Abstract
Objective
The current coronavirus disease 2019 (COVID‐19 outbreak) demands an increased need for hospitalizations in emergency departments (EDs) and critical care units. Owing to refractory hypoxemia, prone position ventilation has been used more frequently and patients will need repeated hemodynamic assessments. Our main objective was to show the feasibility of obtaining images to measure multiple parameters with transthoracic echocardiography during the prone position ventilation.
Methods
We enrolled 15 consecutive mechanically ventilated patients with confirmed severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection that required prone position ventilation as a rescue maneuver for refractory hypoxemia. The studies were performed by 2 operators with training in critical care echocardiography. Measurements were done outside the patient's room and the analysis of the images was performed by 3 cardiologists with training in echocardiography.
Results
Adequate image acquisition of the left ventricle was possible in all cases; we were not able to visualize the right ventricular free wall only in 1 patient. The mean tricuspid annular plane systolic excursion was 17.8 mm, tricuspid peak systolic S wave tissue Doppler velocity 11.5 cm/s, and the right ventricular basal diameter 36.6 mm; left ventricle qualitative function was reduced in 6 patients; pericardial effusion or valvular abnormalities were not observed.
Conclusion
We showed that echocardiographic images can be obtained to measure multiple parameters during the prone position ventilation. This technique has special value in situations where there is sudden hemodynamic deterioration and it is not possible to return the patient in the supine position.
Keywords: echocardiography, mechanical ventilation, prone position
1. INTRODUCTION
1.1. Background
Severe coronavirus disease 2019 (COVID‐19) infections require admissions into emergency departments and critical care units, and despite invasive mechanical ventilation they have high mortality rates. 1 , 2 When deep hypoxemia appears there is an increased need of prone position ventilation as a rescue maneuver. 3 In these critically ill patients, it is necessary to perform repeated and adequate cardiac and hemodynamic evaluation because acute instability can appear suddenly during prone position ventilation.
1.2. Importance
Many societies provided their recommendations for conventional echocardiographic evaluation, 4 but there is a lack of information on how to obtain images during the prone position ventilation. Transthoracic echocardiography (TTE) in the supine position is the ideal method; however, in those patients for whom returning to supine position is not feasible, this should not be a limitation to perform an echocardiographic evaluation. Therefore, we propose an echocardiographic technique applied in 15 mechanically ventilated patients in prone position during COVID‐19 pandemic performed in our critical care unit.
1.3. Goals of this investigation
Our objective was to show the feasibility of obtaining echocardiographic images to measure multiple parameters with TTE during the prone position ventilation.
2. METHODS
2.1. Study design and setting
Cross‐sectional study performed in our critical care unit from April 1, 2020 to May 15, 2020.
2.2. Selection of participants
We enrolled 15 consecutive mechanically ventilated patients with confirmed severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection that required prone position ventilation as a rescue maneuver for refractory hypoxemia; none were excluded.
2.3. Interventions
Transthoracic echocardiograms in prone position were performed by 2 critical care specialists with training in critical care echocardiographic image acquisition. The echocardiographic views and parameters were recorded and measured according to the guidelines of the American Society of Echocardiography to perform a comprehensive transthoracic echocardiographic examination in adults and the guidelines of the American Society of Echocardiography and the European Association of Cardiovascular Imaging for cardiac chamber quantification. 5 , 6 The following measures were applied to minimize the exposure of the staff to the infection: (1) all studies were performed during regular patient rounds; (2) the machine and sector probe were sanitized adequately after each evaluation; (3) all physicians had adequate personal protective equipment; (4) image measurements were performed outside the patient's room and (5) analysis and registration of the measurements were performed by other physicians (3 cardiologists with training in echocardiography –EGC, ALMO and RJAA‐); each reviewed the images from the 15 patients.
The Bottom Line
The use of prone positioning during mechanical ventilation has increased during the COVID‐19 pandemic, but it is unknown whether transthoracic echocardiographic views can be obtained in prone patients by physicians trained in point‐of‐care ultrasound. This case series demonstrates that complete apical 4‐ and 5‐chamber views and related measurements were feasible in 14 of 15 prone patients.
2.4. Proposal of echocardiographic technique during the prone position ventilation
Raise the patient's left arm and place a pillow or a folded sheet underneath the mid‐thoracic wall to maintain the left hemithorax slightly elevated for a comfortable transducer manipulation (Figure 1A).
Using a 2–3 mHz phased array sector probe, the operator should obtain the images with the right hand on the right side of the bed (where the left side of the patient lays closer). The probe should be placed in the 5th‐6th intercostal space at mid‐clavicular line (or at the point of maximal apical impulse if palpable), where the conventional apical 4‐chamber view is usually obtained, with the notch pointing to the patient's back (Figure 1B).
Tilting, sliding, and “rocking” the probe helps to optimize image resolution (Figure 1C and 1D). The operator should visualize the same anatomic structures as in a conventional apical 4‐chamber view (Figure 2A). By tilting the transducer in the direction of the patient's abdominal wall, an apical 5‐chamber view can be obtained (Figure 1E and 1F). The apical views in the prone position were obtained in ≈5 minutes.
FIGURE 1.

Performing an echocardiogram on a human model in prone position. See text for explanation of the position and measurements
FIGURE 2.
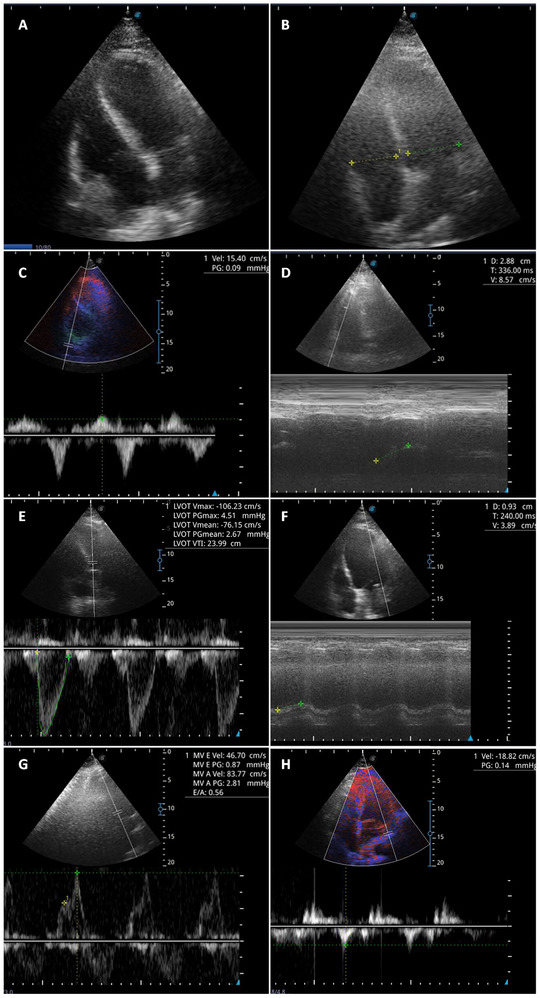
Evaluation of right and left ventricular function in mechanically ventilated patients in prone position. Panel A: Apical 4‐chamber view. Panel B: right ventricle/left ventricle ratio. Panel C: tricuspid peak systolic S wave tissue Doppler velocity (S wave).Panel D: tricuspid annular plane systolic excursion (TAPSE). Panel E: left ventricular outflow tract velocity integral time (LVOT VTI). Panel F: mitral annular plane systolic excursion (MAPSE). Panel G: E velocity of mitral inflow filling pattern. Panel H: lateral e′ velocity
2.5. Measurements
After image acquisition, the following measurements could be obtained in 10 minutes:
Evaluation of right ventricular function: right ventricle (RV) basal diameter and RV/left ventricular (LV) ratio, tricuspid peak systolic S wave tissue Doppler velocity (S wave), and tricuspid annular plane systolic excursion (TAPSE) (Figure 2B, 2C and 2D).
Evaluation of left ventricular function: left ventricular outflow tract velocity time integral (LVOT VTI) (Figure 2E) (and its variation for predicting fluid responsiveness), qualitative LV systolic function; regional wall motion (inferoseptal and anterolateral walls), and mitral annular plane systolic excursion (MAPSE) (Figure 2F).
Evaluation of diastolic function: mitral inflow filling pattern (Figure 2G) and E/e′ ratio (Figure 2H).
Others: abnormal flow patterns at mitral, tricuspid and/or aortic valves with color Doppler and searching for pericardial effusion.
2.6. Outcomes
Feasibility of obtaining echocardiographic images in order to measure parameters with TTE during the prone position ventilation.
2.7. Analysis
We performed a descriptive analysis of the measurements in each patient; in order to know the values of the whole population we reported the mean value in the secondary results section. We assessed the interrater reliability for image interpretation using a kappa coefficient among the 3 interpretations of the categorical echocardiographic variables.
3. RESULTS
3.1. Characteristics of study subjects
In Table 1, demographic characteristics, comorbidities, symptoms at admission, chest X‐ray, oxygenation index, and treatment are shown. The echocardiographic measurements of the 15 patients evaluated with this technique are described in Table 2. Patients are labeled as P1 to P15 in tables.
TABLE 1.
Patients clinical characteristics
| Case | BMI | Age | Comorbidities | Presenting symptoms | Chest X‐ray | paFiO2 | IOT‐ Prono time | Treatment |
|---|---|---|---|---|---|---|---|---|
| 1 | 29.1 | 39 | Overweight | Diarrhea, fever, dry cough, and dyspnea | Bilateral ground‐glass opacification | 67 | 24h | Lung protective and prone position ventilation vasopressors, steroids, broad‐spectrum antibiotics, antiviral and anticoagulation. |
| 2 | 28.3 | 66 | Overweight and type 2 diabetes | Arthralgias, fever and dyspnea | Cardiomegaly and patchy peripheral left mid to lower lung opacities | 80 | 24h | Lung protective and prone position ventilation, antiviral and anticoagulation |
| 3 | 24.5 | 56 | Smoking | Odynophagia and dyspnea | Diffuse interstitial involvement, predominantly peripheral | 111 | 72h | Lung protective and prone position ventilation, antiviral, systemic steroids, and anticoagulation |
| 4 | 33.1 | 50 | Obesity | Odynophagia, fever, and dyspnea | Severe interstitial thickening at lower lobes | 91 | 48h | Lung protective and prone position ventilation, lopinavir/ritonavir, systemic steroids, and anticoagulation |
| 5 | 32.4 | 63 | Overweight, gout, and dyslipidemia | Dry cough, odynophagia fever, and dyspnea | Ground‐glass opacification at lung bases | 93 | 12h | Lung protective and prone position ventilation, hydroxychloroquine, azithromycin, anticoagulation, steroids, and hemodialysis |
| 6 | 35.1 | 64 | Obesity | Arthralgias, odynophagia, fever, and dyspnea | Severe peripheral interstitial involvementpredominantlyat lower lobes | 52 | 6h | Lung protective and prone position ventilation, systemic steroids, and hemodialysis |
| 7 | 24.9 | 64 | Type 2 diabetes and hypertension | Lipothymy, AV block, and fever | Peripheralbilateral ground‐glass opacification | 76 | 72h | Lung protective and prone position ventilation, antiviral, systemic steroids, and anticoagulation |
| 8 | 31.1 | 79 | Obesity, type 2 diabetes, and hypertension | Arthralgia, odynophagia, fever, and dyspnea | Diffuse interstitial involvement, predominantly peripheral | 111 | 48h | Lung protective and prone position ventilation, antiviral, systemic steroids, and anticoagulation |
| 9 | 36.3 | 50 | Obesity, hypertension, hyperuricemia, gout, and dyslipidemia | Odynophagia fever and dyspnea severe | Diffuse ground glass opacities predominantly at lung bases | 96 | 5 days | Lung protective and prone position ventilation, systemic steroids, and hemodialysis |
| 10 | 24.4 | 71 | Hypertension, dyslipidemia, and ischemic heart disease | Dry cough, fever, and dyspnea | Cardiomegaly and bilateral ground‐glass opacification | 53 | 72h | Lung protective and prone position ventilation, antiviral and anticoagulation |
| 11 | 23.6 | 70 | Type 2 diabetes | Dry cough, fever, and dyspnea | Peripheral interstitial involvement and right basal consolidation | 85 | 12h | Lung protective and prone position ventilation, hydroxychloroquine, azithromycin, and anticoagulation |
| 12 | 30.2 | 52 | Obesity | Dry cough, fever, and dyspnea | Severe interstitial involvement predominantly in lung bases | 65 | 8h | Lung protective and prone position ventilation, antiviral, and anticoagulation |
| 13 | 22.9 | 66 | Type 2 diabetes | Asthenia, fever, and dyspnea | Severe interstitial involvement predominantly peripheral | 79 | 48h | Lung protective and prone position ventilation, systemic steroids, antiviral, and anticoagulation |
| 14 | 24.1 | 69 | Alcoholism | Dry cough, fever, and dyspnea | Diffuse interstitial involvement | 66 | 12h | Lung protective and prone position ventilation, antiviral, and anticoagulation |
| 15 | 34.4 | 57 | Obesity | Productive cough, fever, and dyspnea | Bilateral diffuse ground‐glass opacities | 100 | 4h | Lung protective and prone position ventilation, antiviral, and anticoagulation |
TABLE 2.
Echocardiographic measurements during the prone position ventilation
| Patient (P) | TAPSE | S′ wave | RV basal diameter | RV/LV ratio | LVOT VTI | LVOT VTI variability | LVF | E/e´ | MAPSE | PE |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 21 | 13 | 41 | 0.8 | 17 | NO | N | 11 | 14 | NO |
| 2 | 23 | 13 | 40 | 0.7 | 15 | YES | MR | 5 | 12 | NO |
| 3 | NA | NA | NA | NA | 23 | NO | MR | 5 | 11 | NO |
| 4 | 18 | 14 | 38 | 0.7 | 23 | NO | N | 10 | 18 | NO |
| 5 | 18 | 13 | 40 | 0.8 | 16 | NO | N | 8 | 13 | NO |
| 6 | 23 | 11 | 41 | 0.9 | 25 | YES | N | 9 | 17 | NO |
| 7 | 19 | 15 | 43 | 0.9 | 18 | NO | MR | 12 | 11 | NO |
| 8 | 27 | 19 | 39 | 0.8 | 19 | NO | N | 8 | 15 | NO |
| 9 | 22 | 11 | 35 | 0.85 | 17 | NO | N | 13 | 13.5 | NO |
| 10 | 14 | 9 | 37 | 0.8 | 13 | NO | MR | 15 | 9 | NO |
| 11 | 13 | 8 | 35 | 0.7 | 13 | YES | MR | 16 | 9 | NO |
| 12 | 16 | 11 | 39 | 0.8 | 17 | NO | N | 10 | 14 | NO |
| 13 | 18 | 9 | 43 | 0.9 | 14 | NO | MR | 10 | 10 | NO |
| 14 | 18 | 14 | 39 | 0.8 | 15 | YES | N | 5 | 15 | NO |
| 15 | 17 | 13 | 40 | 0.9 | 15 | NO | N | 8 | 13 | NO |
LV, left ventricular; LVF, left ventricular qualitative systolic function; LVOT, left ventricular outflow tract; MAPSE, mitral annular plane systolic excursion; MR, moderately reduced); N, normal; NA, not available; PE, pericardial effusion; RV, right ventricular; S wave, tricuspid peak systolic S wave tissue Doppler velocity; TAPSE, tricuspid annular plane systolic excursion; VTI, velocity‐time integral.
Normal values: TAPSE ≥17 mm, S wave ≥9.5 cm/s, RV basal diameter <42 mm, RV/LV ratio <1, LVOT VTI 18–22 cm, LVOT VTI variability ≥ 12%, MAPSE ≥13 mm.
3.2. Main results
An adequate evaluation of LV function, diastolic function, valves (mitral, tricuspid, and aortic), and pericardium was possible in 14 of 15 patients. In 1 patient, the RV free wall was unable to be assessed.
3.3. Secondary results
The mean TAPSE was 17.8 mm, the RV S wave 11.5 cm/s, and RV basal diameter 36.6 mm. RV/LV ratio was <1 in all patients. Four patients had LV VTI variability, which suggested fluid responsiveness. There was a moderate decrease in LV qualitative function in 6 patients that correlated with a low MAPSE (<13 mm). Pericardial effusion or valvular abnormalities were not observed in any patient. Using a kappa‐coefficient, agreement between raters was >0.8 for all categorical measurements.
4. LIMITATIONS
There are some limitations that should be considered in the interpretation of our results. We have to mention that we included consecutive patients with no other selection criteria other than IMV in prone position; therefore, there can be a selection bias. Also in the apical view, the inferior vena cava cannot be evaluated. Finally, this is a preliminary report of the application of a novel technique and it should be validated in other centers.
5. DISCUSSION
Critical care echocardiography has rapidly evolved as the election technique in the evaluation of the critically ill patients during the COVID‐19 pandemic. These patients have deep hypoxemia and when it cannot be reversed with conventional maneuvers, rescue therapies must be implemented, particularly prone position ventilation, which is indicated when the paO2/FiO2 ratio is lower than 150 after positive end‐expiratory pressure (PEEP) titration. This technique produces an improvement in oxygenation by increasing the ventilation/perfusion ratio in the dependent lung regions. 7 This is particularly relevant because acute respiratory distress syndrome (ARDS) is a major complication of COVID‐19 that occurs in 20%–41% of patients with severe disease. 8 Prone position ventilation is the mainstay of treatment in COVID‐19‐related ARDS and has been recommended in the Surviving Sepsis Campaign COVID‐19 guidelines. 9 This strategy has been used in as many as 27% of ventilated patients, 10 although before the pandemic, it was used in just 8% of patients with ARDS. 11
In our study, we were able to perform TTE in mechanically ventilated patients in prone position without technical difficulties. There are anecdotic reports of TTE 12 and a more extensive experience in transesophageal echocardiography during prone position ventilation, 13 but there is no standardization in the technique for image acquisition and measurements. Santos et al showed an adequate correlation of the RV measurements in prone compared with the supine position in 50 individuals; however, in this study, the evaluation was in healthy patients, not mechanically ventilated, 14 and the performance of critical care echocardiography in patients under IMV has unique challenges because the positive pressure caused by the pulmonary insuflation limits the acoustic window.
We demonstrated the feasibility to obtain an apical 4‐chamber and 5‐chamber views to measure multiple echocardiographic parameters with TTE to perform a qualitative and quantitative evaluation in patients with IMV and prone positioning. During prone position ventilation the patient can develop sudden hemodynamic instability without the possibility to return the patient to the supine position because of the risk to develop refractory hypoxemia, therefore highlighting the need to perform the TTE in prone position. A larger series will be required to assess its correlation with the usual measurements in supine position and its impact in clinical decisionmaking and outcomes. This evaluation can help the physician make a better assessment of the heart‐lung interactions during IMV and this could help to improve patient's outcomes.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Edgar García‐Cruz and Daniel Manzur‐Sandoval: Original idea, methodology, image acquisition, analysis, and writing the original draft, review and editing. Rodrigo Gopar‐Nieto, Adriana L. Murillo‐Ochoa, Gabriela Bejarano‐Alva, Gustavo Rojas‐Velasco, Rolando J. Álvarez‐Álvarez, and Francisco Baranda‐Tovar: Analysis and writing (final draft, review and editing).
ACKNOWLEDGMENT
We thank the INC Critical Care Ultrasonography Working Group.
Biography
Daniel Manzur‐Sandoval, MD, is an attending physician at the Instituto Nacional de Cardiologia Ignacio Chávez, Cardiovascular Critical Care Unit, Mexico City, Mexico.

García‐Cruz E, Manzur‐Sandoval D, Gopar‐Nieto R, et al. Transthoracic echocardiography during prone position ventilation: Lessons from the COVID‐19 pandemic. JACEP Open. 2020;1:730–736. 10.1002/emp2.12239
Grants: This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Nicholas Johnson, MD.
REFERENCES
- 1. Richardson S, Hirsch J, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York city area. JAMA. 2020;323:2052‐2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. Covid‐19 does not lead to a “Typical” acute respiratory distress syndrome. Am J Respir Crit. 2020;201:1299‐1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kirkpatrick JN, Mitchell C, Taub C, Kort S, Hung J, Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak: endorsed by the American College of Cardiology. J Am Soc Echocardiogr. 2020;33(6):648‐653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2019;32:1‐64. [DOI] [PubMed] [Google Scholar]
- 6. Lang RM, Badano LP, Mor‐Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:412. [DOI] [PubMed] [Google Scholar]
- 7. Gattinoni L, Taccone P, Carlesso E, Marini J. Prone position in acute respiratory distress syndrome. rationale, indications, and limits. Am J Respir Crit Care Med. 2013;188(11):1286‐1293. [DOI] [PubMed] [Google Scholar]
- 8. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China JAMA Intern Med. 2020;180(7):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID‐19). Crit Care Med. 2020;48(6):e440‐e469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS‐CoV‐2 admitted to ICUs of the lombardy region, Italy. JAMA. 2020;323(16):1574‐1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788‐800. [DOI] [PubMed] [Google Scholar]
- 12. Ugalde D, Medel J, Romero C, Cornejo R. Transthoracic cardiac ultrasound in prone position: a technique variation description. Intensive Care Med. 2018;44(6):986‐987. [DOI] [PubMed] [Google Scholar]
- 13. Mekontso Dessap A, Proost O, Boissier F, Louis B, Roche Campo F, Brochard L. Transesophageal echocardiography in prone position during severe acute respiratory distress syndrome. Intensive Care Med. 2011;37(3):430‐434. [DOI] [PubMed] [Google Scholar]
- 14. Santos‐Martínez LE, Mendoza‐Copa G, García‐Cruz E, et al. Feasibility in the echocardiographic estimation parameters of the right ventricle in prone position. Arch Cardiol Mex. 2020;90(2):130‐137. [DOI] [PubMed] [Google Scholar]


