPE availability. The team created a visual status whiteboard (Figure 5) to keep track of resources and supplies and to help keep all staff members and leaders updated on PPE status.
Figure 5.
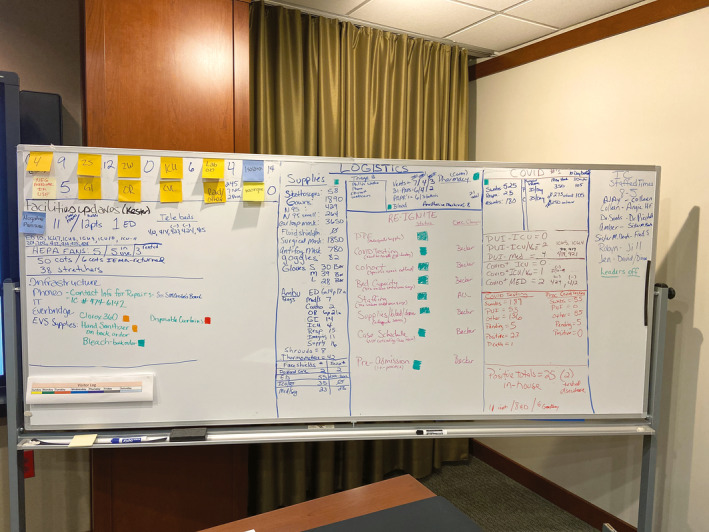
Visual status board for daily monitoring of personal protective equipment. Copyright © 2020, OSF HealthCare Saint Anthony's Health Center, Alton, IL. Photo by Colleen Becker.
Some teams used online tools to help disseminate information. At BIDMC, leaders created a “Coronavirus Central” section in its online portal that included clinical resources, employee resources, and manager resources. The perioperative policy and procedure book in the portal also was updated with a separate COVID‐19 section.
The leadership team at Baylor University Medical Center used Lean principles to create and implement an online dashboard as a communication tool, according to DeFrehn. The dashboard helped leaders monitor various metrics, such as how many patients were in the hospital, how many patients were being tested for COVID‐19, and when tests results were expected, to understand what was going on and facilitate decision making. They also used their facility's smartphone app to communicate with patients and staff members alike. Patients could use the app to obtain their test results. The app also risk‐stratified patients based on their symptoms, so the health care team members could call higher‐risk patients back more quickly and nurse navigators could steer the patient through the system.
Communication—whether it was verbal or written, in‐person or electronic—helped perioperative team members respond to the crisis. By providing the most current information and responding to questions in a timely manner, leaders helped their teams feel confident and be successful in saving patients’ lives. “Communication was extraordinary,” McKoin said. “I think that's the key. Rather than responding to rumors, we were managing the information. If people had a question, they had a place to go and they got their questions answered very quickly, and that was amazing.”
Editor's note: CentraCare is a trademark of CentraCare Health System, St Cloud, MN.
This special report features a collection of tools that leaders from some of the featured facilities implemented in response to the COVID‐19 pandemic. The tools have been left in their original format to preserve authenticity. To access the collection, visit https://www.aorn.org/AORN-Journal/COVID19-Tools.
Biography
Kimberly J. Retzlaff is a freelance writer and editor based in Denver, CO. Ms Retzlaff has no declared affiliation that could be perceived as posing a potential conflict of interest in the publication of this article.


