Abstract
Purpose:
The aim is to assess the relationship between cervicothoracic inflection point and baseline disability, as well as the relationship between clinical outcomes and pre- to postoperative changes in inflection point.
Methods:
Cervical deformity (CD) patients with baseline and 3-month (3M) postoperative radiographic, clinical, and inflection data were grouped by region of inflection point: C6 or above, C6-C7 to C7-T1, T1, or below. Inflection was defined as: Distal-most level where cervical lordosis (CL) changes to thoracic kyphosis (TK). Differences in alignment and patient factors across pre- and postoperative inflection point groups were assessed, as were outcomes by the inclusion of inflection in the CD-corrective fusion construct.
Results:
A total of 108 patients were included. Preoperative inflection breakdown: C6 or above (42%), C6-C7 to C7-T1 (44%), T1 or below (15%). Surgery was associated with a caudal migration of inflection by 3M: C6 or above (8%), C6-C7 to C7-T1 (58%), T1 or below (33%). For patients with preoperative inflection T1 or below, the inclusion of inflection in the fusion construct was associated with improvements in horizontal gaze (McGregor's Slope included: −11.3° vs. not included: 1.6°, P = 0.038). The inclusion of preoperative inflection in fusion was associated with the superior cervical sagittal vertical axis (cSVA) changes for C6-C7 to C7-T1 patients (−5.2 mm vs. 3.2 mm, P = 0.018). The location of postoperative inflection was associated with variation in 3M alignment: Inflection C6 or above was associated with less Pelvic Tilt (PT), PT and a trend of larger cSVA. Location of inflection or inclusion in fusion was not associated with reoperation or distal junctional kyphosis.
Conclusions:
Incorporating the inflection point between CL and TK in the fusion construct was associated with superior restoration of cervical alignment and horizontal gaze for surgical CD patients.
Keywords: Cervical deformity, cervicothoracic junction, inflection, outcomes, surgery
INTRODUCTION
The cervical spine serves as a crucial column of support responsible for transmitting the weight of the cranium. Critical in establishing the harmonious sagittal balance of the cervical spine is the cervicothoracic junction.[1] As the cervicothoracic junction serves as a transition point between the flexible cervical spine and the rigid thoracic spine, it is thought to be a biomechanically important site in bearing axial weight from the head.[2,3]
To date, few studies have investigated the inflection point between cervical lordosis (CL) and thoracic kyphosis (TK), particularly in the context of cervical deformity (CD). One radiographic survey of 172 lateral spinal radiographs from nondeformed patients suggests that the natural inflection point between the cervical and thoracic curves is near T3 and that an age-related cranial shift in the cervicothoracic inflection point may be normal.[4] Cranial migration of the cervicothoracic inflection point may be associated with an anterior shift in cervical sagittal alignment, resulting in increased shear stress at the cervicothoracic transition. It remains unclear, however, whether a relationship exists between cervicothoracic inflection point, sagittal alignment, or neck disability for patients diagnosed with CD.
The present study aims to assess the relationship between cervicothoracic inflection point, sagittal alignment, and neck disability for surgical CD patients. Specifically, as CD-corrective surgery is associated with significant pre- to postoperative changes in cervical sagittal alignment, this study seeks to investigate whether operative intervention is associated with similar changes in cervicothoracic inflection point and whether including inflection point in the fusion construct is associated with superior clinical or radiographic outcomes.
MATERIALS AND METHODS
Study design
This study analyzes a database of consecutive CD patients >18 years old prospectively enrolled at 13 spine centers across the United States. All patients presented for surgical evaluation of CD, defined from baseline radiographs as cervical kyphosis (C2-C7 sagittal Cobb angle >10°), cervical scoliosis (C2-C7 coronal Cobb angle >10°), C2-C7 sagittal vertical axis (cSVA) >4 cm or chin-brow vertical angle >25°. Patients with active tumors, infection, or deformity of neuromuscular etiology were excluded from the database.
Data collection and radiographic assessment
Standardized forms collected patient demographic and comorbidity (including Charlson Comorbidity Index score) information.[5] Patient frailty was assessed using the previously published modified CD frailty index.[6] The following validated health-related quality of life (HRQL) measures were administered to patients at baseline and follow-up intervals: Numeric Rating Scales for Neck and Back Pain, Neck Disability Index (NDI), and the 5-dimension, 3-level EuroQol questionnaire.[7,8] The modified Japanese Orthopaedic Association (mJOA) was also administered as a measure of cervical myelopathy severity.[9]
Standing anterior-posterior and lateral long-cassette radiographs and corresponding cervical radiographs were analyzed using validated software (Spine view, ENSAM Laboratory of Biomechanics, Paris, France) as previously published.[10,11,12] Long cassette radiographs were used to assess global alignment through the SVA (horizontal distance from C7 plumbline relative to the posterosuperior corner of S1). Regional alignment parameters assessed were pelvic tilt (PT), pelvic incidence (PI), TK, lumbar lordosis (LL), CL, cSVA, and T1 slope [Figure 1]. Upper-cervical alignment parameters included C0-C2 sagittal Cobb angle (C0-C2), C2 slope, and McGregor's slope (McGS; a validated measure of horizontal gaze).[13] Mismatches between T1 slope and CL (TS-CL), and PI and LL (PI-LL) were calculated as measures of harmonious cervical and thoracolumbar alignment, respectively. The cervicothoracic inflection point was identified numerically as the level where CL changes to TK. For patients with multiple inflection points, the distal-most was included in the analysis.
Figure 1.
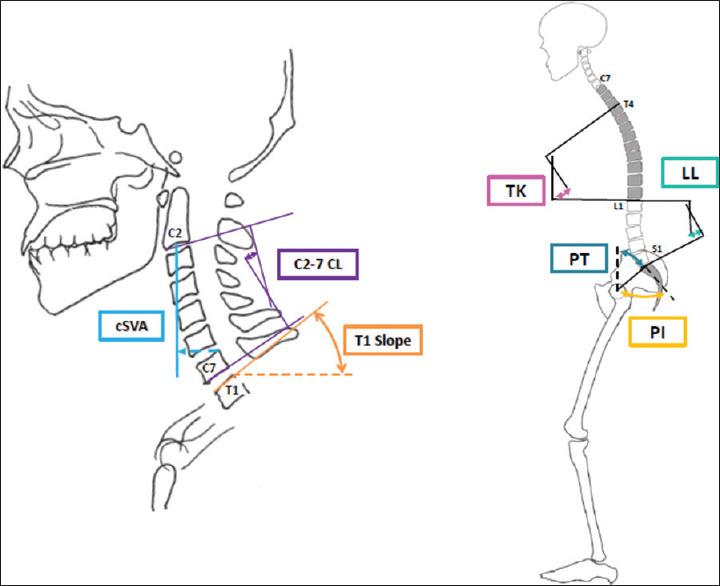
Schematic demonstrating common cervical sagittal alignment parameters (C2-C7 cervical lordosis [CL], C2-C7 sagittal vertical axis [cSVA], T1 slope) and regional alignment paramters (T4-T12 thoracic kyphosis [TK], L1-S1 lumbar lordosis [LL], pelvic tilt [PT], pelvic incidence [PI])
Statistical analysis
This study hypothesizes that there is a relationship between cervicothoracic inflection points and outcomes following CD-corrective surgery. Only patients with available radiographic, HRQL, and cervicothoracic inflection point data at pre- and 3-month (3M) postoperative study intervals were retained for the analysis. Descriptive analyses summarized demographic, clinical, and radiographic variables. Pre- to postoperative changes in alignment were assessed with paired samples t-tests. Patients were grouped by region of postoperative cervicothoracic inflection point: C6 or above, C6-C7 to C7-T1, and T1 or below. Differences in demographic, clinical, surgical, and radiographic variables were assessed across patient groups using analysis of variance for continuous variables and Chi-squared tests for categorical variables. Secondary analysis grouped patients by the inclusion of postoperative inflection points in the fusion construct. Independent samples t- tests compared patients whose inflection points were included in the fusion construct to patients whose inflection points were not for differences in clinical and radiographic variables. Pearson bivariate correlation assessed the relationship between pre-to postoperative changes in an inflection point, alignment, and clinical outcomes. All analyses were conducted with SPSS software (version 23.0, IBM, Armonk, New York). All statistical tests were two-tailed; P < 0.05 were considered statistically significant.
RESULTS
Cohort overview
Overall, 108 patients met inclusion criteria and were included in the analysis. Table 1 provides a demographic, surgical, and radiographic description of the overall cohort. By Ames Classification descriptor, 55.7% of patients had “cervical” deformity drivers, 26.4% had “cervicothoracic,” 11.3% had “thoracic” and 6.6% had “coronal.” At baseline, patients presented with moderate horizontal gaze disruption (McGS: 4.4°±13.6) and moderate-to-severe cervical malalignment, as assessed by TS-CL (37.6°±18.5) and cSVA (47.0 mm ± 25.7). At 3M postop, the overall cohort showed significant improvement in cervical alignment: cSVA (37.3 mm ± 18.9), TS-CL (26.8°±13.2), McGS (-2.0°±8.2, all P < 0.001), as well as distal alignment: TK (-40.3°±15.7 to-43.0°±15.5, P = 0.013).
Table 1.
Preoperative demographic, surgical, and radiographic overview of the included cervical deformity cohort (n=108)
| Mean (± Standard Deviation) or Frequency (%) | |
|---|---|
| Demographics | |
| Age (years) | 61.2±10.5 |
| Body Mass Index (kg/m2) | 29.2±7.7 |
| Sex (% female) | 66.4% |
| Surgical Factors | |
| Levels fused | 8.3±4.5 |
| Posterior-only surgical approach | 52.8% |
| Anterior-only surgical approach | 15.7% |
| Combined surgical approach | 31.5% |
| Any osteotomy | 55.6% |
| Smith Petersen osteotomy | 18.5% |
| Pedicle subtraction osteotomy | 16.7% |
| Vertebral column resection | 6.0% |
| Sagittal Radiographic Alignment | |
| PT (°) | 19.7±11.0 |
| PI-LL (°) | 1.0±17.0 |
| SVA (mm) | 3.7±68.0 |
| TK (°) | -40.3±15.7 |
| CL (°) | -5.0±20.8 |
| TS-CL (°) | 37.6±18.5 |
| cSVA (mm) | 47.0±25.7 |
| C0-C2 sagittal Cobb (°) | 33.3±11.3 |
| McGregor’s Slope (°) | 4.4±13.6 |
Cohort breakdown by the inflection point
Preoperatively, the overall breakdown by inflection point was: C6 or above (42%), C6-C7 to C7-T1 (44%), T1 or below (15%). There was significant variation in inflection point across Ames descriptor groups, with the majority of “cervical” patients having inflection points from C6-C7 to C7-T1, the majority of “cervicothoracic” patients having inflection points C6 or above, and the majority of “thoracic” patients having inflection points T1 or below [Table 2, P = 0.002].
Table 2.
Breakdown of baseline cervicothoracic inflection point location (C6 or above, C6-C7 to C7-T1, T1 or below) across patients stratified by Ames cervical deformity types
| Ames Descriptor Group | C6 or above (n=9) | C6-C7 to C7-T1 (n=63) | T1 or below (n=36) | p |
|---|---|---|---|---|
| Cervical | 35.6% | 52.5% | 11.9% | 0.002 |
| Cervicothoracic | 64.3% | 25.0% | 10.7% | |
| Thoracic | 33.3% | 25.0% | 41.7% | |
| Coronal | 0.0% | 85.7% | 14.3% |
Radiographic assessment by inflection point
Overall, CD-corrective surgery was associated with a caudal migration of cervicothoracic inflection by 3M postop: C6 or above (8%), C6-C7 to C7-T1 (58%), T1 or below (33%). Figure 2 shows the breakdown of postoperative inflection point by preoperative inflection point groups–of note, the majority of patients with preoperative inflection points C6 or above showed caudal migration of inflection point to C6-C7/C7-T1 (55.6%), while the majority of patients with preoperative inflection points T1 or below showed cranial migration of inflection point to C6-C7/C7-T1 (68.8%).
Figure 2.
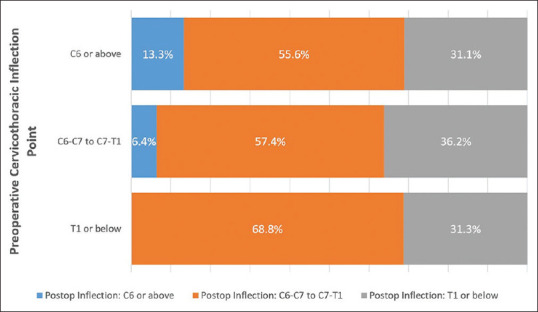
A breakdown of postoperative inflection point by preoperative inflection point groups
Across postop inflection point groups, there were no differences in preopertive alignment for upper-cervical, cervical, or global alignment parameters, though those with postop inflection C6 or above showed significantly less pelvic retroversion (PT) and a trend of larger cSVA [Table 3]. Following surgery, inflection points C6 or above were associated with a greater deformity in cSVA and CL. Postop inflection groups did not differ in pre-to postop alignment changes for any radiographic parameters (all P > 0.05).
Table 3.
Comparison of baseline (BL) and 3-month postoperative (3M) sagittal alignment across patients grouped by location of postoperative inflection point (C6 or above, C6-C7 to C7-T1, T1 or below)
| C6 or above (n=9) | C6-C7 to C7-T1 (n=63) | T1 or below (n=36) | p | ||
|---|---|---|---|---|---|
| Sagittal Alignment | |||||
| PT (°) | BL | 8.1±12.6 | 21.6±9.3 | 19.1±12.0 | *P=0.002 |
| 3M | 11.0±12.4 | 22.3±9.1 | 20.5±12.0 | *P=0.011 | |
| PI-LL (°) | BL | -11.1±26.4 | 1.9±14.0 | 2.4±18.3 | P=0.081 |
| 3M | -6.9±22.3 | 5.4±13.3 | 3.6 ±20.0 | P=0.119 | |
| SVA (mm) | BL | -12.8±55.3 | -2.4±65.7 | 18.4±73.8 | P=0.267 |
| 3M | -16.1±44.6 | 32.2±69.4 | 32.8±72.0 | P=0.133 | |
| TK (°) | BL | -35.2±21.1 | -40.1±15.3 | -41.9±15.2 | P=0.520 |
| 3M | -36.7±20.4 | -43.7±14.0 | -43.3±16.9 | P=0.439 | |
| cSVA (mm) | BL | 57.8±17.5 | 49.9±24.4 | 38.9±28.4 | P=0.066 |
| 3M | 52.7±11.8 | 41.9±17.5 | 29.7±19.0 | *P<0.001 | |
| CL (°) | BL | -9.8±15.4 | -2.4±22.5 | -8.2±18.9 | P=0.353 |
| 3M | -1.9±15.0 | 10.6±16.4 | 4.5±14.8 | *P=0.040 | |
| TS-CL (°) | BL | 39.7±17.5 | 38.3±24.4 | 38.9±28.4 | P=0.796 |
| 3M | 29.0±13.4 | 28.4±13.0 | 25.6±15.9 | P=0.617 | |
| C0-C2 sagittal Cobb (°) | BL | 36.8±9.6 | 32.0±11.6 | 35.0±11.0 | P=0.369 |
| 3M | 32.4±9.5 | 27.0±10.7 | 27.0±10.8 | P=0.350 | |
| McGregor’s Slope (°) | BL | 6.4±13.0 | 6.0±14.5 | 0.7±11.5 | P=0.244 |
| 3M | -0.8±9.2 | -2.1±8.5 | -3.5±8.1 | P=0.623 | |
| C2 slope (°) | BL | 42.8±18.4 | 38.6±20.6 | 35.9±17.5 | P=0.599 |
| 3M | 31.7±13.0 | 26.2±13.0 | 23.9±14.3 | P=0.303 | |
Bolded and asterisked values indicate statistical significance to p<0.05.
Demographic and surgical assessment by the cervicothoracic inflection point
There were no differences in baseline demographics, frailty, or comorbidity burden across postop inflection point groups [Table 4]. There was no difference in fusion length across inflection point groups, though osteotomy was associated with higher rates of postoperative cervicothoracic inflection above T1.
Table 4.
Comparison of demographic and surgical factors across patients grouped by postoperative location of inflection point (C6 or above, C6-C7 to C7-T1, T1 or below)
| C6 or above (n=9) | C6-C7 to C7-T1 (n=63) | T1 or below (n=36) | p | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 64.1±10.2 | 61.4±9.9 | 60.1±11.7 | P=0.572 |
| BMI (kg/m2) | 30.3±7.2 | 29.0±7.3 | 29.1±8.7 | P=0.889 |
| Sex (% female) | 33% | 67% | 74% | P=0.068 |
| Charlson Comorbidity Index (CCI score) | 1.22±1.09 | 0.89±1.19 | 1.35±1.76 | P=0.319 |
| Frailty (mCD-FI score) | 0.34±0.14 | 0.29±0.14 | 0.31±0.14 | P=0.473 |
| Surgical Factors | ||||
| Number of levels fused | 8.8±4.7 | 8.8±4.9 | 7.2±3.6 | P=0.305 |
| Any Posterior Osteotomy (%) | 56% | 65% | 39% | *P=0.041 |
| Smith Petersen Osteotomy (%) | 22.2% | 19.0% | 16.7% | P=0.916 |
| Pedicle Subtraction Osteotomy (%) | 33.3% | 19.0% | 8.3% | P=0.145 |
| Vertebral Column Resection (%) | 0.0% | 7.9% | 2.8% | P=0.419 |
Bolded and asterisked values indicate statistical significance to p<0.05
Clinical assessment by inflection point
There were no differences across preoperative inflection point groups in baseline HRQL scores (all P > 0.1). Although patients with postoperative inflection points T1 or below showed significantly lower levels of preoperative back pain, there were no significant differences across inflection point groups in clinical outcomes at 3M postop [Table 5]. There was a trend of superior postop NDI (P = 0.078) and back pain (P = 0.054) outcomes for patients with inflection points T1 or below. Pre-to postoperative changes in clinical outcomes did not differ across inflection groups (all P > 0.05). The length of inpatient stay similarly did not differ across inflection groups (P = 0.890).
Table 5.
Comparison of health-related quality of life scores at both baseline (BL) and 3-month postoperative (3M) intervals across patients grouped by location of postoperative inflection point (C6 or above, C6-C7 to C7-T1, T1 or below)
| C6 or above (n=9) | C6-C7 to C7-T1 (n=63) | T1 or below (n=36) | p | ||
|---|---|---|---|---|---|
| Clinical Outcome Assessment | |||||
| Numeric Rating Scale - Back Pain | BL | 6.0±2.6 | 5.9±2.9 | 4.3±3.3 | *P=0.042 |
| 3M | 5.6±2.7 | 5.5±3.1 | 3.9±3.4 | P=0.054 | |
| Numeric Rating Scale - Neck Pain | BL | 7.4±1.1 | 7.0±2.5 | 6.7±2.5 | P=0.688 |
| 3M | 5.3±2.1 | 4.6±3.0 | 3.4±2.7 | P=0.078 | |
| Neck Disability Index score | BL | 47.8±23.7 | 48.1±17.5 | 47.6±17.5 | P=0.992 |
| 3M | 50.7±15.3 | 44.2±21.6 | 41.2±16.9 | P=0.417 | |
| mJOA score | BL | 13.4±3.4 | 13.4±2.7 | 13.9±2.8 | P=0.992 |
| 3M | 13.1±2.4 | 14.2±2.8 | 14.3±2.8 | P=0.267 | |
| EQ-5D score | BL | 0.72±0.06 | 0.74±0.06 | 0.73±0.07 | P=0.801 |
| 3M | 0.71±0.05 | 0.76±0.08 | 0.76±0.07 | P=0.890 | |
Bolded and asterisked values indicate statistical significance to p<0.05
Outcomes by the inclusion of inflection point in fusion
Overall, 77.8% of patients had their preoperative inflection points included in the fusion construct. Following surgery, 75.9% of patients had inflection points within the fusion construct. Overall, the inclusion of preoperative inflection point in the fusion construct was not associated with differences in postop distal alignment or compensatory global alignment (all P > 0.05); however, for patients with preop inflection points T1 or below, the inclusion of inflection point in the fusion construct was associated with significant pre-to postop improvements in horizontal gaze (McGS of included:-11.3° vs. not included: 1.6°, P = 0.038). Similarly, for patients with preoperative inflection points from C6-C7 to C7-T1, inclusion of inflection point in fusion was associated with superior pre-to postop cSVA changes [−5.2 mm vs. 3.2 mm, P = 0.018, Figure 3]. Including preoperative inflection point in fusion was not associated with superior pre-to postoperative HRQL or mJOA changes, both overall and by the level of inflection point (all P > 0.05).
Figure 3.
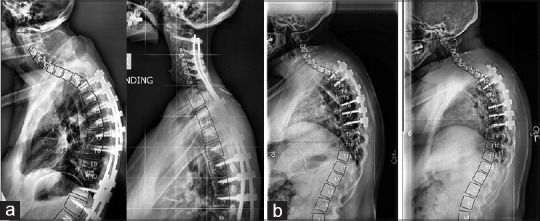
Preoperative (left) and 3-month postoperative (right) case examples of patients with preoperative inflection points C6-C7 to C7-T1. (a) a patient with a preoperative cervicothoracic inflection point at C7-T1 that was included in the fusion construct. This patient's cervical sagittal vertical axis consequently improved from 59.2 mm at baseline to 35.0 mm at 3-months. (b) Shows a patient with a preoperative cervicothoracic inflection point at C7-T1 that was not included in the fusion construct. This patient's cervical sagittal vertical axis consequently deteriorated from 63.8 mm at baseline to 72.5 mm at 3-months
Patients with postoperative inflection points included in the fusion construct showed superior pre-to postop changes in horizontal gaze (McGS: −8.3° vs. not included: −2.3°, P = 0.008), TS-CL (−12.6° vs. −5.3°, P = 0.025), and cSVA (−12.9 mm vs. −1.9 mm, P = 0.007). Including postop inflection point in fusion was not associated with superior pre-to postoperative HRQL or mJOA changes (all P > 0.05). Caudal pre-to postoperative change in inflection point correlated with kyphotic pre-to post-operative changes in CL (r = 0.237, P = 0.026), but greater reductions in cSVA (r = −0.254, P = 0.017), C2 slope (r = −0.200, P = 0.040), and C0-C2 Cobb (r = −0.227, P = 0.037).
Neither location of postoperative inflection point nor the inclusion of pre-operative inflection point in the fusion construct were associated with reoperation (P = 0.526) or distal junctional kyphosis (DJK) development (P = 0.353) by 3M postoperative.
DISCUSSION
Previous research makes clear that the evaluation and treatment of CD requires a thorough understanding of the relationship between the cervical, thoracic, and lumbar curves.[14] Although there is wide variation in the cervical curvature of healthy individuals, asymptomatic subjects typically present with lordotic cervical alignment,[15] as this configuration can resist large compressive loads, effectively minimizing the stress on vertebral body endplates.[16,17] In the cervicothoracic region, transition from the lordotic cervical spine to the kyphotic thoracic spine results in appreciable levels of mechanical stress – as a result, the cervicothoracic junction plays an important role in the biomechanics of CD. Despite this biomechanical importance, relatively few studies in the CD literature have investigated the relationship between cervicothoracic inflection point, sagittal alignment, and neck disability. This study showed that for patients undergoing CD-corrective surgery, there was little relationship between the location of the postoperative cervicothoracic inflection point, alignment outcomes, or clinical outcomes. Incorporating the postoperative inflection point in the fusion construct, however, was associated with superior restoration of cervical alignment and horizontal gaze.
Previous research has used the spatial relationship between vertebral bodies to describe variations in sagittal spinal alignment. For example, Roussouly and Nnadi identified the thoracolumbar inflection point-or the point at which the orientation of the thoracolumbar vertebral bodies change-as a key attribute that can be used to delineate four different types of normal spinal curvatures.[18] In addition to describing variation in sagittal spinal shape among healthy adults, this method of classification has also been used to describe variations in alignment among patients diagnosed with adult spinal deformity.[19] Recent research highlights a relationship between these different spine types and clinical outcomes following lumbar disc arthroplasty, suggesting that variation in the inflection point between spinal curves could be an important consideration in indicating patients for surgery.[20] Although classification systems exist in the literature to describe the sagittal profiles of patients with different types of CD, these frameworks do not incorporate assessments of the cervicothoracic inflection point.[21] The results of this study show significant variations in sagittal alignment across inflection point groups, suggesting a potential rationale for modifying existing CD classification systems to incorporate inflection point.
The results of this study also show that for some CD patients, inclusion of preoperative inflection point in the fusion construct is associated with superior postoperative radiographic outcomes. Specifically, for CD patients with preoperative inflection points T1 or below, the inclusion of inflection point in the fusion construct is associated with superior improvements in the horizontal gaze. For patients with preoperative inflection from C6-C7 to C7-T1, inclusion of inflection point in the fusion construct is also associated with superior cSVA changes. These results are comparable to previous research showing that for CD patients with cervicothoracic drivers of deformity, inclusion of the deformity driver in surgery may be associated with relaxation of lumbopelvic compensation.[22] Importantly, however, whereas previous research shows that including the deformity driver in surgery may be associated with distal changes in alignment, this study shows that including the cervicothoracic inflection point in surgery may be associated with superior changes in cervical alignment and horizontal gaze—both key goals of CD-corrective surgery. These results suggest that the cervicothoracic inflection point may be an important factor to consider in the surgical planning process, though further research is necessary to determine the rate of overlap between inflection point and primary deformity driver.
Guidelines for selecting the appropriate caudal “end level” in long-segment posterior cervical fusion vary across the literature. The consequences of end level selection can be dramatic, with previous research highlighting a potential connection between the inappropriate selection of the lower-most instrumented vertebrae and incidence of DJK.[23] A number of studies suggest that ending posterior fusion constructs at C7 (as opposed to T1) results in inferior postoperative cervical sagittal alignment, and is associated with an increased rate of surgical revision.[24,25] Our study did not show a difference in the rate of DJK between patients whose cervicothoracic inflection points were included in surgery and patients whose inflection points were not; however, it did show superior postoperative alignment outcomes for those with inflection points included in the fusion construct. These results indicate that the cervicothoracic inflection point may warrant additional consideration by the surgeon when deciding the optimal lower-most instrumented vertebrae for patients undergoing CD-corrective surgery.
This study appreciates a number of limitations, including a limited sample size and a retrospective study design. A particularly important limitation of this study was the inclusion of a heterogeneous population of CD patients. Although including patients form 13 surgical centers provides our analysis with increased generalizability and a patient population representative of CD in the United States, it also results in a patient population with many different types of CD. For example, per the radiographic definition of CD used in this study, some patients may have presented with severe cervical kyphosis (C2-C7 sagittal Cobb angle >10°), while others may have presented with cervical hyperlordosis and severe cSVA deformity (>4 cm). These different types of deformity may be associated with substantial differences in treatment strategy, which in turn may influence radiographic outcomes.
CONCLUSION
Surgery to correct CD was associated with caudal migration of the inflection point between CL and TK. For patients with preoperative inflection points at T1 or below, the inclusion of the inflection point in the fusion construct was associated with significant improvements in the horizontal gaze. Similarly, for patients with preoperative inflection points from C6-C7 to C7-T1, inclusion of inflection point in fusion was associated with superior changes in cervical sagittal alignment. The location of the postoperative inflection point was also associated with variation in postoperative cervical and distal alignment. These findings suggest that the assessment of CD may warrant additional consideration of the cervicothoracic inflection point, particularly as it relates to the appropriate “end level” selection of the CD-corrective fusion construct.
Financial support and sponsorship
The International Spine Study Group is funded through research grants from DePuy Synthes and individual donations.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10:994–8. doi: 10.1016/j.spinee.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 2.Scheer JK, Tang JA, Smith JS, Acosta FL, Jr, Protopsaltis TS, Blondel B, et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J Neurosurg Spine. 2013;19:141–59. doi: 10.3171/2013.4.SPINE12838. [DOI] [PubMed] [Google Scholar]
- 3.Yokoyama K, Kawanishi M, Yamada M, Tanaka H, Ito Y, Kawabata S, et al. Age-related variations in global spinal alignment and sagittal balance in asymptomatic Japanese adults. Neurol Res. 2017;39:414–8. doi: 10.1080/01616412.2017.1296654. [DOI] [PubMed] [Google Scholar]
- 4.Boyle JJ, Milne N, Singer KP. Influence of age on cervicothoracic spinal curvature: An ex vivo radiographic survey. Clin Biomech (Bristol, Avon) 2002;17:361–7. doi: 10.1016/s0268-0033(02)00030-x. [DOI] [PubMed] [Google Scholar]
- 5.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 6.Passias PG, Bortz CA, Segreto FA, Horn SR, Lafage R, Lafage V, et al. Development of a Modified Cervical Deformity Frailty Index: A Streamlined Clinical Tool for Preoperative Risk Stratification. Spine (Phila Pa 1976) 2019;44:169–76. doi: 10.1097/BRS.0000000000002778. [DOI] [PubMed] [Google Scholar]
- 7.Vernon H, Mior S. The Neck Disability Index: A study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–15. [PubMed] [Google Scholar]
- 8.Smith JS, Line B, Bess S, Shaffrey CI, Kim HJ, Mundis G, et al. The health impact of adult cervical deformity in patients presenting for surgical treatment: Comparison to United States Population Norms and Chronic Disease States Based on the EuroQuol-5 Dimensions Questionnaire. Neurosurgery. 2017;80:716–25. doi: 10.1093/neuros/nyx028. [DOI] [PubMed] [Google Scholar]
- 9.Tetreault L, Kopjar B, Nouri A, Arnold P, Barbagallo G, Bartels R, et al. The modified Japanese Orthopaedic Association scale: Establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J. 2017;26:78–84. doi: 10.1007/s00586-016-4660-8. [DOI] [PubMed] [Google Scholar]
- 10.Champain S, Benchikh K, Nogier A, Mazel C, Guise JD, Skalli W. Validation of new clinical quantitative analysis software applicable in spine orthopaedic studies. Eur Spine J. 2006;15:982–91. doi: 10.1007/s00586-005-0927-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rillardon L, Levassor N, Guigui P, Wodecki P, Cardinne L, Templier A, et al. Validation of a tool to measure pelvic and spinal parameters of sagittal balance. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:218–27. [PubMed] [Google Scholar]
- 12.O'Brien MF, Kuklo TR, Blanke KM, Lenke LG. Spinal Deformity Study Group Radiographic Measurement Manual. 2005. [Last accessed on 2015 May 14]. Available from: http://www.oref.org/docs/default-source/default-document-library/sdsg-radiographic-measuremnt-manual-pdf?sfvrsn=2 .
- 13.Lafage R, Challier V, Liabaud B, Vira S, Ferrero E, Diebo BG, et al. Natural head posture in the setting of sagittal spinal deformity: Validation of chin-brow vertical angle, slope of line of sight, and McGregor's slope with health-related quality of life. Neurosurgery. 2016;79:108–15. doi: 10.1227/NEU.0000000000001193. [DOI] [PubMed] [Google Scholar]
- 14.Mizutani J, Verma K, Endo K, Ishii K, Abumi K, Yagi M, et al. Global spinal alignment in cervical kyphotic deformity: The importance of head position and thoracolumbar alignment in the compensatory mechanism. Neurosurgery. 2018;82:686–94. doi: 10.1093/neuros/nyx288. [DOI] [PubMed] [Google Scholar]
- 15.Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: A ten-year follow-up. Spine (Phila Pa 1976) 2001;26:2463–6. doi: 10.1097/00007632-200111150-00013. [DOI] [PubMed] [Google Scholar]
- 16.Miura T, Panjabi MM, Cripton PA. A method to simulate in vivo cervical spine kinematics using in vitro compressive preload. Spine (Phila Pa 1976) 2002;27:43–8. doi: 10.1097/00007632-200201010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Harrison DE, Harrison DD, Janik TJ, William Jones E, Cailliet R, Normand M. Comparison of axial and flexural stresses in lordosis and three buckled configurations of the cervical spine. Clin Biomech (Bristol, Avon) 2001;16:276–84. doi: 10.1016/s0268-0033(01)00006-7. [DOI] [PubMed] [Google Scholar]
- 18.Roussouly P, Nnadi C. Sagittal plane deformity: An overview of interpretation and management. Eur Spine J. 2010;19:1824–36. doi: 10.1007/s00586-010-1476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bari TJ, Hallager DW, Tøndevold N, Karbo T, Hansen LV, Dahl B, et al. Moderate interrater and substantial intrarater reproducibility of the roussouly classification system in patients with adult spinal deformity. Spine Deform. 2019;7:312–8. doi: 10.1016/j.jspd.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Laouissat F, Scemama C, Delécrin J. Does the type of sagittal spinal shape influence the clinical results of lumbar disc arthroplasty? Orthop Traumatol Surg Res. 2016;102:765–8. doi: 10.1016/j.otsr.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Ames CP, Smith JS, Eastlack R, Blaskiewicz DJ, Shaffrey CI, Schwab F, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine. 2015;23:673–83. doi: 10.3171/2014.12.SPINE14780. [DOI] [PubMed] [Google Scholar]
- 22.Passias PG, Jalai CM, Lafage V, Lafage R, Protopsaltis T, Ramchandran S, et al. Primary drivers of adult cervical deformity: prevalence, variations in presentation, and effect of surgical treatment strategies on early postoperative alignment. Neurosurgery. 2018;83:651–9. doi: 10.1093/neuros/nyx438. [DOI] [PubMed] [Google Scholar]
- 23.Kim HJ, Nemani V, Boachie-Adjei O, Cunningham ME, Iorio JA, O'Neill K, et al. Distal fusion level selection in Scheuermann's kyphosis: A comparison of lordotic disc segment versus the sagittal stable vertebrae. Glob Spine J. 2017;7:254–9. doi: 10.1177/2192568217699183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schroeder GD, Kepler CK, Kurd MF, Mead L, Millhouse PW, Kumar P, et al. Is it necessary to extend a multilevel posterior cervical decompression and fusion to the upper thoracic spine? Spine (Phila Pa 1976) 2016;41:1845–9. doi: 10.1097/BRS.0000000000001864. [DOI] [PubMed] [Google Scholar]
- 25.Choi SJ, Suk KS, Yang JH, Kim HS, Lee HM, Moon SH, et al. What is a right distal fusion level for prevention of sagittal imbalance in multilevel posterior cervical spine surgery: C7 or T1? Clin Spine Surg. 2018;31:441–5. doi: 10.1097/BSD.0000000000000725. [DOI] [PubMed] [Google Scholar]


