Abstract
The objective of social distancing is to slow the rate of viral transmission and thereby spread out the incidence of coronavirus disease 2019 (COVID-19) cases over time (i.e., flattening the curve) so that a surge of patients will not overwhelm the capacity of the healthcare system. Given this objective, the specific curve that requires flattening is that of COVID-19-associated hospitalizations. In this context, we evaluated the rates of COVID-19-associated hospitalization in British Columbia (BC) and Ontario to see if either province shows evidence of flattening the relevant curve. From late March to mid-June 2020, the cumulative rate of COVID-19-associated hospitalization in BC has indeed shown evidence of flattening, whereas that in Ontario has increased linearly. The cumulative hospitalization rate in Ontario first surpassed that of BC on April 14. By June 18, the respective hospitalization rates per 100,000 population were 27.86 for Ontario and 9.96 for BC. In both provinces, the cumulative hospitalization rate has remained lower than that of comparator US states. In conclusion, there is evidence of flattening the relevant curve in BC but not yet in Ontario. The comparison with BC underscores the need for continued caution with the relaxation of social distancing efforts in Ontario.
Keywords: Coronavirus disease 2019, Pandemic, Social distancing, Public health
Résumé
L’objectif de la distanciation sociale est de ralentir le taux de transmission virale et donc d’étaler dans le temps l’incidence des cas de maladie à coronavirus 2019 (COVID-19) (autrement dit d’aplatir la courbe), de sorte que la quantité de patients à soigner ne dépasse pas la capacité du système de santé. Compte tenu de cet objectif, la courbe qui doit être aplatie est celle des hospitalisations associées à la COVID-19. Dans ce contexte, nous avons évalué les taux d’hospitalisation associés à la COVID-19 en Colombie-Britannique et en Ontario pour voir si l’une ou l’autre de ces provinces montre des signes d’aplatissement de cette courbe. De la fin mars à la mi-juin 2020, le taux cumulé d’hospitalisations associées à la COVID-19 en Colombie-Britannique a en effet montré des signes d’aplatissement alors que celui de l’Ontario a augmenté de façon linéaire. Le 14 avril, le nombre total d’hospitalisations en Ontario a dépassé pour la première fois celui de la Colombie-Britannique. Au 18 juin, les taux d’hospitalisation respectifs par 100 000 habitants étaient de 27,86 pour l’Ontario et de 9,96 pour la Colombie-Britannique. Dans les deux provinces, le nombre total d’hospitalisations est resté inférieur à celui des États américains choisis aux fins de comparaison. En conclusion, il y a des signes d’aplatissement de la courbe d’hospitalisations en Colombie-Britannique, mais pas encore en Ontario. La comparaison avec la Colombie-Britannique souligne la nécessité de continuer à faire preuve de prudence avec le relâchement des efforts de distanciation sociale en Ontario.
Mots-clés: Maladie à coronavirus 2019, pandémie, distanciation sociale, santé publique
Introduction
In response to the coronavirus disease 2019 (COVID-19) pandemic, Canadian society is currently undertaking a range of public health and social distancing measures that are designed to limit person-to-person contact and slow the rate of viral transmission in the population (Patrick et al. 2020). In doing so, the societal goal is to spread out the incidence of cases over time (i.e., flattening the curve) so that a surge of patients will not exceed the capacity of the healthcare system. To be effective on a societal level, though, social distancing demands personal sacrifices in the daily life of every individual. Accordingly, it is not surprising that there has been widespread societal interest in the total number of COVID-19 cases within a jurisdiction (city, province, country) for signs that these collective efforts are indeed achieving the goal of flattening the curve.
However, there are two reasons why total number of cases may not be the appropriate indicator for tracking the curve that society needs to flatten. First, the total number of cases may underestimate COVID-19 prevalence depending on the availability and extent of community testing. Second, since most affected individuals will recover with self-quarantine at home, it should be recognized that the total number of cases within a community may not reflect the specific subset of patients that threaten to overwhelm the healthcare system—namely, those who require hospitalization. Accordingly, the curve that needs to be flattened is that of COVID-19-associated hospitalizations. Indeed, besides reflecting the relevant patient population, this measure is less likely to be confounded by the extent of community testing for COVID-19 since the decision on whether to hospitalize a patient will be made on clinical grounds (irrespective of previous testing). Moreover, the admission will likely trigger inpatient testing for COVID-19. Thus, in this context, we evaluated the rates of COVID-19-associated hospitalization in British Columbia and Ontario to see if either province shows evidence of flattening the relevant curve.
Assessing the COVID-19 hospitalization curve in British Columbia and Ontario
To address this question, we drew upon publicly available data from (i) the BC Centre for Disease Control under the Provincial Health Services Authority and (ii) Public Health Ontario. The BC Centre for Disease Control has provided regular surveillance reports on COVID-19 cases in the province since March 23 (except on weekends and holidays) (BC Centre for Disease Control 2020). Public Health Ontario has provided a daily epidemiologic summary of COVID-19 cases in Ontario since March 29 (Public Health Ontario 2020). Both public health authorities provide data on cumulative COVID-19-associated hospitalizations in their respective provinces. We converted these data to rates per 100,000 population based on the provincial populations estimated by Statistics Canada for the first quarter of 2020 (Ontario: 14,711,827; British Columbia: 5,110,917) (Statistics Canada 2020a).
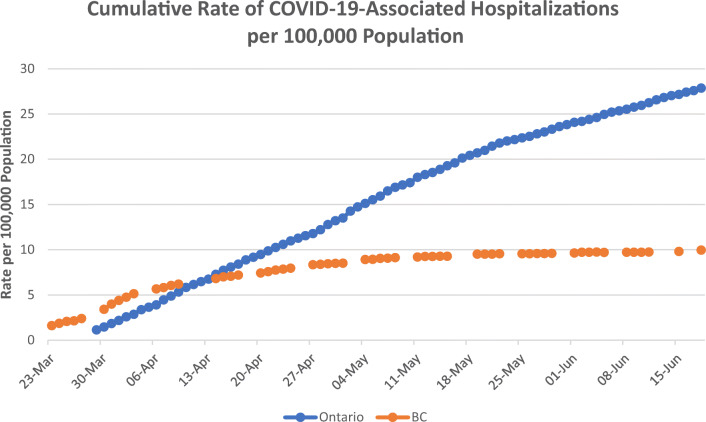
Figure 1 shows the cumulative rates of COVID-19-associated hospitalizations in British Columbia and Ontario from late March to mid-June 2020. These data show that the cumulative rate of hospitalization in Ontario on March 29 was lower than that in British Columbia on March 23. However, since then, there has been a flattening of the cumulative hospitalization curve in British Columbia, whereas the rise in this rate in Ontario has remained linear throughout. Accordingly, the cumulative hospitalization rate in Ontario first surpassed that of British Columbia on April 14 and has remained higher since then. In addition, based on the median age of the provincial population (Statistics Canada 2020b), the age-adjusted average cumulative hospitalization rate in Ontario from March 30 to June 18 (9.5 per 100,000 population) was higher than that of British Columbia (7.14 per 100,000 population).
Fig. 1.
Cumulative rates of COVID-19-associated hospitalizations in British Columbia (BC) and Ontario
To put the absolute rates of cumulative COVID-19-associated hospitalization into perspective, we compared the rates for British Columbia and Ontario over late March and April with those of 10 US states, as reported by the COVID-19-Associated Hospitalization Surveillance Network (COVID-NET 2020). This comparison reveals that, on each of March 28, April 4, April 11, April 18, and April 25 (dates for which US data were available during this window), the cumulative hospitalization rates in both British Columbia and Ontario were lower than in all 10 states (Table 1).
Table 1.
Cumulative COVID-19-associated hospitalization rates per 100,000 population in select US states, British Columbia, and Ontario on March 28, April 4, April 11, April 18, and April 25
| 28-Mar | 04-Apr | 11-Apr | 18-Apr | 25-Apr | |
|---|---|---|---|---|---|
| Connecticut | 23.2 | 57.8 | 94.3 | 130.6 | 156.4 |
| Michigan | 19.8 | 42.4 | 57.9 | 70.5 | 77.5 |
| Colorado | 12.3 | 22.4 | 31.6 | 43.7 | 52.9 |
| Tennessee | 11.7 | 20.9 | 26.1 | 30.5 | 35.2 |
| Maryland | 10.1 | 21.7 | 36.6 | 54.8 | 73.5 |
| New York | 9.2 | 18.1 | 24.7 | 30.0 | 35.3 |
| California | 6.4 | 9.7 | 13.2 | 16.2 | 18.0 |
| Oregon | 5.9 | 10.0 | 12.9 | 15.7 | 18.0 |
| Minnesota | 3.3 | 6.3 | 10.5 | 16.3 | 23.5 |
| Utah | 3.3 | 5.7 | 8.8 | 12.5 | 17.4 |
| British Columbiaa | 2.41 | 5.15 | 6.20 | 7.20 | 7.96 |
| Ontariob | 1.15 | 3.37 | 6.17 | 8.88 | 11.28 |
Data for US states are those which were presented by COVID-NET as of the update to May 2 (COVID-NET: COVID-19-Associated Hospitalization Surveillance Network, Centers for Disease Control and Prevention. https://gis.cdc.gov/grasp/COVIDNet/COVID19_3.html. Accessed on May 13, 2020)
aBritish Columbia data are for March 27, April 3, April 9, April 17, and April 24 respectively (because it is not reported on weekends and holidays)
bOntario data listed under March 28 are from March 29
Implications of these curves
Three findings emerge from these data. First, the change over time in the cumulative rate of COVID-19-associated hospitalization in British Columbia provides evidence that flattening of the relevant curve can be achieved. Second, this effect has not yet been achieved in Ontario. Third, the comparison to British Columbia underscores the need for continued caution with the relaxation of social distancing efforts in Ontario.
The concept of flattening the curve has been broadly embraced by Canadian society as the goal behind the social distancing efforts that we are collectively undertaking. However, the curve in question has been widely perceived as the total number of COVID-19 cases, which is a measure that is potentially confounded by limitations in community testing. Accordingly, we have focussed on COVID-19-associated hospitalizations as a more relevant metric. In this context, the British Columbia experience to date can be interpreted as an encouraging early sign of flattening of the rate of hospitalization. This finding provides a much-needed demonstration for the Canadian public that the societal efforts in this province are indeed achieving their goal.
While the hospitalization curve in Ontario has not yet shown clear flattening, consideration of the British Columbia experience may provide insight relevant to Ontario going forward. Table 2 lists dates of key events or interventions in the public health response to COVID-19 in British Columbia and Ontario. It is notable that recommendations on mass gatherings, social distancing, and self-isolation of returning travellers were generally initiated in early March in British Columbia. The subsequent flattening of the hospitalization curve only became apparent in the second week of April, well beyond the 2-week lag that had been anticipated. A message to be drawn for Ontario, which generally initiated its first public health interventions slightly later than British Columbia, is that this protracted time course for flattening the curve suggests that a prudent course going forward would be one of caution when relaxing current efforts.
Table 2.
Dates of key events/interventions in the public health response to COVID-19 in British Columbia (BC) and Ontario
| Event/intervention | BC | Ontario |
|---|---|---|
| Initial recommendation on limiting mass gatherings | 03-Mar | 13-Mar |
| Initial social distancing recommendation | 07-Mar | 16-Mar |
| Recommendation of self-isolation for returning travellers | 12-Mar | 16-Mar |
| Closure of schools | 17-Mar | 12-Mar |
| Declaration of provincial state of emergency | 18-Mar | 17-Mar |
| Closure of non-essential services | 26-Mar | 23-Mar |
The timing of initiating physical distancing measures may not be the only factor to consider in the differential hospitalization rates of British Columbia and Ontario. Differences in the age profile of the provincial populations also warrant consideration. Age profile is likely not the sole basis for the differential hospitalization rates, considering that the median age of the Ontario population (40.4 years) is slightly lower than that of British Columbia (42.2 years) (Statistics Canada 2020b). However, earlier attention to the risk of elderly individuals in long-term care facilities in British Columbia may have contributed to the flattening of the provincial hospitalization curve, in contrast to that of Ontario. Indeed, one of the key implications to draw from this experience may be that, going forward, enhanced precautions and surveillance of individuals working in long-term care and healthcare facilities may provide a targeted approach for reducing the overall impact of COVID-19 by reducing the exposure of the high-risk elderly population.
Although Ontario is not yet showing evidence of flattening the curve, there are positive signs suggesting that current efforts are helping. First, the absolute hospitalization rate per 100,000 population has remained lower than that of all 10 comparator US states in Table 1 and only surpassed British Columbia on April 14. Second, cautious encouragement may be drawn from the observation that the cumulative rate of COVID-associated hospitalization has been increasing linearly, rather than exponentially. Thus, while flattening of the relevant curve cannot yet be demonstrated for Ontario, there is reason to believe that it may be forthcoming with the continuation of current efforts and surveillance. This encouraging message may be helpful for maintaining societal engagement and commitment to social distancing.
A limitation of this analysis is the ecologic study design, which precludes definitive ascertainment of cause and effect between public health measures and COVID-19-associated health outcomes. Second, while these data were drawn from the daily reports of cumulative COVID-19-associated hospitalization provided by the respective provincial public health authorities in British Columbia and Ontario, it is recognized that their numbers are drawn from local public health reporting that can potentially be subject to inaccuracies and changes within the demands of a fast-moving health crisis such as this pandemic. Nevertheless, it is anticipated that the validity of the overall messages drawn from these data should be preserved since the current analysis has focussed on cumulative rates reported on a daily basis over this critical 10-week window.
Conclusion
In summary, there is evidence of flattening of the curve of COVID-19-associated hospitalization in British Columbia, suggestive of success in the provincial public health response. While this effect has not yet been achieved in Ontario, the absolute cumulative rate of hospitalization and its linear increase over time are signs for cautious optimism. That said, the protracted time course over which the rate of hospitalization changed in British Columbia suggests the need for continued caution with social distancing efforts in Ontario for mitigating the impact of COVID-19.
Acknowledgements
RR holds the Boehringer Ingelheim Chair in Beta-cell Preservation, Function and Regeneration at Mount Sinai Hospital and his research program is supported by the Sun Life Financial Program to Prevent Diabetes in Women. CK holds the Diabetes Canada Clinician-Scientist award.
Contributions
Concept and design: RR; acquisition, analysis, interpretation of data: CK, RR; statistical analysis: CK; drafting of the manuscript: RR; critical revision of the manuscript for important intellectual content: CK, RR; funding and supervision: RR.
Compliance with ethical standards
Conflict of interest
The authors have no conflicts to declare relevant to this manuscript. RR reports grants and personal fees from Novo Nordisk, grants from Boehringer Ingelheim, personal fees from Eli Lilly, and personal fees from Sanofi, outside the submitted work. CK reports grants from Boehringer Ingelheim, outside the submitted work.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- BC Centre for Disease Control. (http://www.bccdc.ca/health-info/diseases-conditions/covid-19/case-counts-press-statements). Accessed daily from March 24, 2020 onwards.
- COVID-NET: COVID-19-Associated Hospitalization Surveillance Network, Centers for Disease Control and Prevention. https://gis.cdc.gov/grasp/COVIDNet/COVID19_3.html. Accessed on May 13, 2020.
- Patrick K, Stanbrook MB, Laupacis A. Social distancing to combat COVID-19: we are all on the front line. CMAJ. 2020;192(19):E516–E517. doi: 10.1503/cmaj.200606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Ontario. (https://www.ontario.ca/page/2019-novel-coronavirus#section-0). Accessed daily from March 29, 2020 onwards.
- Statistics Canada. (2020a). Table 17-10-0009-01 Population estimates, quarterly. 10.25318/1710000901-eng. Accessed April 11, 2020.
- Statistics Canada. (2020b). Table 17-10-0005-01 Population estimates on July 1st, by age and sex. 10.25318/1710000501-eng. Accessed June 23, 2020.