Abstract
Introduction
Disturbed sleep represents a potentially important modifiable risk factor for the development of depression in children and youth. This protocol for a systematic review proposes to investigate whether insomnia and/or sleep disturbances predict child and youth depression in community and clinical-based samples.
Methods and analysis
The protocol adheres to the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols guidelines. English-written, longitudinal studies that quantitatively estimated the prediction of depression by insomnia and/or sleep disturbances in individuals 5–24 years of age will be included. EMBASE, MEDLINE, PsychINFO, Scopus and Web of Science and grey literature will be searched from 1980 to the present. For the selection of studies, two reviewers will be involved. Data extraction will be conducted by one author and checked independently by a second author. Risk of bias will be appraised using the Research Triangle Institute Item Bank tool. Heterogeneity will be measured using the I2 statistics. Meta-analysis will be carried out if ≥3 results are available and if outcome measures can be pooled. The choice between a random-effect or fixed-effect model will be based both on the I2 statistics and the participant and study characteristics of the combined studies. Results of the meta-analyses will be summarised by a forest plot. Analyses will be performed in subgroups stratified by key variables defined depending on the amount and type of information retrieved.
A narrative synthesis will be conducted in place of the meta-analysis should the pooling of data not be possible. Quality of evidence will be rated using the Grading of Recommendations Assessment, Development and Evaluation guidelines.
As this is a protocol for systematic review and meta-analysis of published data, ethics review and approval are not required. The findings will be published in a peer-reviewed journal and disseminated at scientific conferences and in patient advocacy organisations.
PROSPERO registration number
CRD42019136729.
Keywords: sleep medicine, depression & mood disorders, child & adolescent psychiatry, longitudinal studies, systematic review
Strengths and limitations of this study.
This is a protocol for a systematic review and meta-analysis of existing prospective, longitudinal evidence on insomnia and/or sleep disturbances predicting depression in children and youth.
This protocol will adhere to the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols guidelines
This protocol is registered at PROSPERO, the international prospective register of systematic reviews.
Full-text screening and extraction will be performed by two reviewers. Any uncertainty regarding selection will be resolved by consensus and, if necessary, by a third reviewer.
With regards to limitations, the review will not include treatment studies and will include only English-written articles. We include individuals aged 5–24 years, therefore excluding studies on child and youth disturbed sleep predicting depression at later stages of life.
Introduction
A recent epidemiological study analysing data from the 2016 National Survey of Children’s Health reports prevalence estimates of depression of 1.7% and 6.1% in 6–11 and 12–17 years of age ranges, respectively.1 The incidence of depression peaks at 20 years of age2 with disrupting effects on normative developmental trajectories. Prevalence is equal for both sexes prior to puberty, then it is higher in women.3 Treatment shows limited efficacy,4–6 suggesting that prevention may be a more effective resource to reduce the incidence of depression.
Targeting modifiable risk factors of illnesses is becoming a relevant therapeutic strategy for disease prevention.7 Among modifiable risk factors predicting child and youth depression, insomnia is increasingly recognised as an important component of the complex and multifactorial causal pathway of depression.8
Treating insomnia to specifically reduce the incidence and/or severity of depression has been the focus of controlled, high-quality, randomised treatment studies in depressed or at risk for depression adult or elderly individuals.9 10 In a recent meta-analysis, internet-based cognitive behavioural therapy (CBT) for insomnia had a significant, small effect on comorbid depression in individuals older than 18 years.11
Similar evidence in younger individuals is scarce, mostly consists of studies with small sample size/no follow-up, and it is limited to individuals older than 12 years of age.12–18
In a randomised controlled trial, CBT for insomnia for 6 weekly sessions and a booster session after 2 months was significantly more effective in decreasing comorbid depression compared with waitlist in 12–19-year-old individuals with DSM-V (Diagnostic Statistical Manual) insomnia and no comorbid psychiatric disorders. The effect was large, was maintained after 12 months and was fully mediated by the reduction of insomnia symptoms.17
In a longitudinal, randomised controlled trial study (SENSE, ie, Sleep and Education: learning New Skills Early), the preventative effect on the incidence of depression at risk for depression, 12–17-year-old adolescents with sleeping difficulties are investigated.13 The interventions consist of 7 weekly sessions of either a CBT/mindfulness-based sleep intervention or an active control intervention, followed by two booster sessions after 3 and 6 months postintervention. One-hundred and twenty-three participants have completed the interventions,14 15 however, findings regarding the main outcomes of the study (preventative effects of depression) from the 2-year follow-up are not available yet.
It is currently not known whether treating sleep problems in depressed or at risk for depression children (eg, children with a history of abuse, with high emotional dysregulation, offspring of depressed parents) would lead to a reduction or lower incidence of depression, respectively, than it would be if sleep problems were not treated.19 To understand whether earlier prevention efforts could be more effective, a precise quantitative estimate of the prediction of depression by insomnia in the entire developmental population, including depressed and non-depressed individuals, is needed.
Insomnia consists of clinically significant long sleep-onset latency and/or awakening after sleep onset and/or early morning awakening, accompanied by diurnal tiredness and functional impairment. Prevalence of insomnia is 19.5% in children, equally distributed among boys and girls; in youth, prevalence is 17.4%, and higher among girls.20
Six systematic reviews have summarised cohort studies on insomnia predicting depression.21–25 Pooled estimates are consistent across reviews ranging from 2.10 (95% CI 1.86 to 2.38)26 to 2.83 (95% CI 1.55 to 5.17),24 and across subgroups stratified by the most common confounders, for example, sex (male: 1.46 (95% CI 1.13 to 1.88)25; female: 1.96 (95% CI 1.05 to 3.66)),25 type of ascertainment (sample drawn from a special population: 2.05 (95% CI 1.53 to 2.74)25; sample representative of a community or population: 2.34 (95% CI 1.85 to 2.96))25 and age (individuals of age ≥60 years: from 1.87 (95% CI 1.47 to 2.37)25 to 1.92 (95% CI 1.61 to 2.30)23; individuals younger than 60 years of age: 2.50 (95% CI 1.96 to 3.20)).25
However, only three of the six systematic reviews included participants younger than 18 years,22 25 26 and a pooled estimate, that is, OR=2.0 (95% CI 1.5 to 2.7), was provided by only one of the three reviews.26 This estimate was based on three studies up to 2010 and included 7404 participants, whose age ranged between 6 and 16 years.27–29 In all three studies, depression was defined according to DSM-IV and insomnia to DSM-IV-TR criteria. The test for heterogeneity for this group did not show a significant index (Q-value=0.3; df(Q)=2; p=0.9 and I2=0.0). Li et al25 updated and used the same selection criteria of Baglioni et al26 and although 15 new cohort studies were added, no new studies on children and youth were included. Finally, Pigeon et al22 summarised studies published from 2014 to 2017; four studies on children and youth were included, of which three supported insomnia predicting depression30–32 and one found no such association.33 All three systematic reviews of this age group excluded studies that did not control for baseline depression. This led to a greatly reduced number of studies. While the rationale of this choice is clear for studies of risk and prediction, it might not have been the ideal choice, due to the overall paucity of studies in the child and youth age range compared with other age groups. Including studies that did not control for baseline depression would allow testing of whether there are significant differences in the meta-analytic estimates between studies controlling versus not controlling for this variable. If no differences are found, studies not controlling for baseline depression could contribute to the pooled data with an overall increase in the precision for the estimate of the meta-analytic effects.
There is also some evidence available on whether sleep disturbances other than insomnia predict child and youth depression.34–43 This may include increased/short/disrupted sleep duration with/without diurnal sleepiness, sleepwalking/talking, nightmares, bedwetting, breathing-related sleep disorders and/or circadian disturbances. Furthermore, sleep disturbances more broadly defined may include challenges either generically defined with regards to duration and consistency over time, measured by self-reported questionnaires, interview or by EEG/actigraph-based measures, and scored by either single-item or cumulative scores. A recent meta-analysis summarised studies testing the association of broadly defined sleep disturbances on depression in 12–20-year-old already clinically depressed participants. In all selected studies,44–50 sleep was defined by EEG-based, objective measures. Estimates of the meta-analytic effects identified that EEG-based longer sleep-onset latency, more wake after sleep onset and lower sleep efficiency, were significant predictors of depression compared with typical sleep (effect sizes ranging 0.43–0.58).51 Although findings from this review are of crucial importance for potential secondary prevention programmes in depressed youth, it would be useful to have summarised data on the longitudinal association of broadly defined sleep disturbances with depression on the entire developmental population, including non-clinical individuals as well as a broader age range, which would allow to apply findings to primary prevention and/or early intervention programmes.
Finally, insomnia and/or sleep disturbances are often associated to comorbid psychiatric and medical conditions.19 Most previous knowledge synthesis studies have excluded comorbidities, limiting the generalisability and transferability of findings. For this reason, in this systematic review, studies focusing on both primary and comorbid insomnia and/or sleep disturbances will be included. To understand the extent to which insomnia and/or sleep disturbances have a distinct risk to depression across comorbid disorders, subgroup analyses will be performed.
Understanding whether insomnia and/or sleep disturbances significantly increases the risk of depression in children and youth could lead to variation in clinical practice and inform policy development. Preventive strategies could include treating sleep problems starting as early as childhood. This is particularly important in light of evidence on the differential effectiveness of a number of treatment for sleep problems (eg, melatonin,52 53 CBT,54 physical exercise55 and bright light therapy56 and the fact that sleep problems in children are underdiagnosed57 and rarely treated.58
The purpose of this protocol is to outline methods for a systematic review and meta-analysis of data from prospective, longitudinal studies of children and youth ascertained from clinical or community-based samples investigating the role of insomnia and/or sleep disturbances compared with typical sleep as predictors of depression. ‘Do children and youth with insomnia and/or sleep disturbance have higher rates of later depression than children and youth without insomnia and/or sleep disturbance’?
We are interested in testing this relationship in the context of both the absence and presence of baseline depression, that is, whether insomnia and/or sleep disturbance predict both new and relapse/worsening of depression, respectively.
Our study will add to the currently available knowledge synthesis in that:
It will provide an updated meta-analytic estimate of the effects of insomnia predicting child and youth depression, adding studies from 2010 onwards compared with Baglioni et al.26
By including studies on 5–24-year-old participants from both clinical and non-clinical populations, it will provide a more comprehensive and updated meta-analytic estimate compared with Lovato and Gradisar.51
It will include studies on participants with/without baseline depression and whether or not controlling for baseline depression.
It will include studies of both primary and comorbid insomnia and/or sleep disturbances.
As a secondary aim, we will test whether insomnia and/or sleep disturbance predict new-onset and/or worsening/relapse of depression, by testing the pooled estimate in two subgroups of studies, respectively, those including participants with baseline depression or where baseline depression has been controlled for and studies including participants without baseline depression or where baseline depression has not been controlled for.
Finally, we aim to explore the sources of potential heterogeneity and examine the robustness of the primary hypothesis against key confounding variables. Specifically, we will address whether the prediction of child and youth depression by insomnia and/or sleep disturbances significantly differ between studies stratified by key variables, for example, risk of bias score, type of ascertainment, type of sleep disturbance, measurement of outcome, presence of baseline comorbidity, sample size, age group, gender. Subgroups will be defined depending on the amount and type of information retrieved.
Methods
For the protocol, we will follow the guidelines outlined in ‘Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P)’.59 For the final report, we will follow the guidelines set in ‘Meta-analysis Of Observational Studies in Epidemiology: a proposal for reporting’.60
Patient and public involvement
No patient involved.
Inclusion criteria
Study types
This study will include (1) English-written and (2) prospective, longitudinal observational studies that quantitatively estimated the prediction of depression by insomnia and/or sleep disturbances in children and youth. Only those studies reporting OR, relative risk, HR, regression coefficients or correlation coefficients with their respective measurements of error and p values will be selected. Grey literature including relevant dissertations/PhD theses and key conference publications will be included. Case series, case reports, systematic reviews, meta-analyses as well as experimental, retrospective, cross-sectional, treatment, theoretical and position studies will be excluded.
Population type
Mean age to determine eligibility for inclusion of the study is between 5 and 24 years. This age range was chosen to cover the whole age range of risk for depression in childhood and youth and to include the period of peak incidence for depression.1 2 In our review, we identify three categories: ‘childhood’ between 5 and 9 years of age, ‘adolescence’ between 10 and 19 years of age and ‘young adulthood’ between 20 and 24 years of age.61 For simplicity, the term ‘youth’ refers to individuals whose age is between 10 and 24 years. Studies focusing on participants belonging to either community or clinical-based samples with any comorbid psychiatric/neurological/medical diagnosis will be included.
Exposure
Studies will be included if focusing on either one of the following two exposures:
Insomnia, defined as clinically significant difficulty in initiating or maintaining sleep or non-restorative sleep, as based on DSM-III and later versions. Although the criterion of daytime impairment is required to define clinically significant insomnia, it has been shown that pooled estimates of insomnia predicting depression when this criterion is taken into account24 are of comparable magnitude relative to the ones obtained when this criterion is not considered.25 26 Therefore, to allow for inclusion of the highest number of studies, daytime impairment will be free to vary.
Sleep disturbances, defined as patterns of quality and sleep duration which deviate from expected age-related norms, that is, increased/short/fragmented sleep duration with or without daytime fatigue/sleepiness, nightmares/terror attacks, circadian disturbances and/or night walking/talking. Sleep disturbances can be generically defined with regards to duration and consistency over time and can be based on subjective and/or EEG/actigraph-based, objective measures. Measures can be based on single or multiple items or a cumulative score of various items. To increase the generalisability of the results, narcolepsy, breathing-related sleep disorders, central sleep apnoea, non-rapid/rapid eye movement sleep disorder, restless legs syndrome, substance/medication-induced sleep disorder and enuresis nocturna primaria may also be included.
Exposures’ assessment can be administered by a clinician, a researcher or based on self-report, parent-report and/or teacher-report questionnaires.
Outcome
Studies will be included if they focus on either one of the following outcomes: major depressive disorder, depressive disorder not otherwise specified, dysthymic disorder and/or dimensional constructs of depression, that is, defined by scores from single-item or multiple-item questionnaires, internalising disorders or anxious depression. Studies focusing on anxiety without a measure of depression will not be included. Studies including participants with bipolar disorders will be excluded given that sleep problems’ prevalence differs significantly in bipolar versus unipolar disorders.47 62 Outcome is measured by standardised and validated tools administered by a clinician, researcher and/or based on self-report, parent-report and/or teacher-report questionnaires.
To be included, both exposure and outcome have to be measured at mean age ≥5 years and ≤24, and the time between the exposure and outcome is ≥1 month. To address the research question on the role of insomnia and/or sleep disturbances as predictor of depression, only studies reporting on the exposure measured at least 1 month before the outcome will be included. When multiple assessments are conducted on the same cohort, each pair where both exposures and outcomes are measured at mean age ≤24 and ≥5 years and exposures are measured before the outcome will be considered.
Confounders
Studies will be included regardless of whether they contain estimates adjusted for common confounding factors such as sex, socioeconomic status, demographics, type of comorbidity at baseline. Studies that do not control for common confounding factors will be highlighted for potentially confounded results.
Identification of eligible studies and data extraction
Search strategy
The following databases will be searched: EMBASE, MEDLINE, PsychINFO, Scopus and Web of Science. A draft of the Medline search strategy will be developed using a combination of MeSH and keywords terms relating to sleep disorders, depression/depressive disorder and children/adolescents/young adults with the help of a research librarian. The search will be limited to the years 1980 (to focus on current diagnostic terminology from the DSM-III) to the present and will also be limited to observational studies using the search filter developed by the Scottish Intercollegiate Guidelines Network. The draft Medline search will also be piloted to ensure the sensitivity and efficacy of the final search strategy and will also be reviewed by all of the participating authors (figure 1). The finalised Medline search will be adapted for each bibliographic database individually.
Figure 1.
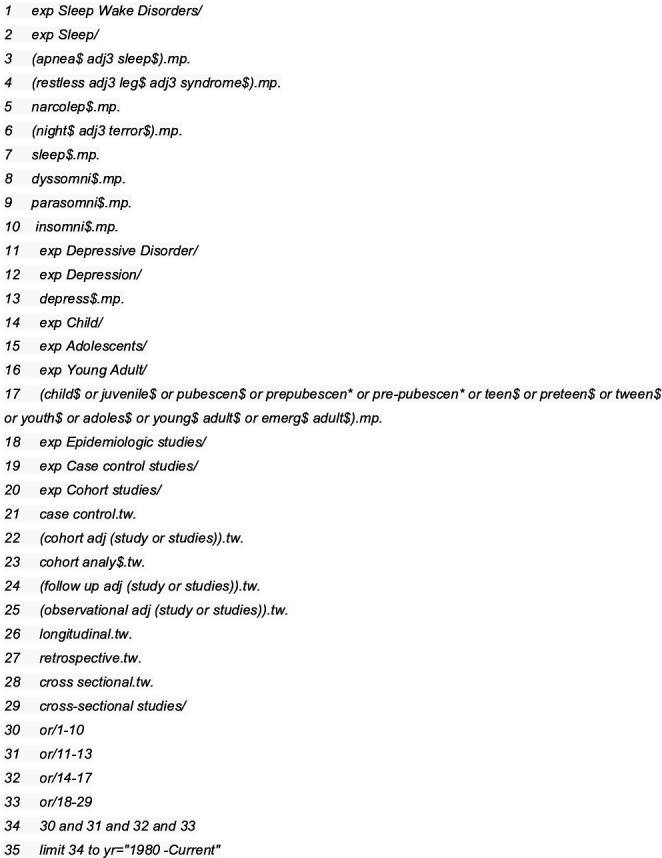
Database: Ovid MEDLINE: Epub ahead of print, in-process and other non-indexed citations, Ovid MEDLINE daily and Ovid MEDLINE<1946–present>search strategy.
Grey literature, that is, dissertations and conference proceeding/papers, will be included in the search in order to mitigate against publication bias.63 Dissertations have been noted as providing a valuable methodology and clinical source of information.64 Additionally, searching for relevant conference proceedings/papers is recommended in order to identify recent, but unpublished research.65
The grey literature will be screened for relevant material, including use of the search checklist Grey Matters: ‘A Practical Search Tool for Evidence-Based Medicine’ from the Canadian Agency for Drugs and Technologies in Health, and by also searching other sources to identify relevant dissertations/PhD theses and conference publications, that is, Proquest Dissertations and Theses, ProceedingsFirst, PapersFirst, Conference Abstracts from Embase, Google Scholar Search. The references of selected articles will also be hand-searched for eligible studies and all the searches will be rerun just before the final analyses to identify additional relevant studies. Experts in the field will be contacted to locate potentially eligible studies and/or unpublished data.
Selection of studies
Search results will be exported into Covidence, merged and checked for duplicates. For the selection of studies, two students will be involved, with minimum an undergraduate level of education in a health-related field and previous experience with the systematic review methodology. They will be given the systematic review protocol and 5-hour training on the content of the systematic review and basic knowledge of the procedure. For the selection of studies based on title and abstract screening, eligible studies will be selected by two reviewers until a kappa score of 0.8 is achieved with the remainder being selected by one reviewer. Full-text papers will be obtained for all references thought potentially eligible by a single reviewer based on title and abstract; all full-text papers will be reviewed by two independent reviewers, with disagreements referred to a third, senior-author reviewer. The PRISMA search flowchart will be used to report the number of studies included and excluded at each step in the process, along with the rationale for the exclusion.
Data extraction
Data extraction will be conducted by one author and checked independently by a second author using a predefined data extraction form. Extracted variables will pertain to the following domains: general study information, study characteristics (ie, year of publication, type of sample ascertainment, sample size), participant characteristics (ie, age at baseline, age at follow-up, number of follow-up, interval between baseline and each follow-up, exposure and outcome definition and diagnostic tool, covariates that were adjusted in the analyses). Outcome data will include OR, relative risk, HR, regression coefficients or correlation coefficients with their respective measurements of error and p values. Information on the sources of funding for each study will be retrieved. Discrepancies between the two authors will be resolved by discussion with a third, senior-author reviewer. When relevant data are missing, corresponding authors will be contacted to obtain the information.
Risk of bias assessment
Risk of bias of included studies’ results will be appraised using the Research Triangle Institute Item Bank (RTI-IB) tool. The RTI-IB is a practical, quality-scoring tool for observational studies with a focus on bias and precision.66 It has a high inter-rater reliability (75%) and consists of 29 items tapping 12 domains (1) background, (2) sample definition and selection, (3) interventions/exposure, (4) outcomes, (5) creation of treatment groups, (6) blinding, (7) soundness of information, (8) follow-up, (9) analysis comparability, (10) analysis outcome, (11) interpretation and (12) presentation and reporting. Possible response categories to each item are ‘yes’, ‘no’, ‘partially’, ‘cannot determine’ and ‘not applicable’. The quality appraisal will be performed by two authors independently with discrepancies being resolved by discussion with a third, senior-author reviewer. Results will be reported narratively and summarised in a descriptive table. Items will be subdivided into six categories: selection bias/confounding, performance bias, attrition bias, detection bias, reporting bias and information bias. Items are scored as high, low or unclear risk of bias. If at least one item in a category is scored as high, the risk of bias within this category is scored as moderate risk. If at least 50% of the items in a category are scored as high, the risk of the category is scored as high. Each study will receive a summary score that corresponds to the highest score obtained in any category.66
Description of primary studies and data analysis
Data will be synthesised by a table reporting study type, participant characteristics, exposure and outcome measures and a second table on the risk of bias assessment. Studies will be combined based on similarities across relevant characteristics, for example, type of sample ascertainment, age at baseline, duration of follow-up, exposure and outcome definition and diagnostic tool and meta-analysis will be performed if ≥3 studies are available. Heterogeneity of pooled estimates will be measured using the I2 statistics, which represents the percentage of variation attributable to between-study heterogeneity. I2 values of 25%, 50% and 75% will be considered as low, medium and high heterogeneity, respectively.67 For the meta-analysis, the choice between a random-effect or fixed-effect model will be based both on the I2 statistics and the participant and study characteristics of the combined studies. Results of the meta-analyses will be summarised by a forest plot. Meta-analysis and test of heterogeneity will be performed using Stata V.14 (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, Texas, USA: StataCorp LP). A narrative synthesis will be conducted in place of the meta-analysis and this latter cannot be performed. To test the robustness of the primary hypothesis against study-level characteristics, for example, risk-of-bias score, sample size, year of publication, duration of follow-up, exposure and outcome definition and diagnostic tool, sensitivity analyses will be performed by excluding those studies with the characteristics that can potentially be a source of heterogeneity, for example, excluding studies with a high risk-of-bias score. Likewise, a sensitivity analysis will be performed by removing studies focusing on medically based sleep disorders, that is, narcolepsy, breathing-related sleep disorders, central sleep apnoea, non-rapid/rapid eye movement sleep disorder, restless legs syndrome, substance/medication-induced sleep disorder and enuresis nocturna primaria, to prevent the possibility that the pooled estimates could be impacted by factors related to the chronicity of these conditions.
Subgroup analyses will be performed related to relevant participant-level characteristics, for example, baseline comorbidity, age at baseline, gender, by calculating pooled estimates in subgroups of studies, for example, studies of children versus adolescents versus young adults, and/or taking different estimates from the same study related to the subgroups of interest, for example, men versus women. Subgroups will be defined depending on the amount and type of information retrieved.
To assess sensitivity of the pooled estimate to each included study, we will apply the leave-one-out method, which consists of repeating the analysis removing one study at a time.68 Potential publication bias and other sources of bias will be further assessed by visual inspection of the symmetry of funnel plots. Quality of evidence will be rated using the Grading of Recommendations Assessment, Development and Evaluation guidelines taking into account risk of bias, applying the RTI-IB tool; heterogeneity; directness, evaluating the relevance of the sample, the outcomes and the exposure; precision, examining the 95% CI and publication bias of the included studies. We will assess inter-rater agreement between investigators for study inclusion, data extraction and methodological quality assessment using kappa Cohen’s coefficient.
Discussion
This systematic review and meta-analysis will synthesise and quantify the existing evidence on insomnia and/or sleep disturbances predicting depression in children and youth.
Understanding the magnitude of the risk of sleep problems predicting later depression in children and youth will contribute significantly to the development of treatment and secondary prevention strategies of depression.5 6 69 Sleep is often impaired in child and youth depression.70 Treating sleep problems in childhood can become an adjunctive tool not only to treat more effectively childhood depression but also to change the risk trajectories of depression, reducing the incidence and severity of depressive episodes later in life.
This study will also potentially inform strategies for primary prevention of depression in healthy children and youth. Sleep patterns physiologically change from birth to early adulthood as a consequence of a number of maturational changes in the brain, and as a result of an adjustment to the social environment.71 72 The most evident change concerns the duration of sleep, which decreases from approximately 14 hours at 6 months of age to 8 hours at 16 years of age.73 74 Another relevant maturational change concerns the sleep-onset time, which delays up to approximately 2 hours when transitioning to adolescence.75 This process is typical of puberty, and it is part of the phase delay of a host of circadian rhythms related to gonadal hormones’ changes.75 The delay in sleep-onset time, called evening chronotype, manifests at a younger age in women than men, corresponding to the sex difference in the onset of puberty.72 75 Evidence shows that over the last century, child and youth sleep has consistently reduced beyond normative maturational changes.76 77 It has been claimed that this ‘epidemic’ shortage of sleep might be related to the concomitant occurrence of the evening chronotype and earlier morning wake-up time of youth compared with younger children.78 Other studies claim that decreased sleep in children and youth may instead be due to the increase in electronic screen media use during late hours.79 As a result, an increasing proportion of otherwise healthy children and youth is exposed to insufficient sleep. An open question is whether this newly occurring, sleep-deprived child and youth cohort is at risk of depression. Understanding if the same risk pathway identified in affected or at-risk for depression individuals exists also in typically developing children and youth is essential to understand the size and potential consequences of the secular trend towards insufficient sleep and to eventually plan effective programmes of primary prevention to reduce the incidence of depression.
Ethics and dissemination
As this is a protocol for systematic review and meta-analysis of published data, ethics review and approval are not required. The findings will be published in a peer-reviewed journal and disseminated at scientific conferences.
Supplementary Material
Footnotes
Twitter: @m_aitken
Contributors: CM, BA, MA and PS conceived the idea, planned and designed the study protocol. CM wrote the first draft. SB provided expertise to the search strategy. WW provided expertise to the data extraction and statistical analysis. JDH provided critical insights. All authors have approved and contributed to the final written manuscript. CM: guarantor of the review.
Funding: The authors acknowledge the support of the Cundill Centre for Child and Youth Depression at the Centre for Addiction and Mental Health (CAMH). The views and opinions expressed in this article are those of the authors and do not necessarily reflect those of CAMH. Funder’s roles consist of evaluating and funding the grant application if suitable, monitoring and evaluating research outputs, facilitating the implementation of findings in healthcare, the interaction between researchers and research users, and the dissemination research findings. Since our project was donor funded, there is no award/grant number.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr 2019;206:256–67. 10.1016/j.jpeds.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avenevoli S, Swendsen J, He J-P, et al. Major depression in the National comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 2015;54:37–44. 10.1016/j.jaac.2014.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park RJ, Goodyer IM. Clinical guidelines for depressive disorders in childhood and adolescence. Eur Child Adolesc Psychiatry 2000;9:0147–61. 10.1007/s007870070038 [DOI] [PubMed] [Google Scholar]
- 4.Cipriani A, Zhou X, Del Giovane C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet 2016;388:881–90. 10.1016/S0140-6736(16)30385-3 [DOI] [PubMed] [Google Scholar]
- 5.Eckshtain D, Kuppens S, Ugueto A, et al. Meta-Analysis: 13-year follow-up of psychotherapy effects on youth depression. J Am Acad Child Adolesc Psychiatry 2020;59:45–63. 10.1016/j.jaac.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 6.Weisz JR, Kuppens S, Ng MY, et al. Are psychotherapies for young people growing stronger? tracking trends over time for youth anxiety, depression, attention-deficit/hyperactivity disorder, and conduct problems. Perspect Psychol Sci 2019;14:216–37. 10.1177/1745691618805436 [DOI] [PubMed] [Google Scholar]
- 7.Gapstur SM, Drope JM, Jacobs EJ, et al. A blueprint for the primary prevention of cancer: targeting established, modifiable risk factors. CA Cancer J Clin 2018;68:446–70. 10.3322/caac.21496 [DOI] [PubMed] [Google Scholar]
- 8.Cairns KE, Yap MBH, Pilkington PD, et al. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J Affect Disord 2014;169:61–75. 10.1016/j.jad.2014.08.006 [DOI] [PubMed] [Google Scholar]
- 9.Christensen H, Batterham PJ, Gosling JA, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight study): a randomised controlled trial. Lancet Psychiatry 2016;3:333–41. 10.1016/S2215-0366(15)00536-2 [DOI] [PubMed] [Google Scholar]
- 10.Freeman D, Sheaves B, Goodwin GM, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry 2017;4:749–58. 10.1016/S2215-0366(17)30328-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye Y-Y, Zhang Y-F, Chen J, et al. Internet-Based cognitive behavioral therapy for insomnia (ICBT-i) improves comorbid anxiety and Depression-A meta-analysis of randomized controlled trials. PLoS One 2015;10:e0142258. 10.1371/journal.pone.0142258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Werner-Seidler A, Wong Q, Johnston L, et al. Pilot evaluation of the sleep Ninja: a smartphone application for adolescent insomnia symptoms. BMJ Open 2019;9:e026502. 10.1136/bmjopen-2018-026502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waloszek JM, Schwartz O, Simmons JG, et al. The sense study (sleep and education: learning new skills early): a community cognitive-behavioural therapy and mindfulness-based sleep intervention to prevent depression and improve cardiac health in adolescence. BMC Psychol 2015;3:39. 10.1186/s40359-015-0096-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blake M, Waloszek JM, Schwartz O, et al. The sense study: post intervention effects of a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep improvement intervention among at-risk adolescents. J Consult Clin Psychol 2016;84:1039–51. 10.1037/ccp0000142 [DOI] [PubMed] [Google Scholar]
- 15.Blake M, Schwartz O, Waloszek JM, et al. The sense study: treatment mechanisms of a cognitive behavioral and Mindfulness-Based group sleep improvement intervention for at-risk adolescents. Sleep 2017;40:zsx061. 10.1093/sleep/zsx061 [DOI] [PubMed] [Google Scholar]
- 16.Kirschbaum-Lesch I, Gest S, Legenbauer T, et al. Feasibility and efficacy of bright light therapy in depressed adolescent inpatients. Z Kinder Jugendpsychiatr Psychother 2018;46:423–9. 10.1024/1422-4917/a000603 [DOI] [PubMed] [Google Scholar]
- 17.de Bruin EJ, Bögels SM, Oort FJ, et al. Improvements of adolescent psychopathology after insomnia treatment: results from a randomized controlled trial over 1 year. J Child Psychol Psychiatry 2018;59:509–22. 10.1111/jcpp.12834 [DOI] [PubMed] [Google Scholar]
- 18.Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. J Child Psychol Psychiatry 2014;55:273–83. 10.1111/jcpp.12157 [DOI] [PubMed] [Google Scholar]
- 19.Fang H, Tu S, Sheng J, et al. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med 2019;23:2324–32. 10.1111/jcmm.14170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barclay NL, Gehrman PR, Gregory AM, et al. The heritability of insomnia progression during childhood/adolescence: results from a longitudinal twin study. Sleep 2015;38:109–18. 10.5665/sleep.4334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry 2003;160:1147–56. 10.1176/appi.ajp.160.6.1147 [DOI] [PubMed] [Google Scholar]
- 22.Pigeon WR, Bishop TM, Krueger KM. Insomnia as a precipitating factor in new onset mental illness: a systematic review of recent findings. Curr Psychiatry Rep 2017;19:44. 10.1007/s11920-017-0802-x [DOI] [PubMed] [Google Scholar]
- 23.Bao Y-P, Han Y, Ma J, et al. Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: meta-analysis and systematic review. Neurosci Biobehav Rev 2017;75:257–73. 10.1016/j.neubiorev.2017.01.032 [DOI] [PubMed] [Google Scholar]
- 24.Hertenstein E, Feige B, Gmeiner T, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev 2019;43:96–105. 10.1016/j.smrv.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 25.Li L, Wu C, Gan Y, et al. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry 2016;16:375. 10.1186/s12888-016-1075-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011;135:10–19. 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 27.Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res 2002;53:561–9. 10.1016/S0022-3999(02)00446-4 [DOI] [PubMed] [Google Scholar]
- 28.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep 2008;31:1351–6. [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson EO, Chilcoat HD, Breslau N. Trouble sleeping and anxiety/depression in childhood. Psychiatry Res 2000;94:93–102. 10.1016/S0165-1781(00)00145-1 [DOI] [PubMed] [Google Scholar]
- 30.Alvaro PK, Roberts RM, Harris JK, et al. The direction of the relationship between symptoms of insomnia and psychiatric disorders in adolescents. J Affect Disord 2017;207:167–74. 10.1016/j.jad.2016.08.032 [DOI] [PubMed] [Google Scholar]
- 31.Ritter PS, Höfler M, Wittchen H-U, et al. Disturbed sleep as risk factor for the subsequent onset of bipolar disorder--Data from a 10-year prospective-longitudinal study among adolescents and young adults. J Psychiatr Res 2015;68:76–82. 10.1016/j.jpsychires.2015.06.005 [DOI] [PubMed] [Google Scholar]
- 32.Hayley AC, Skogen JC, Sivertsen B, et al. Symptoms of depression and difficulty initiating sleep from early adolescence to early adulthood: a longitudinal study. Sleep 2015;38:1599–606. 10.5665/sleep.5056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Armstrong JM, Ruttle PL, Klein MH, et al. Associations of child insomnia, sleep movement, and their persistence with mental health symptoms in childhood and adolescence. Sleep 2014;37:901–9. 10.5665/sleep.3656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Armitage R, Hoffmann RF, Emslie GJ, et al. Sleep microarchitecture as a predictor of recurrence in children and adolescents with depression. Int J Neuropsychopharmacol 2002;5:217–28. 10.1017/S1461145702002948 [DOI] [PubMed] [Google Scholar]
- 35.Gregory AM, O'Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry 2002;41:964–71. 10.1097/00004583-200208000-00015 [DOI] [PubMed] [Google Scholar]
- 36.Fredriksen K, Rhodes J, Reddy R, et al. Sleepless in Chicago: tracking the effects of adolescent sleep loss during the middle school years. Child Dev 2004;75:84–95. 10.1111/j.1467-8624.2004.00655.x [DOI] [PubMed] [Google Scholar]
- 37.Gregory AM, Caspi A, Eley TC, et al. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol 2005;33:157–63. 10.1007/s10802-005-1824-0 [DOI] [PubMed] [Google Scholar]
- 38.Gregory AM, Van der Ende J, Willis TA, et al. Parent-reported sleep problems during development and self-reported anxiety/depression, attention problems, and aggressive behavior later in life. Arch Pediatr Adolesc Med 2008;162:330–5. 10.1001/archpedi.162.4.330 [DOI] [PubMed] [Google Scholar]
- 39.Gregory AM, Rijsdijk FV, Lau JYF, et al. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep 2009;32:189–99. 10.1093/sleep/32.2.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Touchette E, Chollet A, Galéra C, et al. Prior sleep problems predict internalising problems later in life. J Affect Disord 2012;143:166–71. 10.1016/j.jad.2012.05.049 [DOI] [PubMed] [Google Scholar]
- 41.Greene G, Gregory AM, Fone D, et al. Childhood sleeping difficulties and depression in adulthood: the 1970 British cohort study. J Sleep Res 2015;24:19–23. 10.1111/jsr.12200 [DOI] [PubMed] [Google Scholar]
- 42.Wang B, Eastwood PR, Becker A, et al. Concurrent developmental course of sleep problems and emotional/behavioral problems in childhood and adolescence as reflected by the dysregulation profile. Sleep 2019;42:zsy243. 10.1093/sleep/zsy243 [DOI] [PubMed] [Google Scholar]
- 43.Wang B, Isensee C, Becker A, et al. Developmental trajectories of sleep problems from childhood to adolescence both predict and are predicted by emotional and behavioral problems. Front Psychol 2016;7:7. 10.3389/fpsyg.2016.01874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCracken JT, Poland RE, Lutchmansingh P, et al. Sleep electroencephalographic abnormalities in adolescent depressives: effects of scopolamine. Biol Psychiatry 1997;42:577–84. 10.1016/S0006-3223(96)00431-3 [DOI] [PubMed] [Google Scholar]
- 45.Rao U, McCracken JT, Lutchmansingh P, et al. Electroencephalographic sleep and urinary free cortisol in adolescent depression: a preliminary report of changes from episode to recovery. Biol Psychiatry 1997;41:369–73. 10.1016/S0006-3223(96)00430-1 [DOI] [PubMed] [Google Scholar]
- 46.Rao U, Dahl RE, Ryan ND, et al. The relationship between longitudinal clinical course and sleep and cortisol changes in adolescent depression. Biol Psychiatry 1996;40:474–84. 10.1016/0006-3223(95)00481-5 [DOI] [PubMed] [Google Scholar]
- 47.Rao U, Dahl RE, Ryan ND, et al. Heterogeneity in EEG sleep findings in adolescent depression: unipolar versus bipolar clinical course. J Affect Disord 2002;70:273–80. 10.1016/S0165-0327(01)00396-2 [DOI] [PubMed] [Google Scholar]
- 48.Rao U, Poland RE. Electroencephalographic sleep and hypothalamic-pituitary-adrenal changes from episode to recovery in depressed adolescents. J Child Adolesc Psychopharmacol 2008;18:607–13. 10.1089/cap.2008.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shain BN, Naylor M, Shipley JE, et al. Imipramine effects on sleep in depressed adolescents: a preliminary report. Biol Psychiatry 1990;28:459–62. 10.1016/0006-3223(90)90414-W [DOI] [PubMed] [Google Scholar]
- 50.Goetz RR, Wolk SI, Coplan JD, et al. Premorbid polysomnographic signs in depressed adolescents: a reanalysis of EEG sleep after longitudinal follow-up in adulthood. Biol Psychiatry 2001;49:930–42. 10.1016/S0006-3223(00)01092-1 [DOI] [PubMed] [Google Scholar]
- 51.Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev 2014;18:521–9. 10.1016/j.smrv.2014.03.006 [DOI] [PubMed] [Google Scholar]
- 52.Zisapel N. Paediatric use of melatonin: Letter to the Editor regarding the manuscript "Current role of melatonin in pediatric neurology:Clinical recommendations" by Bruni, et al.. Eur J Paediatr Neurol 2015;19:122–33. [DOI] [PubMed] [Google Scholar]
- 53.Bruni O, Alonso-Alconada D, Besag F, et al. Current role of melatonin in pediatric neurology: clinical recommendations. Eur J Paediatr Neurol 2015;19:122–33. 10.1016/j.ejpn.2014.12.007 [DOI] [PubMed] [Google Scholar]
- 54.Ma Z-R, Shi L-J, Deng M-H. Efficacy of cognitive behavioral therapy in children and adolescents with insomnia: a systematic review and meta-analysis. Braz J Med Biol Res 2018;51:e7070. 10.1590/1414-431x20187070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kalak N, Gerber M, Kirov R, et al. Daily morning running for 3 weeks improved sleep and psychological functioning in healthy adolescents compared with controls. J Adolesc Health 2012;51:615–22. 10.1016/j.jadohealth.2012.02.020 [DOI] [PubMed] [Google Scholar]
- 56.van Maanen A, Meijer AM, Smits MG, et al. Effects of melatonin and bright light treatment in childhood chronic sleep onset insomnia with late melatonin onset: a randomized controlled study. Sleep 2017;40:zsw038. 10.1093/sleep/zsw038 [DOI] [PubMed] [Google Scholar]
- 57.Meltzer LJ, Johnson C, Crosette J, et al. Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics 2010;125:e1410–8. 10.1542/peds.2009-2725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Meltzer LJ, Plaufcan MR, Thomas JH, et al. Sleep problems and sleep disorders in pediatric primary care: treatment recommendations, persistence, and health care utilization. J Clin Sleep Med 2014;10:421–6. 10.5664/jcsm.3620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stroup DF, Berlin JA, Morton SC, et al. Meta-Analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (moose) group. JAMA 2000;283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 61.Bundy DAP, de Silva N, Horton S, et al. Investment in child and adolescent health and development: key messages from disease control priorities, 3rd edition. Lancet 2018;391:687–99. 10.1016/S0140-6736(17)32417-0 [DOI] [PubMed] [Google Scholar]
- 62.Lai Y-C, Huang M-C, Chen H-C, et al. Familiality and clinical outcomes of sleep disturbances in major depressive and bipolar disorders. J Psychosom Res 2014;76:61–7. 10.1016/j.jpsychores.2013.10.020 [DOI] [PubMed] [Google Scholar]
- 63.Paez A. Gray literature: an important resource in systematic reviews. J Evid Based Med 2017;10:233–40. 10.1111/jebm.12266 [DOI] [PubMed] [Google Scholar]
- 64.McLeod BD, Weisz JR. Using dissertations to examine potential bias in child and adolescent clinical trials. J Consult Clin Psychol 2004;72:235–51. 10.1037/0022-006X.72.2.235 [DOI] [PubMed] [Google Scholar]
- 65.Scherer RW, Langenberg P, von Elm E. Full publication of results initially presented in Abstracts. Cochrane Database Syst Rev 2007;2:MR000005. [DOI] [PubMed] [Google Scholar]
- 66.Viswanathan M, Berkman ND. Development of the RTI item bank on risk of bias and precision of observational studies. J Clin Epidemiol 2012;65:163–78. 10.1016/j.jclinepi.2011.05.008 [DOI] [PubMed] [Google Scholar]
- 67.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 68.Patsopoulos NA, Evangelou E, Ioannidis JPA. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol 2008;37:1148–57. 10.1093/ije/dyn065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev 2012;16:129–36. 10.1016/j.smrv.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 70.Rao U, Chen L-A. Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues Clin Neurosci 2009;11:45–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Galland BC, Taylor BJ, Elder DE, et al. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev 2012;16:213–22. 10.1016/j.smrv.2011.06.001 [DOI] [PubMed] [Google Scholar]
- 72.Tarokh L, Saletin JM, Carskadon MA. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev 2016;70:182–8. 10.1016/j.neubiorev.2016.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jenni OG, Molinari L, Caflisch JA, et al. Sleep duration from ages 1 to 10 years: variability and stability in comparison with growth. Pediatrics 2007;120:e769–76. 10.1542/peds.2006-3300 [DOI] [PubMed] [Google Scholar]
- 74.Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 2003;111:302–7. 10.1542/peds.111.2.302 [DOI] [PubMed] [Google Scholar]
- 75.Hummer DL, Lee TM. Daily timing of the adolescent sleep phase: insights from a cross-species comparison. Neurosci Biobehav Rev 2016;70:171–81. 10.1016/j.neubiorev.2016.07.023 [DOI] [PubMed] [Google Scholar]
- 76.Matricciani L, Olds T, Petkov J. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev 2012;16:203–11. 10.1016/j.smrv.2011.03.005 [DOI] [PubMed] [Google Scholar]
- 77.Keyes KM, Maslowsky J, Hamilton A, et al. The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. Pediatrics 2015;135:460–8. 10.1542/peds.2014-2707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Adolescent sleep working G, Committee on a, Council on school H. school start times for adolescents. Pediatrics 2014;134:642–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open 2019;9:e023191. 10.1136/bmjopen-2018-023191 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


