Abstract
Smoking during pregnancy can lead to serious health consequences. Given such health risks, an understanding of factors that influence maternal smoking behaviors during pregnancy is critical. The objective of this study is to assess the relationship between tobacco store density, neighborhood socioeconomic status, and neighborhood rates of maternal smoking during pregnancy. Fifty-five community areas in Baltimore City were summarized using data from the Neighborhood Health Profiles. Associations between tobacco store density and smoking while pregnant in a community were determined using Moran's I and spatial regression analyses to account for autocorrelation. The fully adjusted model took into account the following community-level socioeconomic variables as covariates: neighborhood median income, percentage of those living in poverty, percentage of uninsured, and percentage of persons with at least a college degree. In regards to the findings, the percentage of women by community area who identified as actively smoking while pregnant was 10.4% ± 5.8%. The tobacco store density was 21.0 ± 12.7 per 10,000 persons (range 0.0 - 49.1 tobacco store density per 10,000 persons). In the adjusted model, an increase in density of 1 tobacco store per 10,000 persons was associated with a 10% increase in women who reported smoking during pregnancy (β = 0.10, p = 0.04). In conclusion, tobacco store density and neighborhood socioeconomic factors were associated with prevalence of maternal smoking while pregnant. These findings support the need to further assess and develop interventions to reduce the impact of tobacco store density on smoking behaviors and health risks in communities.
Keywords: smoking, pregnancy, community health
INTRODUCTION
Active smoking among women who are pregnant continues to be prevalent, with an estimate of 1 in 4 women worldwide smoking while pregnant.1 Certain populations have even higher rates, such as indigenous communities in industrialized nations.2 In the United States (US), the prevalence of women who smoke while pregnant varies depending on the region of the country, with some areas as low as 5.1% and some as high as 28.7% (with overall prevalence at 10.7%).3,4 In addition to the geographic variations, other sociodemographic variables have been found to be associated with smoking during pregnancy, such as limited formal education, unmarried, and of limited economic status.3 Given there are negative health consequences of smoking while pregnant5,6 and behavior and disease amass through social networks, exploring non-medical factors that influence the prevalence of smoking during pregnancy is a critical step to designing interventions to improve health of mothers and unborn children.
The socioeconomic status of a neighborhood has an association on the health and health outcomes of its individual.7,8 Certain factors that compose a neighborhood, specifically, the density of stores that sell tobacco, have been found to be associated with negative health behaviors (smoking and inability to quit smoking9,10) and health outcomes (lower life expectancy11). Such neighborhood factors hold significant value due to their ability to change and, in turn, to potentially influence the health of the region.
The objective of this study is to assess the relationship between tobacco store density, neighborhood socioeconomic status and neighborhood rates of maternal smoking during pregnancy in Baltimore City, a large, US urban area. It is hypothesized that neighborhoods with higher densities of tobacco stores will exhibit higher rates of women who smoke while pregnant.
METHODS
The Baltimore City data were received through the 2017 Neighborhood Health Profiles12, a data set that compiles a variety of demographic information at the individual and community level, as well as health outcome data. At the time of reporting the 2017 Neighborhood Health Profiles data, the population of Baltimore City was 622,454, with 62.6% of the population aged 0 to 44 years and 52.9% of the population was female.
The Baltimore City Health Department organizes census tracts into community statistical areas (CSAs). Each CSA represents a neighborhood of similar social, demographic and economic characteristics with a total population ranging from 5000 to 20000 persons. The CSA model allows for the collection and aggregation of a wide range of data for a relatively stable geography over a defined period of time. For instance, for the 2017 Neighborhood Health Profiles data, a total of 55 CSAs were identified for Baltimore City with data ranging from 2011-2016. Moving forward, we will substitute the term CSA with the term “neighborhood”. The study was exempt from formal approval by Institutional Review Board at Johns Hopkins School of Medicine as the data analyzed is publicaly available and all actions undertaken by the authors were in accordance with the Declaration of Helsinki.
Sociodemographic variables collected from the Neighborhood Health Profiles included racial make-up of a neighborhood, educational status (defined as the percentage of completion of a Bachelor’s degree or more and aged 25 and older in a neighborhood), median neighborhood income, percentage of uninsured in a neighborhood, and family poverty rate of a neighborhood. Further, we obtained tobacco store density values for each neighborhood. A tobacco store is defined as an establishment that sells cigarettes or other tobacco products such as cigars, pipe tobacco, chewing tobacco, roll-your-own tobacco, snuff, snus, or other smokeless tobacco products. The designation is granted by the Maryland Office of the Comptroller, who supplied the data for the Neighborhood Healthy Profile. . At the time of this data collection, the sale of electronic cigarettes was not included in the definition for a tobacco store. Each tobacco store density is represented as a store per 10000 persons of the neighborhood. For tobacco stores, data were geocoded then aggregated into specific neighborhoods based on spatial location with the Community Statistical Area shapefile, allowing each CSA to have a count of tobacco stores within each CSA. This was performed by the Baltimore City Health Department using Esri’s ArcGIS 10.1 to execute geocoding and geoprocessing analyses.
Neighborhood Health Profiles also included data on percentage of women who reported smoking while pregnant, percentage of births classified as low birthweight (less than 5 pounds 8 ounces), percentage of live births occurring preterm (less than 37 weeks gestation), and infant mortality rate per 1000 live births. Smoking while pregnant did not differentiate at what time during the pregnancy a mother was identified as smoking (e.g. first trimester, second trimester, and/or third trimester). Information for smoking while pregnant was collected by the Maryland Department of Health and Mental Hygiene Vital Statistics Administration between 2010-2014. This variable was collected from birth certificates, where prenatal care, smoking during pregnancy, and maternal body mass index are reported.
Summary data are represented as mean ± standard deviation or median (interquartile range) where appropriate for continuous variables and by value (percentage) for categorical variables. Spatial regression analyses were used to evaluate for spatial autocorrelation for tobacco store densities, given that there is a concern for a clustering effect for tobacco store densities when using cross-sectional data13. Using Moran’s I and spatial regression, spatial autocorrelation was identified for tobacco store densities when evaluating its association with the defined outcome variables in both the unadjusted and adjusted models. For consistency across all models, Moran’s I and spatial regression analyses were run for all unadjusted models and adjusted models. Tobacco store was the sole density measure and in adjusted models, the additional covariates included community-level socioeconomic factors: neighborhood median income, family poverty rate, percentage of uninsured, race (African American), and percentage of persons with at least a Bachelor’s degree. When comparing Moran’s I and spatial regression models with linear regression models (without adjustment for autocorrelation), the results were similar; therefore, only results for Moran’s I and spatial regression models are presented. One neighborhood had significantly higher tobacco store density compared with others and sensitivity analysis was performed excluding this outlier from analyses. Statistical analyses were conducted with R software (V.0.99.903) with a statistical significance level of 0.05.
RESULTS
Neighborhood Characteristics
The collective median household income of the Baltimore City 55 neighborhoods was $38655 (IQR $32531, $54477) with a median poverty rate of 28.4% (IQR 13.5%, 38.8%). The percentage of persons 18 years and older with no healthcare insurance was 12.1% (IQR 9.2%, 14.6%). The percentage of residents 25 or older with a Bachelor’s degree or more was 19.5% (IQR 11.1%, 39.2%). The median tobacco store density was 18.70 (IQR 12.10, 30.65) per 10000 persons, with the highest concentrations of tobacco stores located in the center of Baltimore City.
In regards to pregnancy-related outcomes, the percentage of women who smoked while pregnant was 10.4% ± 5.8%. The percentage of low birthweight births, defined by weighing less than 5 pounds and 8 ounces, was 11.63% ± 3.04%, while the percentage of preterm births, defined as birth before 37 weeks gestation, was 12.44% ± 2.83%. The infant mortality rate was 9.50 ± 4.52 per 1000 live births.
Moran’s I and Spatial Regression Unadjusted Models
In unadjusted models, tobacco store density was associated with higher percentage of smoking while pregnant (β = 0.22, p<0.001) (Table). There was statistically significant correlation of tobacco store densities and smoking while pregnant (r2=0.22, p<0.001; Figure). Further, tobacco store densities were associated with a higher rate of infant mortality per 1000 live births (β = 0.11, p=0.026). There were supportive trends, but tobacco store densities were not found to be significantly associated with low birthweight births (β = 0.06, p=0.080) and preterm births (β = 0.06, p=0.060).
Table.
Moran’s I and spatial regression model for smoking while pregnant and tobacco store density for the 55 neighborhoods of Baltimore City, unadjusted and adjusted models with coefficient (95% confidence interval).
| Characteristic | ||||
|---|---|---|---|---|
| Unadjusted | p-value | Adjusted | p-value | |
| Median household income (US$) per 10,000 residents | −1.97 (−2.53, −1.41) | <0.001 | −0.16 (−1.15, 0.84) | 0.754 |
| Family Poverty Rate (%) | 25.22 (18.00, 32.44) | <0.001 | 8.42 (−2.15, 18.99) | 0.116 |
| Residents 25 or older with a Bachelor’s degree or more (%) | −19.55 (−24.61, −14.49) | <0.001 | −12.43 (−21.50, −3.37) | 0.008 |
| Residents without insurance/uninsured (%) | 7.89 (4.93, 10.87 | <0.001 | 1.05 (−33.73, 35.84) | 0.952 |
| Tobacco store (density per 10000 persons) | 0.22 (0.11, 0.33) | <0.001 | 0.10 (0.03, 0.20) | 0.043 |
| African American | 2.21 (1.69, 11.59) | 0.002 | 1.34 (−1.89, 8.01) | 0.08 |
Adjusted models included race, median household income, family poverty rate, education, and insurance status.
Figure.
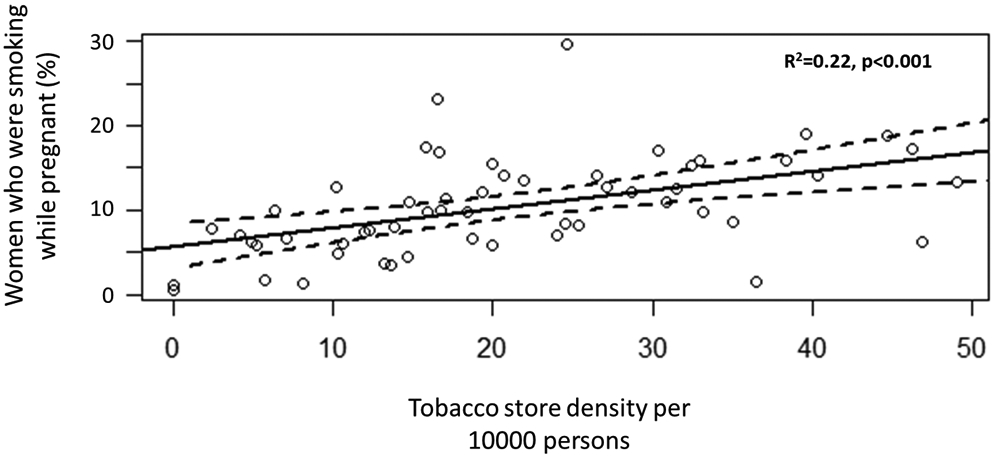
Percentage of women who were smoking while pregnant versus tobacco store density per 10000 persons, with fitted adjusted regression and confidence intervals.
In univariate analyses, lower median income, uninsured, lower formal education, and greater poverty rates were also associated with more women smoking while pregnant (Table).
Moran’s I and Spatial Regression Adjusted Models
In the adjusted model, tobacco store density continued to be associated with more women smoking while pregnant (β = 0.10, p=0.043) (Table), whereby for every 1 unit increase in tobacco store density per 10000 persons, there will be a 10% increase in women smoking while pregnant. Lower neighborhood education level also continued to be associated with more women smoking while pregnant, while race, insurance status, median income, and poverty were not found to be independently associated with smoking while pregnant (Table). Tobacco store density was no longer statistically significant in the remainder of pregnancy-related outcomes.
In sensitivity analysis, excluding the neighborhood with tobacco store density of 114.80 per 1000 residents did not significantly change the results of the regression models (data not shown).
DISCUSSION
Higher tobacco store density of a neighborhood was associated with higher smoking rates while pregnant for women living in Baltimore City. As smoking during pregnancy is associated with significant negative health outcomes, for both the mother and unborn child, these findings suggest that interventions targeting tobacco outlets may have a potential impact in attenuating the rates of smoking while pregnant.
Retail access to cigarettes is assumed to be an important contributor to smoking, in the sense of becoming a new smoker and continuing to smoke.14,15 For instance, Novak et al found that tobacco outlets were more highly concentrated in neighborhoods with high proportion of residents living below the poverty threshold, as well as where there were a large proportion of residents who were younger than 18 years of age.10 This finding by Novak et al is significant given that youth are a particularly vulnerable population, wherein they may have increased exposure to tobacco at a time when tobacco use initiation and transition to daily use is at its greatest.10 Youths residing in areas at the highest percentile of retail tobacco outlet density were more likely to have smoked in the past month (propensity score-adjusted model odds ratio 1.20, 95% CI 1.001 to 1.44) as compared to youth residing in neighborhoods with less tobacco store outlets.9 More recent studies reaffirm these findings, concluding that exposure to tobacco outlets in residential areas may influence adolescent awareness of tobacco products and resulting tobacco use.16,17 Such a finding is consistent with our own data, in that clustering of tobacco outlets had was significantly associated with the percentage of persons who smoke. We identified that there is an association with tobacco store density and amount of women pregnant who smoke, thus showing that clustering of tobacco stores likely has an impact on another vulnerable population, women who are pregnant, reaffirming the influence of local environment on health outcomes.
For women who smoke and are pregnant, an emphasis on smoking cessation is a priority. However, the proximity to tobacco retail stores may pose a challenge on smoking cessation success. Reitzel et al showed that participants living within 500 meters of the closest tobacco retail outlet were less likely to maintain abstinence from cigarette use following a quit attempt, as compared to persons who lived further away from tobacco retail outlets.9 Such a finding is significant in that while proximity to a store that sells tobacco may influence smoking, when an individual wishes to stop smoking, such an environmental factor of accessible tobacco retail outlets may pose an additional barrier to smoking cessation.
Given our results of the association between tobacco store density and smoking during pregnancy, strategies are warranted to attenuate this negative effect. The Family Smoking Prevention and Tobacco Control act of 2009 was intended to promote future public health policies related to tobacco sales for the United States.18 If a path is taken that parallels the regulation of alcohol outlets in communities in order to decrease alcohol usage,19,20 then insight into the effect of tobacco retail outlets on behaviors of tobacco consumption can be further analyzed, potentially providing direction towards tobacco control advocacy and policies. Given the growing body of evidence that the clustering of tobacco retail outlets are associated with smoking behaviors of a community, as well as the smoking behaviors of vulnerable populations such as children and teenager9, the additional insight that our data provides in regards to the impact of women who are pregnant and smoke should demand policy changes in the immediate future.
There are several limitations to take into account. In regards to our main outcome, women who smoked while pregnant, we did not take into account when during their pregnancy they identified as smoking (e.g. first, second or third trimester), which could explain the loss of impact of tobacco store density on other pregnancy-related outcomes explored (preterm births, infant mortality, low birth weight).21,22 Further, since smoking during pregnancy is a self-reported variable on the birth certificates, stigma and bias around smoking may have resulted in an imprecise capturing of how many women smoked during pregnancy. Another limitation is in the inability to accurately convey the smoking topography of the women who smoke, which can change during pregnancy due to higher rates of nicotine metabolism.23,24 Therefore, depending if and how women changed their smoking topography, this could have had implications on our resulting findings regarding the other pregnancy-related outcomes. Third, tobacco store density data (collected in 2016) did not overlap with pregnancy smoking data (from 2010-2014). However, the tobacco store density time frame that we used did not differ significantly from prior data collection of tobacco store densities10 and, therefore, is unlikely to impact our final findings. Fourth, electronic cigarette devices were not taken into account in this study and warrant future investigation. Finally, we do not know if the women who smoked had differential access to recommended obstetric care, which could have helped prevent smoking-related pregnancy complications and fetal complications through aggressive efforts to stop smoking early in the course of the pregnancy.
It is worth mentioning that many markers of high-risk environments cluster together, from alcohol use to tobacco use to homicide rates. Markers of socioeconomic indicators attempt to approximate the material and social conditions and relative disadvantage in a given neighborhood. The markers we identified were chosen due to availability and previous empirical research associating them with smoking. Therefore, while we identified this association with our current data of tobacco store density and women smoking while pregnant in a US urban region, more research is warranted to understand how contextual-level variables in neighborhoods interact with one another to influence behavior and health outcomes, especially in other environments (e.g. rural areas and non-US cities). Further, this study did not detail the areas covered by the CSA, which may result in masking local-level associations in areas with smaller populations, specifically less than 5000 persons.
In conclusion, the relationships between neighborhood socioeconomic variables, tobacco store density, and smoking while pregnant are demonstrated in this study for a US urban region. This study adds to the growing literature in how the clustering of tobacco retail outlets is associated with smoking patterns of local residents, which is of grave concern when smoking poses more of an immediate risk to a specific population: women who are pregnant and developing their fetus. The proximity of the tobacco retail outlets likely contributes to both ongoing smoking and challenges in smoking cessation for women who are pregnant and have some degree of tobacco dependence. Therefore, policies addressing tobacco store distributions in neighborhoods must be a priority for future public health tobacco-oriented goals.
HIGHLIGHTS.
Tobacco use during pregnancy is associated with significant negative health consequences.
Proximity to the sale of tobacco has been associated with tobacco use in young adults.
The density of stores that sell tobacco was associated with women who smoked during pregnancy.
REFERENCES
- 1.Cornelius MD, Day NL. Developmental consequences of prenatal tobacco exposure. Curr Opin Neurol. 2009;22(2):121–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mowery PD, Dube SR, Thorne SL, Garrett BE, Homa DM, Nez Henderson P. Disparities in Smoking-Related Mortality Among American Indians/Alaska Natives. Am J Prev Med. 2015;49(5):738–744. [DOI] [PubMed] [Google Scholar]
- 3.Tong VT, Dietz PM, Farr SL, D’Angelo DV, England LJ. Estimates of smoking before and during pregnancy, and smoking cessation during pregnancy: comparing two population-based data sources. Public Health Rep. 2013;128(3):179–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doogan NJ, Roberts ME, Wewers ME, et al. A growing geographic disparity: Rural and urban cigarette smoking trends in the United States. Prev Med. 2017;104:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. .How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta (GA)2010. [PubMed] [Google Scholar]
- 6.Alberg AJ, Shopland DR, Cummings KM. The 2014 Surgeon General’s report: commemorating the 50th Anniversary of the 1964 Report of the Advisory Committee to the US Surgeon General and updating the evidence on the health consequences of cigarette smoking. Am J Epidemiol. 2014;179(4):403–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh GK, Siahpush M, Azuine RE, Williams SD. Increasing Area Deprivation and Socioeconomic Inequalities in Heart Disease, Stroke, and Cardiovascular Disease Mortality Among Working Age Populations, United States, 1969–2011. Int J MCH AIDS. 2015;3(2):119–133. [PMC free article] [PubMed] [Google Scholar]
- 9.Reitzel LR, Cromley EK, Li Y, et al. The effect of tobacco outlet density and proximity on smoking cessation. Am J Public Health. 2011;101(2):315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Novak SP, Reardon SF, Raudenbush SW, Buka SL. Retail tobacco outlet density and youth cigarette smoking: a propensity-modeling approach. Am J Public Health. 2006;96(4):670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galiatsatos P, Kineza C, Hwang S, et al. Neighbourhood characteristics and health outcomes: evaluating the association between socioeconomic status, tobacco store density and health outcomes in Baltimore City. Tob Control. 2018;27(e1):e19–e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baltimore City Health Department. Baltimore City Health Department’s Neighborhood Health Profiles. health.baltimorecity.gov/stats-and-data. Accessed January 2019 2017.
- 13.Fakunle DO, Milam AJ, Furr-Holden CD, Butler J 3rd, Thorpe RJ Jr., LaVeist TA. The inequitable distribution of tobacco outlet density: the role of income in two Black Mid-Atlantic geopolitical areas. Public Health. 2016;136:35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hyland A, Travers MJ, Cummings KM, Bauer J, Alford T, Wieczorek WF. Demographics and tobacco outlet density. Am J Public Health. 2003;93(11):1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laws MB, Whitman J, Bowser DM, Krech L. Tobacco availability and point of sale marketing in demographically contrasting districts of Massachusetts. Tob Control. 2002;11 Suppl 2:ii71–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shortt NK, Tisch C, Pearce J, Richardson EA, Mitchell R. The density of tobacco retailers in home and school environments and relationship with adolescent smoking behaviours in Scotland. Tob Control. 2016;25(1):75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tunstall H, Shortt NK, Niedzwiedz CL, Richardson EA, Mitchell RJ, Pearce JR. Tobacco outlet density and tobacco knowledge, beliefs, purchasing behaviours and price among adolescents in Scotland. Soc Sci Med. 2018;206:1–13. [DOI] [PubMed] [Google Scholar]
- 18.Family Smoking Prevention and Tobacco Control and Federal Retirement Reform. 2009.
- 19.Fitterer JL, Nelson TA, Stockwell T. A Review of Existing Studies Reporting the Negative Effects of Alcohol Access and Positive Effects of Alcohol Control Policies on Interpersonal Violence. Front Public Health. 2015;3:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fone D, Dunstan F, White J, et al. Change in alcohol outlet density and alcohol-related harm to population health (CHALICE). BMC Public Health. 2012;12:428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abraham M, Alramadhan S, Iniguez C, et al. A systematic review of maternal smoking during pregnancy and fetal measurements with meta-analysis. PLoS One. 2017;12(2):e0170946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blatt K, Moore E, Chen A, Van Hook J, DeFranco EA. Association of reported trimester-specific smoking cessation with fetal growth restriction. Obstet Gynecol. 2015;125(6):1452–1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dukic VM, Niessner M, Benowitz N, Hans S, Wakschlag L. Modeling the relationship of cotinine and self-reported measures of maternal smoking during pregnancy: a deterministic approach. Nicotine Tob Res. 2007;9(4):453–465. [DOI] [PubMed] [Google Scholar]
- 24.Ellard GA, Johnstone FD, Prescott RJ, Ji-Xian W, Jian-Hua M. Smoking during pregnancy: the dose dependence of birthweight deficits. Br J Obstet Gynaecol. 1996;103(8):806–813. [DOI] [PubMed] [Google Scholar]


