Abstract
Pre-exposure prophylaxis (PrEP) is an effective HIV prevention strategy for high-risk adults and recently was given US FDA approval for use among adolescents. Yet, the barriers to medication uptake for this population are unique when compared to adult populations, as parents may be just as likely as prescribers to be gatekeepers to access. To better understand the role of parents in adolescents’ attitudes towards PrEP, we surveyed 491 adolescent men who have sex with men (AMSM) ages 13–18, using forced choice and open-ended response questions. We measured perceived parent-PrEP supportiveness, hypothetical parent reactions to a request to initiate PrEP, and perceived positive and negative aspects of taking PrEP without parents knowing. A mixed-methods approach was employed. Results indicated a majority of AMSM had heard of PrEP and most reported their parents would be unsupportive of their taking PrEP. Teens perceived their parents would likely be angry, accusatory, and punitive if PrEP use was discovered, and that accessing PrEP independent of parents might increase their health autonomy, agency, and prevent awkward conversations about sex. Furthermore, a path model revealed that fears of parental reaction and poor self-efficacy to communicate with parents about PrEP significantly contributed to participants feeling PrEP was not “right” for them, and as a corollary, less interest in starting PrEP. The study suggests that improving parental knowledge of PrEP and encouraging parents to begin the conversation about PrEP could help increase uptake in AMSM.
Keywords: Adolescents, PrEP, Parents, Family Communication, HIV Prevention
RESUMEN
El Profilaxis de preexposición (PrEP) ha sido aprobado por la US FDA como una estrategia efectiva para la prevención del VIH en adolescentes. Las barreras de esta población para el uso de PrEP son únicas, ya que padres y proveedores pueden controlar su acceso. Para entender mejor la influencia que tienen los padres en las actitudes de los adolescentes hacia PrEP, se llevó a cabo una encuesta con 491 adolescentes (13–18) que tienen sexo con otros hombres. Medimos la percepción de apoyo parental hacia el uso PrEP, reacciones hipotéticas de los padres al enterarse de su uso y aspectos positivo y negativos de tomar PrEP sin el conocimiento de los padres. La mayoría de los adolescentes indicó haber escuchado de PrEP y que sus padres no los apoyarían si quisieran tomarlo. Los participantes reportaron que sus padres reaccionarían con coraje, acusaciones y castigos al enterarse del uso de PrEP. También reportaron que acceder a PrEP sin sus padres podría aumentar su autonomía, su agencia y prevenir conversaciones incómodas acerca del sexo. Un análisis de ruta reveló que el miedo a la reacción de sus padres y poca auto-eficacia para comunicarse con sus padres acerca de PrEP, contribuyen significativamente a que los participantes sientan que PrEP no es adecuado para ellos y tengan menos interés en comenzar a tomar PrEP. Nuestro estudio sugiere que mejorar el conocimiento de los padres acerca de PrEP y fomentar la comunicación entre padres y adolescentes acerca del mismo puede aumentar el consumo de PrEP en adolescentes que tienen sexo con otros hombres.
INTRODUCTION
In 2017, adolescent men who have sex with men (AMSM) in the US account for 83% of all new HIV infections among those 13–19 years-old. Racial/ethnic minority youth account for the majority (86%) of those infections among AMSM (1). Even though this youngest group has a documented lower number of HIV diagnoses (21%) relative to their 20–24 year-old counterparts (79%), this difference may be at least partially an artifact of extremely low HIV testing rates in those <18 year olds (2). Risk behaviors are prevalent among AMSM age 18 and younger, with recent studies showing relatively high rates of condomless sex with multiple sex partners (3–5) and with adult partners who may be years older (6). Despite AMSM rates of HIV, inconsistent HIV testing, and sustained risk-taking behaviors by adolescents, there have been virtually no prevention interventions targeted specifically towards AMSM until recently (7). In May 2018, pre-exposure prophylaxis (PrEP) was FDA-approved for use in AMSM as a biomedical prevention method (8). Given the recency of the approval and how little is known about adolescents’ attitudes towards PrEP, research on the barriers to PrEP promotion, uptake, and adherence are urgently needed.
PrEP is a biomedical HIV prevention method initially FDA-approved in 2012. It is a once-daily dose of the antiretroviral therapies branded as either Truvada® or Descovy®. When taken as prescribed, it is >90% effective at reducing sexual transmission of HIV (8). PrEP has untapped potential to curb infection rates among AMSM (9–11). A recent investigation showed that daily oral PrEP was safe and well-tolerated in AMSM (12); however, many AMSM faced challenges with medication adherence and maintenance, which are known to impact PrEP effectiveness. Efficacy studies aside, knowledge of, and access to, PrEP is low among teenagers. Using data collected in 2015, Thoma and Huebner (13) found only 14.7% of 14–16 year olds and 17.5% of 17–18 year olds were aware of PrEP. A recent study using 2018 data documented that of the 219 AMSM aged 15–17 sampled, 55% had heard of it, but 56% did not know how they would access PrEP if they wanted it (14). Although these two studies suggest increasing awareness, they both show low rates of PrEP use (0.5% in the 2015 sample (13) and 2.5% in the 2018 sample (14)). The extent to which awareness translates into actual prescriptions remains dubious and likely stunted by myriad obstacles.
Research into AMSM and PrEP has revealed initial individual and structural barriers (15, 16). For example, teenagers may not know how to navigate the health care systems necessary to obtain a prescription, use insurance, and access supplemental co-insurance programs. Securing transportation to providers and pharmacies, keeping to a PrEP regimen, and knowing how to cope with side effects also have been cited as obstacles towards use (9, 17–19). Research now suggests teens may consider their parents to be just as likely as these other factors to influence access (11). In support of this point, virtually all US States allow for adolescent use of sexual health services without parental consent, under the belief that parents’ judgements about sexual behaviors should not be a preventive factor from adolescent testing and treatment for communicable disease (20). However, as of 2017, only 16 states allow for adolescents to access and use PrEP without parental consent (21).
Parental attitudes towards, and involvement with, medication uptake and adherence have been researched as barriers and facilitators for other treatments outside of PrEP (22). Parental involvement can be influential in adolescents’ control of chronic diseases like HIV (23), asthma (24), and diabetes (25), as well as adherence to psychostimulants for attention-deficit/hyperactivity disorder (26). Regarding sexual health specifically, parents’ positive attitudes and behavioral facilitation were both predictive of initiation and adherence to birth control (27) and completion of the HPV vaccination series (28). In line with these other studies, Thoma and Huebner (13) found AMSM attitudes about, and perceived behavioral control to take, PrEP varied by conversations they had with their parents regarding HIV. Teens who reported their parents conversed in a less open, honest, and knowledgeable way about HIV were less likely to favor PrEP and less likely to perceive their ability to obtain and take it.
Thoma and Huebner’s findings on behavioral control (13) point toward the Theory of Planned Behavior (TPB) (29, 30) as a framework to understand parental influence and AMSM PrEP attitudes. The theory shows subjective norms as a key influence over behavioral intentions and behavioral enactment, and an important variable affecting individual attitudes towards behaviors and perceived behavioral control to engage in a behavior. Subjective norms refer to the perceived social approval or disapproval of a behavior by others (e.g., AMSM perceptions of the support or lack of support their parents might show towards PrEP use). They are derived from individuals’ normative beliefs, which are perceptions of the likely reactions and expectations of friends, family, and peers pertaining to a behavior (31). Researchers have used this theory to explore PrEP use intentions and behavioral uptake in adult MSM (32–34). Studies show individuals’ perceptions of how positively or negatively others perceive PrEP to be influential over intentions to start it and actually starting it. As of yet, TPB remains unexplored regarding AMSM attitudes towards PrEP, including the subjective norms and underlying normative beliefs AMSM might attribute to their parents. AMSM may find their interest and attitudes towards PrEP largely impacted by the subjective norms they perceive from their parents. Subjective norms, specifically regarding parents, have been found to impact adolescents’ attitudes regarding sexual initiation (35, 36), substance and alcohol use (37–40), and birth control (41, 42). As such, what AMSM perceive about their parents, including their ability even to discuss it with them, may influence their attitudes towards PrEP and their interest in its initiation.
The Thoma and Huebner (13) study notwithstanding, it still remains unknown if, how, and why teens perceive their parents to be barriers towards PrEP uptake. We opted for a mixed-methods approach, given how novel PrEP availability is for adolescents, to identify these beliefs and investigate how they impact norms, attitudes, and behavioral intentions about PrEP. Moreover, there exists no known battery that measures parent-oriented barriers to PrEP use. To build on prior work (13) and establish the beliefs and norms on which future quantitative measures might be built, we asked AMSM to explain how their parents might react to conversations about PrEP, the potential positive and negative parent-child relationship dynamics that might impact disclosure of use, and the reasons that AMSM may choose to conceal PrEP use from their parents. Themes were derived from these responses, which represented AMSM’s differing normative beliefs and behavioral control to discuss PrEP with parents. Finally, we tested the direct and indirect paths between these normative beliefs, behavioral control to discuss PrEP, subjective norms, attitudes about PrEP use, and behavioral intention (i.e., likelihood to start PrEP soon).
METHODS
Data were collected between July 2018 and February 2019 (N=491) as part of SMART, an ongoing pragmatic trial of a suite of HIV prevention interventions for AMSM. SMART uses a sequential multiple assignment randomized trial design (43) to assess the effects of a package of increasingly intensive HIV prevention programs on sexual risk behaviors among racially-diverse AMSM across the United States and three territories (Puerto Rico, Guam, and American Samoa). The first intervention in the stepped care sequence is delivered to all participants; “SMART Sex Ed,” is a comprehensive LGBTQ-inclusive sex education program developmentally adapted from the “Queer Sex Ed” intervention (44). The next step is “SMART Squad,” a developmental adaptation of the “Keep it Up!” intervention (45–47) that was classified by the Centers for Disease Control and Prevention (CDC) as a “best evidence” intervention for HIV risk reduction (48). The last intervention in the stepped care package is “SMART Sessions,” a motivational interviewing protocol based on the CDC-best evidence “Young Men’s Health Project” that aims to reduce substance use and sexual risk behaviors (49). This intervention was adapted developmentally and for delivery via videoconferencing.
Eligibility criteria for SMART include: 1) being 13–18 years old; 2) assigned male at birth; 3) identifying as gay, bisexual, queer or attracted to cisgender men; 4) reporting some sexual experience (i.e., prior contact with another individual’s genitals); 5) being able to speak and read English or Spanish; 6) having consistent Internet access; and 7) self-reporting an HIV-negative or HIV-unknown serostatus. Participants were recruited via free and paid social media campaigns on Facebook, Instagram, Snapchat, and Twitter, and participants from prior studies who had indicated interest in future research participation. Prospective participants clicked on a URL to an online screener. Those who met eligibility criteria were automatically routed to an online consent form, after which they completed four capacity to consent questions that assessed their understanding of the research procedures (50). A brief videochat was scheduled with research staff to confirm participant eligibility, consent capacity, and complete enrollment; if participants were confirmed as eligible during this call, they were emailed a URL to the baseline survey, which was hosted on REDCap. Data were collected using a computer-assisted selfinterview, and participants were paid $25 for their time. All procedures were approved by the institutional review board with waivers of parental permission (50). Data for this study were taken from the baseline assessment of SMART and were collected prior to any intervention participation. At the time of analysis, 491 participants had completed the baseline measures, which included our specific questions on parents and PrEP.
Measures
Demographics such as age, race/ethnicity, and geographic region (West, South, Northeast, Midwest) were assessed. Outness to mother and/or father were measured, along with parents’ level of acceptance. We asked about participant lifetime sexual activity (i.e., yes/no for these behaviors: kissing, touching a genital, oral sex, vaginal sex, and anal sex). Participants reported total number of lifetime anal sex partners and total number of lifetime condomless anal sex partners. Percent of lifetime condomless anal sex partners was calculated by dividing the number of condomless partners by the total number of partners.
Participants were then given a brief description of PrEP: “PrEP (pre-exposure prophylaxis) is a medication that prevents people from getting HIV. PrEP involves HIV-negative guys taking a pill once a day, every day, to reduce the chances of getting HIV if you come into contact with the virus. People on PrEP go to a doctor or medical provider every 3 months for HIV/STI testing, bloodwork, and a new 3-month prescription for PrEP.” Following the definition, closed-ended questions were asked to assess familiarity with, interest in, and barriers to PrEP. Specifically, participants were asked if they had been on PrEP in their lifetime (no/yes), had heard of PrEP before the survey (no/yes), and, if they had heard of it, where they first learned about it (51). Participants reported their attitudes towards PrEP fit (i.e., was PrEP “right” for them, measured on a 5-point scale from definitely no to definitely yes). They reported whether they intended to start PrEP soon, measured on a 5-point scale from definitely will not to definitely will start it (i.e., behavioral intention). To explore barriers, we asked the likelihood of starting PrEP under specific conditions (e.g., if they were able to get it for free; if they were able to get it for free and without their parents’ knowledge, both measured on a 5-point scale from definitely not to definitely) (52). Finally, we assessed parent-PrEP subjective norms by asking the closed-ended question, “how do you think your parents would react if you asked to start taking PrEP,” on a 4-point scale from very unsupportive to very supportive.
Following, we asked three open-ended questions to assess AMSM normative beliefs about their parents and PrEP, as well as behavioral control to discuss PrEP with them. (Q1) How would you feel about asking your parent(s) if you could start taking PrEP? (Q2) What do you think might be some of the good and bad things about taking PrEP without your parent(s) knowing about it? (Q3) Imagine you started taking PrEP without your parents knowing about it. How do you think your parents would react if they found out you were taking PrEP (for example, they found a bottle of PrEP pills)?
Qualitative Data Analysis and Coding
Content analysis was used to identify normative beliefs, behavioral control, and other attitudinal themes relevant to the open-ended questions (53). Research staff created a codebook by reviewing each of the questions independently, noting themes, and discussing whether these themes were prevalent enough to warrant theme categorization (54). The codebook included a definition of the theme, inclusion and exclusion criteria, and examples of quotes for each code. Two independent coders were trained on the codebook and instructed to code 20% of the 491 responses for each of the questions separately. Reliability per code (i.e., Cohen’s kappa) was established using a standard threshold of 0.7 (55, 56). In instances of code discord, coders met to compare content and discuss how specific codes should be categorized until 100% agreement was met. Following reliability testing and discussion, the remainder of the responses were coded. Lists of excerpts by theme were generated and the coders identified exemplar responses.
Quantitative Statistical Analysis
The descriptive analyses of the quantitative data (closed-ended demographic, behavioral, and attitudinal questions) and bivariate correlations were conducted using SPSS 25.0. When sample sizes within variables varied due to missing data, it is noted. Following the establishment of themes, coding of the qualitative data into quantitative data, and integration of the coded themes back into the dataset, theme-prevalence (i.e., percentage of participants reporting the theme) was calculated through the statistical software.
A path model with multiple mediation was created from variables that represent the TPB theoretical constructs (29–31). This expanded model estimated the direct and indirect impacts of AMSM-parent-PrEP normative beliefs and behavioral control to discuss PrEP with parents on endogenous variables like perceived parental support (i.e., subjective norms), PrEP fit (i.e., attitudes towards the behavior), and whether the AMSM intend to start PrEP (i.e., behavioral intention). We also included within-model indirect effects: AMSM-parent-PrEP normative beliefs and behavioral control to discuss PrEP, through perceived parent support (i.e., subjective norms) onto PrEP fit (i.e., attitudes towards the behavior); and perceived parent support, through PrEP fit onto intending to start PrEP (i.e., behavioral intention). This expanded model was tested with participants who had completed all the measures required for analysis, leaving no missing data (n=488). To assess how well the proposed path model fit the data, a path analysis with fixed error variances and fixed error terms of indicators was conducted with Mplus 7.31. Specifically, we examined chi-square goodness-of-fit, the comparative fit index (CFI), and the root-meansquare error of approximation (RMSEA). Good model fit was indicated by a non-significant chi-square comparing the default model and expanded model with indirect pathways, a CFI greater than .95 (57) and a RMSEA less than .05 (58).
Most germane to our study and TPB, we focused on four indirect paths in our model, which explored how basic beliefs held about parents by AMSM might ultimately help or hinder behavioral intentions to start PrEP. These were the three normative belief themes and one behavioral control theme predicting subjective norms (parental support), which then predicted attitudes towards the behavior (PrEP fit) and then finally, behavioral intentions (intending to start PrEP). Because the distribution of indirect coefficients was not normally distributed, a bootstrap method was used to calculate the significance of indirect paths (59). Biased-corrected 95% confidence intervals were created from 5,000 samples. If the intervals did not contain zero, the indirect effect was significant.
RESULTS
Sample Characteristics
The sample was relatively diverse with 55.7% reporting being of an ethnic/racial minority; almost a third (29.5%) reported a Latino ethnicity (see Table 1). Participants ranged in age from 13 to 18 years old with the majority (50.5%) reporting 16 or 17 years old. Additionally, the sample was geographically diverse with the largest portion of participants (44.3%) coming from the South. Most participants were out to their mother (62.3%), but about half the sample (48.2%) was out to both parents; participants reported their mothers (51.5%) were more accepting than fathers (37.2%). Regarding self-reported HIV status, 51.1% of participants reported being HIV-negative, 47.3% had never been tested, and 1.6% reported an unknown status. Almost two-thirds of participants had had anal sex in their life (58.7%), which was the most endorsed sexual behavior from the list of choices. Condomless anal sex occurred with 59.0% of lifetime partners (SD=40.1%, 0–100%). The average number of lifetime condomless anal sex partners was 2.32 (SD=3.63, 0–25).
Table 1.
Description of the sample
| Count | % of N | M | SD | |
|---|---|---|---|---|
| Age (n=491) a | 16.56 | 1.30 | ||
| Race (n=481) | ||||
| White | 213 | 44.3 | ||
| African-American/Black | 76 | 15.8 | ||
| Hispanic/Latino | 142 | 29.5 | ||
| Asian | 17 | 3.5 | ||
| Other/mixed race | 33 | 6.9 | ||
| Geographic location (n=481) | ||||
| South | 213 | 44.3 | ||
| West | 111 | 23.1 | ||
| Northeast | 77 | 16.0 | ||
| Midwest | 80 | 16.6 | ||
| Sexual Orientation (n=483) | ||||
| Gay | 312 | 64.6 | ||
| Bisexual | 127 | 26.3 | ||
| Queer/Pansexual | 29 | 6.0 | ||
| Unsure/Questioning | 10 | 2.1 | ||
| Other | 5 | 1.0 | ||
| Outness to Parents | ||||
| Out to mother (n=485) | 307 | 63.3 | ||
| Out to father (n=453) | 223 | 49.2 | ||
| Out to both mother and father (n=448) | 216 | 48.2 | ||
| Acceptance of Outness, Mother (n=307) | ||||
| Not accepting | 28 | 9.1 | ||
| Somewhat not accepting | 38 | 12.4 | ||
| Somewhat accepting | 83 | 27.0 | ||
| Accepting | 158 | 51.5 | ||
| Acceptance of Outness, Father (n=223) | ||||
| Not accepting | 37 | 16.6 | ||
| Somewhat not accepting | 41 | 18.4 | ||
| Somewhat accepting | 62 | 27.8 | ||
| Accepting | 83 | 37.2 | ||
| HIV status (n=491) | ||||
| HIV-negative | 251 | 51.1 | ||
| Never been HIV tested | 232 | 47.3 | ||
| HIV-unknown | 8 | 1.6 | ||
| Lifetime Sexual activity (n=491) | ||||
| Kissing | 150 | 30.5 | ||
| Touching a genital | 167 | 34.0 | ||
| Oral Sex | 141 | 28.7 | ||
| Vaginal sex | 87 | 17.7 | ||
| Anal sex | 288 | 58.7 | ||
| Number of lifetime condomless anal sex partners (n=280) b | 2.32 | 3.63 | ||
| Number of lifetime condomless anal sex partners (n=288) c | 4.31 | 7.76 | ||
| Lifetime condomless anal sex partners (%) (n=278) d | 59.0 | 40.1 | ||
Note. Ranges:
13–18.99
0–25
0–70
0–100
In terms of PrEP, a majority of participants had heard about it; however, very few (i.e, ten participants) had ever taken it in their life (see Table 2). The sample learned about PrEP in diverse ways with approximately one in four (28.2%) reporting having looked it up online. It is noteworthy that one in ten (10.6%) learned about PrEP as embedded content within a TV or online program. When asked about PrEP fit (i.e., whether it was “right for them”), more than half the participants were unsure (52.7%); a similar amount (52.9%) were unsure about intending to start taking PrEP. The most endorsed reason participants did not currently use PrEP was concern that their parents might find out (32.2%). In follow-up questions that explored their likelihood of taking it under specific circumstances (e.g., if it were free), four out of five participants (82.2%) said they definitely or probably would take the medication if it were free and their parents would not find out. As a corollary, 60.5% of participants reported their parents would be very unsupportive or somewhat unsupportive of their using it; and 62.9% said that if they took PrEP, they would not want their parents to know. No demographic variables were predictive of whether PrEP was right for the participants and/or predictive of parental support for PrEP.
Table 2.
AMSM PrEP knowledge and attitudes
| Heard of PrEP? (n=491) | ||
| No | 220 | 44.8 |
| Yes | 271 | 55.2 |
| Have been on PrEP in lifetime (n=271) | 10 | 3.7* |
| Where did you first learn about it? (n=271) | ||
| Looked it up online | 72 | 28.2 |
| A doctor or HIV testing counselor | 31 | 12.2 |
| TV shows or online shows | 27 | 10.6 |
| Friends | 20 | 7.8 |
| TV ad | 19 | 7.4 |
| Someone I was dating or having sex with | 18 | 7.1 |
| Research staff | 17 | 6.7 |
| Online ad | 13 | 5.1 |
| Social media | 9 | 3.5 |
| Family member | 8 | 3.1 |
| On grindr/scruff | 8 | 3.1 |
| Out in my community | 7 | 2.7 |
| In a school health class | 6 | 2.4 |
| Parent or parents | 0 | 0.0 |
| Is PrEP right for you?** (n=491) | ||
| Definitely yes | 46 | 9.4 |
| Yes | 125 | 25.5 |
| Not sure | 259 | 52.7 |
| No | 48 | 9.8 |
| Definitely no | 13 | 2.6 |
| Why do you not use PrEP? (n=491) | ||
| I am worried my parents would find out I was taking PrEP | 158 | 32.2 |
| I don’t know enough about it | 101 | 20.6 |
| I think I am at no or low risk for HIV | 87 | 17.7 |
| I do not want to go to the doctor and get blood work every 3 months | 86 | 17.5 |
| Not sexually active | 75 | 15.3 |
| I cannot afford it and/or I do not have insurance | 47 | 9.6 |
| I do not want to take a pill everyday | 38 | 7.7 |
| I think condoms are a better choice than PrEP | 32 | 6.5 |
| People who use PrEP are perceived negative by others | 21 | 4.3 |
| I am in a serious relationship | 21 | 4.3 |
| Do you intend to start taking PrEP? (n=488) | ||
| Yes, I will definitely start taking PrEP | 34 | 7.1 |
| Yes, I will probably start taking PrEP | 61 | 12.7 |
| I’m not sure – I might start taking PrEP | 255 | 52.9 |
| No, I probably will not start taking PrEP | 116 | 24.1 |
| No, I definitely will not start taking PrEP | 16 | 3.3 |
| Would you take PrEP if it were free? (n=488) | ||
| Definitely | 185 | 37.9 |
| Probably | 146 | 29.9 |
| I might take it | 113 | 23.2 |
| Probably not | 38 | 7.8 |
| Definitely not | 6 | 1.2 |
| Would you take PrEP if it were free AND without your parents knowing? (n=488) | ||
| Definitely | 289 | 59.2 |
| Probably | 112 | 23.0 |
| I might take it | 62 | 12.7 |
| Probably not | 19 | 3.9 |
| Definitely not | 6 | 1.2 |
| Imagine you could get PrEP without your parents’ permission. Would you want your parents to know you were taking it? (n=490) | ||
| No, I would not | 309 | 62.9 |
| Yes, I would want them to know | 49 | 10.0 |
| I would not care if they know | 132 | 26.9 |
| How do you think your parents would react if you asked to start taking PrEP? (n=491) | ||
| Very unsupportive | 151 | 30.8 |
| Somewhat unsupportive | 146 | 29.7 |
| Somewhat supportive | 136 | 27.7 |
| Very supportive | 58 | 11.8 |
Note.
10 of the 271 participants (3.7%) who had heard of PrEP reported having taken it in the past. Of the total sample, 10 of the 491 (2.0%) reported having taken it in the past.
For reference, this variable is called “PrEP fit” throughout the results.
Among the quantitative measures described in Table 2, four variables showed significant bivariate associations with an increase in PrEP fit (i.e., PrEP being “right” for the participant) were total number of condomless lifetime anal sex partners (r=.21, p<.001), being out to mother (r=.11, p=.02), being out to father (r=.11, p=.02), and parental support for PrEP (r=.15, p<.001). Parental support for PrEP was positively related to being out to mother (r=.26, p<.001) and father (r=.19, p<.001), and acceptance of sexual orientation by the mother (r=.46, p<.001) and father (r=.40, p<.001). Finally, in line with the TPB prediction that behavioral attitudes predict intentions, PrEP fit was highly correlated with intending on starting PrEP (r=.52, p<.001).
Normative Beliefs and Behavioral Control Regarding Asking Parents to Go on PrEP
Table 3 describes the four themes emerging from the first open-ended response question exploring how participants might feel asking their parents if they could go on PrEP. These four themes represented their normative beliefs regarding their parents (i.e., awkward, fearful, and comfortable) and their perceived behavioral control (i.e., ability/inability) to discuss future PrEP use. One in three participants (35.8%) reported it would be awkward, while one in five (20.4%) believed they simply were unable to have the conversation. There were some positive responses (13.4%) in which participants reported they and their parents would be comfortable discussing it. Finally, 12.2% reported they would be fearful to engage in PrEP communication with their parents.
Table 3.
How would you feel about asking your parent(s) if you could start taking PrEP?
| Themes | K | Definition | Example |
|---|---|---|---|
| Awkward (n=176) | .93 | Feelings of embarrassment, discomfort; the conversation would be difficult to handle or deal with | “I would be embarrassed to ask them because I don’t really feel that comfortable talking to them about that kind of stuff” |
| Unable (n=100) | .70 | Participant is emphatic that they could not have this conversation with their parent(s); they lacked the ability | “I can’t talk to them about it cause I’m not out” |
| Comfortable (n=66) | .77 | Confidence surrounding such conversations and/or the mention of positive or neutral feelings | “I would feel completely fine with it” |
| Fearful (n=60) | .88 | Description of feelings of fear, terror, or being afraid; causing fear or punishment | “I would be scared and I probably would wait to take it” |
Note. N=491. In the quantitative results, these four themes represent the normative beliefs and perceived behavioral control of AMSM regarding their parents and PrEP discussions.
Turning to some of the qualitative content from these themes, participants were quite explicit in their beliefs about parent-PrEP communication. Regarding fear, one Latinx, 16 year old participant said he would be, “Afraid because then they’ll know I’m sexually active and I think they’ll perceive that as a negative thing since I’m under 18.” A 17 year old Black participant said he would be, “scared. My mom is a staunch Christian and already doesn’t approve of my gay lifestyle and believes that any sex I have should be with a woman to whom I am married.” Regarding inability to have such conversations about PrEP, a White, 16 year old said, “I could never ask my parents because I really don’t want them to know I’m sexually active.” Conversely, and representing the comfort theme, another White, 16 year old said, “I’d feel comfortable. They’re very accepting of who I am and they’re not afraid to talk about sexual health with me.”
Positive Aspects of Parents Not Knowing About PrEP Use
Participants reported three positive themes (shown within Table 4) when asked about potential future accessing of PrEP without parental involvement. The most popular (29.7%) was feeling good about protecting themselves from HIV (i.e., feeling they were actively preventing HIV infection). While this was not specific to parents, it reflected a general perceived benefit of being on PrEP. For example, a White, 17 year old said, “good things would be that I was at lower risk for HIV, and it would allow me more control over my sex life.” Second most common (22.2%), participants reported feeling that their private PrEP use would increase their sense of autonomy. “I would know I’m taking steps to protect myself sexually without having to explain to my parents why I want to take prep,” said a multiracial, 16 year old. Some participants (13.4%) described that private PrEP use would allow them to avoid parental judgments about how much sex they might be having. A Latinx, 16 year old was relieve that, “They wouldn’t judge me about taking it or having sex while not married and that would be nice!”
Table 4.
What do you think might be some of the good and bad things about taking PrEP without your parent(s) knowing about it?
| Themes | K | Definition | Example |
|---|---|---|---|
| HIV Prevention (+) (n=146) | .95 | Participant describes the use of PrEP as an HIV prevention strategy; mentions that PrEP can protect against HIV or is a way to stay healthy, feeling safe | “good- i would feel safer about starting to have sex more frequently, i would feel more protected.” |
| Autonomy (+) (n=109) | .82 | Participant mentions their ability to maintain privacy, independence, autonomy; don’t have to worry about parental approval or support regarding PrEP or possible confiscation; can make their own choices |
“I wouldn’t have to worry about my parents being all over me and watching everything I do.” |
| Avoid assumptions about sex (+) (n=66) | .72 | Participant describes how hiding PrEP use can avoid parents finding out or making assumptions that they are sexually active. | “The good things would be that they wouldn’t have to find out that I’m sexually active.” |
| Secrecy (−) (n=124) | .74 | Participant discusses keeping PrEP a secret, possible lying, hiding, loss of trust, possibility of getting caught or damaging the relationship; having to sneak around for care |
“They won’t say anything to me but a bad thing would be that I would have to sneak it around every day until I move out.” |
| Incomplete medical information (−) (n=92) | .78 | Participant discusses how parents will not have participant’s full medical history readily available in case of an emergency, allergic reaction, during side effects, complications, overdose, questions surrounding PrEP use, or finding PrEP |
“If i was allergic to the pill, and had a bad reaction they wouldnt know where it came from.” |
| Logistical difficulties getting/taking PrEP (−) (n=67) | .74 | Participants mention logistical difficulties surrounding getting to the doctor/pharmacy, payment, prescriptions, and insurance without parents’ assistance; Would need familial social support | “ bad- it would probably cost money that i don’t have to spend on PrEP because i couldn’t use their insurance. also i wouldn’t be able to get a ride to the store to get it.” |
Note. N=491. Themes denoted by “+” are perceived by participants to be a positive, good, or beneficial aspect of accessing PrEP without parental involvement. Themes denoted by “−” are perceived by participants to be a negative, bad, or detrimental aspect of accessing PrEP without parental involvement.
Negative Aspects of Parents Not Knowing About PrEP Use
Three negative themes emerged when participants were asked about the consequences of keeping future use of PrEP from their parents (see Table 4). One in four participants (25.3%) reported secrecy to be a significant consequence of not disclosing use. Specifically, having to “sneak around” or merely “keeping it [PrEP use] from them,” would create guilt and would undermine the parent-teen relationship they had built. “We are very open and if I never told them, I feel like I would be lying to them and they would be hurt about that” (Multiracial, 16 year old). For one in five participants (18.7%), concerns were voiced that a parent would not have relevant medical information should a medical accident occur or should the participant exhibit side effects. “I might not be taking a proper dosage, or I might have a reaction to a chemical or ingredient” (Latinx, 17 year old). Similarly, 13.6% of participants reported medication logistical concerns, where one participant thought, “I wouldn’t know how to navigate prescriptions, insurance, and financing the medication without them [parents]” (White, 18 year old). Other teens stated it would be difficult to schedule provider appointments, obtain PrEP, store it, and (without social support from parents) follow the regimen as prescribed.
Parents’ Reactions If PrEP Use Was Discovered
Participants described six potential reactions to their parents’ discovery of their future PrEP use (see Table 5). The most widely described parental response was anger (38.1%). They would “freak out,” “be upset,” or “shocked” about a teen’s PrEP uptake. One in four participants (24.6%) projected that the parent would ask them many questions. The third most common response (14.7%) was punishment. An 18 year old, Latinx participant described this disclosurepunishment likelihood in detail. “They would freak out. It took years of coaxing to get them to be ok with me having a boyfriend, and they still don’t like that I have sex with him. If they found a bottle of PrEP pills they would kill me, because they would assume I had been having sex with multiple men. My dad might hit me, and I would certainly be stuck in the house and not allowed to see anyone for a couple months.” Other participants were similarly concerned that there would be some retaliation for taking PrEP such as banishing them from the family home, slapping or hitting them, having a phone taken away, or being grounded. For 12.8% of participants, parents finding PrEP would lead to accusations of promiscuity; some in the sample were concerned that they would be called a “whore” or have to explain the sexual behaviors in which they were engaging. Conversely, 10.0% of participants suggested through their response that their parents would be somewhat or very supportive. A Latinx, 17 year old said, “They honestly wouldn’t care much. They would probably look it up for themselves and be like oh I guess that’s good he’s taking care of himself.” Finally, for a minority of participants, they reported their parents would mistake PrEP for illegal drugs (6.5%). “My dad would probably do his own research then mind his business. My mother in the other hand would probably think I’m taking random drugs and freak out” (Latinx, 16 year old).
Table 5.
Now, imagine you started taking PrEP without your parents knowing about it. How do you think your parents would react if they found out you were taking PrEP?
| Themes | K | Definition | Example |
|---|---|---|---|
| Angry (n=187) | .79 | Participant discusses possibilities and varying levels of anger, fury, or overreaction that can result from discovering participant’s PrEP use. | “They would be shocked and probably upset.” |
| Ask questions/ inquisitive (n=121) | .82 | Participant describes how parents would ask them many questions about PrEP/the pills | “My mom would ask A LOT of questions and she would most likely say I was being smart.. My dad would be mad because he doesn’t approve of me being with boys.” |
| Punish (n=72) | .76 | Participant discusses the varying levels of punishment or abuse that can result from parents finding PrEP; homelessness, confiscation, disownment, grounded | “My mom would probably die, like no joke bc right now she’s super stressed out bc of my Dad. But if my Dad found out he’d probably slap me across the face bc that means 1) I’m taking drugs 2) I’m sexually active with a culturally perceived ‘wrong sex’” |
| Question sexual activity (n=63) | .80 | Participant describes how finding out they are taking PrEP may cause their parents to assume they are having sex or ask related questions | “Once they found out, my parents probably would assume that I have HIV and assume that I am having sex every day. I would like to think they would be calm, but I feel they would be… be grossed out.” |
| Be supportive (n=49) | .76 | Participant broadly describes how parents would ultimately be supportive of them taking PrEP; mentioning how PrEP would be positively perceived; mentioning that parents would be proud | “They’ll be happy I’m safe. They would obviously have questions, but my dad would probably be relatively supportive.” |
| Mistake for PrEP for illegal drugs (n=32) | .90 | Participant describes how parents might mistake PrEP for illegal drugs or recreation pharmaceuticals | “They would be worried it was some other kind of pill and they’d probably take it away because they don’t want me taking medication they don’t think I need.” |
Note. N=491
Pathways Between AMSM-Parent Normative Beliefs and Intending to Start PrEP
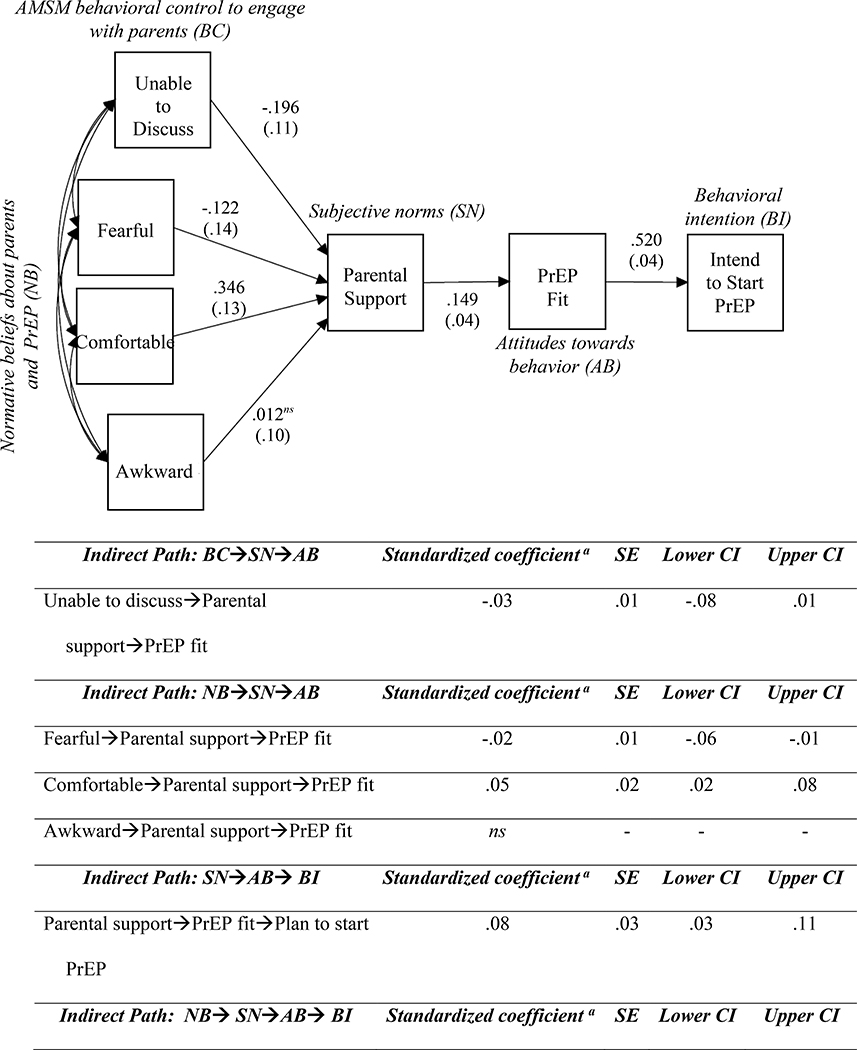
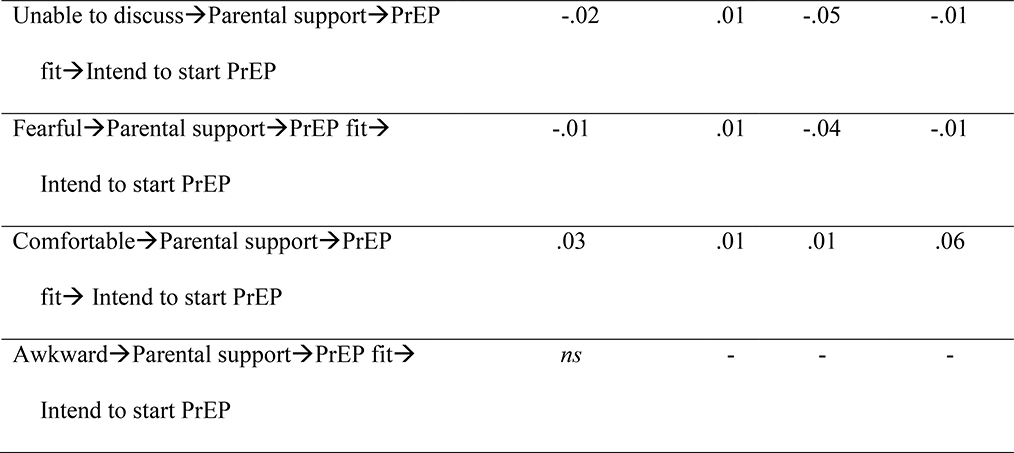
In returning to TPB, Figure 1 shows the path model created from the coded qualitative data (see Table 3) on perceived parental support, perceived PrEP fit, and intending to start it, χ2(15) = 288.56, R2 = .27, p<.001. All three fit indicators were acceptable. The CFI of the model fell within the predefined standard parameters (CFI = .98), as did its RMSEA (estimate = 0.04, 90%CI = 0.00–0.07). Also, the chi-square analysis between the default model and expanded model with indirect pathways (Figure 1) was not significant, χ2(9) = 14.63, p = .10. Table 6 shows the correlations between the included variables and their means, standard deviations, and ranges. Considering the theory, we were looking for whether AMSM assessments of potential parental support (i.e., subjective norms) and PrEP fit (i.e., attitudes towards the behavior) acted as indirect pathways between normative and behavioral control beliefs about parent-teen PrEP communication (see Table 3 themes; i.e., fear, awkwardness, and comfort) and ultimately intending to start PrEP. Three of those four themes were significant and directly related to parental support, and indirectly related through support and PrEP fit to intending to start PrEP. Being fearful about reactions (βindirect = −.01, SE =.01, CI95% = −.04, −.01) and feeling unable to talk to parents (βindirect = −.02, SE =.01, CI95% = −.05, −.01) led to lower support, which in turn led to less PrEP fit, and finally, fewer intentions to start taking PrEP. However, being comfortable talking about PrEP with parents (βindirect = .03, SE =.01, CI95% = .01, .06) led to increased perceived support, increased perceptions that PrEP is a good fit, and increased attitudes towards intending on starting PrEP.
Figure 1. Path model of the relationships between AMSM-parent perceived reactions (normative beliefs) regarding PrEP and their direct and indirect effects on intending to start PrEP (behavioral intention).
The model (N=488) explains 27.0% of the variance, χ2(15) = 288.56, p<.001. CFI =.98. RMSEA estimate = 0.04, 90%CI = 0.00–0.07. Values along the arrows represent the direct standardized coefficients. Parenthesized values represent the standard error of the coefficients. For each indirect effect, we report the statistically significant indirect standardized coefficient (p<.05), the standard error, and the biased-corrected 95% confidence intervals based on 5,000 samples. a Indirect standardized coefficients were derived from the multiplication of the direct standardized coefficients within a path, from start to finish. ns = Not significant (statistically).
Table 6.
Correlation matrix of the direct and indirect variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | M | SD | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Unable to discuss PrEP with parentsa | -- | −.16** | −.17** | −.28** | −.24** | .05 | −.12** | .20 | .40 |
| 2. Fearful of parentsa | -- | −.15** | −.20** | −.15** | −.01 | .03 | .12 | .33 | |
| 3. Comfortable discussing PrEP with parentsa | -- | −.26 ** | .40** | .01 | .09 | .14 | .34 | ||
| 4. Awkward to discuss with parents a | -- | .01 | −.02 | −.05 | .35 | .48 | |||
| 5. Parental support b | -- | .15** | .11* | 2.21 | 1.01 | ||||
| 6. PrEP fit c | -- | .52** | 3.28 | .86 | |||||
| 7. Intend to start PrEP c | -- | 2.96 | .89 |
Note. N = 488.
p<.05.
p<.01.
Ranges:
0–1
1–4
1–5
DISCUSSION
The results of our mixed-methods study extend many of the findings from the few studies exploring adolescents’ knowledge of PrEP and the perceptions about their parents’ role regarding future PrEP use (11, 13, 14). They also support TPB as a theoretical framework explaining parent-related beliefs and norms as obstacles to PrEP uptake. First, virtually the same number of teens had heard of PrEP as in the Macapagal and colleagues sample (about 55%) (14); and relative to the 14–18% having heard in the Thoma and Huebner study (13), there may be a fair increase in awareness over the past 36–48 months. Overall actual use of PrEP remained extremely low (at 2.0% of the entire sample) and in line with these other studies. In terms of where our sample of AMSM had heard about PrEP, the teens reported more diversity than in both of those two studies, including from television commercials and programs. This likely reflects that in a brief timespan, PrEP messaging has begun to infiltrate into mass media, on- and offline (60). None from the sample said they had heard about PrEP from a parent or parents. Unfortunately, parents, who represent an incredibly important influence over teens, remain untapped as a promotional source. Perhaps it is because parents are not aware or knowledgeable regarding PrEP that has led many teens to assume they would be barriers to the biomedical prevention (11, 19); six in ten of our sample reported they perceived their parents would be unsupportive towards PrEP initiation. Ultimately, because of how recently PrEP has been approved for teens, it remains unknown whether parents actually would be unsupportive after they are made aware of PrEP and educated about its implementation as a protective strategy. Inquiry into parental attitudes and perceptions about PrEP is a logical next step.
In turning to some of the qualitative evidence, the normative beliefs held by teens explained why they thought their parents would be an obstacle towards PrEP. Most participants reported feeling they could not ask their parent(s) to go on PrEP because they were fearful or they simply lacked the efficacy to engage in such conversations. In fact, the path model in Figure 1 supports that such feelings are far-reaching and can govern AMSM’s behavioral beliefs about PrEP fit for them and their behavioral intentions to start taking it. Granted, many teenagers, independent of sexual orientation, have reported talking about sex with a parent as difficult to do (61); yet, talking about PrEP for these teens has the added layer of discussing sexual orientation and sexual behaviors at the same time. With one-third of teens in the sample not out to their mother and half not out to their father, it is plausible that, for teens who view PrEP and their sexual orientation as intertwined, conversations about PrEP would be seemingly impossible. This idea was further reinforced when we asked the teenagers to imagine if they were caught using PrEP. Some participants claimed their parents would be extremely upset or angry at this discovery; others even said they would be punished. These perceived reactions mirror research on parents’ varying reactions to sexual orientation disclosure (62–66). Our findings unfortunately may mean that for some, who find themselves with very homophobic parents, PrEP uptake may be too risky for them.
An overwhelming majority of teens suggested that if PrEP were free and their parents would not discover their use of it, they would take it. As a corollary, a majority of teens also said that if they took PrEP, they would actively not want their parents to know. The reasons for these trends became apparent, with the frequency of positive rationales for taking PrEP without parents’ knowledge being greater than the negative ones. The teens claimed that using PrEP without parental knowledge could activate key health and interpersonal needs, such as increased health autonomy, HIV prevention agency, and decreased negative parental assumptions. It would simply allow them to feel more adult-like and responsible. These attitudes support the importance of more States legislating to allow PrEP use without parental consent for those under 18 years old. Considering the data, such legal changes could lead to a measurable increase in use from the 2.0% reported by our sample.
Parents were not described as barriers by all AMSM in our study. Some within the sample understood the logistical complexities of PrEP acquisition and imagined it would be fairly impossible to successfully take the medication without help. Others did not want to be secretive with their parents or had extremely transparent relationships with them. These dueling attitudes towards parental involvement in PrEP uptake suggest the need for diversity in AMSMfocused PrEP promotional campaigns. For some, equipping teens and parents with basic knowledge about PrEP will be enough to provoke conversations, especially among those with open, accepting, and honest family dynamics. Though for most AMSM, information about PrEP will not be enough to overcome myriad fears about parental judgement. This is why allowing teens to access PrEP without their parents’ involvement is so crucial. States that allow for PrEP use without parental consent need to more publicly educate adolescents about their rights. Additionally, messaging that promotes how to discreetly acquire and maintain PrEP could be beneficial for those still living with their parents. Finally and perhaps most important, increasing the total number of States that allow teens to access and use PrEP without parental consent should be a top priority for public health practitioners and legislators who are concerned with ending the epidemic.
Limitations
While the current study provides much needed insight into the fears and barriers surrounding AMSM, parents, and PrEP, it does have limitations. A small percentage of participants came from previous studies implemented by our institute and partner institutes (n=26 or 5.3%)—studies which explicitly introduced or discussed PrEP. This may not have impacted the responses elicited regarding parents and their potential reactions, but it might have contributed to a slight increase in the number of participants previously aware of PrEP. Seventeen participants reporting having learned about PrEP from “research staff.” As a result, our finding 55.2% of participants previously aware of PrEP, while consistent with a different sample from a previous study (14), may therefore not be completely generalizable to AMSM in the general population.
Regarding the qualitative measures, some participants may not have seen PrEP as relevant, which might have contributed to some writing less (or nothing) within their open-ended responses. For example, we asked participants to imagine situations in which they would take PrEP, but some in our sample had not yet experienced anal intercourse or other risk-taking behaviors that would make them PrEP candidates. We did not want to remove them from the analysis and so coded those as not present for the themes. Replicating the study only with teens who have engaged in some condomless penetrative sex might yield different results.
Both the quantitative and qualitative data reported come from a cross-sectional, baseline sample. This has its own limitations, particularly as we employed a path analysis to test the relationships between variables representing TPB theoretical constructs. There may be temporality concerns when exploring the relationship between the normative belief themes (e.g., comfortable discussing PrEP) and subjective norms (i.e., parental support). While research has long suggested normative beliefs influence perceptions of subjective norms (31), it could be argued that believing one’s parents will be generally supportive of PrEP use might lead one to imagine that conversing about use would be easy or comfortable. However, the full path model described was the best fitting model from the data; and it favored normative beliefs as exogenous variables directly and indirectly predicting subjective norms, attitudes towards the behavior, and behavioral intention. Research that more fully measures these theoretical constructs over time is an important future direction for AMSM-PrEP research.
Finally, the teens in the study were enrolled in an intervention research trial, so they might have different experiences or attitudes from those AMSM who are not eligible for, or who otherwise would be unwilling to participate in, such a study. These limitations aside, our study sample was large and diverse—particularly for a rarely studied population like AMSM—and provided extremely detailed fears and concerns that need to be addressed for better uptake of PrEP among adolescents.
CONCLUSIONS
Epidemiological and behavioral understanding of PrEP use among adolescents is in its infancy. With on-label use for minors in its early stages, the barriers and facilitators to increased medication awareness, access, uptake, and maintenance are just being established. What remains clear, even at this early stage, is that parents will be key to increasing access to this novel biomedical prevention technique among AMSM. Our research suggests two considerations. Because the burden will almost certainly fall on parents to begin conversations about PrEP and gauge adolescent interest in its initiation, PrEP awareness among parents needs to increase. Popular media is doing well to promote it (e.g., through commercials aired during popular shows); however, better messaging through social media outlets and in other spaces where parents find health information about their teenagers should be prioritized (e.g., at pediatrician offices). A final consideration suggested by our research concerns how parents should be educated about PrEP. Similar to how birth control has been framed for teenage girls (67–69) and HPV vaccination for teenage girls and boys (70–73), future messaging needs to frame adolescent PrEP use as proactive protection. Teens are clearly afraid of parental assumptions about their behavior, where they fear that discussions about PrEP or discovery of its use will lead to disappointment and punishment. However, if parents are able to enter the conversation with the understanding that taking this medication is a precaution, it opens the door to change AMSM perceived normative beliefs and have better communication about sexual health.
ACKNOWLEDGEMENTS
This work was supported by a grant from the National Institute on Minority Health and Health Disparities (U01MD011281; PI: B. Mustanski). The sponsor had no involvement in the conduct of the research or the preparation of the article. We would like to thank all of the staff across Northwestern University, University of Puerto Rico, Hunter College of the City University of New York, and North Carolina State University for their hard work. Finally, we would like to thank all of the participants in SMART for their time and commitment to the study.
Footnotes
Conflict of Interest
All authors declare that they have no conflicts of interests.
COMPLIANCE WITH ETHICAL STANDARDS
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964
Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
This study (STU#00201997) was granted a waiver of parental consent and waiver of written consent by the institutional review board at Northwestern University.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
REFERENCES
- 1.Centers for Disease Control and Prevention. HIV Surveillance Report, 2017 2018 [updated November 2018. Available from: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2017-vol-29.pdf.
- 2.Mustanski B, Moskowitz DA, Moran KO, Rendina HJ, Newcomb ME, Macapagal K. Factors associated with HIV testing in teenage men who have sex with men. Pediatrics. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ybarra ML, Prescott TL, Phillips GL 2nd, Bull SS, Parsons JT, Mustanski B. Pilot RCT results of an mHealth HIV prevention program for sexual minority male adolescents. Pediatrics. 2017;140(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Macapagal K, Moskowitz DA, Li DH, Carrion A, Bettin E, Fisher CB, et al. Hookup app use, sexual behavior, and sexual health among adolescent men who have sex with men in the United States. J Adolesc Health. 2018;62(6):708–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shannon CL, Keizur EM, Fehrenbacher A, Wood-Palmer D, Ramos W, Koussa M, et al. Sexually Transmitted Infection Positivity Among Adolescents With or at High-Risk for Human Immunodeficiency Virus Infection in Los Angeles and New Orleans. Sexually transmitted diseases. 2019;46(11):737–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macapagal K, Kraus A, Moskowitz DA, Birnholtz J. Geosocial Networking Application Use, Characteristics of App-Met Sexual Partners, and Sexual Behavior Among Sexual and Gender Minority Adolescents Assigned Male at Birth. The Journal of Sex Research. 2019:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mustanski B, Fisher CB. HIV rates are increasing in gay/bisexual teens: IRB barriers to research must be resolved to bend the curve. Am J Prev Med. 2016;51(2):249–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. Pre-exposure prophylaxis (PrEP) Atlanta, GA: Centers for Disease Control and Prevention; 2018. [Available from: https://www.cdc.gov/hiv/risk/prep/. [Google Scholar]
- 9.Pace JE, Siberry GK, Hazra R, Kapogiannis BG. Preexposure Prophylaxis for Adolescents and Young Adults at Risk for HIV Infection: Is an Ounce of Prevention Worth a Pound of Cure? Clinical Infectious Diseases. 2013;56(8):1149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mullins TLK, Lehmann CE. Oral pre-exposure prophylaxis (PrEP) for HIV prevention in adolescents and young adults. Current pediatrics reports. 2018;6(2):114–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huebner DM, Mustanski B. Navigating the long road forward for maximizing PrEP impact among adolescent men who have sex with men. Archives of Sexual Behavior. 2019:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosek SG, Landovitz RJ, Kapogiannis B, Siberry GK, Rudy B, Rutledge B, et al. Safety and feasibility of antiretroviral preexposure prophylaxis for adolescent men who have sex with men aged 15 to 17 years in the United States. JAMA Pediatr. 2017;171(11):1063–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thoma BC, Huebner DM. Brief report: HIV pre-exposure prophylaxis engagement among adolescent men who have sex with men: The role of parent-adolescent communication about sex. J Acquir Immune Defic Syndr. 2018;79(4):453–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Macapagal K, Kraus A, Korpak AK, Jozsa K, Moskowitz DA. PrEP awareness, uptake, barriers, and correlates among adolescent males who have sex with males in the USA. Archives of Sexual Behavior. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher CB, Arbeit MR, Dumont MS, Macapagal K, Mustanski B. Self-consent for HIV prevention research involving sexual and gender minority youth: Reducing barriers through evidence-based ethics. J Empir Res Hum Res Ethics. 2016;11(1):3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fisher CB, Fried AL, Macapagal K, Mustanski B. Patient-provider communication barriers and facilitators to HIV and STI preventive services for adolescent MSM. AIDS Behav. 2018;22(10):3417–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fletcher FE, Fisher C, Buchberg MK, Floyd B, Hotton A, Ehioba A, et al. “Where Did This [PrEP] Come From?” African American Mother/Daughter Perceptions Related to Adolescent Preexposure Prophylaxis (PrEP) Utilization and Clinical Trial Participation. Journal of Empirical Research on Human Research Ethics. 2018;13(2):173–84. [DOI] [PubMed] [Google Scholar]
- 18.Hosek SG, Rudy B, Landovitz R, Kapogiannis B, Siberry G, Rutledge B, et al. An HIV Preexposure Prophylaxis Demonstration Project and Safety Study for Young MSM. J Acquir Immune Defic Syndr. 2017;74(1):21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mustanski B, Macapagal K, Thomann M, Feinstein BA, Newcomb ME, Motley D, et al. Parents’ Perspectives About Adolescent Boys’ Involvement in Biomedical HIV Prevention Research. Arch Sex Behav. 2018;47(7):1923–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasstedt K Ensuring adolescents’ ability to obtain confidential family planning services in Title X. Guttmacher Policy Review. 2018;21:48–54. [Google Scholar]
- 21.Centers for Disease Control and Prevention. Minors’ consent laws for HIV and STD services 2018. [updated November 30, 2018. Available from: https://www.cdc.gov/hiv/policies/law/states/minors.html.
- 22.Hanghøj S, Boisen KA. Self-reported barriers to medication adherence among chronically ill adolescents: a systematic review. Journal of adolescent health. 2014;54(2):121–38. [DOI] [PubMed] [Google Scholar]
- 23.Haberer J, Mellins C. Pediatric adherence to HIV antiretroviral therapy. Current HIV/AIDS Reports. 2009;6(4):194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhee H, Belyea MJ, Brasch J. Family support and asthma outcomes in adolescents: barriers to adherence as a mediator. Journal of adolescent health. 2010;47(5):472–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berg CA, King PS, Butler JM, Pham P, Palmer D, Wiebe DJ. Parental involvement and adolescents’ diabetes management: The mediating role of self-efficacy and externalizing and internalizing behaviors. Journal of pediatric psychology. 2010;36(3):329–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hébert J, Polotskaia A, Joober R, Grizenko N. Adherence to psychostimulant medication in children with attention-deficit/hyperactivity disorder: the role of attitudes. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2013;22(4):317. [PMC free article] [PubMed] [Google Scholar]
- 27.Widman L, Choukas-Bradley S, Noar SM, Nesi J, Garrett K. Parent-adolescent sexual communication and adolescent safer sex behavior: a meta-analysis. JAMA Pediatr. 2016;170(1):52–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: a systematic review. Preventive medicine. 2017;95:26–37. [DOI] [PubMed] [Google Scholar]
- 29.Ajzen I The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [Google Scholar]
- 30.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, N.J.: Prentice-Hall; 1980. 278 p. [Google Scholar]
- 31.Glassman M, Fitzhenry N. Fishbein’s subjective norm: Theoretical considerations and empirical evidence. ACR North American Advances. 1976. [Google Scholar]
- 32.Rendina HJ, Whitfield TH, Grov C, Starks TJ, Parsons JT. Distinguishing hypothetical willingness from behavioral intentions to initiate HIV pre-exposure prophylaxis (PrEP): Findings from a large cohort of gay and bisexual men in the US. Social Science & Medicine. 2017;172:115–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schnarrs PW, Gordon D, Martin-Valenzuela R, Sunil T, Delgado AJ, Glidden D, et al. Perceived social norms about oral PrEP use: differences between African–American, Latino and White gay, bisexual and other men who have sex with men in Texas. AIDS and Behavior. 2018;22(11):3588–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir Immune Defic Syndr. 2009;50(1):77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sieverding JA, Adler N, Witt S, Ellen J. The influence of parental monitoring on adolescent sexual initiation. Archives of pediatrics & adolescent medicine. 2005;159(8):724–9. [DOI] [PubMed] [Google Scholar]
- 36.Coley RL, Lombardi CM, Lynch AD, Mahalik JR, Sims J. Sexual partner accumulation from adolescence through early adulthood: The role of family, peer, and school social norms. Journal of Adolescent Health. 2013;53(1):91–7. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marcoux BC, Shope JT. Application of the theory of planned behavior to adolescent use and misuse of alcohol. Health education research. 1997;12(3):323–31. [Google Scholar]
- 38.Murnaghan DA, Blanchard CM, Rodgers WM, LaRosa JN, MacQuarrie CR, MacLellan DL, et al. Predictors of physical activity, healthy eating and being smoke-free in teens: A theory of planned behaviour approach. Psychology and Health. 2010;25(8):925–41. [DOI] [PubMed] [Google Scholar]
- 39.Lac A, Alvaro EM, Crano WD, Siegel JT. Pathways from parental knowledge and warmth to adolescent marijuana use: An extension to the theory of planned behavior. Prev Sci. 2009;10(1):22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Coley RL, Votruba-Drzal E, Schindler HS. Trajectories of parenting processes and adolescent substance use: reciprocal effects. Journal of Abnormal Child Psychology. 2008;36(4):613–25. [DOI] [PubMed] [Google Scholar]
- 41.Hutchinson MK, Montgomery AJ. Parent communication and sexual risk among African Americans. Western Journal of Nursing Research. 2007;29(6):691–707. [DOI] [PubMed] [Google Scholar]
- 42.Hutchinson MK, Jemmott JB 3rd, Jemmott LS, Braverman P, Fong GT. The role of mother-daughter sexual risk communication in reducing sexual risk behaviors among urban adolescent females: a prospective study. J Adolesc Health. 2003;33(2):98–107. [DOI] [PubMed] [Google Scholar]
- 43.Murphy SA. An experimental design for the development of adaptive treatment strategies. Stat Med. 2005;24(10):1455–81. [DOI] [PubMed] [Google Scholar]
- 44.Mustanski B, Greene GJ, Ryan D, Whitton SW. Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: The Queer Sex Ed intervention. J Sex Res. 2015;52(2):220–30. [DOI] [PubMed] [Google Scholar]
- 45.Mustanski B, Parsons JT, Sullivan PS, Madkins K, Rosenberg E, Swann G. Biomedical and behavioral outcomes of Keep It Up!: An eHealth HIV prevention program RCT. Am J Prev Med. 2018;55(2):151–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mustanski B, Garofalo R, Monahan C, Gratzer B, Andrews R. Feasibility, acceptability, and preliminary efficacy of an online HIV prevention program for diverse young men who have sex with men: The Keep It Up! intervention. AIDS Behav. 2013;17(9):2999–3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Madkins K, Moskowitz DA, Moran K, Dellucci TV, Mustanski B. Measuring Acceptability and Engagement of The Keep It Up! Internet-Based HIV Prevention Randomized Controlled Trial for Young Men Who Have Sex With Men. AIDS Education and Prevention. 2019;31(4):287–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.CDC. Compendium of evidence-based interventions and best practices for HIV prevention Atlanta, GA: Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention; 2019. [Available from: https://www.cdc.gov/hiv/research/interventionresearch/compendium/index.html. [Google Scholar]
- 49.Parsons JT, Lelutiu-Weinberger C, Botsko M, Golub SA. A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. J Consult Clin Psychol. 2014;82(1):9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mustanski B Ethical and regulatory issues with conducting sexuality research with LGBT adolescents: A call to action for a scientifically informed approach. Arch Sex Behav. 2011;40(4):673–86. [DOI] [PubMed] [Google Scholar]
- 51.Bauermeister JA, Meanley S, Pingel E, Soler JH, Harper GW. PrEP awareness and perceived barriers among single young men who have sex with men. Curr HIV Res. 2013;11(7):520–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Parsons JT, Rendina HJ, Lassiter JM, Whitfield TH, Starks TJ, Grov C. Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States: The motivational PrEP Cascade. J Acquir Immune Defic Syndr. 2017;74(3):285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. [DOI] [PubMed] [Google Scholar]
- 54.Neuendorf KA. The content analysis guidebook: Sage; 2016. [Google Scholar]
- 55.Fleiss JL. Measuring nominal scale agreement among many raters. Psychological Bulletin. 1971;76(5):378–82. [Google Scholar]
- 56.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. [PubMed] [Google Scholar]
- 57.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–46. [DOI] [PubMed] [Google Scholar]
- 58.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling-a Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- 59.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–91. [DOI] [PubMed] [Google Scholar]
- 60.Finlayson T Changes in HIV Preexposure Prophylaxis Awareness and Use Among Men Who Have Sex with Men—20 Urban Areas, 2014 and 2017. MMWR Morbidity and mortality weekly report. 2019;68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thompson SH, Yannessa JF, Dunn MS, McGough FM, Duffy JL. Let’s talk about sex: Parents’ and teen’s comfort levels during these discussions. American Journal of Health Studies. 2015;30(1). [Google Scholar]
- 62.Chrisler AJ. Understanding parent reactions to coming out as lesbian, gay, or bisexual: A theoretical framework. Journal of Family Theory & Review. 2017;9(2):165–81. [Google Scholar]
- 63.Newcomb ME, Feinstein BA, Matson M, Macapagal K, Mustanski B. “I have no idea what’s going on out there:” Parents’ perspectives on promoting sexual health in lesbian, gay, bisexual and transgender adolescents. Sexuality Research and Social Policy. 2018;15(2):111–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baiocco R, Fontanesi L, Santamaria F, Ioverno S, Marasco B, Baumgartner E, et al. Negative parental responses to coming out and family functioning in a sample of lesbian and gay young adults. Journal of Child and Family Studies. 2015;24(5):1490–500. [Google Scholar]
- 65.Pistella J, Salvati M, Ioverno S, Laghi F, Baiocco R. Coming-out to family members and internalized sexual stigma in bisexual, lesbian and gay people. Journal of Child and Family Studies. 2016;25(12):3694–701. [Google Scholar]
- 66.Baiocco R, Fontanesi L, Santamaria F, Ioverno S, Baumgartner E, Laghi F. Coming out during adolescence: Perceived parents’ reactions and internalized sexual stigma. Journal of health psychology. 2016;21(8):1809–13. [DOI] [PubMed] [Google Scholar]
- 67.Duncan R, Anderson L, Pickering N. Closing the Gap between Need and Uptake: a Case for Proactive Contraception Provision to Adolescents. Asian Bioethics Review. 2019;11(1):95–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Akers AY, Schwarz EB, Borrero S, Corbie-Smith G. Family discussions about contraception and family planning: a qualitative exploration of black parent and adolescent perspectives. Perspectives on sexual and reproductive health. 2010;42(3):160–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Melo J, Peters M, Teal S, Guiahi M. Adolescent and young women’s contraceptive decision-making processes: choosing “The Best Method for Her”. Journal of pediatric and adolescent gynecology. 2015;28(4):224–8. [DOI] [PubMed] [Google Scholar]
- 70.Fu LY, Bonhomme L-A, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014;32(17):1901–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alexander AB, Stupiansky NW, Ott MA, Herbenick D, Reece M, Zimet GD. What parents and their adolescent sons suggest for male HPV vaccine messaging. Health Psychology. 2014;33(5):448. [DOI] [PubMed] [Google Scholar]
- 72.Nan X, Madden K, Richards A, Holt C, Wang MQ, Tracy K. Message framing, perceived susceptibility, and intentions to vaccinate children against HPV among African American parents. Health communication. 2016;31(7):798–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sadaf A, Richards JL, Glanz J, Salmon DA, Omer SB. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine. 2013;31(40):4293–304. [DOI] [PubMed] [Google Scholar]