Abstract
The pentraxin is a superfamily of proteins with the same domain known as the pentraxin domain at C-terminal. This family has two subgroups, namely; short pentraxins (C-reactive protein and serum amyloid P component) and long pentraxins (neuronal pentraxin 1, neuronal pentraxin 2, neuronal pentraxin receptor, pentraxin 3 and pentraxin 4). Each group shares a similar structure with the pentameric complexes arranged in a discoid shape. Previous studies revealed the functions of different pentraxin family members. Most of them are associated with human innate immunity. Inflammation has commonly been associated with tumor progression, implying that the pentraxin family might also participate in tumor progression. Therefore, we reviewed the basic characteristics and functions of the pentraxin family and their role in tumor progression.
Keywords: C-reactive protein, serum amyloid P component, the long pentraxins, pentraxin 3, tumor
Introduction
The pentraxin family is a superfamily of protein that share the same domain and are made from monomers arranged in pentameric structures with a discoid shape (1). The members of the family are characterized by a 205 amino acids (AA) long conserved sequence located at C-terminal called the pentraxin domain. Members of the pentraxin family share a similar 8 AA (His-x-Cys-x-Ser/Thr-Trp-x-Ser, in which x represent any AA) long conserved sequence called the pentraxin signature within the pentraxin domain (2). Based on the length of the protein sequence, the pentraxin family can be classified into two subfamilies: the short and long pentraxins. The short pentraxins are comprised of C-reactive protein (CRP) and serum amyloid P component (SAP), whereas the long pentraxins are composed of neuronal pentraxin 1(NPTX1), neuronal pentraxin 2 (NPTX2), neuronal pentraxin receptor (NPTXR), pentraxin 3 (PTX3), and pentraxin 4 (PTX4) (3). The long pentraxins are approximately twice the size of the short pentraxins with an un-related long N-terminal sequence. This structure variability of family members could explain their function difference.
In the past decades, studies have revealed the functions of specific members of the pentraxin family. For example, the member of the short pentraxin family, CRP, and SAP were previously reported as mediators in human immune system regulation (4–6). Their functions in immune regulation include acting against pathogen invasion, removing mutant cells, and triggering inflammation. The neuronal pentraxins are involved in the development of the central nervous system and neurodegenerative diseases (7). PTX3 not only participates in immune system activation but also affects tumor progression (8, 9).
Chronic inflammations such as chronic atrophic gastritis and cervical intraepithelial neoplasia have been recognized as precancerous lesions (10). Therefore, inflammation is closely associated with tumor progression, including tumorigenesis, metastasis. Reactive oxygen/nitrogen species (ROS/RNS) produced by immune cells and epithelial cells fight against microbial invasion and eliminate the mutant cell. However, they can cause cell dysfunction and promote tumorigenesis (11, 12). Tumors induce inflammation by either producing antibodies or rejecting immunocytes infiltration to avoid immune system surveillance (13). Additionally, the tumor microenvironment facilitates the growth of cancer cells, metastasis, and enhances drug resistance (14). It is necessary to explore the mechanisms through which inflammation and tumor microenvironment enhances tumor progression.
Several reports have also been documented on the role of the pentraxin family in tumor progression. Likewise, several receptors and pathways have been proposed that could be associated with the mechanisms employed by the pentraxin family in mediating tumor progression. Most members of the pentraxin family can activate the PI3K/AKT/mTOR pathways, thereby interfering with the normal cell- cycle. The neuronal pentraxins and PTX3 possess specific unique receptors that mediates tumor progression (15). In this review, we have summarized the basic characteristics and functions of each pentraxin family member and highlighted the existing connection between their structures and specific roles in tumor progression.
C-Reactive Protein
The human C-reactive protein (CRP) gene is located on the chromosome 1q23.2 (16), and has a length of 1.8-kb. It consists of 0.1 kb at untranslated region (UTR) in the 5′ terminal and a 1.2 kb pair UTR region in the 3′ terminal, with two exons separated by an intron. The first exon encodes 18 AA signal peptide and the first two amino acids, whereas, the second exon encodes the rest AA (16). The X-ray derived structures of CPR are pentameric with five subunits arranged in a discoid shape. Each unit contains 206 AA with two anti-parallel b-sheets appearing as a flattened b-barrel with a jellyroll topology. The two sides of its discoid have distinct functions. The Ca2+ binds to the “A” side and activates the classical complement pathway and phagocytosis by interacting with C1q and Fcγ receptor, respectively (17, 18). The “B” side, CRP recognizes phosphocholine (PCh), a bacterial cell wall component, and eliminates the pathogen (19). The CRP also binds to soluble control protein factor H regulating the alternative-pathway amplification and C3 convertase (18). The secretion of CRP by hepatocytes can be stimulated by the IL6 and IL1 (20), which enhances innate immunity by triggering inflammation and neutralizing pathogen (18, 21).
CRP and Tumor
CRP activates various signaling pathways by binding to the Fcγ receptor (22, 23), which links it with inflammation (17). The PI3K/AKT/mTOR signaling pathway is associated with tumor cell proliferation, metabolic reprogramming, apoptosis, and metastasis (24). For instance, the CRP arrest cell-cycle at the sub G1 phase by negatively regulating the PI3K/AKT/mTOR signaling pathway in myeloid leukemia (25) and tongue squamous cell carcinoma (26) thus promoting tumor progression. It has been reported that interaction between CRP and Fcγ receptor I facilitate tumor cell metastasis in breast cancer (23). Furthermore, CRP targets to the p38/MAPK pathway causing lytic bone lesions (27) and activates the PI3K/AKT/mTOR and the ERK/NF-κB pathway thereby inhibiting tumor cell apoptosis via the Fcγ receptor II in multiple myeloma (22).
Previous reports showed that CRP is a clinical marker for infection and has a regulatory role in innate immunity (17, 28). The IL-6/JAK/STAT signaling pathway has been reported to enhance CRP expression in glioblastoma (29), clear cell renal cell carcinoma (30) and gastroesophageal cancers (31). Moreover, the pathway enhances the formation of CRP-mediated tumor microenvironment by activating tumor-associated macrophages (30) and tumor angiogenesis (32, 33). CRP regulates cell apoptosis and cell-cycle in clear cell renal cell cancer (34). Notably, inhibiting CRP expression by targeting IL-1 can prolong overall survival time for patients with multiple myeloma (35).
Multiple studies have, therefore, confirmed that CRP could be used as a prognosis factor (36–38). This has been reported in different tumors including breast cancer (39), prostate cancer (40), non-small cell lung cancer (41), hepatocellular carcinoma (42), cervical cancer (43), head and neck squamous cell carcinoma (44), diffuse large B-cell lymphoma (45) and osteosarcoma (46). The specific mechanisms involved are still lacking. Controversies have also emerged in determining the role of CRP in pancreatic cancer (47, 48) and colorectal cancer (49–51). Considering that CRP also affects tumor progression, more effort in explicating its role in the tumor might be beneficial in understanding the connection between tumor and human innate immunity (Figure 1).
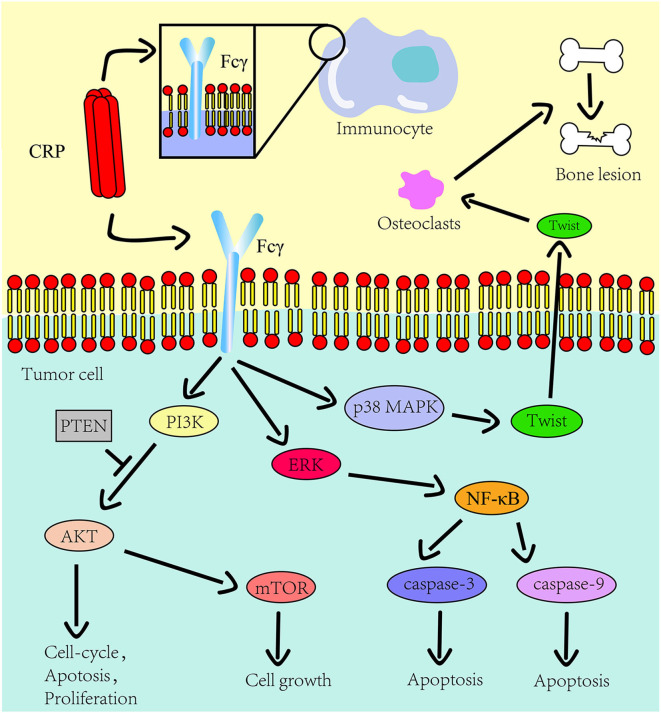
Figure 1.
The role CRP on the innate immune system and tumor progression. The Fcγ receptor is expressed on the cell surface of immunocyte and multiple myeloma cells. CRP binds to Fcγ receptor to promote inflammation and tumor progression. The downstream pathways of this receptor in tumors include the PI3K/AKT/mTOR pathway, the ERK/NF-κB pathway and the p38/MAPK pathway. CRP regulates the expression of osteolytic cytokines in myeloma cells through p38 MAPK-Twist signaling.
Serum Amyloid P Component
The serum amyloid P component (SAP) gene, identified as a close CRP paralog, is also localized on the chromosome 1q23.2 and shares the same gene architecture (52). The gene is approximately 1.1 kb long with 0.1 kb 5′ UTR and 0.15 kb 3′ UTR. The SAP structure is similar to CRP except that its subunits consist of 204 AA and has a slight difference at the calcium-binding site (4, 53, 54). In the absence of calcium, SAP form decamers composed of two pentamers facing each other (4). The two ligands of SAP, deoxyadenosine 5′-monophosphate (dAMP), and the 4,6-pyruvate acetal of β-D-galactose (MoβDG), bind calcium and amyloid fibrils, respectively (55). To distinguish structure and gene sequence of short pentraxins, we archived data on the 3D structure for CRP and SAP from the PDB web portal (https://www.rcsb.org/, Figures 2A,B). The prediction of their domain was inferred from the Pfam database (http://pfam.xfam.org/, Figure 3) and the Genecard database (https://www.genecards.org/, Table 1).
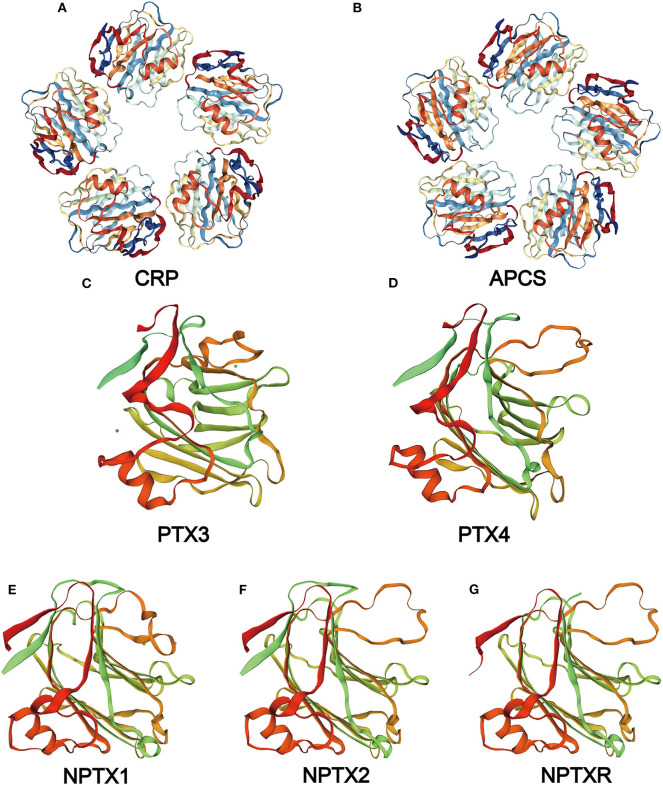
Figure 2.
Structure of the pentraxin family members. Protein structure of CRP (A) and SAP (B) from the PDB website and the hypothetical structure of the full monomer (C-terminal domain and N-terminal domain) of PTX3 (C), PTX4 (D), NPTX1 (E), NPTX2 (F), NPTXR (G) from the Swiss database.
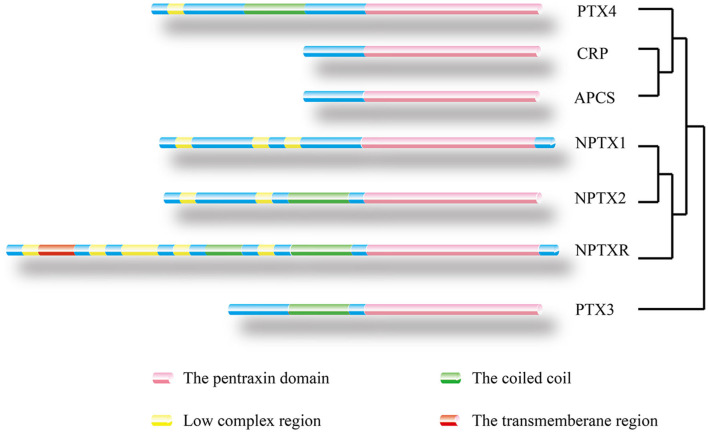
Figure 3.
Location of protein domain for each family member and their sequence homology. The outcome was predicted by the Pfam database. Pink box: Pentraxin domain. Green box: Coiled coil. Yellow box: Low complex region. Red box: Transmembrane region. A homology tree based on the similarity of the protein sequence of members of the pentraxin family is generated.
Table 1.
The basic characteristics of two short pentraxins, CRP and SAP.
| Characteristics | CRP | SAP |
|---|---|---|
| Genomic location | 1q23.2 | 1q23.2 |
| Gene sequence | 1.8 kb in length, 0.1 kb of 5' UTR, 1.2 kb of 3' UTR | 1.1 kb in length, 0.1 kb of 5' UTR, 0.15 kb of 3' UTR |
| Domain structures | Pentraxin-related, ConA-like_dom_sf, Pentaxin_CS | Pentraxin-related, ConA-like_dom_sf, Pentaxin_CS |
| Top tissue expression | Liver | Liver |
| Signaling pathway | PI3K/Akt signaling pathway (25), JAK/STAT signaling pathway (35) | PI3K/Akt/ERK signaling pathway (56) |
CRP, C-reactive protein; SAP, serum amyloid P component; UTR, un-translated region; The domain structures were obtained from the Genecard database.
Like CRP, SAP is also secreted by hepatocytes and mediates innate immunity by interacting with the complement system and the Fcγ receptor (17). This decreases neutrophil adhesion, inhibits neutrophil spreading, regulates macrophage activation (56), and inhibits fibrocyte differentiation (57). Besides, SAP is involved in immunological tolerance by binding to DNA or chromatin resulting from necrosis and apoptosis cell (58). Furthermore, SAP binds to amyloid fibrils through MoβDG, thereby causing amyloidosis disease (4–6). SAP is also associated with tuberculosis (59) and sickle cell disease (60), but the specific mechanisms are unknown. Despite limited reports on the role of SAP in tumors, SAP is considered a prognosis factor in non-small cell lung cancer (61). The highly structural homology between SAP and CRP suggests that SAP has the potential to mediate tumor progression through the Fcγ receptor.
The Neuronal Pentraxins
Neuronal pentraxin 1 (NPTX1 or NP1) is a 47–50 kDa secreted glycoprotein mainly expressed in neurons. The NPTX1 gene is located on chromosome 17q25.3. Its cDNA clones sequence is made up of a 150 bp 5′UTR, a 1.3 kb coding region, and a 3.6 kb 3′UTR with four introns (62). NPTX1 contains three main domains: a putative ligand- and calcium-binding site, the pentraxin domain, and an Asn-linked glycosylation site (62). Three NPTX1 domains, including the Pentraxin-related domain, the Pentraxin_CS (Pentraxin, conserved site), and glucanase domain superfamily (ConA-like_dom_sf) are speculated from the Genecard database.
Neuronal pentraxin 2 (NPTX2 or NP2, also known as apexin/p50 in guinea pig or narp in rat), is a ~47 kDa secretory glycoprotein with 431 AA. It is expressed in various tissues of the brain, testicle, pancreas, and skeletal muscle (1). The human NPTX2 gene is located on chromosome 7q22.1. Its cDNA sequence is made up of a 1.3 kb coding region and 1.2 kb 3′-UTR with four introns (1). Domains of NPTX2 are the same as those of NPTX1, according to the speculation from the Genecard website.
Neuronal pentraxin receptor (NPTXR or NPR) is an ~53 kDa type-II transmembrane protein with 500 AA and is mostly expressed in the brain. It is the only pentraxin family member anchored to the cell membrane by a putative N-terminal transmembrane domain. The receptor binds tightly to its ligands, such as taipoxin, TCBP49, NPTX1, and NPTX2, and activates different downstream signal transduction processes (63). In the human genome, the NPTXR gene is located on chromosome 22q13.1 and has the longest cDNA clones sequence containing a 3.9 kb 3′ UTR and a 1.5 kb open reading frame (63). From the Gencard database, this protein consists of two main domains, Pentraxin-related domain and glucanase domain superfamily (ConA-like_dom_sf). The N-terminal structure of the neuronal pentraxins is unrelated to other known human protein structures (64). Therefore, multiple online databases were used to generated detailed information about the structures of the neuronal pentraxins. The 3D structures of monomer were referenced from the Swiss database (https://www.swissmodel.expasy.org/, Figures 2E–G), and their domains were projected from the Pfam (Figure 3) and the Genecard databases (Table 2).
Table 2.
The basic characteristics of the long pentraxins.
| Characteristics | NPTX1 | NPTX2 | NPTXR | PTX3 | PTX4 |
|---|---|---|---|---|---|
| Genomic location | 17q25.3 | 7q22.1 | 22q13.1 | 3q25.32 | 16p13.3 |
| Sequence features | 150 bp of 5' UTR, 1.3 kb coding sequence, 3.6 kb 3' UTR | 1.3 kb coding sequence, 1.2 kb 3'-UTR | 5.5 kb in length, 3.9 kb of 3' UTR, 1.5 kb open reading frame | 68 bp of 5' UTR, 650 bp of 3' UTR, | – |
| Domain structures | Pentraxin-related, Pentraxin_CS, ConA-like_dom_sf | Pentraxin-related, Pentraxin_CS,ConA-like_dom_sf | Pentraxin-related, ConA-like_dom_sf, N-terminal transmembrane domain | Pentraxin-related, Pentraxin_CS, ConA-like_dom_sf | Pentraxin-related, Pentraxin_CS,ConA-like_dom_sf |
| Top tissue expression | Brain | Brain, liver, testis, skeletal muscle, heart, pancreas | Brain | Monocytes, macrophage, fibroblasts, epithelial cells | Thymus, spleen, small intestine, liver |
| Signaling pathway | HIF-1 signaling pathway (65), IRS-1/PI3K/Akt signaling pathway (66), JNK and GSK3 signaling pathways (67), Rb/E2F pathway (68), Nodal and BMP signaling pathway (69) | Wnt/β-catenin signaling pathway (70), p53/PTEN/Akt/NF-κB signaling pathway (71) | – | Akt/NF-kB signaling pathway (9), JNK signaling pathway (72), IL-6/Stat3 signaling pathway (73), PI3K signaling pathway (74) | – |
NPTX1, neuronal pentraxin 1; NPTX2, neuronal pentraxin 2; NPTXR, neuronal pentraxin receptor; PTX3, pentraxin 3; PTX4, pentraxin 4; UTR, un-translated region; Domain structure were obtained from the Genecard database.
The Function of the Neuronal Pentraxins
The neuronal pentraxins have different functions in the development of the central nervous system (7) such as mediation of neural differentiation (69), synaptogenesis (75) and synapse plasticity (76, 77). Abnormal expression of the neuronal pentraxins has been reported in some mental diseases such as bipolar disorder (78), central precocious puberty (79), anxiety (80), depression (80), childhood-onset mood disorders (81) and schizophrenia (82). The neuronal pentraxins are associated with neurodegenerative diseases, including Alzheimer's disease (AD) (83, 84) and Parkinson's disease (PD) (85, 86). Researchers concluded that NPTXR protein in cerebrospinal fluid is a novel potential biomarker of AD progression and could have important utility in assessing treatment success in clinical trials (83), and NPTX1 could significantly contribute to the pathogenesis of PD (87). Moreover, only NPTX1 among all the neuronal pentraxins participates in inflammation by inducing mitochondria dysfunction (65, 67). Despite the neuronal pentraxins contains the pentraxin domain like the short pentraxins, few studies have classified their roles in human innate immunity which might result from the difference in their tertiary structure.
The Neuronal Pentraxins in Cancer
Several pathways were identified as potential mechanisms through which the neuronal pentraxins promote tumor progression. NPTX1 and NPTX2 were reported to cause dysfunction of the PI3K/AKT/mTOR pathway thereby affecting tumor progression in glioma (66), gastrointestinal stromal tumors (GIST) (88) and subependymal giant cell astrocytoma (89). Additionally, NPTX2 promotes tumor cell proliferation and metastasis by activating the NF-κB pathway (71, 90) and the Wnt/β-catenin pathway (70). It also induces tissue edema via an independent pathway from the classical VEGF-relate pathway (91). The dysfunction of the PI3K/AKT/mTOR pathway interferes with the normal cell-cycle and causes tumorigenesis. Similarly, NPTX1 and NPTX2 can inhibit cyclin A2 and CDK2 through the Rb/E2F signaling pathway (68), respectively, thus inducing G0/G1 arrest in pancreatic cancer (92, 93). Overexpression of NPTX2 has been identified as a prognosis factor in clear cell renal cell carcinoma, and its interaction with AMPA-selective glutamate receptor-4 affects tumor cell viability and metastasis (94, 95).
Abnormal expression of the neuronal pentraxins has been reported in different tumors such as cervical carcinoma (96), primary lung cancer (97), Ewing sarcoma (98), neuroblastoma (99), small cell lung cancer (100) and neuroblastoma (99). Another study has reported an increase in NPTX1 expression in pancreatic cancer after treatment with metformin and aspirin (101). On the contrary, a low level of NPTX2 showed better response to neoadjuvant chemoradiation (CRT) treatment in rectal adenocarcinomas (102).
The neuronal pentraxins are crucial in the central nervous system development when they interact with the AMPA receptor. The AMPA receptor has been proved to be associated with tumors (103, 104). Therefore, the AMPA receptor is a potential linkage between the neuronal pentraxins and tumor development as opposed to other members of the pentraxin family. Conclusively, the above-reviewed studies did not reveal the explicit mechanism through which the neuronal pentraxins affect tumor progression; however, they form the basis for in-depth studies on the existing association between the two.
Pentraxin 3 and Pentraxin 4
Pentraxin 3 (PTX3) and pentraxin 4 (PTX4) are characterized as long pentraxins. The PTX3 gene is located on chromosome 3q25 and has three exons and two introns (105). The three exons encode the leader peptide, an N-terminal domain, and the pentraxin domain, respectively (106). The N-terminal domain of PTX3 and PTX4 is not related to any known protein. However, based on previous research, PTX3 has a putative N-terminal domain that shows structural similarity to the mannose-binding protein and the surfactant proteins (107). PTX3 is secreted by different cell types that include dendritic cells, macrophages, and fibroblasts (108).
PTX4 gene is located on chromosome 16p13.3 and consists of three exons. However, the human PTX4 cDNA sequence and its first exon failed to amplify because it was different from the sequences in the various database (109). The sequence analysis of the protein showed a highly structural homology between PTX4 and the short pentraxins (Figure 2D). This indicates that PTX4 might be playing specific roles in innate immunity or tumor progression. To compare the PTX3 and PTX4 structures, their 3D structures were predicted from the Swiss database (https://www.swissmodel.expasy.org/, Figures 2C,D), and their domain predicted from the Pfam (Figure 3) and the Genecard databases (Table 2).
Functions of PTX3 and PTX4
From the previous study, an increase in blood PTX3 concentration serves as a monitor of inflammation initiation. The maximal PTX3 level increased slightly earlier than the CRP level (110), suggesting that PTX3 could be a highly sensitive inflammation-related factor. The interaction between PTX3 and the complement system has broad implications in host defense against microbial infections, regulation of the inflammatory reaction, and removal of dead cells. PTX3 is actively involved in the complement pathways activation (111). For example, the classical activation cascade may be initiated when PTX3 binds to C1q via the Fcγ receptor III once the latter is bound on a microbial surface (64, 112, 113). However, the process can be inhibited if the interaction occurs in the fluid-phase (114).
Furthermore, the N-terminal domain of PTX3 enhances tissue repair and remodeling functions (115). A study reported that PTX3 inhibited interstitial fibrosis in acute renal injury (73), indicating its role in an extracellular matrix formation. The N-terminal domain also combines with FGF2 to mediate angiogenic activity (116). For PTX4, there is currently no evidence supporting its functions in innate immunity or tumor progression.
PTX3 and Cancer
PTX3 interacts with the PI3K/AKT/mTOR signaling pathway to induce tumor cell proliferation, apoptosis and metastasis in lung cancer (9), head and neck squamous cell carcinoma (74) and breast cancer (117). PTX3 also inhibits cell proliferation and tumor metastasis by modulating the expression of protein related to the G2/M phase cell-cycle in cervical cancer (118). Furthermore, it arrests cell-cycle at the G0/G1 phase by stimulating the secretion of p21 protein in glioma (119).
Notably, we reported that PTX3 interacts with the fibroblast growth factor-2 (FGF2)/FGF receptor (FGFR) system that mediates the epithelial-mesenchymal transition (EMT) through its N-terminal domain (120). Through this system, PTX3 inhibits tumor metastasis, tumor growth and tumor angiogenesis in melanoma (8), breast cancer (121), prostate cancer (122) and multiple myeloma (123). Besides, PTX3 binds to fibroblast growth factor-8b receptor (FGF8b) and inhibits tumor cell proliferation in steroid hormone-regulated tumors (124). Compared to other pentraxin family members, the PTX3 is highly associated with the FGFR system.
Abnormal PTX3 expression was also observed in different tumors, including glioma (125), esophageal squamous cell carcinoma (126), pancreatic cancer (127), gastric cancer (128), colorectal cancer (129), leiomyosarcoma and desmoid tumors (130). Previous studies have shown that the activation of Fcγ receptor promotes tumor progression (131, 132). Of note, Fcγ receptor expression on NK cells modulates tumor response to immunotherapy (133), and PTX3 can exert its function in human immunity by interacting with this receptor. However, no current research has bridged PTX3 and tumor progression through the Fcγ receptor. Therefore, the multifaceted role of PTX3 in cancer requires further comprehensive study.
Overall Survival Analysis Prediction
We conducted the overall survival analysis of the pentraxin family to establish the relationship between the tumor and the pentraxin family members using the Gepia web portal (http://gepia.cancer-pku.cn/, Supplementary Table).
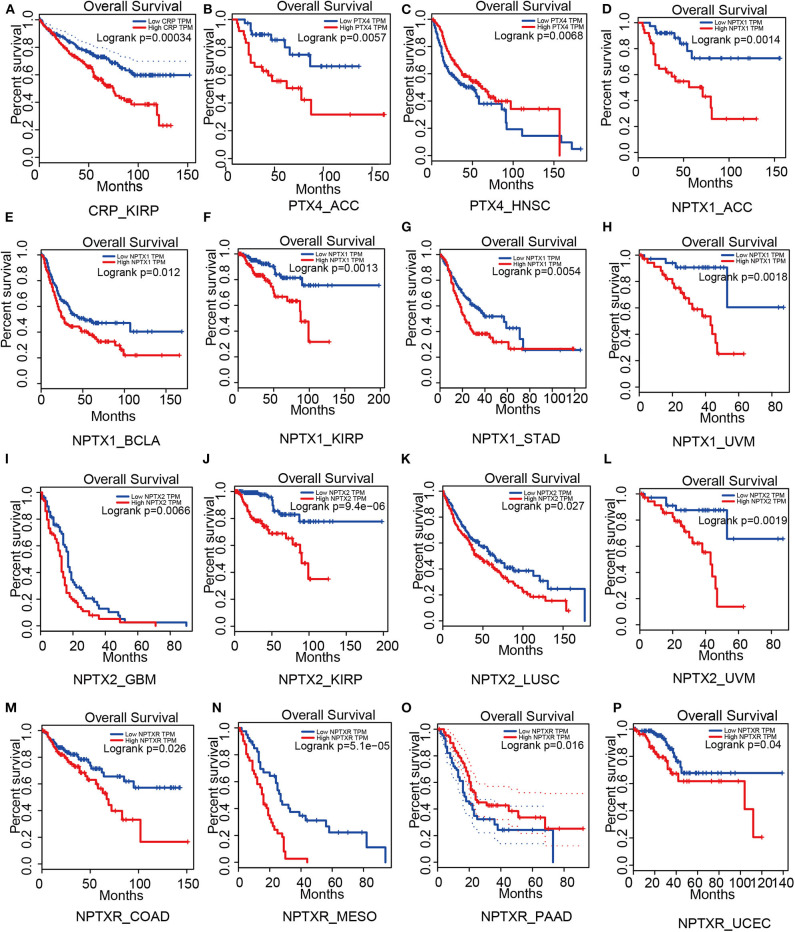
For short pentraxins, low expression of CRP showed better survival outcomes in kidney renal papillary cell carcinoma (KIRP) than high CRP expression (Figure 4A). There was no significant difference in survival outcome between the high and low expression of SAP. The expression levels of PTX4, with similar protein sequence as short pentraxins, showed a significant difference in survival outcome in adrenocortical carcinoma (ACC) and head and neck squamous cell carcinoma (HNSC) (Figures 4B,C).
Figure 4.
Survival analysis based on members of the pentraxin family from the Gepia website. Outcome of survival analysis predicted by the Gepia database including CRP (A), PTX4 (B,C) and the neuronal pentraxins (D–P).
We revealed that low NPTX1 expression improved the survival outcomes in patients with adrenocortical carcinoma (ACC), urothelial bladder carcinoma (BCLA), kidney renal papillary cell carcinoma (KIRP), stomach adenocarcinoma (STAD) and uveal melanoma (UVM), (Figures 4D–H). Patients that showed high expression of NPTX2 frequently exhibited worse survival outcomes for glioblastoma multiforme (GBM), kidney renal papillary cell carcinoma (KIRP), lung squamous cell carcinoma (LUSC) and uveal melanoma (UVM), (Figures 4I–L). On the other hand, overexpression of NPTXR predicted worse survival outcomes for colon adenocarcinoma (COAD), mesothelioma (MESO), and pancreatic adenocarcinoma (PAAD) and better survival outcome in uterine corpus endometrial carcinoma (UCEC) (Figures 4M–P).
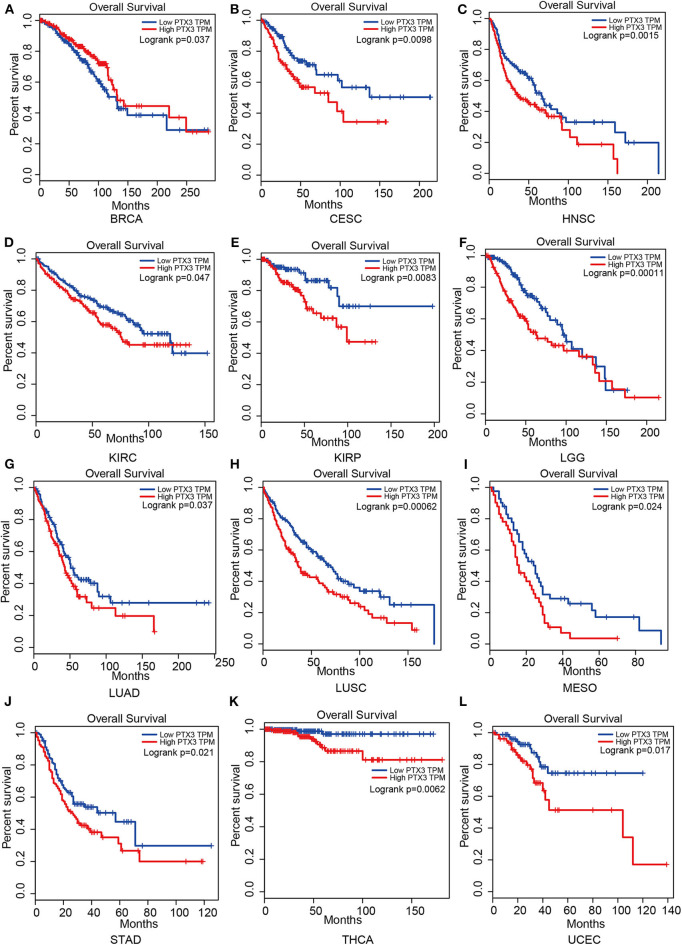
Therefore, PTX3 is considered a promoter in tumor progression since its overexpression resulted in worse survival outcomes in invasive breast carcinoma (BRCA), cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC), head and neck squamous cell carcinoma (HNSC), kidney renal clear cell carcinoma (KIRC), kidney renal papillary cell carcinoma (KIRP), brain lower-grade glioma (LGG), lung adenocarcinoma (LUAD), lung squamous cell carcinoma (LUSC), mesothelioma (MESO), stomach adenocarcinoma (STAD), thyroid carcinoma (THCA) and uterine corpus endometrial carcinoma (UCEC), (Figure 5).
Figure 5.
Impact of PTX3 on overall survival and tumor phenotypes based on the Gepia dataset. (A) Breast invasive carcinoma. (B) Cervical squamous cell carcinoma and endocervical adenocarcinoma. (C) Head and Neck squamous cell carcinoma. (D) Kidney renal clear cell carcinoma. (E) Kidney renal papillary cell carcinoma. (F) Brain Lower Grade Glioma. (G) Lung adenocarcinoma. (H) Lung squamous cell carcinoma. (I) Mesothelioma. (J) Stomach adenocarcinoma. (K) Thyroid carcinoma. (L) Uterine Corpus Endometrial Carcinoma. The overall survival of tumor that cannot be predicted by PTX3 expression is not listed.
The protein structure variability sheds light on the prognosis prediction ability of members of the pentraxin family. The expression of PTX3 affects multiple tumor types compared to other members of the pentraxin family, implying a potential association between its putative N-terminal domain and tumor progression. PTX4 shares a similar protein structure with the short pentraxins, and they are both poor predictors of survival outcomes of patients suggesting that they mainly concentrate on monitoring inflammation. However, this deduced relationship between protein structure and their prognosis capability requires further confirmation.
Conclusions
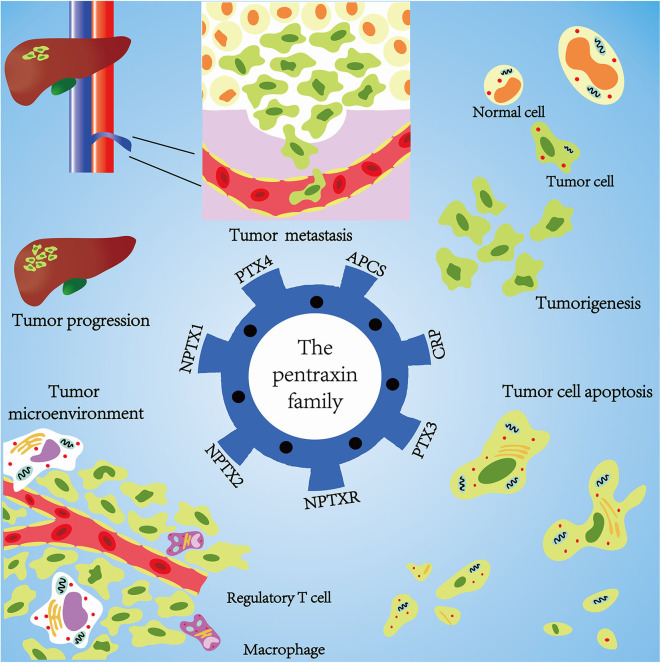
Emerging evidence confirms that the pentraxin family is associated with tumor progression by affecting tumor proliferation, mediating tumor cell apoptosis, inducing tumor metastasis, and promoting tumor tissue edema (Table 3, Figure 6). The tumor microenvironment is an extremely complex network consisting of cancer-associated fibroblasts, adipose cells, immunocytes, new-born vessels, and extracellular matrix. The pentraxin family promotes the formation of tumor microenvironment by facilitating macrophage infiltration and stimulating cytokines secretion. The pentraxin family, therefore, plays an essential role in tumor progression, although the exact mechanisms are still unknown and require further in-depth studies.
Table 3.
Role of pentraxins in the control of various tumors.
| Tumor | Gene | Expression | References | Mechanism |
|---|---|---|---|---|
| Glioma | PTX3 | Differ from low and high grade | (134) | Arrest cell cycle at the G0/G1 phase to affect glioma proliferation and metastasis. |
| Glioma | NPTX1 | Increased | (66) | Promote tumor proliferation and metastasis via the IRS-1/PI3K/AKT signaling pathway |
| Glioma | NPTX2 | Increased | (91) | Induce tumor tissue edema independent of the classical VEGF-relate pathway |
| Glioblastoma | CRP | Increased | (29) | Stimulate microglial cells to secret IL-1β which could induce tumor angiogenesis. |
| Glioblastoma | NPTX2 | Decreased | (90) | Increase survival ratio through reducing NF-κB activity via inhibiting AKT by p53/PTEN-dependent pathway |
| Neuroblastoma | NPTX2 | Increased | (92) | NPTX2 antagonist could reduce tumor progression |
| Neuroblastoma | NPTXR | Increased | (92) | Give NPTXR antagonist inhibit tumor progress |
| Subependymal giant cell astrocytoma | NPTX1 | Decreased | (89) | After inhibiting the mTOR signaling pathway not only decrease tumor volume but also increase the expression of NPTX1 |
| Colorectal cancer | NPTX2 | Increased | (70) | Combine to frizzled class receptor 6(FZD6) which activate the Wnt/β-catenin signaling pathway to promote tumor growth and metastasis |
| Rectal adenocarcinomas | NPTX2 | Decreased | (102) | Low level expression improve response to neoadjuvant chemoradiation (CRT) treatment |
| Colorectal cancer | NPTX1 | Decreased | (68) | Inhibit cell proliferation by influence the combination of cyclin A2 and CDK2 and the Rb-E2F signaling pathway |
| Lung cancer | PTX3 | Increased | (9) | Deglycosylased PTX3 observed suppress tumor migration via inactivating the PI3K/AKT and the NF-κB signaling pathway. |
| Non-small Cell Lung Cancer | SAP | Increased | (61) | SAP contributes to the clearance of apoptotic cells. |
| Breast cancer | CRP | Increased | (23) | Binds to Fcγ receptor I and to promote tumor metastasis. |
| Breast cancer | PTX3 | Decreased | (124) | PTX3 inhibit tumor progression via combining to receptor of fibroblast growth factor-8b (FGF8b) and metastasis by activating the EMT process. |
| Clear cell renal cell cancer | NPTX2 | Increased | (94) | Promote tumor viability and invasion via binding to AMPA-selective glutamate receptor-4 |
| Clear cell renal cell cancer | CRP | Increased | (34) | Up–regulate the expression of ATG9B gene to inhibit tumor cell apoptosis and the formation of tumor microenvironment. |
| Head and neck cancer | PTX3 | Increased | (135) | Affect tumor metastasis via the PI3K/AKT and the NF-κB signaling pathway. |
| Head and heck squamous cell carcinoma | CRP | Increased | (44) | Promote tumor cell proliferation, metastasis and angiogenesis through the PI3K/AKT signaling pathway. |
| Multiple myeloma | CRP | Increased | (25) | Binds to Fcγ receptor II to protect tumor and cause lytic bone lesions |
| Multiple myeloma | PTX3 | Increased | (123) | Promote tumor cell proliferation, metastasis and angiogenesis through the PI3K/AKT signaling pathway. |
| Melanoma | CRP | Increased | (136) | Inhibit tumor angiogenesis, via FGF2/FGFR system, proliferation and apoptosis. |
| Melanoma | PTX3 | Increased | (8) | Cause vitamin D deficiency. |
| Cervical cancer | PTX3 | Increased | (118) | Inhibit tumor metastasis via FGF2/FGFR system which impair the EMT process |
| Gastroesophageal cancer | CRP | Increased | (31) | Modulate the G2/M phase cell-cycle related protein expression to affect cell proliferation. |
| Hepatocellular carcinoma | CRP | Increased | (137) | Promote tumor angiogenesis via influencing certain cytokines. |
| Myeloid leukemia | CRP | Increased | (25) | Its expression level is parallel with HBV activity while silence could promote tumor progression. |
| Pancreatic cancer | NPTX2 | Decreased | (92) | Inhibits cell proliferation through the PI3K/AKT signaling pathway. |
| Prostate cancer | PTX3 | Decreased | (122) | Inhibit tumor progression and migration decrease via inducing cell G0–G1 arrest and inhibiting cell apoptosis |
Data from merely abnormal expression or with lack of specific relationships are not mentioned.
CRP, C-reactive protein; SAP, serum amyloid P component; NPTX1, neuronal pentraxin 1; NPTX2, neuronal pentraxin 2; NPTXR, neuronal pentraxin receptor; PTX3, pentraxin 3; PTX4, pentraxin 4.
Figure 6.
Mechanisms of pentraxin family in tumor progression. At the core is the pentraxin family and its seven members. The pentraxin family mainly participates in tumor metastasis, tumorigenesis, tumor cell apoptosis, tumor cell proliferation, and regulation of tumor microenvironment.
Protein structure of short pentraxins and their role in the immune system has highly been explored compared to the long pentraxins. It has been reported that PTX3 and NPTXR, for example, have an additional N-terminal domain other than the known pentraxin domain and exhibit different functions. Each pentraxin family member has their specific unique functions, for instance, SAP binds to amyloid fibrils and the neuronal pentraxins and extensively participates in the central nervous system development. Furthermore, the pentraxin family affects tumor progression through their unique receptors and pathways. Therefore, an in-depth analysis of the protein structure of the pentraxins family and their underlying mechanisms using advanced electron microscopy technologies, such as cryo-electron microscopy, is important for future research.
The PI3K/AKT/mTOR pathway is commonly associated with the pentraxin family in inducing tumor progression. Nevertheless, each pentraxin family member poses a specific receptor linked with tumor progression. Short pentraxins bind with the Fcγ receptor to activate different pathways. Studies have proposed that the AMPA receptor bridges the neuronal pentraxins and tumor by mediating intracellular free concentration of calcium known to be vital for various downstream pathways. PTX3 modulates tumor cell adhesion and metastasis by interacting with the FGFR system. SAP and PTX4 share highly structural homology with CRP, but limited research has focused on their association with the tumor, similarly with the neuronal pentraxins. Tumor microenvironment and inflammation are two crucial components that influence tumor progression through active communication with each other (138, 139). The pentraxin family can both initiate inflammation and promote tumor progression.
Author Contributions
QC, ZL, and GX: offered the idea of this review, and acted as the mentors and guarantors of the review. ZW and XW: wrote the review. ZW, XW, and ZD: modified the review. ZW: drew the figures. HZ, MZ, and SF: offered modification advice and checked grammar. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. This work was supported by the National Nature Science Foundation of China (Nos. 81703622 and 81803582); the China Postdoctoral Science Foundation (No. 2018M63302); Hunan Provincial Natural Science Foundation of China (Nos. 2018JJ3838, 2019JJ50949, and 2020JJ8111); Grants from Xiangya Hospital Central South University postdoctoral foundation; Grants from Clinical medical technology innovation guidance program of Hunan Province (No. 2017SK50109); and grants from the research projects of Hunan Provincial Health Commission of China (Nos. C2019186 and B2019187).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2020.01757/full#supplementary-material
References
- 1.Hsu YC, Perin MS. Human neuronal pentraxin II (NPTX2): conservation, genomic structure, and chromosomal localization. Genomics. (1995) 28:220–7. 10.1006/geno.1995.1134 [DOI] [PubMed] [Google Scholar]
- 2.Liu Q, Tu T, Bai Z, Liu Z, Zhou S. Elevated plasma pentraxin 3: a potential cardiovascular risk factor? Med Hypotheses. (2011) 77:1068–70. 10.1016/j.mehy.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez OA, Kirakodu S, Novak MJ, Stromberg AJ, Orraca L, Gonzalez-Martinez J, et al. Comparative analysis of microbial sensing molecules in mucosal tissues with aging. Immunobiology. (2018) 223:279–87. 10.1016/j.imbio.2017.10.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson D, Pepys MB, Tickle I, Wood S. The structures of crystalline complexes of human serum amyloid P component with its carbohydrate ligand, the cyclic pyruvate acetal of galactose. J Mol Biol. (2002) 320:1081–6. 10.1016/S0022-2836(02)00514-4 [DOI] [PubMed] [Google Scholar]
- 5.Richards DB, Cookson LM, Berges AC, Barton SV, Lane T, Ritter JM, et al. Therapeutic clearance of amyloid by antibodies to serum amyloid P component. N Engl J Med. (2015) 373:1106–14. 10.1056/NEJMoa1504942 [DOI] [PubMed] [Google Scholar]
- 6.Richards DB, Cookson LM, Barton SV, Liefaard L, Lane T, Hutt DF, et al. Repeat doses of antibody to serum amyloid P component clear amyloid deposits in patients with systemic amyloidosis. Sci Transl Med. (2018) 10:eaan3128. 10.1126/scitranslmed.aan3128 [DOI] [PubMed] [Google Scholar]
- 7.Farhy-Tselnicker I, van Casteren ACM, Lee A, Chang VT, Aricescu AR, Allen NJ. Astrocyte-secreted glypican 4 regulates release of neuronal pentraxin 1 from axons to induce functional synapse formation. Neuron. (2017) 96:428–45.e13. 10.1016/j.neuron.2017.09.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ronca R, Di Salle E, Giacomini A, Leali D, Alessi P, Coltrini D, et al. Long pentraxin-3 inhibits epithelial-mesenchymal transition in melanoma cells. Mol Cancer Ther. (2013) 12:2760–71. 10.1158/1535-7163.MCT-13-0487 [DOI] [PubMed] [Google Scholar]
- 9.Ahmmed B, Khan MN, Nisar MA, Kampo S, Zheng Q, Li Y, et al. Tunicamycin enhances the suppressive effects of cisplatin on lung cancer growth through PTX3 glycosylation via AKT/NF-kappaB signaling pathway. Int J Oncol. (2019) 54:431–42. 10.3892/ijo.2018.4650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landskron G, De la Fuente M, Thuwajit P, Thuwajit C, Hermoso MA. Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res. (2014) 2014:149185. 10.1155/2014/149185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duan Y, Li Z, Cheng S, Chen Y, Zhang L, He J, et al. Nasopharyngeal carcinoma progression is mediated by EBER-triggered inflammation via the RIG-I pathway. Cancer Lett. (2015) 361:67–74. 10.1016/j.canlet.2015.02.037 [DOI] [PubMed] [Google Scholar]
- 12.Murata M. Inflammation and cancer. Environ Health Prev Med. (2018) 23:50. 10.1186/s12199-018-0740-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joyce JA, Fearon DT. T cell exclusion, immune privilege, and the tumor microenvironment. Science. (2015) 348:74–80. 10.1126/science.aaa6204 [DOI] [PubMed] [Google Scholar]
- 14.Wang M, Zhao J, Zhang L, Wei F, Lian Y, Wu Y, et al. Role of tumor microenvironment in tumorigenesis. J Cancer. (2017) 8:761–73. 10.7150/jca.17648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ronca R, Tamma R, Coltrini D, Ruggieri S, Presta M, Ribatti D. Fibroblast growth factor modulates mast cell recruitment in a murine model of prostate cancer. Oncotarget. (2017) 8:82583–92. 10.18632/oncotarget.19773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woo P, Korenberg JR, Whitehead AS. Characterization of genomic and complementary DNA sequence of human C-reactive protein, and comparison with the complementary DNA sequence of serum amyloid P component. J Biol Chem. (1985) 260:13384–8. [PubMed] [Google Scholar]
- 17.Lu J, Marjon KD, Mold C, Du Clos TW, Sun PD. Pentraxins and Fc receptors. Immunol Rev. (2012) 250:230–8. 10.1111/j.1600-065X.2012.01162.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vilahur G, Badimon L. Biological actions of pentraxins. Vascul Pharmacol. (2015) 73:38–44. 10.1016/j.vph.2015.05.001 [DOI] [PubMed] [Google Scholar]
- 19.Clark SE, Weiser JN. Microbial modulation of host immunity with the small molecule phosphorylcholine. Infect Immun. (2013) 81:392–401. 10.1128/IAI.01168-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ridker PM. From C-reactive protein to interleukin-6 to interleukin-1: moving upstream to identify novel targets for atheroprotection. Circ Res. (2016) 118:145–56. 10.1161/CIRCRESAHA.115.306656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang YA, Salinas I, Li J, Parra D, Bjork S, Xu Z, et al. IgT, a primitive immunoglobulin class specialized in mucosal immunity. Nat Immunol. (2010) 11:827–35. 10.1038/ni.1913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang J, Wezeman M, Zhang X, Lin P, Wang M, Qian J, et al. Human C-reactive protein binds activating Fcgamma receptors and protects myeloma tumor cells from apoptosis. Cancer Cell. (2007) 12:252–65. 10.1016/j.ccr.2007.08.008 [DOI] [PubMed] [Google Scholar]
- 23.Kim ES, Kim SY, Koh M, Lee HM, Kim K, Jung J, et al. C-reactive protein binds to integrin alpha2 and Fcgamma receptor I, leading to breast cell adhesion and breast cancer progression. Oncogene. (2018) 37:28–38. 10.1038/onc.2017.298 [DOI] [PubMed] [Google Scholar]
- 24.Aoki M, Fujishita T. Oncogenic roles of the PI3K/AKT/mTOR axis. Curr Top Microbiol Immunol. (2017) 407:153–89. 10.1007/82_2017_6 [DOI] [PubMed] [Google Scholar]
- 25.Chen W, Pilling D, Gomer RH. C-reactive protein (CRP) but not the related pentraxins serum amyloid P and PTX3 inhibits the proliferation and induces apoptosis of the leukemia cell line Mono Mac 6. BMC Immunol. (2017) 18:47 10.1186/s12865-017-0230-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Du J, Hu W, Yang C, Wang Y, Wang X, Yang P. C-reactive protein is associated with the development of tongue squamous cell carcinoma. Acta Biochim Biophys Sin. (2018) 50:238–45. 10.1093/abbs/gmy004 [DOI] [PubMed] [Google Scholar]
- 27.Yang J, Liu Z, Liu H, He J, Yang J, Lin P, et al. C-reactive protein promotes bone destruction in human myeloma through the CD32-p38 MAPK-Twist axis. Sci Signal. (2017) 10:eaan6282. 10.1126/scisignal.aan6282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morrison L, Laukkanen JA, Ronkainen K, Kurl S, Kauhanen J, Toriola AT. Inflammatory biomarker score and cancer: a population-based prospective cohort study. BMC Cancer. (2016) 16:80. 10.1186/s12885-016-2115-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nijaguna MB, Schroder C, Patil V, Shwetha SD, Hegde AS, Chandramouli BA, et al. Definition of a serum marker panel for glioblastoma discrimination and identification of Interleukin 1beta in the microglial secretome as a novel mediator of endothelial cell survival induced by C-reactive protein. J Proteomics. (2015) 128:251–61. 10.1016/j.jprot.2015.07.026 [DOI] [PubMed] [Google Scholar]
- 30.Nakayama T, Saito K, Kumagai J, Nakajima Y, Kijima T, Yoshida S, et al. Higher serum C-reactive protein level represents the immunosuppressive tumor microenvironment in patients with clear cell renal cell carcinoma. Clin Genitourin Cancer. (2018) 16:e1151–8. 10.1016/j.clgc.2018.07.027 [DOI] [PubMed] [Google Scholar]
- 31.Xu BB, Lu J, Zheng ZF, Xie JW, Wang JB, Lin JX, et al. The predictive value of the preoperative C-reactive protein-albumin ratio for early recurrence and chemotherapy benefit in patients with gastric cancer after radical gastrectomy: using randomized phase III trial data. Gastric Cancer. (2019) 22:1016–28. 10.1007/s10120-019-00936-w [DOI] [PubMed] [Google Scholar]
- 32.Krzystek-Korpacka M, Matusiewicz M, Diakowska D, Grabowski K, Blachut K, Kustrzeba-Wojcicka I, et al. Acute-phase response proteins are related to cachexia and accelerated angiogenesis in gastroesophageal cancers. Clin Chem Lab Med. (2008) 46:359–64. 10.1515/CCLM.2008.089 [DOI] [PubMed] [Google Scholar]
- 33.Kuribayashi K, Motoyama S, Sasaki T, Sato Y, Yoshino K, Wakita A, et al. C-reactive protein reduces the relative number of tumor-associated M2 macrophages and intratumoral angiogenesis in mice. Tohoku J Exp Med. (2014) 233:249–55. 10.1620/tjem.233.249 [DOI] [PubMed] [Google Scholar]
- 34.Ma Z, Qi Z, Shan Z, Li J, Yang J, Xu Z. The role of CRP and ATG9B expression in clear cell renal cell carcinoma. Biosci Rep. (2017) 37:BSR20171082. 10.1042/BSR20171082 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 35.Lust JA, Lacy MQ, Zeldenrust SR, Witzig TE, Moon-Tasson LL, Dinarello CA, et al. Reduction in C-reactive protein indicates successful targeting of the IL-1/IL-6 axis resulting in improved survival in early stage multiple myeloma. Am J Hematol. (2016) 91:571–4. 10.1002/ajh.24352 [DOI] [PubMed] [Google Scholar]
- 36.Saito K, Tatokoro M, Fujii Y, Iimura Y, Koga F, Kawakami S, et al. Impact of C-reactive protein kinetics on survival of patients with metastatic renal cell carcinoma. Eur Urol. (2009) 55:1145–53. 10.1016/j.eururo.2008.10.012 [DOI] [PubMed] [Google Scholar]
- 37.Xia WK, Wu X, Yu TH, Wu Y, Yao XJ, Hu H. Prognostic significance of lymphocyte-to-monocyte ratio and CRP in patients with nonmetastatic clear cell renal cell carcinoma: a retrospective multicenter analysis. Onco Targets Ther. (2016) 9:2759–67. 10.2147/OTT.S101458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dalpiaz O, Luef T, Seles M, Stotz M, Stojakovic T, Pummer K, et al. Critical evaluation of the potential prognostic value of the pretreatment-derived neutrophil-lymphocyte ratio under consideration of C-reactive protein levels in clear cell renal cell carcinoma. Br J Cancer. (2017) 116:85–90. 10.1038/bjc.2016.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaur RP, Rubal Banipal RPS, Vashistha R, Dhiman M, Munshi A. Association of elevated levels of C-reactive protein with breast cancer, breast cancer subtypes, and poor outcome. Curr Probl Cancer. (2019) 43:123–9. 10.1016/j.currproblcancer.2018.05.003 [DOI] [PubMed] [Google Scholar]
- 40.Liu ZQ, Chu L, Fang JM, Zhang X, Zhao HX, Chen YJ, et al. Prognostic role of C-reactive protein in prostate cancer: a systematic review and meta-analysis. Asian J Androl. (2014) 16:467–71. 10.4103/1008-682X.123686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muller DC, Larose TL, Hodge A, Guida F, Langhammer A, Grankvist K, et al. Circulating high sensitivity C reactive protein concentrations and risk of lung cancer: nested case-control study within Lung Cancer Cohort Consortium. BMJ. (2019) 364:k4981. 10.1136/bmj.k4981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. (2015) 22:803–10. 10.1245/s10434-014-4048-0 [DOI] [PubMed] [Google Scholar]
- 43.He X, Li JP, Liu XH, Zhang JP, Zeng QY, Chen H, et al. Prognostic value of C-reactive protein/albumin ratio in predicting overall survival of Chinese cervical cancer patients overall survival: comparison among various inflammation based factors. J Cancer. (2018) 9:1877–84. 10.7150/jca.23320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park MJ, Roh JL, Kim SB, Choi SH, Nam SY, Kim SY. Prognostic value of circulating biomarker score in advanced-stage head and neck squamous cell carcinoma. Eur J Cancer. (2018) 92:69–76. 10.1016/j.ejca.2018.01.069 [DOI] [PubMed] [Google Scholar]
- 45.Qin W, Yuan Q, Wu J, Yu H, Wang Y, Chen Q. Prognostic value of pre-therapy C-reactive protein level in diffuse large B-cell lymphoma: a meta-analysis. Leuk Lymphoma. (2019) 60:358–66. 10.1080/10428194.2018.1482540 [DOI] [PubMed] [Google Scholar]
- 46.Li W, Luo X, Liu Z, Chen Y, Li Z. Prognostic value of C-reactive protein levels in patients with bone neoplasms: A meta-analysis. PLoS ONE. (2018) 13:e0195769. 10.1371/journal.pone.0195769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Grote VA, Kaaks R, Nieters A, Tjonneland A, Halkjaer J, Overvad K, et al. Inflammation marker and risk of pancreatic cancer: a nested case-control study within the EPIC cohort. Br J Cancer. (2012) 106:1866–74. 10.1038/bjc.2012.172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Szkandera J, Stotz M, Absenger G, Stojakovic T, Samonigg H, Kornprat P, et al. Validation of C-reactive protein levels as a prognostic indicator for survival in a large cohort of pancreatic cancer patients. Br J Cancer. (2014) 110:183–8. 10.1038/bjc.2013.701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chan AT, Ogino S, Giovannucci EL, Fuchs CS. Inflammatory markers are associated with risk of colorectal cancer and chemopreventive response to anti-inflammatory drugs. Gastroenterology. (2011) 140:799–808, quiz e711. 10.1053/j.gastro.2010.11.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nimptsch K, Aleksandrova K, Boeing H, Janke J, Lee YA, Jenab M, et al. Association of CRP genetic variants with blood concentrations of C-reactive protein and colorectal cancer risk. Int J Cancer. (2015) 136:1181–92. 10.1002/ijc.29086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Farsad-Naeimi A, Alizadeh M, Esfahani A, Darvish Aminabad E. Effect of fisetin supplementation on inflammatory factors and matrix metalloproteinase enzymes in colorectal cancer patients. Food Funct. (2018) 9:2025–31. 10.1039/C7FO01898C [DOI] [PubMed] [Google Scholar]
- 52.Xi D, Luo T, Xiong H, Liu J, Lu H, Li M, et al. SAP: structure, function, and its roles in immune-related diseases. Int J Cardiol. (2015) 187:20–6. 10.1016/j.ijcard.2015.03.179 [DOI] [PubMed] [Google Scholar]
- 53.Emsley J, White HE, O'Hara BP, Oliva G, Srinivasan N, Tickle IJ, et al. Structure of pentameric human serum amyloid P component. Nature. (1994) 367:338–45. 10.1038/367338a0 [DOI] [PubMed] [Google Scholar]
- 54.Mikolajek H, Kolstoe SE, Pye VE, Mangione P, Pepys MB, Wood SP. Structural basis of ligand specificity in the human pentraxins, C-reactive protein and serum amyloid P component. J Mol Recognit. (2011) 24:371–7. 10.1002/jmr.1090 [DOI] [PubMed] [Google Scholar]
- 55.Hind CR, Collins PM, Renn D, Cook RB, Caspi D, Baltz ML, et al. Binding specificity of serum amyloid P component for the pyruvate acetal of galactose. J Exp Med. (1984) 159:1058–69. 10.1084/jem.159.4.1058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang W, Xu W, Xiong S. Macrophage differentiation and polarization via phosphatidylinositol 3-kinase/Akt-ERK signaling pathway conferred by serum amyloid P component. J Immunol. (2011) 187:1764–77. 10.4049/jimmunol.1002315 [DOI] [PubMed] [Google Scholar]
- 57.Cox N, Pilling D, Gomer RH. Serum amyloid P: a systemic regulator of the innate immune response. J Leukoc Biol. (2014) 96:739–43. 10.1189/jlb.1MR0114-068R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bickerstaff MC, Botto M, Hutchinson WL, Herbert J, Tennent GA, Bybee A, et al. Serum amyloid P component controls chromatin degradation and prevents antinuclear autoimmunity. Nat Med. (1999) 5:694–7. 10.1038/9544 [DOI] [PubMed] [Google Scholar]
- 59.Jacobs R, Tshehla E, Malherbe S, Kriel M, Loxton AG, Stanley K, et al. Host biomarkers detected in saliva show promise as markers for the diagnosis of pulmonary tuberculosis disease and monitoring of the response to tuberculosis treatment. Cytokine. (2016) 81:50–6. 10.1016/j.cyto.2016.02.004 [DOI] [PubMed] [Google Scholar]
- 60.Chantrathammachart P, Mackman N, Sparkenbaugh E, Wang JG, Parise LV, Kirchhofer D, et al. Tissue factor promotes activation of coagulation and inflammation in a mouse model of sickle cell disease. Blood. (2012) 120:636–46. 10.1182/blood-2012-04-424143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhao J, Chi A, Mao R, Hu G, Ji M. Serum amyloid P-component level may be a biomarker for lung toxicities and overall survival after thoracic radiotherapy for non-small cell lung cancer. Clin Lab. (2016) 62:2183–90. 10.7754/Clin.Lab.2016.160411 [DOI] [PubMed] [Google Scholar]
- 62.Omeis IA, Hsu YC, Perin MS. Mouse and human neuronal pentraxin 1 (NPTX1): conservation, genomic structure, and chromosomal localization. Genomics. (1996) 36:543–5. 10.1006/geno.1996.0503 [DOI] [PubMed] [Google Scholar]
- 63.Dodds DC, Omeis IA, Cushman SJ, Helms JA, Perin MS. Neuronal pentraxin receptor, a novel putative integral membrane pentraxin that interacts with neuronal pentraxin 1 and 2 and taipoxin-associated calcium-binding protein 49. J Biol Chem. (1997) 272:21488–94. 10.1074/jbc.272.34.21488 [DOI] [PubMed] [Google Scholar]
- 64.Du Clos TW. Pentraxins: structure, function, and role in inflammation. ISRN Inflamm. (2013) 2013:379040. 10.1155/2013/379040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thatipamula S, Al Rahim M, Zhang J, Hossain MA. Genetic deletion of neuronal pentraxin 1 expression prevents brain injury in a neonatal mouse model of cerebral hypoxia-ischemia. Neurobiol Dis. (2015) 75:15–30. 10.1016/j.nbd.2014.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huo L, Wang B, Zheng M, Zhang Y, Xu J, Yang G, et al. miR-128-3p inhibits glioma cell proliferation and differentiation by targeting NPTX1 through IRS-1/PI3K/AKT signaling pathway. Exp Ther Med. (2019) 17:2921–30. 10.3892/etm.2019.7284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Guzeloglu-Kayisli O, Basar M, Shapiro JP, Semerci N, Huang JS, Schatz F, et al. Long-acting progestin-only contraceptives enhance human endometrial stromal cell expressed neuronal pentraxin-1 and reactive oxygen species to promote endothelial cell apoptosis. J Clin Endocrinol Metab. (2014) 99:E1957–66. 10.1210/jc.2014-1770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Peng X, Pan K, Zhao W, Zhang J, Yuan S, Wen X, et al. NPTX1 inhibits colon cancer cell proliferation through down-regulating cyclin A2 and CDK2 expression. Cell Biol Int. (2018) 42:589–97. 10.1002/cbin.10935 [DOI] [PubMed] [Google Scholar]
- 69.Boles NC, Hirsch SE, Le S, Corneo B, Najm F, Minotti AP, et al. NPTX1 regulates neural lineage specification from human pluripotent stem cells. Cell Rep. (2014) 6:724–36. 10.1016/j.celrep.2014.01.026 [DOI] [PubMed] [Google Scholar]
- 70.Xu C, Tian G, Jiang C, Xue H, Kuerbanjiang M, Sun L, et al. NPTX2 promotes colorectal cancer growth and liver metastasis by the activation of the canonical Wnt/beta-catenin pathway via FZD6. Cell Death Dis. (2019) 10:217. 10.1038/s41419-019-1467-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shukla S, Pia Patric IR, Thinagararjan S, Srinivasan S, Mondal B, Hegde AS, et al. A DNA methylation prognostic signature of glioblastoma: identification of NPTX2-PTEN-NF-kappaB nexus. Cancer Res. (2013) 73:6563–73. 10.1158/0008-5472.CAN-13-0298 [DOI] [PubMed] [Google Scholar]
- 72.Liu H, Jiang Q, Ju Z, Guan S, He B. Pentraxin 3 promotes cardiac differentiation of mouse embryonic stem cells through JNK signaling pathway. Cell Biol Int. (2018) 42:1556–63. 10.1002/cbin.11049 [DOI] [PubMed] [Google Scholar]
- 73.Xiao Y, Yang N, Zhang Q, Wang Y, Yang S, Liu Z. Pentraxin 3 inhibits acute renal injury-induced interstitial fibrosis through suppression of IL-6/Stat3 pathway. Inflammation. (2014) 37:1895–901. 10.1007/s10753-014-9921-2 [DOI] [PubMed] [Google Scholar]
- 74.Chan SH, Tsai JP, Shen CJ, Liao YH, Chen BK. Oleate-induced PTX3 promotes head and neck squamous cell carcinoma metastasis through the up-regulation of vimentin. Oncotarget. (2017) 8:41364–78. 10.18632/oncotarget.17326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sia GM, Beique JC, Rumbaugh G, Cho R, Worley PF, Huganir RL. Interaction of the N-terminal domain of the AMPA receptor GluR4 subunit with the neuronal pentraxin NP1 mediates GluR4 synaptic recruitment. Neuron. (2007) 55:87–102. 10.1016/j.neuron.2007.06.020 [DOI] [PubMed] [Google Scholar]
- 76.Cummings DM, Benway TA, Ho H, Tedoldi A, Fernandes Freitas MM, Shahab L, et al. Neuronal and peripheral pentraxins modify glutamate release and may interact in blood-brain barrier failure. Cereb Cortex. (2017) 27:3437–48. 10.1093/cercor/bhx046 [DOI] [PubMed] [Google Scholar]
- 77.Lee SJ, Wei M, Zhang C, Maxeiner S, Pak C, Calado Botelho S, et al. Presynaptic neuronal pentraxin receptor organizes excitatory and inhibitory synapses. J Neurosci. (2017) 37:1062–80. 10.1523/JNEUROSCI.2768-16.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rajkumar AP, Christensen JH, Mattheisen M, Jacobsen I, Bache I, Pallesen J, et al. Analysis of t(9;17)(q33.2;q25.3) chromosomal breakpoint regions and genetic association reveals novel candidate genes for bipolar disorder. Bipolar Disord. (2015) 17:205–11. 10.1111/bdi.12239 [DOI] [PubMed] [Google Scholar]
- 79.Liu H, Kong X, Chen F. Mkrn3 functions as a novel ubiquitin E3 ligase to inhibit Nptx1 during puberty initiation. Oncotarget. (2017) 8:85102–9. 10.18632/oncotarget.19347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li T, Mamillapalli R, Ding S, Chang H, Liu ZW, Gao XB, et al. Endometriosis alters brain electrophysiology, gene expression and increases pain sensitization, anxiety, and depression in female mice. Biol Reprod. (2018) 99:349–59. 10.1093/biolre/ioy035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Strauss J, McGregor S, Freeman N, Tiwari A, George CJ, Kovacs M, et al. Association study of early-immediate genes in childhood-onset mood disorders and suicide attempt. Psychiatry Res. (2012) 197:49–54. 10.1016/j.psychres.2011.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Manchia M, Piras IS, Huentelman MJ, Pinna F, Zai CC, Kennedy JL. Pattern of gene expression in different stages of schizophrenia: down-regulation of NPTX2 gene revealed by a meta-analysis of microarray datasets. Eur Neuropsychopharmacol. (2017) 27:1054–63. 10.1016/j.euroneuro.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 83.Begcevic I, Tsolaki M, Brinc D, Brown M, Martinez-Morillo E, Lazarou I, et al. Neuronal pentraxin receptor-1 is a new cerebrospinal fluid biomarker of Alzheimer's disease progression. F1000Res. (2018) 7:1012. 10.12688/f1000research.15095.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Goetzl EJ, Abner EL, Jicha GA, Kapogiannis D, Schwartz JB. Declining levels of functionally specialized synaptic proteins in plasma neuronal exosomes with progression of Alzheimer's disease. FASEB J. (2018) 32:888–93. 10.1096/fj.201700731R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Charbonnier-Beaupel F, Malerbi M, Alcacer C, Tahiri K, Carpentier W, Wang C, et al. Gene expression analyses identify Narp contribution in the development of L-DOPA-induced dyskinesia. J Neurosci. (2015) 35:96–111. 10.1523/JNEUROSCI.5231-13.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Li J, Sun Y, Chen J. Transcriptome sequencing in a 6-hydroxydopamine rat model of Parkinson's disease. Genes Genet Syst. (2019) 94:61–9. 10.1266/ggs.18-00036 [DOI] [PubMed] [Google Scholar]
- 87.Qu Z, D'Mello SR. Proteomic analysis identifies NPTX1 and HIP1R as potential targets of histone deacetylase-3-mediated neurodegeneration. Exp Biol Med. (2018) 243:627–38. 10.1177/1535370218761149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zook P, Pathak HB, Belinsky MG, Gersz L, Devarajan K, Zhou Y, et al. Combination of imatinib mesylate and AKT inhibitor provides synergistic effects in preclinical study of gastrointestinal stromal tumor. Clin Cancer Res. (2017) 23:171–80. 10.1158/1078-0432.CCR-16-0529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tyburczy ME, Kotulska K, Pokarowski P, Mieczkowski J, Kucharska J, Grajkowska W, et al. Novel proteins regulated by mTOR in subependymal giant cell astrocytomas of patients with tuberous sclerosis complex and new therapeutic implications. Am J Pathol. (2010) 176:1878–90. 10.2353/ajpath.2010.090950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Skiriute D, Vaitkiene P, Asmoniene V, Steponaitis G, Deltuva VP, Tamasauskas A. Promoter methylation of AREG, HOXA11, hMLH1, NDRG2, NPTX2 and Tes genes in glioblastoma. J Neurooncol. (2013) 113:441–9. 10.1007/s11060-013-1133-3 [DOI] [PubMed] [Google Scholar]
- 91.Carlson MR, Pope WB, Horvath S, Braunstein JG, Nghiemphu P, Tso CL, et al. Relationship between survival and edema in malignant gliomas: role of vascular endothelial growth factor and neuronal pentraxin 2. Clin Cancer Res. (2007) 13:2592–8. 10.1158/1078-0432.CCR-06-2772 [DOI] [PubMed] [Google Scholar]
- 92.Zhang L, Gao J, Li L, Li Z, Du Y, Gong Y. The neuronal pentraxin II gene (NPTX2) inhibit proliferation and invasion of pancreatic cancer cells in vitro. Mol Biol Rep. (2011) 38:4903–11. 10.1007/s11033-010-0632-y [DOI] [PubMed] [Google Scholar]
- 93.Zhang L, Gao J, Li Z, Gong Y. Neuronal pentraxin II (NPTX2) is frequently down-regulated by promoter hypermethylation in pancreatic cancers. Dig Dis Sci. (2012) 57:2608–14. 10.1007/s10620-012-2202-8 [DOI] [PubMed] [Google Scholar]
- 94.von Roemeling CA, Radisky DC, Marlow LA, Cooper SJ, Grebe SK, Anastasiadis PZ, et al. Neuronal pentraxin 2 supports clear cell renal cell carcinoma by activating the AMPA-selective glutamate receptor-4. Cancer Res. (2014) 74:4796–810. 10.1158/0008-5472.CAN-14-0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schrodter S, Braun M, Syring I, Klumper N, Deng M, Schmidt D, et al. Identification of the dopamine transporter SLC6A3 as a biomarker for patients with renal cell carcinoma. Mol Cancer. (2016) 15:10. 10.1186/s12943-016-0495-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yang N, Eijsink JJ, Lendvai A, Volders HH, Klip H, Buikema HJ, et al. Methylation markers for CCNA1 and C13ORF18 are strongly associated with high-grade cervical intraepithelial neoplasia and cervical cancer in cervical scrapings. Cancer Epidemiol Biomarkers Prev. (2009) 18:3000–7. 10.1158/1055-9965.EPI-09-0405 [DOI] [PubMed] [Google Scholar]
- 97.Zhou C, Qin Y, Xie Z, Zhang J, Yang M, Li S, et al. NPTX1 is a novel epigenetic regulation gene and associated with prognosis in lung cancer. Biochem Biophys Res Commun. (2015) 458:381–6. 10.1016/j.bbrc.2015.01.124 [DOI] [PubMed] [Google Scholar]
- 98.Alholle A, Brini AT, Gharanei S, Vaiyapuri S, Arrigoni E, Dallol A, et al. Functional epigenetic approach identifies frequently methylated genes in Ewing sarcoma. Epigenetics. (2013) 8:1198–204. 10.4161/epi.26266 [DOI] [PubMed] [Google Scholar]
- 99.Bartolini A, Di Paolo D, Noghero A, Murgia D, Sementa AR, Cilli M, et al. The neuronal pentraxin-2 pathway is an unrecognized target in human neuroblastoma, which also offers prognostic value in patients. Cancer Res. (2015) 75:4265–71. 10.1158/0008-5472.CAN-15-0649 [DOI] [PubMed] [Google Scholar]
- 100.Poulsen TT, Pedersen N, Perin MS, Hansen CK, Poulsen HS. Specific sensitivity of small cell lung cancer cell lines to the snake venom toxin taipoxin. Lung Cancer. (2005) 50:329–37. 10.1016/j.lungcan.2005.06.011 [DOI] [PubMed] [Google Scholar]
- 101.Yue W, Wang T, Zachariah E, Lin Y, Yang CS, Xu Q, et al. Transcriptomic analysis of pancreatic cancer cells in response to metformin and aspirin: an implication of synergy. Sci Rep. (2015) 5:13390. 10.1038/srep13390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Karagkounis G, Thai L, DeVecchio J, Gantt GA, Duraes L, Pai RK, et al. NPTX2 is associated with neoadjuvant therapy response in rectal cancer. J Surg Res. (2016) 202:112–7. 10.1016/j.jss.2015.12.042 [DOI] [PubMed] [Google Scholar]
- 103.de Groot J, Sontheimer H. Glutamate and the biology of gliomas. Glia. (2011) 59:1181–9. 10.1002/glia.21113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Radin DP, Patel P. A current perspective on the oncopreventive and oncolytic properties of selective serotonin reuptake inhibitors. Biomed Pharmacother. (2017) 87:636–9. 10.1016/j.biopha.2017.01.024 [DOI] [PubMed] [Google Scholar]
- 105.Breviario F, d'Aniello EM, Golay J, Peri G, Bottazzi B, Bairoch A, et al. Interleukin-1-inducible genes in endothelial cells. Cloning of a new gene related to C-reactive protein and serum amyloid P component. J Biol Chem. (1992) 267:22190–7. [PubMed] [Google Scholar]
- 106.Lee GW, Lee TH, Vilcek J. TSG-14, a tumor necrosis factor- and IL-1-inducible protein, is a novel member of the pentaxin family of acute phase proteins. J Immunol. (1993) 150:1804–12. [PubMed] [Google Scholar]
- 107.Presta M, Camozzi M, Salvatori G, Rusnati M. Role of the soluble pattern recognition receptor PTX3 in vascular biology. J Cell Mol Med. (2007) 11:723–38. 10.1111/j.1582-4934.2007.00061.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Moalli F, Jaillon S, Inforzato A, Sironi M, Bottazzi B, Mantovani A, et al. Pathogen recognition by the long pentraxin PTX3. J Biomed Biotechnol. (2011) 2011:830421. 10.1155/2011/830421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Martinez de la Torre Y, Fabbri M, Jaillon S, Bastone A, Nebuloni M, Vecchi A, et al. Evolution of the pentraxin family: the new entry PTX4. J Immunol. (2010) 184:5055–64. 10.4049/jimmunol.0901672 [DOI] [PubMed] [Google Scholar]
- 110.Mantovani A, Garlanda C, Doni A, Bottazzi B. Pentraxins in innate immunity: from C-reactive protein to the long pentraxin PTX3. J Clin Immunol. (2008) 28:1–13. 10.1007/s10875-007-9126-7 [DOI] [PubMed] [Google Scholar]
- 111.Ma YJ, Doni A, Hummelshoj T, Honore C, Bastone A, Mantovani A, et al. Synergy between ficolin-2 and pentraxin 3 boosts innate immune recognition and complement deposition. J Biol Chem. (2009) 284:28263–75. 10.1074/jbc.M109.009225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bottazzi B, Vouret-Craviari V, Bastone A, De Gioia L, Matteucci C, Peri G, et al. Multimer formation and ligand recognition by the long pentraxin PTX3. Similarities and differences with the short pentraxins C-reactive protein and serum amyloid P component. J Biol Chem. (1997) 272:32817–23. 10.1074/jbc.272.52.32817 [DOI] [PubMed] [Google Scholar]
- 113.Inforzato A, Peri G, Doni A, Garlanda C, Mantovani A, Bastone A, et al. Structure and function of the long pentraxin PTX3 glycosidic moiety: fine-tuning of the interaction with C1q and complement activation. Biochemistry. (2006) 45:11540–51. 10.1021/bi0607453 [DOI] [PubMed] [Google Scholar]
- 114.Nauta AJ, Bottazzi B, Mantovani A, Salvatori G, Kishore U, Schwaeble WJ, et al. Biochemical and functional characterization of the interaction between pentraxin 3 and C1q. Eur J Immunol. (2003) 33:465–73. 10.1002/immu.200310022 [DOI] [PubMed] [Google Scholar]
- 115.Bottazzi B, Inforzato A, Messa M, Barbagallo M, Magrini E, Garlanda C, et al. The pentraxins PTX3 and SAP in innate immunity, regulation of inflammation and tissue remodelling. J Hepatol. (2016) 64:1416–27. 10.1016/j.jhep.2016.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Presta M, Foglio E, Churruca Schuind A, Ronca R. Long pentraxin-3 modulates the angiogenic activity of fibroblast growth factor-2. Front Immunol. (2018) 9:2327. 10.3389/fimmu.2018.02327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Thomas C, Henry W, Cuiffo BG, Collmann AY, Marangoni E, Benhamo V, et al. Pentraxin-3 is a PI3K signaling target that promotes stem cell-like traits in basal-like breast cancers. Sci Signal. (2017) 10:eaah4674. 10.1126/scisignal.aah4674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ying TH, Lee CH, Chiou HL, Yang SF, Lin CL, Hung CH, et al. Knockdown of Pentraxin 3 suppresses tumorigenicity and metastasis of human cervical cancer cells. Sci Rep. (2016) 6:29385. 10.1038/srep29385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pfeifer GP. Defining driver DNA methylation changes in human cancer. Int J Mol Sci. (2018) 19:1166. 10.3390/ijms19041166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Giacomini A, Ghedini GC, Presta M, Ronca R. Long pentraxin 3: A novel multifaceted player in cancer. Biochim Biophys Acta Rev Cancer. (2018) 1869:53–63. 10.1016/j.bbcan.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 121.Kampo S, Ahmmed B, Zhou T, Owusu L, Anabah TW, Doudou NR, et al. Scorpion venom analgesic peptide, BmK AGAP inhibits stemness, and epithelial-mesenchymal transition by down-regulating PTX3 in breast cancer. Front Oncol. (2019) 9:21. 10.3389/fonc.2019.00021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ronca R, Alessi P, Coltrini D, Di Salle E, Giacomini A, Leali D, et al. Long pentraxin-3 as an epithelial-stromal fibroblast growth factor-targeting inhibitor in prostate cancer. J Pathol. (2013) 230:228–38. 10.1002/path.4181 [DOI] [PubMed] [Google Scholar]
- 123.Basile A, Moschetta M, Ditonno P, Ria R, Marech I, De Luisi A, et al. Pentraxin 3. (PTX3) inhibits plasma cell/stromal cell cross-talk in the bone marrow of multiple myeloma patients. J Pathol. (2013) 229:87–98. 10.1002/path.4081 [DOI] [PubMed] [Google Scholar]
- 124.Leali D, Alessi P, Coltrini D, Ronca R, Corsini M, Nardo G, et al. Long pentraxin-3 inhibits FGF8b-dependent angiogenesis and growth of steroid hormone-regulated tumors. Mol Cancer Ther. (2011) 10:1600–10. 10.1158/1535-7163.MCT-11-0286 [DOI] [PubMed] [Google Scholar]
- 125.Locatelli M, Ferrero S, Martinelli Boneschi F, Boiocchi L, Zavanone M, Maria Gaini S, et al. The long pentraxin PTX3 as a correlate of cancer-related inflammation and prognosis of malignancy in gliomas. J Neuroimmunol. (2013) 260:99–106. 10.1016/j.jneuroim.2013.04.009 [DOI] [PubMed] [Google Scholar]
- 126.Ma D, Zong Y, Zhu ST, Wang YJ, Li P, Zhang ST. Inhibitory role of pentraxin-3 in esophageal squamous cell carcinoma. Chin Med J. (2016) 129:2233–40. 10.4103/0366-6999.189921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zambirinis CP, Pushalkar S, Saxena D, Miller G. Pancreatic cancer, inflammation, and microbiome. Cancer J. (2014) 20:195–202. 10.1097/PPO.0000000000000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Choi B, Lee EJ, Park YS, Kim SM, Kim EY, Song Y, et al. Pentraxin-3 silencing suppresses gastric cancer-related inflammation by inhibiting chemotactic migration of macrophages. Anticancer Res. (2015) 35:2663–8. Available online at: http://ar.iiarjournals.org/content/35/5/2663.long [PubMed] [Google Scholar]
- 129.Tsuji S, Midorikawa Y, Seki M, Takayama T, Sugiyama Y, Aburatani H. Network-based analysis for identification of candidate genes for colorectal cancer progression. Biochem Biophys Res Commun. (2016) 476:534–40. 10.1016/j.bbrc.2016.05.158 [DOI] [PubMed] [Google Scholar]
- 130.Bonavita E, Gentile S, Rubino M, Maina V, Papait R, Kunderfranco P, et al. PTX3 is an extrinsic oncosuppressor regulating complement-dependent inflammation in cancer. Cell. (2015) 160:700–14. 10.1016/j.cell.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 131.Dahan R, Sega E, Engelhardt J, Selby M, Korman Alan J, Ravetch Jeffrey V. FcγRs modulate the anti-tumor activity of antibodies targeting the PD-1/PD-L1 axis. Cancer Cell. (2015) 28:285–95. 10.1016/j.ccell.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 132.Brandsma AM, Bondza S, Evers M, Koutstaal R, Nederend M, Jansen JHM, et al. Potent Fc receptor signaling by IgA leads to superior killing of cancer cells by neutrophils compared to IgG. Front Immunol. (2019) 10:704. 10.3389/fimmu.2019.00704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sanseviero E. NK cell-Fc receptors advance tumor immunotherapy. J Clin Med. (2019) 8:1667. 10.3390/jcm8101667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Liu Q, Wang XY, Qin YY, Yan XL, Chen HM, Huang QD, et al. SPOCD1 promotes the proliferation and metastasis of glioma cells by up-regulating PTX3. Am J Cancer Res. (2018) 8:624–35. Available online at: http://www.ajcr.us/files/ajcr0067117.pdf [PMC free article] [PubMed] [Google Scholar]
- 135.Chang WC, Wu SL, Huang WC, Hsu JY, Chan SH, Wang JM, et al. PTX3 gene activation in EGF-induced head and neck cancer cell metastasis. Oncotarget. (2015) 6:7741–57. 10.18632/oncotarget.3482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Fang S, Sui D, Wang Y, Liu H, Chiang YJ, Ross MI, et al. Association of vitamin D levels with outcome in patients with melanoma after adjustment for C-reactive protein. J Clin Oncol. (2016) 34:1741–7. 10.1200/JCO.2015.64.1357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.She S, Xiang Y, Yang M, Ding X, Liu X, Ma L, et al. C-reactive protein is a biomarker of AFP-negative HBV-related hepatocellular carcinoma. Int J Oncol. (2015) 47:543–54. 10.3892/ijo.2015.3042 [DOI] [PubMed] [Google Scholar]
- 138.Huang A, Cao S, Tang L. The tumor microenvironment and inflammatory breast cancer. J Cancer. (2017) 8:1884–91. 10.7150/jca.17595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Xie X, Yang M, Ding Y, Chen J. Microbial infection, inflammation and epithelial ovarian cancer. Oncol Lett. (2017) 14:1911–9. 10.3892/ol.2017.6388 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.