Abstract
Frailty is an important factor determining a higher risk of adverse health outcomes in older adults. Although scientific community in the last two decades put a lot of effort for its definition, to date no consensus was reached on its assessment. The mainstream thinking describes frailty as a loss of physical functions or as accumulation of multiple deficits. Recently, a novel conceptual model of frailty has emerged based on the loss of harmonic interaction between multiple domains (also referred as dimensions) including genetic, biological, functional, cognitive, psychological and socio-economic domain that ultimately lead to homeostatic instability. Therefore, the multidimensional aspects of frailty condition could be captured by the comprehensive geriatric assessment (CGA) and its derived Multidimensional Prognostic Index (MPI). This instrument has been applied in different clinical settings and in several cohorts of older adults with specific acute and chronic diseases, showing always excellent accuracy in stratifying population according the mortality risk and other negative health outcomes, i.e. hospitalization, institutionalization or admission to homecare services. This MPI “plasticity” provides a single numerical prognostic index which could be helpful in clinical decision making for the management of frail older adults.
Keywords: Comprehensive geriatric assessment, Multidimensional prognostic index, Frailty
1. Introduction
Frailty is a common condition in older people. Among models traditionally used in geriatric medicine to define this condition, the multidimensional model can be considered as a novel approach to frailty characterized by the loss of harmonic interaction between multiple domains/dimensions (including genetic, biological, functional, cognitive, psychological and socio-economic domain) that ultimately lead to homeostatic instability. Therefore, the multidimensional aspects of frailty condition could be captured by the comprehensive geriatric assessment (CGA) and its derived Multidimensional Prognostic Index (MPI).
In this viewpoint article, we aim to summarize the current state of the art, the applications and the future directions of applicability of the CGA-based MPI for measuring frailty in older people.
2. Frailty
Frailty is a condition characterized by a decline in functioning across multiple physiological systems, accompanied by an elevated vulnerability to stressors (Hoogendijk et al., 2019). Frailty occurs with ageing and carries a high risk of multiple adverse health outcomes, which ultimately causes hospitalization, falls, institutionalization, and death (Clegg et al., 2013; Hoogendijk et al., 2019).
Frailty is a prevalent condition among older adults, with an estimated prevalence of 10 % in community-dwellers (Collard et al., 2012), but higher in other settings such as hospital where the frailty prevalence may range from 18 % to 40 % of patients (Cunha et al., 2019).
Recent literature has also reported that frailty is associated with a higher risk of cardiovascular disease (Veronese et al., 2017a), depression (Soysal et al., 2017) and finally to a reduction in quality of life (Kojima et al., 2016) and an important economic burden (Hajek et al., 2017).
Moreover, research suggests that frailty is caused by an overt age-associated dysregulation of multiple homeostatic systems that causes progressive loss of physiological reserves that is so severe that results in a multifunctional impairment and eventually in pathology and death (Fontana et al., 2013).
3. Underlying mechanisms of frailty
The aging process is modulated by the neuro-immuno-endocrine system, nutritional status and physical activity. These regulatory mechanisms become less effective in frail older persons, at least in part because of the presence of low-grade inflammation, i.e. inflammageing, and excessive and unopposed oxidative stress. Probably other common mechanisms are shared with the aging process, age-related diseases and geriatric syndromes including frailty (Franceschi et al., 2018). Over the long term, the accumulation of unrepaired damage at both somatic and stem cells may lead to a loss of their metabolic and functional activities, including the age-associated decline in immune function, i.e. immunosenescence. Indeed, inflammageing and immunosenescence have been suggested as contributors to frailty and sarcopenia (Wilson et al., 2017), i.e. the progressive loss of skeletal muscle mass and strength associated to reduced physical performances, conditions that are generally considered characteristic components of physical frailty (Cruz-Jentoft et al., 2019). Of note, similar mechanisms probably explain the effect of frailty of cardiovascular, respiratory, renal, hemopoietic and metabolic systems (Ferrucci and Fabbri, 2018; Franceschi et al., 2018). Hence, not surprisingly, poor nutritional status, may sustain directly and/or indirectly the downward cascade typical of frailty or, vice-versa, most of the interventions that reverse or slow down frailty are based, at least in part, on improving nutrition (Calder et al., 2017; Custodero et al., 2018) (Fig. 1).
Fig. 1.
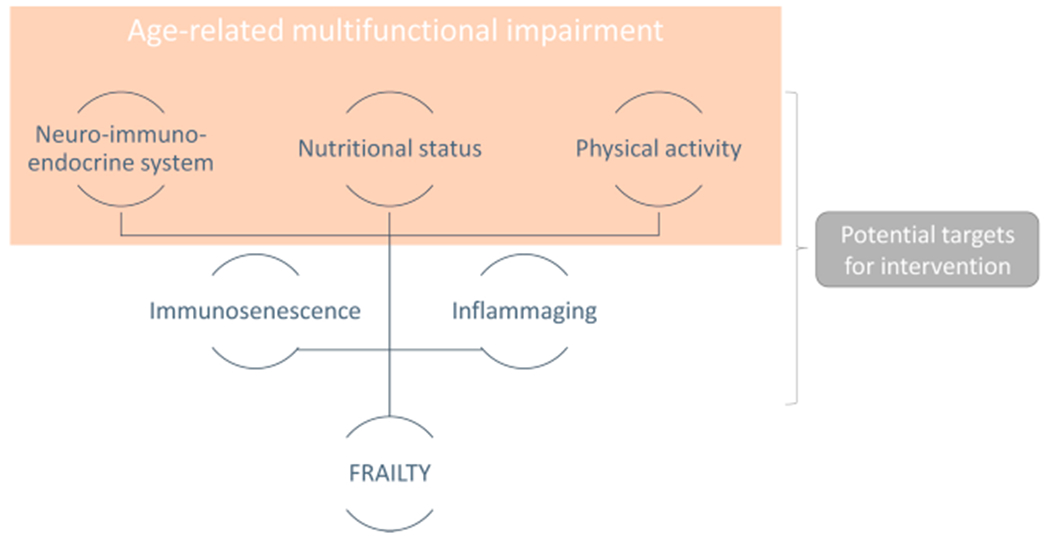
The underlying mechanisms of frailty.
4. Frailty models
Over the last two decades, several methods have been proposed to assess frailty condition which underlie different conceptual models of frailty. The phenotypic model identifies frailty by the presence of more than two of five features: a) unintentional weight loss; b) exhaustion; c) low physical activity level; d) slow walking speed; e) muscle weakness (Fried et al., 2001). The multiple-deficits model rates frailty by the number of functional, sensory and clinical deficits (Rockwood and Mitnitski, 2007). These two models and relative measurement tools, catch different trajectories of frailty in older persons and, not surprisingly, studies based on the two different definitions produced quite different results (Collard et al., 2012). For this reason, it has been suggested that in spite of the evidence that these tools convey important information on response to treatments and risk of adverse health outcomes, the translation of this evidence into clinical practice is still limited (Clegg et al., 2013; Dent et al., 2016). We argue that in both cases, these tools have limited applicability to clinical practice.
5. Clinical approach to frailty: the “multidimensional” model
Recently, a novel, general conceptual model of frailty has emerged based on a hierarchical organization of three different levels of complexity, organized like the overlapping layers of an onion (Table 1) (Ferrucci et al., 2017). The inner dimension refers to biological mechanisms involved in frailty at the subcellular level (e.g. mitochondrial dysfunction, oxidative stress, DNA damage, shortening of telomere length, maladaptive DNA methylation). The intermediate layer refers to potential physiopathological mechanisms leading to frailty condition, including chronic low-grade inflammation, energetic imbalance, anabolic deficiency, neurodegeneration. The external dimension encompasses the clinical consequences and the manifestations of frailty: functional deficits, reduced mobility, cognitive impairment, loss of independence in the activities of daily living, multiple chronic diseases, polypharmacy, and geriatric syndromes. Frailty is conceptualized as the loss of harmonic interaction between domains (also referred as dimensions) including genetic, biological, functional, cognitive, psychological and socio-economic domain. In this model, multimorbidity and polypharmacy, typically encountered in older patients, are considered both as causes and effects. Regardless of the specific tool, the diagnosis of frailty could be approximated by collecting information on physical performance, mobility, cognitive and nutritional status (Rodriguez-Manas et al., 2013). The evaluation of contribution of different illnesses, in particular chronic disease, on general health status is another important aspect of frailty (Rodriguez-Manas et al., 2013). In this exception, the condition of frailty could be captured by the traditional comprehensive geriatric assessment (CGA) that have already been introduced in geriatric clinic (Fig. 2).
Table 1.
The frailty model according three overlapping dimensions: biological, physiopathological mechanisms and clinical features.
| Biological mechanisms | Mitochondrial dysfunction Oxidative stress DNA damage Shortening of telomere length Defective autophagy DNA methylation Stem cells exhaustion Chronic low-grade inflammation |
| Pathophysiologic | Neurodegeneration Anabolic deficiency Energetic imbalance Reduced protein synthesis |
| Clinical features | Functional deficits in activity of daily living Reduced mobility Cognitive impairment Malnutrition Sarcopenia Multimorbidity Polypharmacy Geriatric syndromes |
Fig. 2.
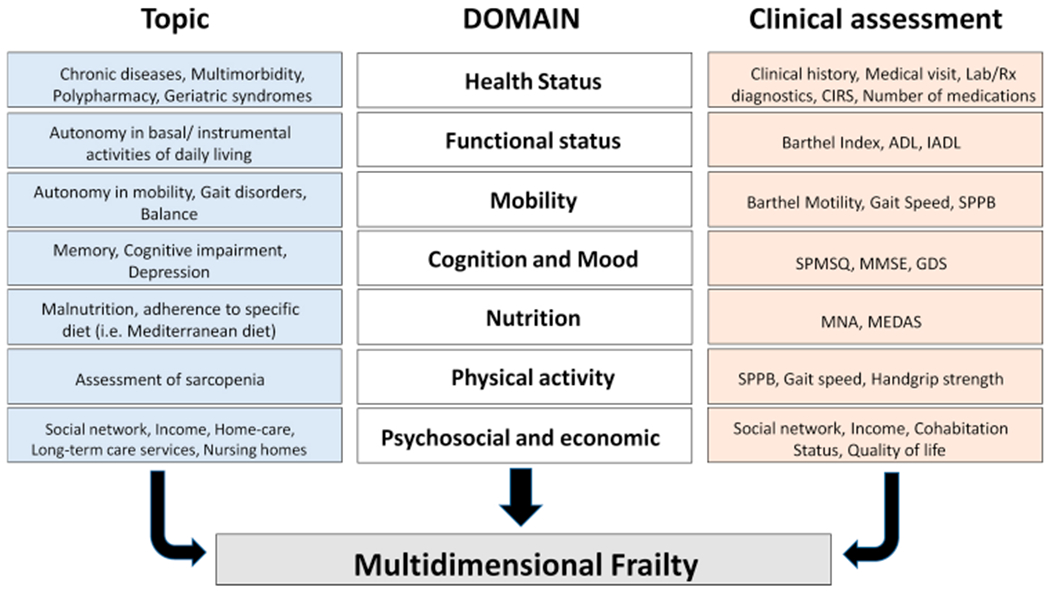
Domains of the multidimensional model of frailty.
Abbreviations: ADL: Activities of Daily Living; IADL: Instrumental Activities of Daily Living; CIRS: Cumulative Illness Rating Scale; GDS: Geriatric Depression Scale; MEDAS: Mediterranean Diet Adherence Screener; MMSE: Mini Mental State Examination; MNA: Mini Nutritional Assessment; SPMSQ: Short Portable Mental State Questionnaire; SPPB: Short Physical Performance Battery.
6. Frailty diagnosis: the comprehensive geriatric assessment (CGA)
A systematic revision of the literature on frailty tools showed that they have excellent sensitivity, but very low specificity, limiting therefore their reliability in current clinical use for the identification and diagnosis of frailty (Clegg et al., 2015). Indeed, principal international guidelines from geriatric scientific societies discourage the use of “short” instruments as tools in community-based setting, but rather recommend an approach centered on CGA (Turner et al., 2014).
According to the multidimensional model, the identification of frailty could be approximated by CGA especially if a tool that conveys information on biological, functional, psychological, clinical, social dimensions is used (Clegg et al., 2013). Operatively, CGA is administered to the patient using specific scales that explore functional disability, cognition, depression, nutritional status, comorbidities, number of drugs used by patient, falls and pressure sores risk, cohabitation status, and social and welfare context. Growing evidence from meta-analyses and systematic reviews of randomized controlled studies carried out in different clinical settings and several specific diseases, showed that routine application of CGA significantly reduce mortality. Moreover, CGA has a positive influence on other outcomes such as institutionalization, hospitalization, and functional and cognitive status of older patients. The CGA help ensure good appropriateness of prescribing and intervention in frail older adults (Pilotto et al., 2017).
Taken together, these data suggest that CGA could be used for the identification of frailty in clinical practice. Noteworthy, a recent reflection paper on physical frailty by the European Medicines Agency (EMA) reported that a complete evaluation of frailty to support its management requires a multidimensional interdisciplinary CGA (European Medicines Agency. Committee for Medicinal Products for Human Use, 2018). In this context, the Multidimensional Prognostic Index (MPI), is recognized as a CGA-based predictive tool, able to extract information from a standard CGA to categorize frailty in three subgroups with excellent prognostic value for the identification of frailty (European Medicines Agency. Committee for Medicinal Products for Human Use, 2018).
7. The Multidimensional Prognostic Index (MPI)
The Multidimensional Prognostic Index (MPI) is a common tool for evaluating frailty, particularly in primary care and hospital settings (Dent et al., 2019). The MPI was initially developed and validated as a prognostic index predicting mortality in hospitalized older patients (Pilotto et al., 2008). MPI is a product of the CGA, that uses a mathematic algorithm including information about eight domains: functional status as assessed by basal and instrumental Activities of Daily Living, cognitive status as assessed by the Short Portable Mental Status Questionnaire (SPMSQ), nutritional status as assessed by the Mini Nutritional Assessment (MNA), mobility and risk of pressure sore evaluated by the Exton-Smith score (ESS), multi-morbidity according to the Cumulative Illness Rating Scale (CIRS), the number of drugs to assess polypharmacy and co-habitation status (Pilotto et al., 2008). Interestingly, the domains included in the MPI are assessed by means of already aggregated and multidimensional in nature tools (i.e. ADL, IADL, SPMSQ, MNA, ESS, CIRS) validated in older people and widely diffuse in clinical practice. For each domain, a tripartite hierarchy was used (0 = no problems; 0.5 = minor problems; 1 = major problems), based on conventional cut-off points derived from the literature for the singular tests. In this sense, we can say that MPI is able to translate the clinical evaluation of CGA in a score, between 0 and 1, that can accurately predict mortality and other negative outcomes and so be used as prognostic tool in older people. Then, the sum of the calculated scores from the eight domains was divided by 8 to obtain a final MPI risk score ranging from 0 = no risk to 1 = higher risk of mortality (Pilotto et al., 2008). Usually, the MPI was expressed as three grades of risk: MPI-1 low risk (MPI value ≤ 0.33), MPI-2 moderate risk (MPI value between 0.34 and 0.66) and MPI-3 high risk (MPI value > 0.66). MPI requires between 15–25 min for its complete execution and the results can be automatically obtained through the program Calculate-MPI that it is possible to download for free by the www.mpiage.eu website.
A modified short-form MPI, showed similar degree of accuracy as the original MPI, but could be completed in around 20 min (Sancarlo et al., 2011). Another MPI version, the MPI-SVaMA, has been developed and validated in community-dwelling older adults who underwent a standard CGA for being admitted to nursing home and/or homecare services in Italy (Pilotto et al., 2013). The effectiveness of MPI has been tested also in population-based studies. In a large cohort of elderly subjects living in Sweden and followed-up for over 10 years, higher MPI values predicted lower survival and more days in hospital (Angleman et al., 2015). Finally, in the context of the international project called EFFICHRONIC, it has been created and validate a self-administered version of the MPI (SELFY_MPI) proposed as screening tool for community-dwelling population (Pilotto et al., 2019a). Therefore, the MPI “plasticity” allows its application on scales derived from different clinical settings and may provide a single numerical prognostic index exploring multiple dimensions that overlap with frailty of the older subject (Table 2).
Table 2.
Clinical studies using the CGA-based Multidimensional Prognostic Index (MPI).
| Tool | Setting | Outcomes and Diseases | Study type | Number of participants | Main findings |
|---|---|---|---|---|---|
| MPI 8 domains 63 items | Hospital | All-cause mortality at 6-12 months | Prospective cohort study (Brunet et al., 2019; Bryant et al., 2019; De Luca et al., 2015; Pilotto et al., 2008) | 3,236 | MPI accurately stratifies the risk of 6- and 12-month mortality; MPI at admission and at discharge is equally predictive of 12-month mortality |
| All-cause mortality at 3-5 years | Prospective cohort study (Jung et al., 2016) | 1,109 | MPI stratifies the risk of 3- and 5-year mortality | ||
| In hospital mortality and length of stay | Multicenter prospective cohort studies (FIRI-SIGG Study Group (Pilotto et al., 2016c), MPI_TriVeneto Study Group (Volpato et al., 2015)) and single center prospective cohort study (De Luca et al., 2015) |
3,902 | MPI at admission is an independent predictor of in-hospital death and length of stay | ||
| MPI change during hospitalization | Multicenter prospective cohort study (MPI_TriVeneto Study Group) (Volpato et al., 2016) | 960 | MPI decreases for patients with short hospitalization (1-6 days) and tendes to increase for those with longer lenght of stay | ||
| Dementia | Prospective cohort study (Pilotto et al., 2009c) | 262 | MPI predicts 1-, 6-, and 12-month mortality in hospitalized elderly patients with dementia | ||
| Late-life depression | Prospective cohort study (Pilotto et al., 2012a) | 485 | MPI decreases after treatment with selective serotonin reuptake inhibitors in late-life major depressive disorder | ||
| Gastrointestinal bleeding | Prospective cohort studies (Pilotto et al., 2009a; Pilotto et al., 2007) | 127 | MPI predicts short- and long-term mortality in older patients with upper gastrointestinal bleeding; Greater accuracy than organ-specific prognostic indices (Rockall and Blatchford scores); MPI predicts the risk of 2-year mortality in elderly patients with upper gastrointestinal bleeding | ||
| Liver cirrhosis | Prospective cohort study (Pilotto et al., 2009a) | 154 | MPI predicts short- and long-term mortality in older patients with liver cirrhosis; Greater accuracy than Child-Plugh score | ||
| Femoral and hip fracture | Prospective cohort study (Musacchio et al., 2018; Sciume et al., 2018), retrospective cohort study (Ortho-MPI) (Vitale et al., 2014) | 422 | MPI predicts 6-month mortality among elderly patients with hip or neck femur fractures; MPI is an independent predictor of the waiting time to surgery in older patients with hip fracture | ||
| Chronic kidney disease | Prospective cohort study (Pilotto et al., 2012c), cross-sectional cohort study (Aucella et al., 2012) | 1,360 | Adding MPI to the estimated glomerular filtration rate (eGFR) improves the prediction of 2-year all-cause mortality in older patients with chronic kidney disease; Hemodialysis elderly patients have higher MPI scores compared to geriatric patients without renal failure | ||
| Pneumonia | Prospective cohort studies (Pilotto et al., 2009b, 2018b, 2018c) | 233 | MPI predicts mortality risk at 30 days, 6 months, and 12 months in older patients with community-acquired pneumonia; Greater accuracy than pneumonia severity index; Adding procalcitonin or proadrenomedullin levels to admission MPI increases the prognostic accuracy for 1-month mortality | ||
| Cardiovascular disease | Prospective cohort study (Carriere et al., 2018) | 216 (¾ 80 years old) | MPI independently predicts 1-year mortality in elderly patients with cardiovascular diseases; Adding serum creatinine and albumine to MPI increases the prognostic accuracy | ||
| Heart failure | Prospective cohort study (Pilotto et al., 2010) | 376 | MPI predicts 1-month mortality in older patients with heart failure; Greater accuracy compared to the New York Heart Association, the Enhanced Feedback for Effective Cardiac Treatment, and the Acute Decompensated Heart Failure National Registry regression model scores | ||
| Transient Ischmic Attack (TIA) | Prospective cohort study (Sancarlo et al., 2012) | 654 | MPI predicts 1-, 6-, and 12-month mortality in older patients hospitalized for TIA | ||
| Cancer | Prospective cohort study (Giantin et al., 2018) | 160 | MPI predicts 12-month mortality in elderly patients with locally-advanced or metastatic solid cancers | ||
| Peripheral artery disease | Two-center prospective cohort study (Drudi et al., 2019) | 148 | MPI does not predict mortality and worsening disability at 12 months after interventions for peripheral artery disease | ||
| Ambulatory care | Cognitive impairment and dementia | Cross-sectional cohort studies (Amanzio et al., 2017; D’Onofrio et al., 2016), prospective cohort studies (Coin et al., 2012; Gallucci et al., 2014), pilot single-blind randomized controlled clinical trial with rivastigmine (D’Onofrio et al., 2015) | 930 | MPI is associated with cognitive and behavioural domains, and impaired awareness for instrumental activities disabilities in people with cognitive deficits; Alzheimer’s disease (AD) patients with delusions have higher MPI scores compared to those without delusions; MPI increases over 12-month follow-up in elderly patients with untreated dementia and BMI ¼ 25 kg/m2; MPI predicts the risk of death and of hospitalizations in outpatients with cognitive impairment; Rivastigmine transdermal patch and cognitive stimulation in AD patients improve MPI at 6-month follow-up | |
| Type 2 diabetes mellitus | Multicenter cross-sectional cohort study (Metabolic Working Group) (Noale et al., 2016) | 1,342 | Diabetic elderly patients receiving polypharmacy (>5 medications/day) have higher MPI scores | ||
| Dysthyroidism | Prospective cohort study (Pasqualetti et al., 2018) | 643 | Reduction of FT3/FT4 ratio is associated with higher MPI scores | ||
| Cancer | Prospective cohort study (Onco-MPI) (Brunello et al., 2016) | 658 | Onco-MPI accurately predicts 1-year mortality in older cancer patients | ||
| Nursing home | Overweight and obese | Prospective cohort study (Pizzato et al., 2015) | 161 | People with BMI ¼ 25 kg/m2 and weight loss have the worst decline in the MPI over 1-year follow-up | |
| Community-dwelling | Survival at 12 years Days in hospital during 10 years | Prospective population-based study (SNAC-K study) (Angleman et al., 2015) | 2,472 | Higher MPI scores are associated with more days in hospital and with reduced survival, across different age groups | |
| Falls in older adults with knee osteoarthritis | Prospective cohort study (Osteoarthritis Initiative) (Veronese et al., 2019b) | 885 | Higher MPI scores are associated with increased risk of recurrent falls over 8-year follow-up | ||
| 8 domains 53 items | Hospital | All-cause mortality at 1-12 months | Prospective cohort study (Sancarlo et al., 2011) | 4,088 | MPI accurately stratifies the risk of 1- and 12-month mortality |
| 8 domains 53 items | In-hospital mortality All-cause mortality at 1 year Institutionalization at 1 year Access to homecare services at 1 year Re-hospitalization at 1 year | Multicenter prospective study (MPI_AGE) (Pilotto et al., 2019b) | 1,140 | Higher MPI scores are associated with higher risk of overall mortality, institutionalization, rehospitalization, and access to home care services during 12 months | |
| Geriatric syndromes and resources | Cross-sectional cohort study (Meyer et al., 2019) | 135 | Fewer geriatric syndromes and a higher number of geriatric resources are significantly correlated with lower MPI scores | ||
| Burden on healthcare resources and allocation at discharge | Prospective cohort study (Meyer et al., 2019a) | 135 | MPI is significantly related to grade of care and length of hospital stay; Patients with higher MPI scores are more often transferred from other hospital settings and less likely to be discharged home | ||
| Atrial fibrillation | International multicenter prospective cohort study (EUROSAF) (Quispe Guerrero et al., 2019) | 1,281 (study ongoing) | The use of oral anticoagulants seems to decrease the risk of death at 1 year compared to people not taking anticoagulants; The effect seems to be stronger in people with lower MPI | ||
| Patients undergoing transcatheter aortic valve implantation (TAVI) | Prospective cohort study (Bureau et al., 2017), international multicenter prospective registry (van Mourik et al., 2019) | 187 | MPI accurately predicts 6-, and 12-month mortality in elderly patients undergoing TAVI; MPI predicts the likelihood of combination of death and/or non-fatal stroke by 12 months after TAVI in elderly patients | ||
| Mortality risk associated with enteral tube feeding | Multicenter retrospective cohort study (Veronese et al., 2019a) | 1,064 | Patients with enteral tube feeding and higher MPI scores have higher 1-year mortality | ||
| General practice | Grade of care Hospitalization rate Mortality at 1 year Nursing home admission Use of home care services Falls Number of general practitioner contacts, of geriatric resources and geriatric syndromes |
Prospective cohort study (Meyer et al., 2019c) | 135 | MPI is strongly associated with adverse outcomes in older patients and predicts the number of general practitioner contacts over 1 year follow-up | |
| MPI-SVaMA 9 domains | Community-dwelling | All-cause mortality | Prospective cohort study (Pilotto et al., 2013) | 12,020 | MPI-SVaMA accurately stratifies the risk of 1- and 12-month mortality |
| Dementia | Multicenter retrospective cohort study (Pilotto et al., 2018) | 6,818 | Use of antidementia drugs is associated with reduced 2-year mortality in elderly patients with lower MPI-SVaMA scores | ||
| Type 2 diabetes mellitus | Multicenter retrospective cohort study (Pilotto et al., 2015) | 1,712 | Statin treatment is associated with reduced 3-year mortality independently of age and MPI-SVaMA in elderly patients with diabetes mellitus | ||
| Atrial fibrillation | Multicenter retrospective cohort study (Pilotto et al., 2016a) | 1,827 | Warfarin treatment is significantly associated with lower 2-year mortality in elderly patients with atrial fibrillation, irrespective of MPI-SVaMA group | ||
| Coronary artery disease | Multicenter retrospective cohort study (Pilotto et al., 2016b) | 2,597 | Statin treatment is associated with lower 3-year mortality risk in elderly patients with coronary artery disease, irrespective of age and MPI-SVaMA group | ||
| SELFY-MPI 8 domains Self-administered | Ambulatory care | Any disease | Cross-sectional cohort study (EFFICHRONIC) (Pilotto et al., 2019a) | 167 (¾18 years old) | SELFY-MPI shows high agreement with MPI irrespective of age groups |
| HIV + patients | Cross-sectional cohort study (Mora et al., 2019) | 50 | SELFY MPI (i.e. quality of life and cognitive functions) is associated with the laboratory exam’s parameter TCD4+ and viral load in senior HIV + patients | ||
| Community-dwelling | Any disease | Multicenter cohort study EFFICHRONIC (Zora et al., 2019) | 310 (>18 years old) | SELFY-MPI shows a very good feasibility demonstrating potential usefulness both as a screening and an outcome measure tool |
This instrument has been applied in several cohorts of older adults with specific acute and chronic diseases, showing always excellent calibration, reproducibility and accuracy in stratifying population according the risk of short and long-term mortality (Dent et al., 2016; Yourman et al., 2012).
Evidence derived from many multicenter studies demonstrated that MPI is (Table 2): 1) significantly more accurate in predicting mortality compared to frailty indexes based on both phenotypic model and multiple-deficits model at 32 and 70 items (Pilotto et al., 2012); 2) sensitive to changes of health and functional status during hospitalization (Volpato et al., 2016) and antidepressant treatments in outpatients (Pilotto et al., 2012a); 3) able to predict in-hospital length of stay for equal diagnosis (Volpato et al., 2015); 4) able to identify hospitalized elderly subjects who access homecare services, are institutionalized and/or re-hospitalized within one year from discharge (Pilotto et al., 2019b); 5) able to predict burden on healthcare resources and more problematic discharge allocation (Meyer et al., 2019a). All these data suggest that MPI is an excellent diagnostic tool in terms of validity, reliability and feasibility for the management of older persons in clinical practice (Warnier et al., 2016).
8. Comprehensive Geriatric Assessment, prognosis and clinical strategies in elders
Recently, the international project MPI_AGE, cofounded by European Union, explored in deep the role of the CGA, and the derived MPI, as tool for guiding clinical decisions in vulnerable older adults with multimorbidity. Noteworthy, several clinical studies evaluated the appropriateness of few “critical” treatments in geriatric setting, like statin use in secondary prevention among people with diabetes mellitus (Pilotto et al., 2015) or with coronary artery disease (Pilotto et al., 2016b), anticoagulants in atrial fibrillation (Pilotto et al., 2016a), antidementia drugs in late-life cognitive impairment (Pilotto et al., 2018) or transcatheter aortic valve implantation (TAVI) in elderly patients with aortic stenosis (Bureau et al., 2017; van Mourik et al., 2019) and enteral tube feeding intervention in malnourished hospitalized older patients (Veronese et al., 2019a). Finally, recent literature has shown the use of the MPI could also extend to specific fields for personalized therapies such as for guiding immunotherapy in older patients with advanced malignancies (Sbrana et al., 2019) or in helping physicians in giving oral anticoagulants in older patients with non-valvular atrial fibrillation (Veronese et al., 2018a). Promising findings from these studies showed that in older adults the multidimensional approach warrants better clinical decisions (i.e. to treat or not to treat) depending on degree of multidimensional impairment of the subject (Pilotto et al., 2018a).
9. Prevention and treatment of frailty
In the English Longitudinal Study of Ageing, the Authors found a stepwise increase of frailty condition over time with greater prevalence in women compared to men. The analysis on 4638 respondents 65–89 years, followed-up every four years between 2004 and 2012, identified the following factors as potential predictors of future frailty: 1 chronic disease, 2 allostatic load based on measurement of nine biological and clinical biomarkers including blood pressure, anthropometric measurements, and blood tests for cholesterol levels, glucose control, and inflammatory markers, 3 low physical activity, 4 cognitive impairment and depressive symptoms, 5 poor social support (Ding et al., 2017).
These findings remark the need for health and socio-economic policies on preventive interventions targeting, in general population, these conditions that are highly relevant and potentially reversible predisposing factors to frailty. For example, it is now widely established, that physical activity not only is related to reduced physical frailty, but also improves physical performance in pre-frail subjects and in those at risk for sarcopenia (Piercy et al., 2018).
Also polypharmacy, namely the treatment with five or more medications daily, has been associated with higher frailty risk in elderly subjects (Veronese et al., 2017c). Deprescribing interventions, in accordance with well-accepted criteria, could reduce potentially inappropriate medications and adverse drug events, optimizing management of frailty condition (Maclagan et al., 2017).
Growing evidence show a strict relationship between higher adherence to healthy diet, in particular Mediterranean diet, and lower incidence of frailty (Kojima et al., 2018; Veronese et al., 2018b). To support the multidimensional concept of frailty, however, in the “FRAIL” project, a prospective study carried out in older adults living in Genoa (the city with the highest ageing index in Europe), a lower prevalence of frailty was associated with higher quality of protein intake with diet (Cella et al., 2019), more physical activity, better economic conditions and higher levels of cultural fruition that, engaging in social and cultural events, fosters the growth of cultural interests, and social and affective interactions (Poli et al., 2017). All these finding suggest that the adoption of healthy lifestyle since youth and adulthood might help to prevent (and maybe to treat) frailty in older adults.
10. Future perspective
To date, identification, treatment and prevention of frailty represent a major challenge of geriatric science. Because of its multidimensionality, it is not surprising that frailty is not only a powerful risk factor for mortality but also profoundly affects response, effectiveness and tolerance to medical and surgical treatment and negatively influences quality of life (Hoogendijk et al., 2019; Kojima et al., 2016; Saum et al., 2014). Although specific tools for the assessment of frailty have been developed and validated, their clinical use is lingering because of their complexity and because their effectiveness in guiding a successful care plan is limited (Walston et al., 2019). Given the widespread application of the multidimensional approach in clinical practice, we suggest that at this stage CGA could be used to identify “frailty” and use this information to improve the overall management of frail older adults. It is possible that in future new, more effective tools may be developed and their efficacy in the specific management of frailty can be demonstrated. Until then, CGA is a valid alternative.
Acknowledgments
Funding source
This work was supported by the MPI_AGE European project cofunded by the Consumers, Health, Agriculture, and Food Executive Agency (CHAFEA) in the frame of the European Innovation Partnership on Active and Healthy Ageing Second Health Programme 2008-2013. The contents of this article are the sole responsibility of the above mentioned authors and can under no circumstances be regarded as reflecting the position of the European Union. The funding agencies had no role in design or conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The study was based on administrative data sets, and the participants were not identifiable to the authors.
Footnotes
Declaration of Competing Interest
None to declare.
References
- Amanzio M, Palermo S, Zucca M, Rosato R, Rubino E, Leotta D, Bartoli M, Rainero I, 2017. Neuropsychological correlates of pre-frailty in neurocognitive disorders: a possible role for metacognitive dysfunction and mood changes. Front. Med. (Lausanne) 4, 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angleman SB, Santoni G, Pilotto A, Fratiglioni L, Welmer AK, 2015. Multidimensional prognostic index in association with future mortality and number of hospital days in a population-based sample of older adults: results of the EU funded MPI_AGE project. PLoS One 10, eOl 33789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aucella F, Stoico L, Cicchella A, Gesuete A, Greco A, Grandaliano G, Pilotto A, 2012. Comprehensive geriatric assessment in the hemodialysis elderly population. J. Nephrol 25 (Suppl 19), S85–89. [DOI] [PubMed] [Google Scholar]
- Brunello A, Fontana A, Zafferri V, Panza F, Fiduccia P, Basso U, Copetti M, Lonardi S, Roma A, Falci C, Monfardini S, Celia A, Pilotto A, Zagonel V, 2016. Development of an oncological-multidimensional prognostic index (Onco-MPI) for mortality prediction in older cancer patients. J. Cancer Res. Clin. Oncol 142, 1069–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet T, Bureau ML, Caupenne A, Liuu E, Saulnier PJ, Gand E, Paccalin M, 2019. Interest of the multidimensional prognostic index (MPI) as an assessment tool in hospitalized patients in geriatrics. Geriatr. Psychol. Neuropsychiatr. Vieil 17, 386–392. [DOI] [PubMed] [Google Scholar]
- Bryant K, Sorich MJ, Woodman RJ, Mangoni AA, 2019. Validation and adaptation of the multidimensional prognostic index in an older Australian cohort. J. Clin. Med 8, 11 10.3390/jcm8111820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau ML, Liuu E, Christiaens L, Pilotto A, Mergy J, Bellarbre F, Ingrand P, Paccalin M, 2017. Using a multidimensional prognostic index (MPI) based on comprehensive geriatric assessment (CGA) to predict mortality in elderly undergoing transcatheter aortic valve implantation. Int. J. Cardiol 236, 381–386. [DOI] [PubMed] [Google Scholar]
- Calder PC, Bosco N, Bourdet-Sicard R, Capuron L, Delzenne N, Dore J, Franceschi C, Lehtinen MJ, Recker T, Salvioli S, Visioli F, 2017. Health relevance of the modification of low grade inflammation in ageing (inflammageing) and the role of nutrition. Ageing Res. Rev 40, 95–119. [DOI] [PubMed] [Google Scholar]
- Carriere C, Stolfo D, Baglio V, Gerloni R, Merlo M, Barbati G, Cannata A, Biolo G, Sinagra G, 2018. Outcome of the multidimensional prognostic index in ultra-octogenarian patients hospitalized for cardiovascular diseases. J. Cardiovasc. Med. (Hagerstown) 19, 536–545. [DOI] [PubMed] [Google Scholar]
- Celia A, Veronese N, Poll S, Custureri R, Delrio A, Musacchio C, Mello AM, Tavella E, Velio N, Zigoura E, Pilotto A, 2019. Higher animal-derived dietary protein intake is associated with lower prevalence of frailty. Intern J Gerontol 13, 121–124. [Google Scholar]
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K, 2013. Frailty in elderly people. Lancet 381, 752–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clegg A, Rogers L, Young J, 2015. Diagnostic test accuracy of simple instruments for identifying frailty in community-dwelling older people: a systematic review. Age Ageing 44, 148–152. [DOI] [PubMed] [Google Scholar]
- Coin A, Bolzetta F, De Rui M, Veronese N, Granziera S, Girardi A, Manzato E, Sergi G, 2012. Nutritional and global indexes of progression in dementia: a 12-month prospective study. Am. J. Alzheimers Dis. Other Demen 27, 504–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collard RM, Boter H, Schoevers RA, Oude Voshaar RC, 2012. Prevalence of frailty in community-dwelling older persons: a systematic review. J. Am. Geriatr. Soc 60, 1487–1492. [DOI] [PubMed] [Google Scholar]
- Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, 2019. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha AIL, Veronese N, de Melo Borges S, Ricci NA, 2019. Frailty as a predictor of adverse outcomes in hospitalized older adults: a systematic review and meta-analysis. Ageing Res. Rev 56, 100960. [DOI] [PubMed] [Google Scholar]
- Custodero C, Mankowski RT, Lee SA, Chen Z, Wu S, Manini TM, Hincapie Echeverri J, Sabba C, Beavers DP, Cauley JA, Espeland MA, Fielding RA, Kritchevsky SB, Liu CK, McDermott MM, Miller ME, Tracy RP, Newman AB, Ambrosius WT, Pahor M, Anton SD, 2018. Evidence-based nutritional and pharmacological interventions targeting chronic low-grade inflammation in middle-age and older adults: a systematic review and meta-analysis. Ageing Res. Rev 46, 42–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G, Sancarlo D, Addante F, Ciccone F, Cascavilla L, Paris F, Elia AC, Nuzzaci C, Picoco M, Greco A, Panza F, Pilotto A, 2015. A pilot randomized controlled trial evaluating an integrated treatment of rivastigmine transdermal patch and cognitive stimulation in patients with Alzheimer’s disease. Int. J. Geriatr. Psychiatry 30, 965–975. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G, Panza F, Sancarlo D, Paris FF, Cascavilla L, Mangiacotti A, Lauriola M, Paroni GH, Seripa D, Greco A, 2016. Delusions in patients with Alzheimer’s disease: a multidimensional approach. J. Alzheimers Dis 51, 427–437. [DOI] [PubMed] [Google Scholar]
- De Luca E, Perissinotto E, Fabris L, Pengo V, Zurlo A, De Toni P, De Zaiacomo F, Manzato E, Giantin V, 2015. Short- and longer-term predictive capacity of the multidimensional prognostic index: the timing of the assessment is of no consequence. Arch. Gerontol. Geriatr 61, 458–463. [DOI] [PubMed] [Google Scholar]
- Dent E, Kowal P, Hoogendijk EO, 2016. Frailty measurement in research and clinical practice: a review. Eur. J. Intern. Med 31, 3–10. [DOI] [PubMed] [Google Scholar]
- Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD, 2019. Management of frailty: opportunities, challenges, and future directions. Lancet 394, 1376–1386. [DOI] [PubMed] [Google Scholar]
- Ding YY, Kuha J, Murphy M, 2017. Multidimensional predictors of physical frailty in older people: identifying how and for whom they exert their effects. Biogerontology 18, 237–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drudi LM, Ades M, Mancini R, Boudrias C, Obrand DI, Steinmetz OK, Afilalo J, 2019. Frailty assessment in older adults undergoing interventions for peripheral arterial disease. J. Vase. Surg 70, 1594–1602. [DOI] [PubMed] [Google Scholar]
- European Medicines Agency. Committee for Medicinal Products for Human Use, 2018. Reflection Paper on Physical Frailty: Instruments for Baseline Characterization of Older Populations in Clinical Trials. [Google Scholar]
- Ferrucci L, Fabbri E, 2018. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol 15, 505–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrucci L, Fabbri E, Walston JD, 2017. Frailty, Hazzard’s Geriatric Medicine and Gerontology, 7^ edition. McGraw Hill Education, pp. 691–708. [Google Scholar]
- Fontana L, Addante F, Copetti M, Paroni G, Fontana A, Sancarlo D, Pellegrini F, Ferrucci L, Pilotto A, 2013. Identification of a metabolic signature for multidimensional impairment and mortality risk in hospitalized older patients. Aging Cell 12, 459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franceschi C, Garagnani P, Morsiani C, Conte M, Santoro A, Grignolio A, Monti D, Capri M, Salvioli S, 2018. The continuum of aging and age-related diseases: common mechanisms but different rates. Front. Med. (Lausanne) 5, 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research, G, 2001. Frailty in older adults: evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci 56, Ml46–156. [DOI] [PubMed] [Google Scholar]
- Gallucci M, Battistella G, Bergamelli C, Spagnolo P, Mazzuco S, Carlini A, Di Giorgi E, Boldrini P, Pilotto A, 2014. Multidimensional prognostic index in a cognitive impairment outpatient setting: mortality and hospitalizations. The Treviso Dementia (TREDEM) study. J. Alzheimers Dis 42, 1461–1468. [DOI] [PubMed] [Google Scholar]
- Giantin V, Falci C, De Luca E, Valentini E, Iasevoli M, Siviero P, Maggi S, Martella B, Crepaldi G, Monfardini S, Manzato E, 2018. Performance of the Multidimensional Geriatric Assessment and Multidimensional Prognostic Index in predicting negative outcomes in older adults with cancer. Eur. J. Cancer Care (Engl) 27. [DOI] [PubMed] [Google Scholar]
- Hajek A, Bock J-O, Saum K-U, Matschinger H, Brenner H, Holleczek B, Haefeli WE, Heider D, Konig H-H, 2017. Frailty and healthcare costs—longitudinal results of a prospective cohort study. Age Ageing 47, 233–241. [DOI] [PubMed] [Google Scholar]
- Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP, 2019. Frailty: implications for clinical practice and public health. Lancet 394, 1365–1375. [DOI] [PubMed] [Google Scholar]
- Jung HW, Kim JW, Han JW, Kim K, Kim JH, Kim KI, Kim CH, Kim KW, 2016. Multidimensional geriatric prognostic index, based on a geriatric assessment, for long-term survival in older adults in Korea. PLoS One 11, e0147032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kojima G, Avgerinou C, Iliffe S, Walters K, 2018. Adherence to mediterranean diet reduces incident frailty risk: systematic review and meta-analysis. J. Am. Geriatr. Soc 66, 783–788. [DOI] [PubMed] [Google Scholar]
- Kojima G, Iliffe S, Jivraj S, Walters K, 2016. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J. Epidemiol. Community Health 70, 716–721. [DOI] [PubMed] [Google Scholar]
- Maclagan LC, Maxwell CJ, Gandhi S, Guan J, Bell CM, Hogan DB, Daneman N, Gill SS, Morris AM, Jeffs L, Campitelli MA, Seitz DP, Bronskill SE, 2017. Frailty and potentially inappropriate medication use at nursing home transition. J. Am. Geriatr. Soc 65, 2205–2212. [DOI] [PubMed] [Google Scholar]
- Meyer AM, Becker I, Siri G, Brinkkotter PT, Benzing T, Pilotto A, Polidori MC, 2019a. New associations of the multidimensional prognostic index. Z. Gerontol. Geriatr 52, 460–467. [DOI] [PubMed] [Google Scholar]
- Meyer AM, Becker I, Siri G, Brinkkotter PT, Benzing T, Pilotto A, Polidori MC, 2019. The prognostic significance of geriatric syndromes and resources. Aging Clin. Exp. Res 32, 115–124. [DOI] [PubMed] [Google Scholar]
- Meyer AM, Siri G, Becker I, Betz T, Bodecker AW, Robertz JW, Krause O, Benzing T, Pilotto A, Polidori MC, 2019c. The multidimensional prognostic index in general practice: one-year follow-up study. Int. J. Clin. Pract, el 3403. [DOI] [PubMed] [Google Scholar]
- Mora S, Venturini A, Cenderello G, Fiorellino D, Pilotto A, Giacomini M, 2019. A web-based tool for a complete evaluation of fragility in senior hiv + patients. Stud. Health Technol. Inform 261, 299–302. [PubMed] [Google Scholar]
- Musacchio C, Razzano M, Raiteri R, Del Rio A, Torriglia D, Stella M, Barone A, Puntoni M, Siri G, Pilotto A, 2018. Time to surgery and Multidimensional Prognostic Index (MPI) in older patients with hip fracture. Eur. Geriatr. Med 9, S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noale M, Veronese N, Cavallo Perin P, Pilotto A, Tiengo A, Crepaldi G, Maggi S, 2016. Polypharmacy in elderly patients with type 2 diabetes receiving oral anti-diabetic treatment. Acta Diabetol. 53, 323–330. [DOI] [PubMed] [Google Scholar]
- Pasqualetti G, Calsolaro V, Bernardini S, Linsalata G, Bigazzi R, Caraccio N, Monzani F, 2018. Degree of peripheral thyroxin deiodination, frailty, and long-term survival in hospitalized older patients. J. Clin. Endocrinol. Metab 103, 1867–1876. [DOI] [PubMed] [Google Scholar]
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD, 2018. The physical activity guidelines for Americans. JAMA 320, 2020–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Ferrucci L, Scarcelli C, Niro V, Di Mario F, Seripa D, Andriulli A, Leandro G, Franceschi M, 2007. Usefulness of the comprehensive geriatric assessment in older patients with upper gastrointestinal bleeding: a two-year follow-up study. Dig. Dis 25, 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Ferrucci L, Franceschi M, D’Ambrosio LP, Scarcelli C, Cascavilla L, Paris F, Placentino G, Seripa D, Dallapiccola B, Leandro G, 2008. Development and validation of a multidimensional prognostic index for one-year mortality from comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res. 11, 151–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Addante F, DOnofrio G, Sancarlo D, Ferrucci L, 2009a. The Comprehensive Geriatric Assessment and the multidimensional approach. A new look at the older patient with gastroenterological disorders. Best Pract. Res. Clin. Gastroenterol 23, 829–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Addante F, Ferrucci L, Leandro G, DOnofrio G, Corritore M, Niro V, Scarcelli C, Dallapiccola B, Franceschi M, 2009b. The multidimensional prognostic index predicts short- and long-term mortality in hospitalized geriatric patients with pneumonia. J. Gerontol. A Biol. Sci. Med. Sci 64, 880–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Sancarlo D, Panza F, Paris F, DOnofrio G, Cascavilla L, Addante F, Seripa D, Solfrizzi V, Dallapiccola B, Franceschi M, Ferrucci L, 2009c. The Multidimensional Prognostic Index (MPI), based on a comprehensive geriatric assessment predicts short- and long-term mortality in hospitalized older patients with dementia. J. Alzheimers Dis 18, 191–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Addante F, Franceschi M, Leandro G, Rengo G, D’Ambrosio P, Longo MG, Rengo F, Pellegrini F, Dallapiccola B, Ferrucci L, 2010. Multidimensional Prognostic Index based on a comprehensive geriatric assessment predicts short-term mortality in older patients with heart failure. Circ. Heart Fail 3, 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, D’Onofrio G, Panza F, Copetti M, Cascavilla L, Paris F, Pellegrini F, Seripa D, Ferrucci L, 2012a. Treatment of late-life major depressive disorder with selective serotonin reuptake inhibitors improves the multidimensional prognostic index. J. Clin. Psychopharmacol 32, 726–729. [DOI] [PubMed] [Google Scholar]
- Pilotto A, Polidori MC, Veronese N, Panza F, Arboretti Giancristofaro R, Pilotto A, Daragjati J, Carrozzo E, Prete C, Gallina P, Padovani A, Maggi S, 2018. Association of Antidementia Drugs and Mortality in Community-Dwelling Frail Older Patients With Dementia: The Role of Mortality Risk Assessment. J. Am. Med. Dir. Assoc 19, 162–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Rengo F, Marchionni N, Sancarlo D, Fontana A,, Panza F., Ferrucci L, 2012. Comparing the prognostic accuracy for all-cause mortality of frailty instruments: a multicentre 1-year follow-up in hospitalized older patients. PLoS One 7, e29090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Sancarlo D, Aucella F, Fontana A, Addante F, Copetti M, Panza F, Strippoli GF, Ferrucci L, 2012c. Addition of the multidimensional prognostic index to the estimated glomerular filtration rate improves prediction of long-term all-cause mortality in older patients with chronic kidney disease. Rejuvenation Res. 15, 82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Gallina P, Copetti M, Pilotto A, Marcato F, Mello AM, Simonato M, Logroscino G, Padovani A, Ferrucci L, Panza F, 2016a. Warfarin treatment and all-cause mortality in community-dwelling older adults with atrial fibrillation: a retrospective observational study. J. Am. Geriatr. Soc 64, 1416–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Gallina P, Fontana A, Sancarlo D, Bazzano S, Copetti M, Maggi S, Paroni G, Marcato F, Pellegrini F, Donato D, Ferrucci L, 2013. Development and validation of a Multidimensional Prognostic Index for mortality based on a standardized Multidimensional Assessment schedule (MPI-SVaMA) in community-dwelling older subjects. J. Am. Med. Dir. Assoc 14, 287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Gallina P, Panza F, Copetti M, Celia A, Cruz-Jentoft A, Daragjati J, Ferrucci L, Maggi S, Mattace-Raso F, Paccalin M, Polidori MC, Topinkova E, Trifiro G, Welmer AK, Strandberg T, Marchionni N, 2016b. Relation of statin use and mortality in community-dwelling frail older patients with coronary artery disease. Am. J. Cardiol 118, 1624–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Panza F, Copetti M, Simonato M, Sancarlo D, Gallina P, Strandberg T, 2015. Statin treatment and mortality in community-dwelling frail older patients with diabetes mellitus: a retrospective observational study. PLoS One 10, eOl 30946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Celia A, Pilotto A, Daragjati J, Veronese N, Musacchio C, Mello AM, Logroscino G, Padovani A, Prete C, Panza F, 2017. Three decades of comprehensive geriatric assessment: evidence coming from different healthcare settings and specific clinical conditions. J. Am. Med. Dir. Assoc 18 (192) el 91–192 el 11. [DOI] [PubMed] [Google Scholar]
- Pilotto A, Daragjati J, Veronese N, 2018a. CGA and clinical decision-making the multidimensional prognostic index In: Pilotto A, Martin FC (Eds.), Comprehensive Geriatric Assessment. Springer International, pp. 79–92. [Google Scholar]
- Pilotto A, Dini S, Daragjati J, Miolo M, Mion MM, Fontana A, Storto ML, Zaninotto M, Celia A, Carraro P, Addante F, Copetti M, Plebani M, 2018b. Combined use of the multidimensional prognostic index (MPI) and procalcitonin serum levels in predicting 1-month mortality risk in older patients hospitalized with community-acquired pneumonia (CAP): a prospective study. Aging Clin. Exp. Res 30, 193–197. [DOI] [PubMed] [Google Scholar]
- Pilotto A, Dini S, Veronese N, Daragjati J, Miolo M, Mion MM, Fontana A, Lo Storto M, Zaninotto M, Bragato G, Celia A, Carraro P, Addante F, Copetti M, Plebani M, 2018c. Multidimensional Prognostic Index and pro-adrenomedullin plasma levels as mortality risk predictors in older patients hospitalized with community-acquired pneumonia: a prospective study. Panminerva Med. 60, 80–85. [DOI] [PubMed] [Google Scholar]
- Pilotto A, Sancarlo D, Pellegrini F, Rengo F, Marchionni N, Volpato S, Ferrucci L, 2016c. The Multidimensional Prognostic Index predicts in-hospital length of stay in older patients: a multicentre prospective study. Age Ageing 45, 90–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Veronese N, Daragjati J, Cruz-Jentoft AJ, Polidori MC, Mattace-Raso F, Paccalin M, Topinkova E, Siri G, Greco A, Mangoni AA, Maggi S, Ferrucci L, 2019b. Using the multidimensional prognostic index to predict clinical outcomes of hospitalized older persons: a prospective, multicentre, international study. J. Gerontol. A Biol. Sci. Med. Sci 74 (10), 1643–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilotto A, Veronese N, Quispe Guerrero KL, Zora S, Boone ALD, Puntoni M, Giorgeschi A, Celia A, Rey Hidalgo I, Pers YM, Ferri A, Fernandez JRH, Pisano Gonzalez M, 2019a. Development and validation of a self-administered multidimensional prognostic index to predict negative health outcomes in community-dwelling persons. Rejuvenation Res. 22, 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzato S, Sergi G, Bolzetta F, De Rui M, De Ronch I, Carraro S, Berton L, Orr E, Imoscopi A, Perissinotto E, Coin A, Manzato E, Veronese N, 2015. Effect of weight loss on mortality in overweight and obese nursing home residents during a 5-year follow-up. Eur. J. Clin. Nutr 69, 1113–1118. [DOI] [PubMed] [Google Scholar]
- Poli S, Celia A, Puntoni M, Musacchio C, Pomata M, Torriglia D, Velio N, Molinari B, Pandolfini V, Torrigiani C, Pilotto A, 2017. Frailty Is associated with socioeconomic and lifestyle factors in community-dwelling older subjects. Aging Clin. Exp. Res 29, 721–728. [DOI] [PubMed] [Google Scholar]
- Quispe Guerrero KL, Veronese N, Argusti A, Ferri A, Maggi S, Strandberg T, Polidori MC, Pilotto A, 2019. The European Study of older Subjects with Atrial Fibrillation (EUROSAF): preliminary data on anticoagulant prescription in frail older patients. Geriatr. Care 5, SI8–19. [Google Scholar]
- Rockwood K, Mitnitski A, 2007. Frailty in relation to the accumulation of deficits. J. Gerontol. A Biol. Sci. Med. Sci 62, 722–727. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Manas L, Feart C, Mann G, Vina J, Chatterji S, Chodzko-Zajko W, Gonzalez-Colaco Harmand M, Bergman H, Carcaillon L, Nicholson C, Scuteri A, Sinclair A, Pelaez M, Van der Cammen T, Beland F, Bickenbach J, Delamarche P, Ferrucci L, Fried LP, Gutierrez-Robledo LM, Rockwood K, Rodriguez Artalejo F, Serviddio G, Vega E, 2013. Searching for an operational definition of frailty: a Delphi method based consensus statement: the frailty operative definition-consensus conference project. J. Gerontol. A Biol. Sci. Med. Sci 68, 62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancarlo D, DOnofrio G, Franceschi M, Scarcelli C, Niro V, Addante F, Copetti M, Ferrucci L, Fontana L, Pilotto A, 2011. Validation of a Modified-Multidimensional Prognostic Index (m-MPI) including the Mini Nutritional Assessment Short-Form (MNA-SF) for the prediction of one-year mortality in hospitalized elderly patients. J. Nutr. Health Aging 15, 169–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancarlo D, Pilotto A, Panza F, Copetti M, Longo MG, D’Ambrosio P, DOnofrio G, Ferrucci L, Pilotto A, 2012. A Multidimensional Prognostic Index (MPI) based on a comprehensive geriatric assessment predicts short- and long-term all-cause mortality in older hospitalized patients with transient ischemic attack. J. Neurol 259, 670–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saum KU, Dieffenbach AK, Muller H, Holleczek B, Hauer K, Brenner H, 2014. Frailty prevalence and 10-year survival in community-dwelling older adults: results from the ESTHER cohort study. Eur. J. Epidemiol 29, 171–179. [DOI] [PubMed] [Google Scholar]
- Sbrana A, Antognoli R, Pasqualetti G, Linsalata G, Okoye C, Calsolaro V, Paolieri F, Bloise F, Ricci S, Antonuzzo A, 2019. Effectiveness of Multi-Prognostic Index in older patients with advanced malignancies treated with immunotherapy. J. Geriatr. Oncol, 10.1016/j.jgp.2019.09.010. [DOI] [PubMed] [Google Scholar]
- Sciume L, Rebagliati GAA, Iannello P, Mottini A, Alessandro A, Caserta AV, Gattoronchieri V, Panella L, 2018. Rehabilitation after urgent or elective orthopedic surgery: the role of resilience in elderly patients. Rehabil. Nurs 43, 267–274. [DOI] [PubMed] [Google Scholar]
- Soysal P, Veronese N, Thompson T, Kahl KG, Fernandes BS, Prina AM, Solmi M, Schofield P, Koyanagi A, Tseng PT, Lin PY, Chu CS, Cosco TD, Cesari M, Carvalho AF, Stubbs B, 2017. Relationship between depression and frailty in older adults: a systematic review and meta-analysis. Ageing Res. Rev 36, 78–87. [DOI] [PubMed] [Google Scholar]
- Turner G, Clegg A, British Geriatrics S, Age UK, Royal College of General, P, 2014. Best practice guidelines for the management of frailty: a British geriatrics society, age UK and royal college of general practitioners report. Age Ageing 43, 744–747. [DOI] [PubMed] [Google Scholar]
- van Mourik MS, van der Velde N, Mannarino G, Thibodeau MP, Masson JB, Santoro G, Baan J, Jansen S, Kurucova J, Thoenes M, Deutsch C, Schoenenberger AW, Ungar A, Bramlage P, Vis MM, 2019. Value of a comprehensive geriatric assessment for predicting one-year outcomes in patients undergoing transcatheter aortic valve implantation: results from the CGA-TAVI multicentre registry. J. Geriatr. Cardiol 16, 468–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Cereda E, Stubbs B, Solmi M, Luehini C, Manzato E, Sergi G, Manu P, Harris T, Fontana L, Strandberg T, Amieva H, Dumurgier J, Elbaz A, Tzourio C, Eicholzer M, Rohrmann S, Moretti C, D’Ascenzo F, Quadri G, Polidoro A, Lourengo RA, Moreira VG, Sanehis J, Scotti V, Maggi S, Correll CU, 2017a. Risk of cardiovascular disease morbidity and mortality in frail and pre-frail older adults: results from a meta-analysis and exploratory meta-regression analysis. Ageing Res. Rev 35, 63–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Noale M, Solmi M, Pilotto A, Vaona A, Demurtas J, Mueller C, Huntley J, Crepaldi G, Maggi S, 2017c. Polypharmacy is associated with higher frailty risk in older people: an 8-Year longitudinal cohort study. J. Am. Med. Dir. Assoc 18, 624–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Argusti A, Canepa E, Polidori MC, Maggi S, Strandberg T, Pilotto A, 2018a. Evaluating the effectiveness and risks of oral anticoagulant treatments in multimorbid frail older subjects with atrial fibrillation using the multidimensional prognostic index: the EURopean study of older subjects with atrial fibrillation—EUROSAF. Eur. Geriatr. Med 9, 149–154. [DOI] [PubMed] [Google Scholar]
- Veronese N, Stubbs B, Noale M, Solmi M, Rizzoli R, Vaona A, Demurtas J, Crepaldi G, Maggi S, 2018b. Adherence to a Mediterranean diet is associated with lower incidence of frailty: a longitudinal cohort study. Clin. Nutr 37, 1492–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Celia A, Cruz-Jentoft AJ, Polidori MC, Mattace-Raso F, Paccalin M, Topinkova E, Greco A, Mangoni AA, Daragjati J, Siri G, Pilotto A, 2019a. Enteral tube feeding and mortality in hospitalized older patients: a multicenter longitudinal study. Clin. Nutr 10.1016/j.clnu.2019.07.011. [DOI] [PubMed] [Google Scholar]
- Veronese N, Siri G, Celia A, Maggi S, Zigoura E, Puntoni M, Smith L, Musacchio C, Barone A, Sabba C, Vallone F, Pilotto A, 2019b. The multidimensional prognostic index predicts falls in older people: an 8-Year longitudinal cohort study of the osteoarthritis initiative. J. Am. Med. Dir. Assoc 10.1016/j.jamda.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitale E, Notarnicola A, Tafuri S, Vicenti G, Cassano M, Moretti B, 2014. Orthopedic Multidimensional Prognostic Index (Ortho-MPI) in the elderly with hip or neck femur fracture: a pilot study. Arch. Gerontol. Geriatr 58, 101–104. [DOI] [PubMed] [Google Scholar]
- Volpato S, Bazzano S, Fontana A, Ferrucci L, Pilotto A, 2015. Multidimensional Prognostic Index predicts mortality and length of stay during hospitalization in the older patients: a multicenter prospective study. J. Gerontol. A Biol. Sci. Med. Sci 70, 325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpato S, Daragjati J, Simonato M, Fontana A, Ferrucci L, Pilotto A, 2016. Change in the multidimensional prognostic index score during hospitalization in older patients. Rejuvenation Res 19, 244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walston J, Bandeen-Roche K, Buta B, Bergman H, Gill TM, Morley JE, Fried LP, Robinson TN, Afilalo J, Newman AB, Lopez-Otin C, De Cabo R, Theou O, Studenski S, Cohen HJ, Ferrucci L, 2019. Moving frailty toward clinical practice: NIA intramural frailty science symposium summary. J. Am. Geriatr. Soc 67, 1559–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warmer RM, van Rossum E, van Velthuijsen E, Mulder WJ, Schols JM, Kempen GI, 2016. Validity, reliability and feasibility of tools to identify frail older patients in inpatient hospital care: a systematic review. J. Nutr. Health Aging 20, 218–230. [DOI] [PubMed] [Google Scholar]
- Wilson D, Jackson T, Sapey E, Lord JM, 2017. Frailty and sarcopenia: the potential role of an aged immune system. Ageing Res. Rev 36, 1–10. [DOI] [PubMed] [Google Scholar]
- Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK, 2012. Prognostic indices for older adults: a systematic review. JAMA 307, 182–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zora S, Quispe Guerrero KL, Veronese N, Ferri A, Boone ALD, Pisano Gonzalez M, Pers YM, Raat H, Baker G, Celia A, Pilotto A, on behalf of EFFICHRONIC Investigators, 2019. Implementation of the SELFY-MPI in five European Countries: a multicenter international feasibility study. Geriatr. Care 5, S23–24. [Google Scholar]


