Abstract
Background
Longevity as a phenotype entails living longer than average and typically includes living without chronic age-related diseases. Recently, several common genetic components to longevity have been identified. This study aims to identify additional genetic variants associated with longevity using unique and powerful analyses of pedigrees with a statistical excess of healthy elderly individuals identified in the Utah Population Database (UPDB).
Methods
From an existing biorepository of Utah pedigrees, six independent cousin pairs were selected from four extended pedigrees that exhibited an excess of healthy elderly individuals; whole exome sequencing (WES) was performed on two elderly individuals from each pedigree who were either first cousins or first cousins once removed. Rare (<0.01 population frequency) variants shared by at least one elderly cousin pair in a region likely to be identical by descent were identified as candidates. Ingenuity Variant Analysis was used to prioritize putative causal variants based on quality control, frequency, and gain or loss of function. The variant frequency was compared in healthy cohorts and in an Alzheimer’s disease cohort. Remaining variants were filtered based on their presence in genes reported to have an effect on the aging process, aging of cells, or the longevity process. Validation of these candidate variants included tests of segregation on other elderly relatives.
Results
Fifteen rare candidate genetic variants spanning 17 genes shared within cousins were identified as having passed prioritization criteria. Of those variants, six were present in genes that are known or predicted to affect the aging process: rs78408340 (PAM), rs112892337 (ZFAT), rs61737629 (ESPL1), rs141903485 (CEBPE), rs144369314 (UTP4), and rs61753103 (NUP88 and RABEP1). ESPL1 rs61737629 and CEBPE rs141903485 show additional evidence of segregation with longevity in expanded pedigree analyses (p-values=0.001 and 0.0001, respectively).
Discussion
This unique pedigree analysis efficiently identified several novel rare candidate variants that may affect the aging process and added support to seven genes that likely contribute to longevity. Further analyses showed evidence for segregation for two rare variants, ESPL1 rs61737629 and CEBPE rs141903485, in the original longevity pedigrees in which they were initially observed. These candidate genes and variants warrant further investigation.
Keywords: Longevity, Genomics, Pedigree, Utah Population Database, rare variant sharing
INTRODUCTION
Aging is a major risk factor for various chronic diseases (Franceschi et al., 2018), but can also be considered as a phenotype (e.g. healthy aging with no chronic disease or exceptional longevity) (Lara et al., 2013). Genome-wide association studies have identified factors associated with longevity (Deelen et al., 2019; Pilling et al., 2017; Sebastiani et al., 2017). Genome-wide association studies identify associations between genotypes and phenotypes by testing individual genetic variants across a genome (Tam et al., 2019). However, they often lack sufficient power to identify rare variants because small effect sizes are diluted across thousands of individuals (Maher, 2008).
Pedigree-based analyses provide additional power to identify rare variants because they control for parent-of-origin effects, population stratification, and other hidden effects (Ott et al., 2011). Atzmon et al. (2006) capitalized on familial relationships in a case-control analysis of Ashkenazi Jews to identify variants specific to longevity. This study included 213 cases defined as individuals 95–107 years old living independently and in good health, and participants were required to have a child participate in the study. The offspring group, which was used to increase sample size and perform additional analyses, consisted of 216 individuals. An age-matched Ashkenazi control group consisted of 258 individuals This study suggested that pathways involved in lipoprotein metabolism appear to influence longevity in humans.
An additional study on longevity was conducted as part of the Hawaii Lifespan Study, and included healthy elderly individuals from the original population of the Honolulu Heart Program and Honolulu Asia Aging Study (Willcox et al., 2008). The Honolulu Heart Program is a population-based, prospective study that began in 1965 by studying cardiovascular disease among 8,006 Japanese American men. This study contained 213 cases who survived to at least 95 years of age. The mean age of death for the 402 control individuals in the Honolulu Asia Aging Study and the Hawaii Lifespan Study who died near the mean death age for the 1910 U.S. birth cohort was 78.5 years of age. This study identified common, natural genetic variation strongly associated with longevity in the FOXO3A gene.
The Long Life Family study also contains a multi-center family-based cohort that was used to identify genetic components of longevity. This study demonstrated the use of sequencing within pedigrees to identify 24 inherited rare variants in two long-lived families influencing healthy aging (Druley et al., 2016).
The Utah Population Database (UPDB) includes extensive sets of demographic and medical records for more than 11 million individuals, three million of whom are linked to Utah genealogy data (Cannon-Albright, 2008). From an existing collection of stored DNA for Utah individuals identified in the UPDB over many decades, clusters of related sampled healthy elderly individuals (age at death greater than 90 years) that exhibited a statistical excess of individuals who died at an age older than 90 years (high-risk pedigrees) were identified. Six sampled elderly cousin pairs selected from four of these extended pedigrees were sequenced. Putative causal variants were identified using an efficient and powerful analytical approach previously used to identify rare variants that influence risk and resilience to Alzheimer’s disease (Patel et al., 2019; Ridge et al., 2017), melanoma (Teerlink et al., 2018), Osteoporosis (Teerlink et al., 2020), and colorectal cancer (Thompson et al., 2020) in UPDB pedigrees.
MATERIALS AND METHODS
Data
Utah Population Database (UPDB)
The UPDB includes population-based resources linking demographic and health data to the genealogical records of the 19th century founders of Utah and their descendants to modern day (Cannon-Albright, 2008). The multigenerational pedigrees represented in UPDB were constructed from data provided by the Genealogical Society of Utah and have been expanded extensively based on Utah State vital records. There are currently over 11 million individuals included in the database, including approximately three million people with at least three generations of family history connected to the original Utah settlers. Age at death was calculated from death dates provided in genealogy records and from over 900,000 death certificates linked to the UPDB genealogy.
Longevity Pedigrees
Among a collection of approximately 36,000 individuals from the UPDB for whom stored DNA samples exist from high-risk disease pedigree studies performed over many decades we identified all healthy elderly individuals (sampled for research at age greater than 90 years; n=214). These 214 sampled healthy elderly individuals were related in 25 independent descending pedigrees among whose descendants there was a statistical excess of individuals dying at an age older than 90 years. Four of these sampled high-risk pedigrees that also included at least one sampled healthy elderly cousin pair were selected for analysis; a sampled cousin pair was selected from each for sequencing. One selected member of a cousin pair was a member of two independent pedigrees, through different ancestors, so an additional sampled case (cousin) from one pedigree was also included for a total of eight individuals sequenced. Figure S1 depicts the six independent pedigrees consisting of eight sequenced individuals. For the purpose of identifying shared variants, each of the six cousin pairs with sequence data was analyzed. All samples had proper consent and all data collection and analysis was approved by the University of Utah Institutional Review Board.
Alzheimer’s Disease Genetic Consortium
Additional filtering and validating of variants was conducted using the Alzheimer’s Disease Genetic Consortium (ADGC) datasets compiled by Naj et al. (2011). ADGC is a collection of 30 merged datasets spanning 1984 to 2012, and was established to help identify genetic markers of late-onset Alzheimer’s disease (Boehme et al., September 2014). ADGC contains imputed SNP array data for 28,730 subjects (58.34% female), including 13,042 Alzheimer’s disease cases and 13,410 healthy controls. ADGC imputed the 30 datasets to the Haplotype Reference Consortium (HRC) reference panel, which includes 64,976 haplotypes and 39,235,157 SNPs (Loh et al., 2016; Naj et al., 2017). Genotyped markers with a minor allele frequency less than 0.01 and markers that deviated from Hardy Weinberg Equilibrium were removed. All aspects of the study were approved by institutional review boards, and each applicant signed a written form of consent for their genetic data to be used for research purposes.
The Wellderly Study
The Wellderly Study, an ongoing Scripps Translational Science Institute research project, includes more than 1,400 individuals over the age of 80 with no chronic disease or chronic use of medication (Erikson et al., 2016). The purpose of this study was to determine whether genetic factors underlie the phenotype of exceptional longevity. Researchers performed whole genome sequencing on 511 Wellderly participants and compared their results to whole genome sequencing data from 686 young adults from the Inova Translational Medicine Institute (ITMI), which served as an ethnicity-matched control group that simulated the general population (Bodian et al., 2014).
Wellderly individuals had significantly reduced genetic risk for coronary artery disease (p-value=2.54 × 10−3) and Alzheimer’s disease (p-value=9.84 × 10−4), although there was no decrease in the number of identified rare pathogenic variants. These findings suggest the presence of other disease-resistant factors (e.g., protective rare variants) within this longevity cohort to overcome the deleterious effects of these pathogenic variants.
Bioinformatic Analysis
Whole exome sequencing for the eight elderly individuals selected as cousin pairs was performed at the Huntsman Cancer Institute’s Genomics Core facility. A DNA library was prepared from 2μg of DNA per sample using the Agilent SureSelect XT Human All Exon + UTR (v5) capture kit. Samples were run on the Illumina HiSeq 2000 sequencer that generates paired-end reads of up to 150 base pairs in length. Raw reads were mapped to the human genome v37 (GRCh37) reference genome using BWA-MEM (Li, 2013; Li and Durbin, 2009). Variants were called using Genome Analysis Toolkit 3.5.0 (GATK) (McKenna et al., 2010) software following Broad Institute Best Practices Guidelines. Variants occurring outside the exon capture kit intended area of coverage were removed. Variants were annotated with ANNOVAR (Wang et al., 2010). Candidate variants were filtered on the criteria of being rare in population (minor allele frequency less than 0.01) and shared by a cousin pair.
Genetic Support for Pedigree Enrichment
In order to evaluate the effectiveness of pedigree enrichment for longevity, a polygenic risk score analysis was conducted for each of the eight individuals in the dataset. A polygenic risk score calculates the cumulative risk for a certain phenotype determined from aggregating the effect sizes of multiple genetic loci (Sugrue and Desikan, 2019). The polygenic risk score was calculated from the following equation, where ai is the number of alleles at the ith locus, ri is the odds ratio at the ith locus, and p is the p-value of the odds ratio:
For each sample, the polygenic risk score for Alzheimer’s disease was calculated using the odds ratios from Lambert et al. (2013), coronary artery disease using the odds ratios from Schunkert et al. (2011), and heart failure using the odds ratios from Shah et al. (2020). The same genome-wide association studies were used to calculate polygenic risk scores for each individual in the ADGC controls.
Segregation Validation using Rare Variant Sharing
Candidate variants were assayed with TaqMan in a set of 196 sampled individuals who consented and were sampled after 90 years of age, as well as in 11 additional longevity samples (individuals consented and sampled after age 85 years) who were members of the pedigree in which both of the variants were originally observed. The RVsharing program (Bureau et al., 2014) was used to statistically assess segregation of candidate rare variants in other sampled affected relatives. RVsharing calculates the probability of seeing rare variants in the observed pattern of carriage for a specified pedigree structure based on a relatedness matrix between cases, based on genealogy data. A p-value threshold of 0.05 effectively discriminates between rare variants that segregate (Teerlink et al., 2016).
RESULTS
Whole exome sequencing data was generated for the six elderly cousin pairs with a statistical excess of long-lived individuals in their pedigrees. Using UPDB pedigrees to identify candidate predisposition variants for a phenotype of interest allows efficient generation of the set of rare variants that are shared in related (typically cousin) pairs of individuals with the phenotype of interest who are also members of pedigrees that have been established to be at “high-risk” for the phenotype. Since the affected cousin pairs are members of the same high-risk pedigree, they are hypothesized to share the predisposition variant of interest. The set of rare variants shared in any of the cousin pairs from the high-risk pedigrees therefore constitute likely candidate predisposition variants. Using a small set of six independent cousin pairs from four extended “high-risk longevity” pedigrees, 83 rare variants with a minor allele frequency less than 0.01 in the general population that were shared within at least one cousin pair were efficiently identified.
Polygenic Risk Score Analysis
Figure 1 displays the distribution of polygenic risk scores for Alzheimer’s disease, coronary artery disease, and heart failure in the longevity dataset (n=8) against the distribution of risk scores for ADGC controls (n=13,410). Although the first cousins and first cousins once removed are related, on average they are expected to share a relatively low proportion of their genomic variants (12.5% for first cousins and 6.25% for first cousins once removed), which allows most common variants used in calculating polygenic risk scores to maintain the same degree of independence between cousins as between unrelated individuals. In all but one instance, the most similar polygenic risk score for an individual in the dataset for any of the three tested diseases was not with their cousin, but with a different unrelated individual in the dataset. Therefore, a Welch’s two-sample t-test was performed to reveal a significant difference between the mean scores of the longevity cousin pairs and the ADGC controls for coronary artery disease (t=−30.192; p-value = 7.35×10−9) and heart failure (t=−21.746; p-value = 9.78 × 10−8). No significant difference in mean Alzheimer’s disease scores between the longevity cousin pairs and the ADGC controls was revealed (t=−1.139; p-value=0.292. These analyses indicate that the cousin pairs have fewer common variants that contribute to common heart-related diseases in elderly individuals than the ADGC control group, suggesting that the pedigree identification effectively selected families enriched with exceptional longevity that might be attributed to decreased risk for coronary artery disease and heart failure. Supplemental Table S1 outlines the polygenic risk scores for each individual in the dataset, including the prioritized variants present in each person. A similar analysis was conducted on the ADGC Alzheimer’s disease cases, and Figure S2 shows that significant differences in polygenic risk scores for coronary artery disease, heart failure, and Alzheimer’s disease exist between the cousin pairs and a cohort with Alzheimer’s disease.
Figure 1:
Polygenic Risk Scores for UPDB cousins. The distribution of risk scores for the longevity cousins are plotted against the polygenic risk score distribution of the ADGC controls. The density distribution shows the likelihood of observing the values given the continuous distribution of polygenic risk scores (y-axis). The asterisk (*) shows significant differences (p-value<0.05) between the population means calculated from a Welch’s two-sample t-test.
Variant Prioritization
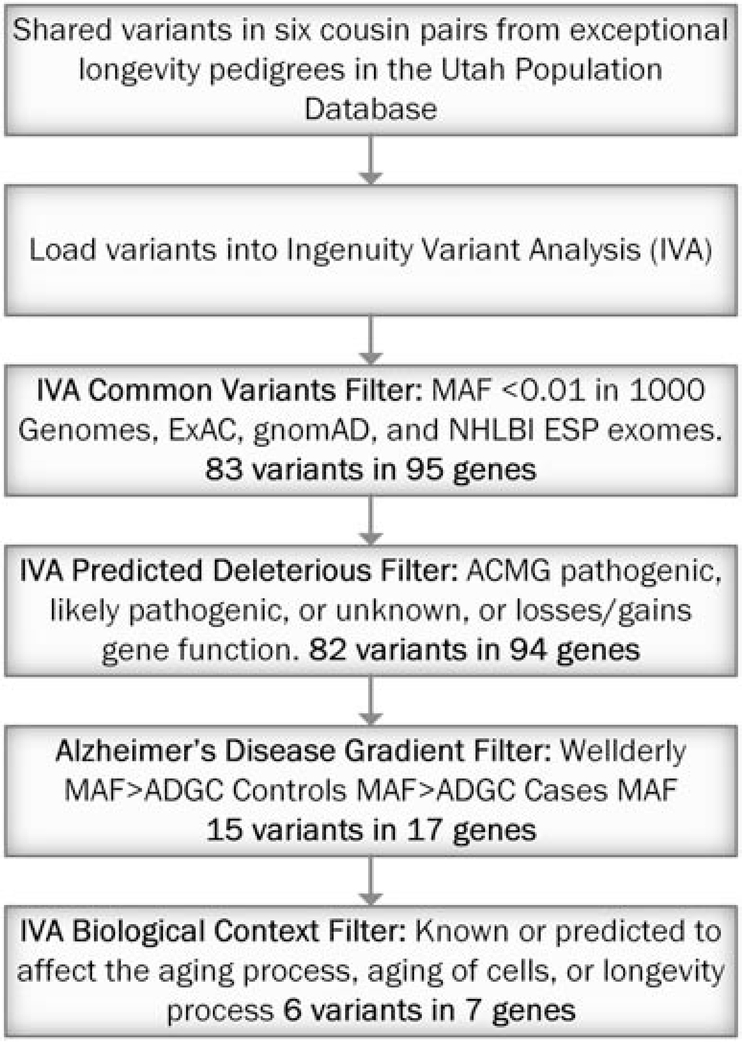
A rare variant analysis was performed on the cousin pairs by first limiting selection to variants that were shared by at least one cousin pair. A Common Variants Filter in Ingenuity® Variant Analysis™ software from QIAGEN, Inc. was used to remove all variants with a minor allele frequency greater than 0.01 in 1000 Genomes (Auton et al., 2015), Exome Aggregation Consortium (ExAC) (Karczewski et al., 2017), The Genome Aggregation Database (gnomAD) (Karczewski et al., 2019), or the NHLBI GO Exome Sequencing Project (ESP), Seattle, WA (URL: http://evs.gs.washington.edu/EVS/) [March 2018]. Text S1 describes these datasets in more detail. This step identified 83 rare candidate variants spanning 95 genes, including 12 variants that each affect two genes. A series of filtration methods on these 83 variants using Ingenuity Variant Analysis was used to prioritize a candidate list of variants associated with longevity (see Figure 2). Variants remaining after each filter are listed in File S1.
Figure 2:
Pipeline for Rare Variant Analysis in Cousin Pairs. Flowchart explaining the filters that we used on our dataset, including the number of variants and genes that passed each filter.
Predicted Deleterious Filter
After the Common Variants Filter, the Predicted Deleterious Filter in Ingenuity Variant Analysis was applied to select variants that were associated with the loss or gain of gene function or were considered ‘Pathogenic’, ‘Likely Pathogenic’, or ‘Unknown’ according to the American College of Medical Genetics and Genomics (ACMG) Guidelines for variant classification (Richards et al., 2015). This analysis excluded only one variant, rs140824939 in SPG11, refining the list to 82 variants spanning 94 genes.
Alzheimer’s Disease Risk Gradient Filter
The purpose of this filter was to identify rare variants that are present more frequently in healthy cohorts than diseased cohorts, since it is expected that protective rare variants that positively impact longevity will not be present as frequently in diseased cohorts. Each variant was compared to the Wellderly dataset and the ADGC dataset to ensure that variants followed expected population allele frequencies based on the number of healthy individuals in each elderly cohort. For this filter, the minor allele frequency of each rare variant was required to be higher in the Wellderly cohort than the ADGC control group, and have a higher minor allele frequency in the ADGC control group than the ADGC Alzheimer’s disease cases. Although rare genotypes (minor allele frequency < 0.01) were previously removed from ADGC for quality control, which may artificially limit the number of prioritized rare variants impacting longevity, genetic variants that passed this filter indicate a higher variant occurrence in healthy individuals than diseased individuals and are the most likely to directly affect longevity. Fifteen variants spanning 17 genes passed this filter.
Biological Context Filter
The final filter evaluated the biological function of each of the 15 remaining variants. This filter included only variants in genes that were known or predicted to affect the aging process, aging of cells, or the longevity process. This filter prioritized six variants spanning seven genes. Recognizing that the biological context filter depends on an accurate understanding of the biological functions of each of the 17 genes that passed the Alzheimer’s Disease Risk Gradient Filter, it is possible that all 15 candidate variants that passed the Alzheimer’s Disease Risk Gradient Filter also positively affect longevity. However, the following six variants that passed the Biological Context Filter are the most supported candidate variants: rs78408340 (PAM), rs112892337 (ZFAT), rs61737629 (ESPL1), rs141903485 (CEBPE), rs144369314 (UTP4), and rs61753103 (NUP88 and RABEP1).
Rare Variant Segregation Analysis
Two rare variants passing all filters were also pursued with segregation analysis. ESPL1 rs61737629 was selected because it was the only variant to be observed in more than one cousin pair, and CEBPE rs141903485 was selected because it has a regulomeDB score of 2b, which indicates that this variant is likely to affect the binding of transcription factors. These two variants were assayed in 196 additional healthy elderly individuals (sampled after age 90 years) from the UPDB-linked sample collection and in 11 additional longevity samples in the pedigree in which both of the variants were originally observed and in 175 sampled Alzheimer’s disease cases (confirmed by Utah death certificate) from the UPDB. ESPL1 rs61737629 was observed in four additional longevity cases. CEBPE rs141903485 was observed in seven additional longevity cases and three Alzheimer’s disease cases. Analyses of individuals sampled after age 85 years in the original longevity pedigree in which both variants were identified also identified two additional carrier of ESPL1 rs61737629 and three additional carriers of CEBPE rs141903485. The Rare Variant Sharing test for ESPL1 rs61737629 (p-value = 0.001) and CEBPE rs141903485 (p-value = 0.0001) reveal that there is a low probability of these variants being shared within healthy elderly individuals in this pedigree by random chance. The constellation of variant carriers of ESPL1 rs61737629 and CEBPE rs141903485 within this extended pedigree was used to calculate the Rare Variant Sharing value for each variant and provides statistical evidence that ESPL1 rs61737629 and CEBPE rs141903485 segregate significantly with longevity.
DISCUSSION
Prioritized Variants
Familial relationships and previously sampled individuals ascertained in the UPDB were leveraged to identify rare candidate variants that influence exceptional longevity. The rare variant analysis pipeline identified six candidate variants located in seven genes that demonstrate a convincing case for association with longevity (see Table 1).
Table 1:
Final Six Prioritized Variants associated with Longevity from the Six Cousin Pairs.
| Chromosome | Position in GRCh37 | Reference | Alternate | Accession Number | Gene Name | SIFT Function Prediction | Translation Impact |
|---|---|---|---|---|---|---|---|
| 5 | 102338739 | C | G | rs78408340 | PAM | Damaging | missense |
| 8 | 135614553 | G | C | rs112892337 | ZFAT | Damaging | missense |
| 12 | 53682043 | C | G | rs61737629 | ESPL1 | Damaging | missense |
| 14 | 23587838 | G | T | rs141903485 | CEBPE | Damaging | missense |
| 16 | 69170741 | G | T | rs144369314 | UTP4 | Tolerated | missense |
| 17 | 5289554 | T | C | rs61753103 | NUP88, RABEP1 | Tolerated | missense |
This table shows the results of the final Ingenuity Variant Analysis Biological Context Filter.
Missense mutation rs78408340 in the PAM gene was identified to have potential association with longevity and is categorized by SIFT (Sim et al., 2012) as ‘Damaging.’ PAM protein catalyzes the conversion of neuroendocrine peptides to active alpha-amidated products. Variants associated with type-2 diabetes in PAM, including rs78408340, reduce the gene’s function, which alters the amidation of peptides critical for insulin secretion. Therefore, rs78408340, along with other alleles in PAM, confers higher risk for type-2 diabetes (Fuchsberger et al., 2016; Steinthorsdottir et al., 2014). One cousin pair shared the variant PAM rs78408340, which may account for these individuals’ shared phenotype.
The individuals in the same cousin pair are also carriers of the variant rs112892337 in the ZFAT gene, which is also labelled by SIFT as ‘Damaging.’ Little is known about the function of this specific allele. However, ZFAT is expressed in B and T lymphocytes and has shown to be a critical transcription regulator involved in apoptosis and cell survival (Fujimoto et al., 2009). Bourguiba-Hachemi et al. (2016) found that another variant, rs733254, in ZFAT is a risk marker for multiple sclerosis (MS) in women. Multiple studies have also detected an association between ZFAT and the severity of autoimmune thyroid disease (Inoue et al., 2012; Sakai et al., 2001).
Missense mutation rs61737629 in ESPL1 was prioritized by the filtration pipeline and shared by two cousin pairs. SIFT also predicts this variant to be ‘Damaging.’ ESPL1, which encodes separase, initiates the final separation of sister chromatids before anaphase by cleaving the subunit SCC1. Disruption of the separase function leads to chromosomal instability, and increasing or reducing the expression of this gene results in severe medical consequences (Gurvits et al., 2017; Mukherjee et al., 2011) including luminal cancers (Finetti et al., 2014). Currently, the behavior of ESPL1 rs61737629 is unknown. This study may lend additional support to luminal cancer studies exploring this variant for its protective benefits because breast cancer can cause death before patients attain the exceptional longevity criteria to be included in this study.
Three individuals, representing two independent cousin pairs, shared CEBPE rs141903485, a missense variant labelled as ‘Damaging’ by SIFT. CEBPE encodes a bZIP transcription factor and plays a role in gene regulation in myeloid and lymphoid lineages (Antonson et al., 1996). The loss of CEBPE function influences the pathogenesis of myeloid disorders, including acute myeloid leukemia (Truong et al., 2003) and pediatric B-cell acute lymphoblastic leukemia (Gharbi et al., 2016; Studd et al., 2019; Sun et al., 2015; Wang et al., 2015). The variant rs141903485 is associated with pediatric B-cell acute lymphoblastic leukemia susceptibility (Xu et al., 2013; Xu et al., 2015).
The missense variant rs144369314 located in UTP4 was shared by one cousin pair. UTP4 encodes a WD40-repeat-containing protein that is localized to the nucleolus. Variation in UTP4 is significantly associated with North American Indian childhood cirrhosis (Freed and Baserga, 2010; Yu et al., 2005).
Individuals in one cousin pair carry the missense mutation rs61753103 in the gene NUP88. NUP88 regulates the flow of macromolecules between the nucleus and the cytoplasm, is overexpressed in malignancies, and is considered a putative marker for tumor growth (Hashizume et al., 2010; Lang et al., 2017; Martinez et al., 1999). Increased expression of this gene is associated with tumor aggressiveness in uterine and breast cancer (Agudo et al., 2004; Schneider et al., 2010) and higher risk for colorectal cancer (Zhao et al., 2012).
This same variant, rs61753103, is located in the RABEP1 gene. RABEP1 is involved in endocytic membrane fusion and membrane trafficking. A recent genome-wide association study identified RABEP1 to be associated with increased Alzheimer’s disease risk (Jansen et al., 2018).
Most prioritized variants identified here are located in genes that directly affect chronic diseases. While additional biological validation is required to better characterize the relationship between these loci and the longevity process, it is promising that the prioritized variants are located on genes previously implicated in disease. Under the assumption that exceptional longevity is often caused by not having a fatal disease earlier in life or a cascade of end-of-life diseases (e.g., Alzheimer’s disease, heart disease, cancer, etc.), these prioritized variants are more likely to have a protective effect against mortality because they affect the same genes that have previously been associated with fatal diseases. Therefore, these variants not only affect longevity, but likely contribute to decreased mortality due to common diseases and may be viable drug targets for disease-specific studies.
Variants in Previously Identified Longevity Candidate Genes
Strict filters were used to identify the most likely causal variants in this set of six independent cousin pairs. However, the filtering criteria likely contribute to a high false negative rate and therefore it is unlikely that this analysis has provided an exhaustive list of all variants associated with longevity in these pedigrees. Furthermore, the use of whole exome sequencing data limits the ability to detect any significant variants that reside outside the protein-coding regions of genes. Five additional variants that were shared in at least one cousin pair were identified in genes previously implicated in longevity: PROX2, SEMA6D, MARK4, MEF2A, and EBF1. These variants, in addition to the other variants identified in this study, may drive the exceptional longevity of these pedigrees and should not be discounted.
PROX2 is a transcription factor specific to RNA polymerase II implicated in lens fiber cell morphogenesis and lymphatic endothelial cell differentiation and associated with parental longevity (Pilling et al., 2017). One cousin pair carried a frameshift variant at position 75321938 on chromosome 14 (no accession) implicated in this locus. This variant was not prioritized here because there was no information about its frequency in the ADGC dataset.
Pilling et al. (2017) also identified variation in SEMA6D associated with longer parental lifespan. SEMA6D is involved in the immune response, and is responsible for the maintenance and modification of neuronal connections (He et al., 2002). Multiple studies have found SEMA6D to be related to tumor angiogenesis and to play an important role in the development of gastric cancer (Qu et al., 2019; Zhao et al., 2006). One cousin pair shared the missense mutation rs769450413 located in this gene. However, the Alzheimer’s Disease Risk Gradient Filter also failed to prioritize this variant because it was not genotyped in the ADGC dataset.
MARK4 regulates the transition between stable and dynamic microtubules and plays a role in cell cycle progression (Rovina et al., 2014). MARK4 also regulates tau protein phosphorylation and is proposed to be functionally important to the progression of Alzheimer’s disease (Gu et al., 2013; Seshadri et al., 2010; Sun et al., 2016) and parental longevity (Pilling et al., 2017). Multiple studies also provide evidence for the expression of MARK4 as a potential marker for breast and prostate cancer (Heidary Arash et al., 2017; Jenardhanan et al., 2014; Pardo et al., 2016). One cousin pair shared the missense variant rs753496642 in this gene, which SIFT categorizes as ‘Damaging.’ This mutation was also excluded by the Alzheimer’s Disease Risk Gradient Filter because there was no information about its frequency in the ADGC dataset.
DMAC2 variant, rs139204637, passed all but the Biological Context filter, because DMAC2 has not previously been implicated in the aging process. MEF2A and EBF1 are regulators for the DMAC2 gene, which was implicated in one cousin pair. MEF2A conveys significant association with healthy aging (Druley et al., 2016). MEF2A is a transcriptional activator involved in muscle development, neuronal differentiation, cell growth control, and apoptosis. Variants in the 3’-UTR region of this gene are associated with coronary artery disease (Huang and Wang, 2015; Xiong et al., 2019; Xu et al., 2016). EBF1 is a transcriptional activator which identifies changes in the palindromic sequence. EBF1 is involved in the regulation of metabolic and inflammatory signaling pathways, and the loss of gene function results in impaired insulin and inflammatory signaling (Griffin et al., 2013). EBF1 plays a role in a variety of diseases including breast cancer (Fernandez-Jimenez et al., 2017; Garcia-Closas et al., 2013; Michailidou et al., 2013), coronary artery disease (Ehret et al., 2011; Li et al., 2017; Singh et al., 2015; Wain et al., 2011), Hodgkin lymphoma (Bohle et al., 2013), multiple sclerosis (Martinez et al., 2005; Sombekke et al., 2010), and leukemia (Heltemes-Harris et al., 2011; Mesuraca et al., 2015; Welsh et al., 2018).
Efforts to understand the genetic basis of longevity phenotypes have yielded few definitive findings to date. As is the case with other traits, heterogeneity in the diagnosis and etiology of these phenotypes creates significant challenges. For example, longevity is clearly influenced by genetics, epigenetics, environment, and chance (e.g., no fatal accidents early in life). The high-risk pedigree-based approach minimizes genetic heterogeneity and may also reduce other sources of heterogeneity; recall bias was reduced by the existence of extensive genealogy data. This analysis of whole exome sequences in longevity pedigrees identified six putative causal variants, including two that showed evidence of segregation in extended pedigree analyses. Biological validation of these candidates is necessary to characterize variant effects, the filtering criteria used might have allowed for false positive results due to chance sharing of rare variants among relatives. These findings suggest that further evaluation of these candidate variants is warranted and highlight the utility of this unique pedigree-based approach to gene discovery.
Supplementary Material
Acknowledgements
We appreciate the contributions of Brigham Young University in supporting this research. This research is supported by RF1AG054052 (PI: Kauwe) and U01AG052411 (PI: Goate).
We thank the Pedigree and Population Resource of Huntsman Cancer Institute, University of Utah (funded in part by the Huntsman Cancer Foundation) for its role in the ongoing collection, maintenance and support of the Utah Population Database (UPDB). We also acknowledge partial support for the UPDB through grant P30 CA2014 from the National Cancer Institute, University of Utah and from the University of Utah’s program in Personalized Health and Center for Clinical and Translational Science.
The authors would like to thank the NHLBI GO Exome Sequencing Project and its ongoing studies which produced and provided exome variant calls for comparison: the Lung GO Sequencing Project (HL-102923), the WHI Sequencing Project (HL-102924), the Broad GO Sequencing Project (HL-102925), the Seattle GO Sequencing Project (HL-102926) and the Heart GO Sequencing Project (HL-103010).
Alzheimer’s Disease Genetics Consortium (ADGC)
Data from ADGC was appropriately downloaded from dbGaP (accession: phs000372.v1.p1). We acknowledge the contributions of
The members of the Alzheimer’s Disease Genetics Consortium are: Marilyn S. Albert1, Roger L. Albin2−4, Liana G. Apostolova5, Steven E. Arnold6, Clinton T. Baldwin7, Robert Barber8, Michael M. Barmada9, Lisa L. Barnes10, 11, Thomas G. Beach12, Gary W. Beecham13, 14, Duane Beekly15, David A. Bennett10, 16, Eileen H. Bigio17, Thomas D. Bird18, Deborah Blacker19,20, Bradley F. Boeve21, James D. Bowen22, Adam Boxer23, James R. Burke24, Joseph D. Buxbaum25, 26, 27, Nigel J. Cairns28, Laura B. Cantwell29, Chuanhai Cao30, Chris S. Carlson31, Regina M. Carney13, Minerva M. Carrasquillo33, Steven L. Carroll34, Helena C. Chui35, David G. Clark36, Jason Corneveaux37, Paul K. Crane38, David H. Cribbs39, Elizabeth A. Crocco40, Carlos Cruchaga41, Philip L. De Jager42,43, Charles DeCarli44, Steven T. DeKosky45, F. Yesim Demirci9, Malcolm Dick46, Dennis W. Dickson33, Ranjan Duara47, Nilufer Ertekin-Taner33,48, Denis Evans49, Kelley M. Faber50, Kenneth B. Fallon34, Martin R. Farlow51, Lindsay A Farrer7,52,76,77,83, Steven Ferris53, Tatiana M. Foroud50, Matthew P. Frosch54, Douglas R. Galasko55, Mary Ganguli56, Marla Gearing57,58, Daniel H. Geschwind59, Bernardino Ghetti60, John R. Gilbert13,14, Sid Gilman2, Jonathan D. Glass61, Alison M. Goate41, Neill R. Graff-Radford33,48, Robert C. Green62, John H. Growdon63, Jonathan L. Haines64, 65, Hakon Hakonarson66, Kara L. Hamilton-Nelson13, Ronald L. Hamilton67, John Hardy68, Lindy E. Harrell36, Elizabeth Head69, Lawrence S. Honig70, Matthew J. Huentelman37, Christine M. Hulette71, Bradley T. Hyman63, Gail P. Jarvik72,73, Gregory A. Jicha74, Lee-Way Jin75, Gyungah Jun7,76,77, M. Ilyas Kamboh9,78, Anna Karydas23, John S.K. Kauwe79, Jeffrey A. Kaye80,81, Ronald Kim82, Edward H. Koo55, Neil W. Kowall83,84, Joel H. Kramer85, Patricia Kramer80,86, Walter A. Kukull87, Frank M. LaFerla88, James J. Lah61, Eric B. Larson38,89, James B. Leverenz90, Allan I. Levey61, Ge Li91, Andrew P. Lieberman92, Chiao-Feng Lin29, Oscar L. Lopez78, Kathryn L. Lunetta76, Constantine G. Lyketsos93, Wendy J. Mack94, Daniel C. Marson36, Eden R. Martin13,14, Frank Martiniuk95, Deborah C. Mash96, Eliezer Masliah55,97, Richard Mayeux70, 109, 110, Wayne C. McCormick38, Susan M. McCurry98, Andrew N. McDavid31, Ann C. McKee83,84, Marsel Mesulam99, Bruce L. Miller23, Carol A. Miller100, Joshua W. Miller75, Thomas J. Montine90, John C. Morris28, 101, Jill R. Murrell50, 60, Amanda J. Myers40, Adam C. Naj13, John M. Olichney44, Vernon S. Pankratz102, Joseph E. Parisi103,104, Margaret A. Pericak-Vance13, 14, Elaine Peskind91, Ronald C. Petersen21, Aimee Pierce39, Wayne W. Poon46, Huntington Potter30, Joseph F. Quinn80, Ashok Raj30, Murray Raskind91, Eric M. Reiman37,105−107, Barry Reisberg53,108, Christiane Reitz70,109,110, John M. Ringman5, Erik D. Roberson36, Ekaterina Rogaeva111, Howard J. Rosen23, Roger N. Rosenberg112, Mary Sano26, Andrew J. Saykin50,113, Gerard D. Schellenberg29, Julie A. Schneider10,114, Lon S. Schneider35,115, William W. Seeley23, Amanda G. Smith30, Joshua A. Sonnen90, Salvatore Spina60, Peter St George-Hyslop111,116, Robert A. Stern83, Rudolph E. Tanzi63, John Q. Trojanowski29, Juan C. Troncoso117, Debby W. Tsuang91, Otto Valladares29, Vivianna M. Van Deerlin29, Linda J. Van Eldik118, Badri N. Vardarajan7, Harry V. Vinters5,119, Jean Paul Vonsattel120, Li-San Wang29, Sandra Weintraub99, Kathleen A. Welsh-Bohmer24, 121, Jennifer Williamson70, Randall L. Woltjer122, Clinton B. Wright123, Steven G. Younkin33, Chang-En Yu38, Lei Yu10
1Department of Neurology, Johns Hopkins University, Baltimore, Maryland, 2Department of Neurology, University of Michigan, Ann Arbor, Michigan, 3Geriatric Research, Education and Clinical Center (GRECC), VA Ann Arbor Healthcare System (VAAAHS), Ann Arbor, Michigan, 4Michigan Alzheimer Disease Center, Ann Arbor, Michigan, 5Department of Neurology, University of California Los Angeles, Los Angeles, California, 6Department of Psychiatry, University of Pennsylvania Perelman School of Medicine, Philadelphia, Pennsylvania, 7Department of Medicine (Genetics Program), Boston University, Boston, Massachusetts, 8Department of Pharmacology and Neuroscience, University of North Texas Health Science Center, Fort Worth, Texas, 9Department of Human Genetics, University of Pittsburgh, Pittsburgh, Pennsylvania, 10Department of Neurological Sciences, Rush University Medical Center, Chicago, Illinois, 11Department of Behavioral Sciences, Rush University Medical Center, Chicago, Illinois, 12Civin Laboratory for Neuropathology, Banner Sun Health Research Institute, Phoenix, Arizona, 13The John P. Hussman Institute for Human Genomics, University of Miami, Miami, Florida, 14Dr. John T. Macdonald Foundation Department of Human Genetics, University of Miami, Miami, Florida, 15National Alzheimer’s Coordinating Center, University of Washington, Seattle, Washington, 16Rush Alzheimer’s Disease Center, Rush University Medical Center, Chicago, Illinois, 17Department of Pathology, Northwestern University, Chicago, Illinois, 18Department of Neurology, University of Washington, Seattle, Washington, 19Department of Epidemiology, Harvard School of Public Health, Boston, Massachusetts, 20Department of Psychiatry, Massachusetts General Hospital/Harvard Medical School, Boston, Massachusetts, 21Department of Neurology, Mayo Clinic, Rochester, Minnesota, 22Swedish Medical Center, Seattle, Washington, 23Department of Neurology, University of California San Francisco, San Francisco, California, 24Department of Medicine, Duke University, Durham, North Carolina, 25Department of Neuroscience, Mount Sinai School of Medicine, New York, New York, 26Department of Psychiatry, Mount Sinai School of Medicine, New York, New York, 27Departments of Genetics and Genomic Sciences, Mount Sinai School of Medicine, New York, New York, 28Department of Pathology and Immunology, Washington University, St. Louis, Missouri, 29Department of Pathology and Laboratory Medicine, University of Pennsylvania Perelman School of Medicine, Philadelphia, Pennsylvania, 30USF Health Byrd Alzheimer’s Institute, University of South Florida, Tampa, Florida, 31Fred Hutchinson Cancer Research Center, Seattle, Washington, 32Department of Psychiatry, Vanderbilt University, Nashville, Tennessee, 33Department of Neuroscience, Mayo Clinic, Jacksonville, Florida, 34Department of Pathology, University of Alabama at Birmingham, Birmingham, Alabama, 35Department of Neurology, University of Southern California, Los Angeles, California, 36Department of Neurology, University of Alabama at Birmingham, Birmingham, Alabama, 37Neurogenomics Division, Translational Genomics Research Institute, Phoenix, Arizona, 38Department of Medicine, University of Washington, Seattle, Washington, 39Department of Neurology, University of California Irvine, Irvine, California, 40Department of Psychiatry and Behavioral Sciences, Miller School of Medicine, University of Miami, Miami, Florida, 41Department of Psychiatry and Hope Center Program on Protein Aggregation and Neurodegeneration, Washington University School of Medicine, St. Louis, Missouri, 42Program in Translational NeuroPsychiatric Genomics, Institute for the Neurosciences, Department of Neurology & Psychiatry, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts, 43Program in Medical and Population Genetics, Broad Institute, Cambridge, Massachusetts, 44Department of Neurology, University of California Davis, Sacramento, California, 45University of Virginia School of Medicine, Charlottesville, Virginia, 46Institute for Memory Impairments and Neurological Disorders, University of California Irvine, Irvine, California, 47Wien Center for Alzheimer’s Disease and Memory Disorders, Mount Sinai Medical Center, Miami Beach, Florida, 48Department of Neurology, Mayo Clinic, Jacksonville, Florida, 49Rush Institute for Healthy Aging, Department of Internal Medicine, Rush University Medical Center, Chicago, Illinois, 50Department of Medical and Molecular Genetics, Indiana University, Indianapolis, Indiana, 51Department of Neurology, Indiana University, Indianapolis, Indiana, 52Department of Epidemiology, Boston University, Boston, Massachusetts, 53Department of Psychiatry, New York University, New York, New York, 54C.S. Kubik Laboratory for Neuropathology, Massachusetts General Hospital, Charlestown, Massachusetts, 55Department of Neurosciences, University of California San Diego, La Jolla, California, 56Department of Psychiatry, University of Pittsburgh, Pittsburgh, Pennsylvania, 57Department of Pathology and Laboratory Medicine, Emory University, Atlanta, Georgia, 58Emory Alzheimer’s Disease Center, Emory University, Atlanta, Georgia, 59Neurogenetics Program, University of California Los Angeles, Los Angeles, California, 60Department of Pathology and Laboratory Medicine, Indiana University, Indianapolis, Indiana, 61Department of Neurology, Emory University, Atlanta, Georgia, 62Division of Genetics, Department of Medicine and Partners Center for Personalized Genetic Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts, 63Department of Neurology, Massachusetts General Hospital/Harvard Medical School, Boston, Massachusetts, 64Department of Molecular Physiology and Biophysics, Vanderbilt University, Nashville, Tennessee, 65Vanderbilt Center for Human Genetics Research, Vanderbilt University, Nashville, Tennessee, 66Center for Applied Genomics, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, 67Department of Pathology (Neuropathology), University of Pittsburgh, Pittsburgh, Pennsylvania, 68Institute of Neurology, University College London, Queen Square, London, 69Sanders-Brown Center on Aging, Department of Molecular and Biomedical Pharmacology, University of Kentucky, Lexington, Kentucky, 70Taub Institute on Alzheimer’s Disease and the Aging Brain, Department of Neurology, Columbia University, New York, New York, 71Department of Pathology, Duke University, Durham, North Carolina, 72Department of Genome Sciences, University of Washington, Seattle, Washington, 73Department of Medicine (Medical Genetics), University of Washington, Seattle, Washington, 74Sanders-Brown Center on Aging, Department Neurology, University of Kentucky, Lexington, Kentucky, 75Department of Pathology and Laboratory Medicine, University of California Davis, Sacramento, California, 76Department of Biostatistics, Boston University, Boston, Massachusetts, 77Department of Ophthalmology, Boston University, Boston, Massachusetts, 78University of Pittsburgh Alzheimer’s Disease Research Center, Pittsburgh, Pennsylvania, 79Department of Biology, Brigham Young University, Provo, Utah, 80Department of Neurology, Oregon Health & Science University, Portland, Oregon, 81Department of Neurology, Portland Veterans Affairs Medical Center, Portland, Oregon, 82Department of Pathology and Laboratory Medicine, University of California Irvine, Irvine, California, 83Department of Neurology, Boston University, Boston, Massachusetts, 84Department of Pathology, Boston University, Boston, Massachusetts, 85Department of Neuropsychology, University of California San Francisco, San Francisco, California, 86Department of Molecular & Medical Genetics, Oregon Health & Science University, Portland, Oregon, 87Department of Epidemiology, University of Washington, Seattle, Washington, 88Department of Neurobiology and Behavior, University of California Irvine, Irvine, California, 89Group Health Research Institute, Group Health, Seattle, Washington, 90Department of Pathology, University of Washington, Seattle, Washington, 91Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle, Washington, 92Department of Pathology, University of Michigan, Ann Arbor, Michigan, 93Department of Psychiatry, Johns Hopkins University, Baltimore, Maryland, 94Department of Preventive Medicine, University of Southern California, Los Angeles, California, 95Department of Medicine - Pulmonary, New York University, New York, New York, 96Department of Neurology, University of Miami, Miami, Florida, 97Department of Pathology, University of California San Diego, La Jolla, California, 98School of Nursing Northwest Research Group on Aging, University of Washington, Seattle, Washington, 99Cognitive Neurology and Alzheimer’s Disease Center, Northwestern University, Chicago, Illinois, 100Department of Pathology, University of Southern California, Los Angeles, California, 101Department of Neurology, Washington University, St. Louis, Missouri, 102Department of Biostatistics, Mayo Clinic, Rochester, Minnesota, 103Department of Anatomic Pathology, Mayo Clinic, Rochester, Minnesota, 104Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota, 105Arizona Alzheimer’s Consortium, Phoenix, Arizona, 106Department of Psychiatry, University of Arizona, Phoenix, Arizona, 107Banner Alzheimer’s Institute, Phoenix, Arizona, 108Alzheimer’s Disease Center, New York University, New York, New York, 109Gertrude H. Sergievsky Center, Columbia University, New York, New York, 110Department of Neurology, Columbia University, New York, New York, 111Tanz Centre for Research in Neurodegenerative Disease, University of Toronto, Toronto, Ontario, 112Department of Neurology, University of Texas Southwestern, Dallas, Texas, 113Department of Radiology and Imaging Sciences, Indiana University, Indianapolis, Indiana, 114Department of Pathology (Neuropathology), Rush University Medical Center, Chicago, Illinois, 115Department of Psychiatry, University of Southern California, Los Angeles, California, 116Cambridge Institute for Medical Research and Department of Clinical Neurosciences, University of Cambridge, Cambridge, 117Department of Pathology, Johns Hopkins University, Baltimore, Maryland, 118Sanders-Brown Center on Aging, Department of Anatomy and Neurobiology, University of Kentucky, Lexington, Kentucky, 119Department of Pathology & Laboratory Medicine, University of California Los Angeles, Los Angeles, California, 120Taub Institute on Alzheimer’s Disease and the Aging Brain, Department of Pathology, Columbia University, New York, New York, 121Department of Psychiatry & Behavioral Sciences, Duke University, Durham, North Carolina, 122Department of Pathology, Oregon Health & Science University, Portland, Oregon, 123Evelyn F. McKnight Brain Institute, Department of Neurology, Miller School of Medicine, University of Miami, Miami, Florida
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Work Cited
- Agudo D, et al. , 2004. Nup88 mRNA overexpression is associated with high aggressiveness of breast cancer. Int J Cancer. 109, 717–20. [DOI] [PubMed] [Google Scholar]
- Antonson P, et al. , 1996. A novel human CCAAT/enhancer binding protein gene, C/EBPepsilon, is expressed in cells of lymphoid and myeloid lineages and is localized on chromosome 14q11.2 close to the T-cell receptor alpha/delta locus. Genomics. 35, 30–8. [DOI] [PubMed] [Google Scholar]
- Atzmon G, et al. , 2006. Lipoprotein Genotype and Conserved Pathway for Exceptional Longevity in Humans. PLOS Biology. 4, e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auton A, et al. , 2015. A global reference for human genetic variation. Nature. 526, 68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodian DL, et al. , 2014. Germline variation in cancer-susceptibility genes in a healthy, ancestrally diverse cohort: implications for individual genome sequencing. PloS one. 9, e94554–e94554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehme KL, et al. , ADGC 1000 genomes combined workflow (electronic document). September 2014. [Google Scholar]
- Bohle V, et al. , 2013. Role of early B-cell factor 1 (EBF1) in Hodgkin lymphoma. Leukemia. 27, 671–9. [DOI] [PubMed] [Google Scholar]
- Bourguiba-Hachemi S, et al. , 2016. ZFAT gene variant association with multiple sclerosis in the Arabian Gulf population: A genetic basis for gender-associated susceptibility. Molecular medicine reports. 14, 3543–3550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau A, et al. , 2014. Inferring rare disease risk variants based on exact probabilities of sharing by multiple affected relatives. Bioinformatics. 30, 2189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon-Albright LA, 2008. Utah family-based analysis: past, present and future. Hum Hered. 65, 209–20. [DOI] [PubMed] [Google Scholar]
- Deelen J, et al. , 2019. A meta-analysis of genome-wide association studies identifies multiple longevity genes. Nature Communications. 10, 3669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druley TE, et al. , 2016. Candidate gene resequencing to identify rare, pedigree-specific variants influencing healthy aging phenotypes in the long life family study. BMC geriatrics. 16, 80–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehret GB, et al. , 2011. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature. 478, 103–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erikson GA, et al. , 2016. Whole-Genome Sequencing of a Healthy Aging Cohort. Cell. 165, 1002–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Jimenez N, et al. , 2017. Lowly methylated region analysis identifies EBF1 as a potential epigenetic modifier in breast cancer. Epigenetics. 12, 964–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finetti P, et al. , 2014. ESPL1 is a candidate oncogene of luminal B breast cancers. Breast Cancer Res Treat. 147, 51–9. [DOI] [PubMed] [Google Scholar]
- Franceschi C, et al. , 2018. The Continuum of Aging and Age-Related Diseases: Common Mechanisms but Different Rates. Front Med (Lausanne). 5, 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freed EF, Baserga SJ, 2010. The C-terminus of Utp4, mutated in childhood cirrhosis, is essential for ribosome biogenesis. Nucleic Acids Res. 38, 4798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchsberger C, et al. , 2016. The genetic architecture of type 2 diabetes. Nature. 536, 41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto T, et al. , 2009. ZFAT is an antiapoptotic molecule and critical for cell survival in MOLT-4 cells. FEBS Lett. 583, 568–72. [DOI] [PubMed] [Google Scholar]
- Garcia-Closas M, et al. , 2013. Genome-wide association studies identify four ER negative-specific breast cancer risk loci. Nat Genet. 45, 392–8, 398e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gharbi H, et al. , 2016. Association of genetic variation in IKZF1, ARID5B, CDKN2A, and CEBPE with the risk of acute lymphoblastic leukemia in Tunisian children and their contribution to racial differences in leukemia incidence. Pediatr Hematol Oncol. 33, 157–67. [DOI] [PubMed] [Google Scholar]
- Griffin MJ, et al. , 2013. Early B-cell factor-1 (EBF1) is a key regulator of metabolic and inflammatory signaling pathways in mature adipocytes. J Biol Chem. 288, 35925–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu GJ, et al. , 2013. Role of individual MARK isoforms in phosphorylation of tau at Ser(2)(6)(2) in Alzheimer’s disease. Neuromolecular Med. 15, 458–69. [DOI] [PubMed] [Google Scholar]
- Gurvits N, et al. , 2017. Separase is a marker for prognosis and mitotic activity in breast cancer. Br J Cancer. 117, 1383–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashizume C, et al. , 2010. Characterization of the role of the tumor marker Nup88 in mitosis. Mol Cancer. 9, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Z, et al. , 2002. Knowing how to navigate: mechanisms of semaphorin signaling in the nervous system. Sci STKE. 2002, re1. [DOI] [PubMed] [Google Scholar]
- Heidary Arash E, et al. , 2017. MARK4 inhibits Hippo signaling to promote proliferation and migration of breast cancer cells. EMBO Rep. 18, 420–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heltemes-Harris LM, et al. , 2011. Ebf1 or Pax5 haploinsufficiency synergizes with STAT5 activation to initiate acute lymphoblastic leukemia. J Exp Med. 208, 1135–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang XC, Wang W, 2015. Association of MEF2A gene 3’UTR mutations with coronary artery disease. Genet Mol Res. 14, 11073–8. [DOI] [PubMed] [Google Scholar]
- Inoue N, et al. , 2012. Associations between autoimmune thyroid disease prognosis and functional polymorphisms of susceptibility genes, CTLA4, PTPN22, CD40, FCRL3, and ZFAT, previously revealed in genome-wide association studies. J Clin Immunol. 32, 1243–52. [DOI] [PubMed] [Google Scholar]
- Jansen IE, et al. , 2018. Genetic meta-analysis identifies 9 novel loci and functional pathways for Alzheimer’s disease risk. bioRxiv. 258533. [Google Scholar]
- Jenardhanan P, et al. , 2014. The structural analysis of MARK4 and the exploration of specific inhibitors for the MARK family: a computational approach to obstruct the role of MARK4 in prostate cancer progression. Mol Biosyst. 10, 1845–68. [DOI] [PubMed] [Google Scholar]
- Karczewski KJ, et al. , 2019. Variation across 141,456 human exomes and genomes reveals the spectrum of loss-of-function intolerance across human protein-coding genes. bioRxiv. 531210. [Google Scholar]
- Karczewski KJ, et al. , 2017. The ExAC browser: displaying reference data information from over 60 000 exomes. Nucleic acids research. 45, D840–D845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert J-C, et al. , 2013. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease . Nature Genetics. 45, 1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang L, et al. , 2017. Prevalence and determinants of undetected dementia in the community: a systematic literature review and a meta-analysis. BMJ open. 7, e011146–e011146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara J, et al. , 2013. Towards measurement of the Healthy Ageing Phenotype in lifestyle-based intervention studies. Maturitas. 76, 189–199. [DOI] [PubMed] [Google Scholar]
- Li H, 2013. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. ArXiv. 1303. [Google Scholar]
- Li H, Durbin R, 2009. Fast and accurate short read alignment with Burrows–Wheeler transform. Bioinformatics. 25, 1754–1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, et al. , 2017. Association in a Chinese population of a genetic variation in the early B-cell factor 1 gene with coronary artery disease. BMC Cardiovasc Disord. 17, 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loh P-R, et al. , 2016. Reference-based phasing using the Haplotype Reference Consortium panel. Nature genetics. 48, 1443–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher B, 2008. Personal genomes: The case of the missing heritability. Nature. 456, 18–21. [DOI] [PubMed] [Google Scholar]
- Martinez A, et al. , 2005. Early B-cell Factor gene association with multiple sclerosis in the Spanish population. BMC Neurol. 5, 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez N, et al. , 1999. The nuclear pore complex protein Nup88 is overexpressed in tumor cells. Cancer Res. 59, 5408–11. [PubMed] [Google Scholar]
- McKenna A, et al. , 2010. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome research. 20, 1297–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesuraca M, et al. , 2015. ZNF423 and ZNF521: EBF1 Antagonists of Potential Relevance in B-Lymphoid Malignancies. Biomed Res Int. 2015, 165238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michailidou K, et al. , 2013. Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat Genet. 45, 353–61, 361e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee M, et al. , 2011. Separase Loss of Function Cooperates with the Loss of p53 in the Initiation and Progression of T- and B-Cell Lymphoma, Leukemia and Aneuploidy in Mice. PLOS ONE. 6, e22167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naj AC, et al. , 2017. GENOME-WIDE RARE VARIANT IMPUTATION AND TISSUE-SPECIFIC TRANSCRIPTOMIC ANALYSIS IDENTIFY NOVEL RARE VARIANT CANDIDATE LOCI IN LATE-ONSET ALZHEIMER’S DISEASE: THE ALZHEIMER’S DISEASE GENETICS CONSORTIUM. Alzheimer’s & Dementia. 13, P189. [Google Scholar]
- Naj AC, et al. , 2011. Common variants at MS4A4/MS4A6E, CD2AP, CD33 and EPHA1 are associated with late-onset Alzheimer’s disease. Nat Genet. 43, 436–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott J, et al. , 2011. Family-based designs for genome-wide association studies. Nat Rev Genet. 12, 465–74. [DOI] [PubMed] [Google Scholar]
- Pardo OE, et al. , 2016. miR-515–5p controls cancer cell migration through MARK4 regulation. EMBO Rep. 17, 570–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel D, et al. , 2019. Association of Rare Coding Mutations With Alzheimer Disease and Other Dementias Among Adults of European Ancestry. JAMA Network Open. 2, e191350–e191350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilling LC, et al. , 2017. Human longevity: 25 genetic loci associated in 389,166 UK biobank participants. Aging. 9, 2504–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu S, et al. , 2019. [Semaphorin 6D and Snail are highly expressed in gastric cancer and positively correlated with malignant clinicopathological indexes]. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 35, 932–937. [PubMed] [Google Scholar]
- Richards S, et al. , 2015. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 17, 405–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridge PG, et al. , 2017. Linkage, whole genome sequence, and biological data implicate variants in RAB10 in Alzheimer’s disease resilience. Genome medicine. 9, 100–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovina D, et al. , 2014. Microtubule-associated protein/microtubule affinity-regulating kinase 4 (MARK4) plays a role in cell cycle progression and cytoskeletal dynamics. Eur J Cell Biol. 93, 355–65. [DOI] [PubMed] [Google Scholar]
- Sakai K, et al. , 2001. Identification of susceptibility loci for autoimmune thyroid disease to 5q31-q33 and Hashimoto’s thyroiditis to 8q23-q24 by multipoint affected sib-pair linkage analysis in Japanese. Hum Mol Genet. 10, 1379–86. [DOI] [PubMed] [Google Scholar]
- Schneider J, et al. , 2010. Nup88 expression is associated with myometrial invasion in endometrial carcinoma. Int J Gynecol Cancer. 20, 804–8. [DOI] [PubMed] [Google Scholar]
- Schunkert H, et al. , 2011. Large-scale association analysis identifies 13 new susceptibility loci for coronary artery disease. Nat Genet. 43, 333–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebastiani P, et al. , 2017. Four Genome-Wide Association Studies Identify New Extreme Longevity Variants. The Journals of Gerontology: Series A. 72, 1453–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seshadri S, et al. , 2010. Genome-wide analysis of genetic loci associated with Alzheimer disease. Jama. 303, 1832–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S, et al. , 2020. Genome-wide association and Mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nature Communications. 11, 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim N-L, et al. , 2012. SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic acids research. 40, W452–W457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A, et al. , 2015. Gene by stress genome-wide interaction analysis and path analysis identify EBF1 as a cardiovascular and metabolic risk gene. Eur J Hum Genet. 23, 854–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sombekke MH, et al. , 2010. Analysis of multiple candidate genes in association with phenotypes of multiple sclerosis. Mult Scler. 16, 652–9. [DOI] [PubMed] [Google Scholar]
- Steinthorsdottir V, et al. , 2014. Identification of low-frequency and rare sequence variants associated with elevated or reduced risk of type 2 diabetes. Nat Genet. 46, 294–8. [DOI] [PubMed] [Google Scholar]
- Studd JB, et al. , 2019. Genetic predisposition to B-cell acute lymphoblastic leukemia at 14q11.2 is mediated by a CEBPE promoter polymorphism. Leukemia. 33, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugrue LP, Desikan RS, 2019. What Are Polygenic Scores and Why Are They Important? Jama. 321, 1820–1821. [DOI] [PubMed] [Google Scholar]
- Sun J, et al. , 2015. Association between CEBPE Variant and Childhood Acute Leukemia Risk: Evidence from a Meta-Analysis of 22 Studies. PLoS One. 10, e0125657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun W, et al. , 2016. Attenuation of synaptic toxicity and MARK4/PAR1-mediated Tau phosphorylation by methylene blue for Alzheimer’s disease treatment. Scientific reports. 6, 34784–34784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam V, et al. , 2019. Benefits and limitations of genome-wide association studies. Nat Rev Genet. 20, 467–484. [DOI] [PubMed] [Google Scholar]
- Teerlink CC, et al. , 2018. A nonsynonymous variant in the GOLM1 gene in cutaneous malignant melanoma. JNCI: Journal of the National Cancer Institute. 110, 1380–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teerlink CC, et al. , 2020. A role for the MEGF6 gene in predisposition to osteoporosis. bioRxiv. 2020.01.09.900696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teerlink CC, et al. , 2016. Genome-wide association of familial prostate cancer cases identifies evidence for a rare segregating haplotype at 8q24.21. Hum Genet. 135, 923–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson BA, et al. , 2020. A novel ribosomal protein S20 variant in a family with unexplained colorectal cancer and polyposis. bioRxiv. 2019.12.16.877084. [DOI] [PubMed] [Google Scholar]
- Truong BT, et al. , 2003. CCAAT/Enhancer binding proteins repress the leukemic phenotype of acute myeloid leukemia. Blood. 101, 1141–8. [DOI] [PubMed] [Google Scholar]
- Wain LV, et al. , 2011. Genome-wide association study identifies six new loci influencing pulse pressure and mean arterial pressure. Nat Genet. 43, 1005–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, et al. , 2015. CEBPE polymorphism confers an increased risk of childhood acute lymphoblastic leukemia: a meta-analysis of 11 case-control studies with 5,639 cases and 10,036 controls. Ann Hematol. 94, 181–5. [DOI] [PubMed] [Google Scholar]
- Wang K, et al. , 2010. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic acids research. 38, e164–e164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh SJ, et al. , 2018. Deregulation of kinase signaling and lymphoid development in EBF1-PDGFRB ALL leukemogenesis. Leukemia. 32, 38–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willcox BJ, et al. , 2008. FOXO3A genotype is strongly associated with human longevity. Proceedings of the National Academy of Sciences of the United States of America. 105, 13987–13992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Y, et al. , 2019. MEF2A alters the proliferation, inflammation-related gene expression profiles and its silencing induces cellular senescence in human coronary endothelial cells. BMC Mol Biol. 20, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu DL, et al. , 2016. Novel 6-bp deletion in MEF2A linked to premature coronary artery disease in a large Chinese family. Mol Med Rep. 14, 649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H, et al. , 2013. Novel susceptibility variants at 10p12.31–12.2 for childhood acute lymphoblastic leukemia in ethnically diverse populations. J Natl Cancer Inst. 105, 733–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H, et al. , 2015. Inherited coding variants at the CDKN2A locus influence susceptibility to acute lymphoblastic leukaemia in children. Nature communications. 6, 7553–7553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B, et al. , 2005. Nucleolar localization of cirhin, the protein mutated in North American Indian childhood cirrhosis. Exp Cell Res. 311, 218–28. [DOI] [PubMed] [Google Scholar]
- Zhao XY, et al. , 2006. Expression of semaphorin 6D in gastric carcinoma and its significance. World J Gastroenterol. 12, 7388–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao ZR, et al. , 2012. Increased serum level of Nup88 protein is associated with the development of colorectal cancer. Med Oncol. 29, 1789–95. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.