Abstract
Objectives
To identify reported (1) common biomechanical asymmetries in the literature after anterior cruciate ligament (ACL) reconstruction in adolescents during landing and (2) timescales for asymmetry to persist postsurgery.
Data Sources
We identified sources by searching the CINAHL, PubMed, Scopus, and SPORTDiscus electronic databases using the following search terms: asymmetry OR symmetry AND landing AND biomechanics OR kinematics OR kinetics.
Study Selection
We screened the titles and abstracts of 85 articles using our inclusion criteria. A total of 13 articles were selected for further analysis.
Data Extraction
Three reviewers independently assessed the methodologic quality of each study. We extracted the effect sizes directly from studies or calculated them for biomechanical variables assessing asymmetry between limbs of participants with ACL reconstruction. We conducted meta-analyses on variables that were assessed in multiple studies for both double- and single-limb landings.
Data Synthesis
Asymmetry was more commonly identified in kinetic than kinematic variables. Anterior cruciate ligament reconstruction appeared to have a large effect on asymmetry between limbs for peak vertical ground reaction force, peak knee-extension moment, and loading rate during double-limb landings, as well as mean knee-extension moment and knee energy absorption during both double- and single-limb landings.
Conclusions
Our findings suggested that return-to-sport criteria after ACL reconstruction should incorporate analysis of the asymmetry in loading experienced by each limb rather than movement patterns alone.
Keywords: anterior cruciate ligament injury, landing, biomechanics
Key Points
Asymmetries between surgical and nonsurgical limbs were more frequently identified in kinetic than in kinematic variables.
The most common asymmetries were peak knee-extension moment and peak vertical ground reaction force during double-limb landing; both values were frequently lower in the surgical than in the nonsurgical limb.
In most cases, lower limb kinematics did not display asymmetry between limbs.
Anterior cruciate ligament reconstruction appeared to have a large effect on asymmetry in peak vertical ground reaction force, peak knee-extension moment, and loading rate during double-limb landing and mean knee-extension moment and knee energy absorption during both double- and single-limb landings.
Return-to-sport criteria after anterior cruciate ligament reconstruction should include analysis of the asymmetry in loading experienced by each limb rather than the movement patterns alone.
Anterior cruciate ligament (ACL) injury most often occurs during noncontact situations (72% of cases),1,2 such as landing, side stepping or cutting, and change of direction, in which no direct blow to the knee occurs at the time of injury. After ACL injury, surgery to reconstruct the ruptured ACL is the most frequent option for patients, with 90% of patients electing to proceed.3 Most ACL reconstructions (ACLRs) are performed in the adolescent population.4,5 After ACLR, adolescent athletes typically aim to return to competitive sport participation. This requires extensive rehabilitation, with the overarching goal of returning the surgical limb to a similar level of function (ie, range of motion, strength, and coordination) as existed before the injury.6–8 However, preexisting levels of function are usually unknown, so the goal instead becomes returning the surgical limb to symmetric function with the nonsurgical limb,6 which is subsequently used by a health care professional as a marker for the athlete's clearance to return to sport.6,9–11
Despite considerable efforts to improve surgical procedures and rehabilitation practices after ACLR, secondary ACL injury is common in athletes who return to sport.9,12–15 Between 6% and 29% of patients who undergo ACLR either injure the graft of the surgical limb or sustain an ACL injury to the contralateral limb.9,12–15 This risk of subsequent ACL injury after reconstruction is highest among adolescent patients.15–18 Shelbourne et al16 reported that the prevalence of rupture to either the contralateral or reconstructed ACL within 5 years of ACLR was 9.6% (4.3% for the reconstructed ACL, 5.3% for the contralateral knee) for the general population (N = 1415). This, however, rose to 17.4% (8.7% for both the ACL-reconstructed and contralateral knees) in patients aged <18 years compared with 6.7% in patients aged 18 to 25 years and 3.9% in patients >25 years.16 Furthermore, Shelbourne et al16 noted that most secondary ACL injuries occurred during sport participation, with the majority sustained during basketball (52%) or soccer (15%) compared with only 6.6% (9 of 136 secondary ACL injuries) sustained during nonsport-related activities.
The reasons for the high prevalence of secondary injury after ACLR are likely deficiencies in the strength of the muscles controlling knee movement, as well as altered movement and loading patterns when performing athletic activities, such as landing, squatting, and cutting.9 Asymmetry in landing mechanics after ACLR has been proposed as a major risk factor for both primary19 and secondary ACL injury.9 Investigators8–11,20–24 observed that after ACLR, athletes who exhibited less asymmetry of lower limb biomechanics during sporting activities had a reduced risk of sustaining a second ACL injury. However, one of the main challenges for health care professionals treating patients with ACLR is how to identify asymmetry between limbs and, therefore, properly clear an athlete to return to sport. Some researchers7,25 have attempted to develop clinical assessment criteria to appropriately define return to sport after ACLR. These criteria typically include consideration of time since surgery; knee-joint stability; symmetry between surgical and nonsurgical limbs in postural control, strength, power, endurance, agility, and hop distance; and qualitative movement analysis during sporting tasks.25 Yet most of these criteria rely on subjective measures and only indirectly assess knee function and loading. For example, a measure of hopping distance provides little information about the lower limb movement and loading patterns that have been identified as risk factors for secondary injury during dynamic movements.9,22,26 This suggests that the current methods used to clear the athlete to return to play after ACLR may not adequately determine mechanical symmetry between limbs. Consequently, many athletes will likely return to competition prematurely, before their reconstructed knee has regained full function in terms of range of motion, strength, and muscle-activity patterns.
Most researchers who examined asymmetries after ACLR have focused on adult populations.26,27 In a recent systematic review and meta-analysis, Lepley and Kuenze28 evaluated hip and knee biomechanics after ACLR during double- and single-limb landing tasks. Patients who underwent ACLR demonstrated a reduced knee-extension moment and reduced ground reaction force (GRF) on the surgical side compared with the nonsurgical side, which suggested potential unloading of the surgical limb. In our study, we aimed to build on the work of Lepley and Kuenze28 by focusing on adolescent athletes because of their increased risk of secondary ACL injury and by including more variables in the analysis, specifically ankle biomechanics. During adolescence, the body undergoes considerable change in structure and maturation of motor coordination and control.29,30 These changes result in altered landing mechanics.4,5 Given the large number of ACLRs performed during adolescence, asymmetry in lower limb mechanics is likely to have a more profound effect on young athletes wanting to return to sport participation after ACLR. Therefore, the purpose of our systematic review and meta-analysis was to identify reported (1) common biomechanical asymmetries in the literature after ACLR in adolescents during landing movements and (2) timescales for asymmetry to persist postsurgery.
METHODS
Literature Search Strategy
We identified relevant sources by searching the following electronic databases from their inceptions to January 2019: CINAHL (1961), PubMed (1966), Scopus (2004), and SPORTDiscus (1930). The following search terms were used: asymmetry OR symmetry AND landing AND biomechanics OR kinematics OR kinetics. We excluded articles not written in English, reviews, meta-analyses, nonpeer-reviewed sources, and abstracts unaccompanied by full-text journal articles, which left 164 articles.
Study Selection
We downloaded the article data, including authors, title, abstract, and journal, into RefWorks (ProQuest, Ann Arbor, MI) citation management software; duplicate citations were deleted. This reduced the number of articles to 85. Next, we reviewed article titles and abstracts to apply our inclusion criteria: human adolescents (mean age >11 and <18 years) who had ACLR and ≥1 kinetic or kinematic measure of asymmetry that compared the surgical and nonsurgical limbs. Kinetic variables included GRF, joint moments (turning effects produced by forces acting around joints), and energy absorption (amount of work performed at a joint, calculated from the joint moment multiplied by the change in joint angle). Kinematic variables included joint angles and angular velocities. Lastly, the task performed was required to be either a double-limb (bilateral) or single-limb (unilateral) landing maneuver. Two independent reviewers (G.H., S.C.) assessed all articles, and any disagreements were resolved through oral discussion after all articles had been reviewed.
After the inclusion criteria were applied, 12 papers remained. We inspected the reference lists of each paper and identified 1 more study, bringing the total to 13. The literature search and study-selection procedures are outlined in Figure 1.
Figure 1.

Flow diagram of literature search strategy.
Data Extraction and Analysis
We extracted the following information from each article: study design, aim, participants (mean age, sex, sporting background, time post-ACLR), task, measure of asymmetry used, and key findings. Three reviewers (G.H., P.M., S.C.) independently assessed each study's methodologic quality using 14 relevant criteria from the Downs and Black31 revised checklist. This checklist was chosen because it is a valid and reliable tool for assessing the methodologic quality of randomized and nonrandomized studies in health care.31 A study that was scored ≤8 was considered to be low quality; 9 to 10, moderate quality; and ≥11, high quality.28,32 We again resolved disagreements through a consensus meeting. The means and standard deviations of each variable that assessed asymmetry were extracted. We then either extracted effect sizes directly from the studies or calculated them by dividing the mean difference between groups by the pooled standard deviation.33 Given that previous authors34 have shown different asymmetries in lower limb biomechanics between single- and double-limb landing tasks, the data were stratified based on landing task. We interpreted Cohen d effect sizes as trivial (<0.2), small (<0.21–0.5), moderate (0.51–0.79), or large (>0.8).33 For 1 study,9 we estimated effect sizes based on the data presented in figures, and for another study,35 we were unable to calculate effect sizes based on the statistical information provided. We conducted meta-analyses on variables that were assessed multiple times (at least 2 measurements of a particular variable) using the metafor package in R software (Vienna, Austria).36
RESULTS
Study Quality
Of the studies assessed, 523,37–41 were scored as high quality, 735,39,42–46 were scored as moderate quality, and only 19 was scored as low quality (Supplemental Table, available online at http://dx.doi.org/10.4085/1062-6050-244-19.S1). The average score was 10.2 out of 14, suggesting moderate quality overall. All criteria were met by the 12 investigations; however, only 1 group37 specifically stated that all participants were recruited during the same time period, and only 1 group23 determined sample size by conducting an a priori power analysis.
Participants
A total of 180 males and 330 females participated in the 13 studies. All authors tested both male and female patients with ACLR. The average sample sizes for patients with ACLR were 13.8 ± 6.0 for males and 25.5 ± 12.1 for females. The smallest number of participants tested who had undergone ACLR was 15,39 and the largest number was 68.37 The mean age across all participants was 16.4 ± 0.8 years. All participants intended to return to competitive sports at a level similar to their preinjury level.
Time After ACLR
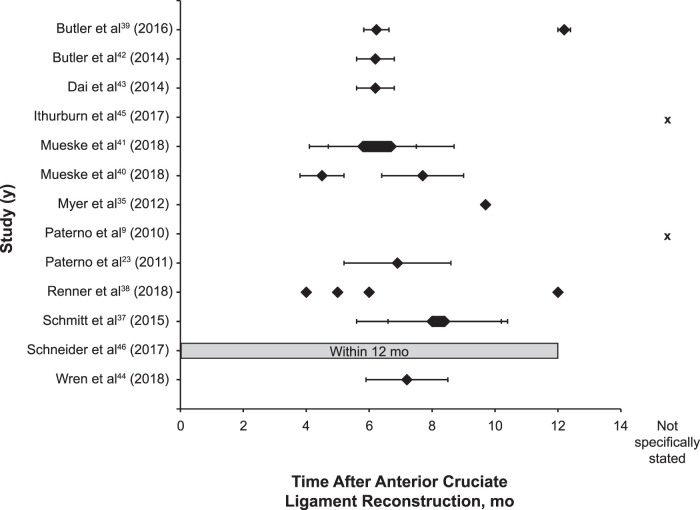
Participants were tested at approximately 4,38 5,38,40 6,38,39,41–43 7,23,44 8,37,40 10,35 and 1238,39 months after ACLR. Ithurburn et al45 reported the time from being cleared to return to sport rather than the time from ACLR (4 weeks after being cleared to return to sport and 2 years later). Schneider et al46 simply stated that testing took place within 1 year after ACLR, and Paterno et al9 did not clearly specify the time after ACLR (Figure 2).
Figure 2.
Time after anterior cruciate ligament (ACL) reconstruction when participants were tested in each study. Diamonds indicate mean time after ACL reconstruction, with error bars indicating standard deviations where reported. A hexagon indicates the range of times after ACL reconstruction was reported for multiple subgroups within that study.
Landing Task
The landing task differed among studies, with some using single-legged vertical jump landing (participants were instructed to jump as high possible on 1 limb and land under control),35,44 single-legged vertical drop landing (participants dropped from a 31-cm box and were instructed to maintain a controlled landing in single-limb stance),45,46 double-legged vertical drop jump (participants dropped off a 31- or 40-cm box, landed on both feet, and immediately jumped straight up as high as possible),9,23,37,40,41 and a vertical stop jump (participants ran forward, took off on 1 foot, landed on 2 feet, and took off again from 2 feet).38,39,42,43
Outcome Measures
Most researchers examined asymmetries only in the sagittal plane; only 3 groups40,41,44 assessed variables in all 3 planes of motion. Kinematic and kinetic joint variables were evaluated 58 times in the sagittal plane (28 kinematic and 30 kinetic analyses) compared with only 14 times in the frontal plane and 6 times in the transverse plane. Differences between surgical and nonsurgical limbs were commonly observed in the sagittal plane: 32% (9/28 included data points) of the time differences for kinematics and 70% (21/30 included data points) for kinetics. Few kinematic variables differed between the surgical and nonsurgical limbs in the frontal and transverse planes (only 1 difference among 13 variables measured), but for kinetic measures in the frontal and transverse planes, 6 differences were demonstrated for only 7 variables measured (5 frontal plane, 2 transverse plane; Tables 1 and 2).
Table 1.
Summary of the Kinematic Variables Measured to Assess Biomechanical Asymmetry in Each Studya
| Variable |
Study (Year) |
Summary Effect Size |
||||||||||||||
| Butler et al39 (2016) |
Butler et al42 (2014) |
Dai et al43 (2014) |
Ithurburn et al45 (2017) |
Mueske et al41 (2018) |
Mueske et al40 (2018) |
Myer et al35 (2012) |
Paterno et al9 (2010) |
Paterno et al23 (2011) |
Renner et al38 (2018) |
Schmitt et al37 (2015) |
Schneider et al46 (2017) |
Wren et al44 (2018) |
Double Limb |
Single Limb |
Combined |
|
| Limb landing type | Double | Double | Double | Single | Double | Double | Single | Double | Double | Double | Double | Single | Single | |||
| Study quality scoreb | 10 | 10 | 10 | 10 | 11 | 11 | 10 | 6 | 12 | 11 | 12 | 9 | 10 | |||
| Limb symmetry index calculatedc | X | X | X | X | X | X | X | |||||||||
| Sagittal-plane kinematics | ||||||||||||||||
| Hip-flexion angle at initial contact | d | d | ||||||||||||||
| Hip range of motion | d | |||||||||||||||
| Peak hip-flexion angle | 0.08, 0.09e | d | d | 0.18, 0.60f | 0.14 | −0.20 | −0.05 | |||||||||
| Knee-flexion angle at initial contact | d | d | d | 0.04 | −0.16 | −0.08 | ||||||||||
| Knee range of motion | d | d | ||||||||||||||
| Peak knee-flexion angle | d | d | 0.6–1.7f | d | 0.04–2.07f | d | 0.28, 0.79f | −0.66g | −0.51g | −0.64g | ||||||
| Peak knee-flexion angular velocity | d | |||||||||||||||
| Knee-flexion angular velocity at initial contact | d | |||||||||||||||
| Knee-flexion angle at peak angular velocity | d | |||||||||||||||
| Ankle plantar-flexion angle at initial contact | 0.25, 0.3f | 0.14, 1.19e | ||||||||||||||
| Peak ankle-dorsiflexion angle | d | 0.6–1.6f | 0.53, 0.40f | d | −0.58g | −0.23 | −0.48g | |||||||||
| Frontal-plane kinematics | ||||||||||||||||
| Hip-flexion angle at initial contact | d | |||||||||||||||
| Peak hip-flexion angle | 0.54, 0.47e | |||||||||||||||
| Mean hip-flexion angle | d | d | ||||||||||||||
| Knee-flexion angle at initial contact | d | |||||||||||||||
| Knee range of motion | d | |||||||||||||||
| Peak knee-flexion angle | d | |||||||||||||||
| Mean knee-flexion angle | d | d | ||||||||||||||
| Transverse-plane kinematics | ||||||||||||||||
| Hip-flexion angle at initial contact | d | |||||||||||||||
| Peak hip-flexion angle | d | |||||||||||||||
| Mean hip-flexion angle | d | d | ||||||||||||||
Where differences were reported, effect sizes are given (1 value if 1 group tested, 2 values if 2 groups tested, and range of values if ≥3 groups tested).
Out of 14 points (≤8 = low, 9–10 = moderate, ≥11 = high).
Calculated as (involved limb/uninvolved limb) × 100.
Variable was measured, but no difference was reported between the surgical and nonsurgical limbs.
Greater in the surgical limb.
Less in the surgical limb.
Significant effect.
Table 2.
Summary of the Kinetic Variables Measured to Assess Biomechanical Asymmetry in Each Studya
| Variable |
Study (Year) |
Summary Effect Size |
||||||||||||||
| Butler et al39 (2016) |
Butler et al42 (2014) |
Dai et al43 (2014) |
Ithurburn et al45 (2017) |
Mueske et al41 (2018) |
Mueske et al40 (2018) |
Myer et al35 (2012) |
Paterno et al9 (2010) |
Paterno et al23 (2011) |
Renner et al38 (2018) |
Schmitt et al37 (2015) |
Schneider et al46 (2017) |
Wren et al44 (2018) |
Double Limb |
Single Limb |
Combined |
|
| Limb landing type | Double | Double | Double | Single | Double | Double | Single | Double | Double | Double | Double | Single | Single | |||
| Study quality scoreb | 10 | 10 | 10 | 10 | 11 | 11 | 10 | 6 | 12 | 11 | 12 | 9 | 10 | |||
| Limb symmetry index calculatedc | X | X | X | X | X | X | X | |||||||||
| Sagittal-plane kinetics | ||||||||||||||||
| Peak hip moment | d | |||||||||||||||
| Mean hip moment | d | d | d | 0.18 | 0.05 | 0.12 | ||||||||||
| Hip energy absorption | d | d | d | −0.05 | −0.15 | −0.06 | ||||||||||
| Peak knee-extension moment | 1.46, 1.03f | 1.33f | 1.23f | d | 1.00, 0.60f | 3.82–9.44f | 0.44, 1.18f | −2.86g | −2.86g | |||||||
| Mean knee-extension moment | 1.32f | 0.8–2.3f | 0.71, 1.15 f | −1.63g | −0.90g | −1.38g | ||||||||||
| Knee-extension moment at peak angular velocity | 1.00f | |||||||||||||||
| Knee-extension moment at initial contact | 1.05f,g | |||||||||||||||
| Knee-energy absorption | 1.31f | 1.0–2.0f | 1.46, 0.80f | 0.75, 1.27f | −1.38g | −0.99g | −1.27g | |||||||||
| Peak ankle moment | 0.55, 0.33f | |||||||||||||||
| Mean ankle moment | 0.8–1.3f | 1.00, 1.00f | 0.00, 0.88e | −1.00g | 0.43 | −0.58 | ||||||||||
| Ankle-energy absorption | 0.9–1.6f | 1.18, 0.39f | d | −1.04g | 0.17 | −0.67g | ||||||||||
| Frontal-plane kinetics | ||||||||||||||||
| Mean hip moment | 0.6–0.9e | 0.55, 0.39e | ||||||||||||||
| Mean knee moment | 0.5–1.1e | 0.45, 0.57e | 0.55, 0.49f | −0.68g | −0.53g | −0.61g | ||||||||||
| Transverse-plane kinetics | ||||||||||||||||
| Mean hip moment | 0.6e | d | ||||||||||||||
| Ground reaction force | ||||||||||||||||
| Peak vertical | 0.9, 0.57f | 0.72f | 0.79f | 0.7–1.5f | 1.33, 1.00f | f | 0.98f | 2.44–5.51f | 0.28, 1.70f | d | −1.67g | −0.06 | −1.50g | |||
| Peak posterior | 0.47f | 1.94–3.64f | ||||||||||||||
| Loading rate | 0.51f | 1.04–4.58f | 0.31–1.06f | −2.08g | −2.08g | |||||||||||
| Vertical impulse | d | 3.09–6.62f | ||||||||||||||
| Anteroposterior impulse | d | |||||||||||||||
| Peak vertical stiffness | 1.25–3.25f | 0.32f | ||||||||||||||
Where differences were reported, effect sizes are given (1 value if 1 group was tested, 2 values if 2 groups were tested, and range of values if ≥3 groups were tested).
Out of 14 points (≤8 = low, 9–10 = moderate, ≥11 = high).
Calculated as (involved limb/uninvolved limb) × 100.
Variable was measured, but no difference was reported between the surgical and nonsurgical limbs.
Greater in the surgical limb.
Less in the surgical limb.
Significant effect.
With respect to which lower limb joints were assessed for asymmetries, 5 studies38–41,44 examined the knee and at least 1 other joint (hip or ankle), 5 studies9,37,42,43,45 examined only the knee joint, 2 studies23,35 examined only GRF, and 1 study46 examined only leg stiffness.
Most investigators included both kinematic and kinetic measures of asymmetry, with 5 studies9,23,35,43,46 examining only kinetic variables. No authors examined purely kinematic measures of asymmetry. Differences between the surgical and nonsurgical limbs were more frequently observed in kinetic variables than in kinematic variables, whereby 76% (44/58 included data points) of the time, a between-limbs difference was present for kinetic variables compared with only 24% (10/41 included data points) for kinematic variables.
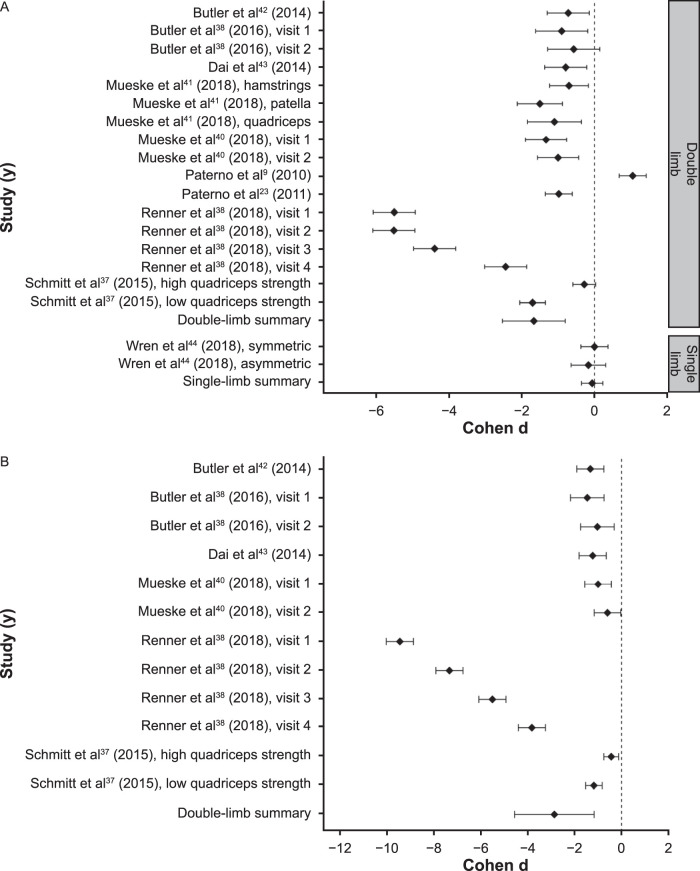
The most commonly measured variable was peak vertical GRF, which was assessed in 1023,35,37–44 of the 13 studies. This variable was also most often different between limbs, with 9 studies23,35,37–43 showing reduced vertical GRF for the surgical limb compared with the nonsurgical limb. The only researchers44 who measured peak vertical GRF and did not find a difference between limbs used a single-limb landing task. The meta-analysis indicated asymmetry between the surgical and nonsurgical limbs for peak vertical GRF with large summary effect sizes for double-limb landings (b = −1.67; 95% confidence interval [CI] = −2.53, −0.80; standard error [SE] = 0.44; z = −3.78; P < .001) but a trivial effect size for single-limb landings (b = −0.06; 95% CI = −0.36, 0.23; SE = 0.15; z = −0.42; P = .23; Figure 3A). The second most commonly measured variable to assess asymmetry was peak knee-extension moment, which was measured in 737–40,42,43,45 of the 13 studies and found to be reduced in the surgical limb compared with the nonsurgical limb in 637–40,42,43 of the 7 studies, all of which employed a double-limb landing task (Table 2). The meta-analysis indicated an asymmetry between the surgical and nonsurgical limbs for peak knee-extension moment with a large summary effect size for double-limb landings (b = −2.86; 95% CI = −4.56, −1.17; SE = 0.86; z = −3.31; P < .001; Figure 3B).
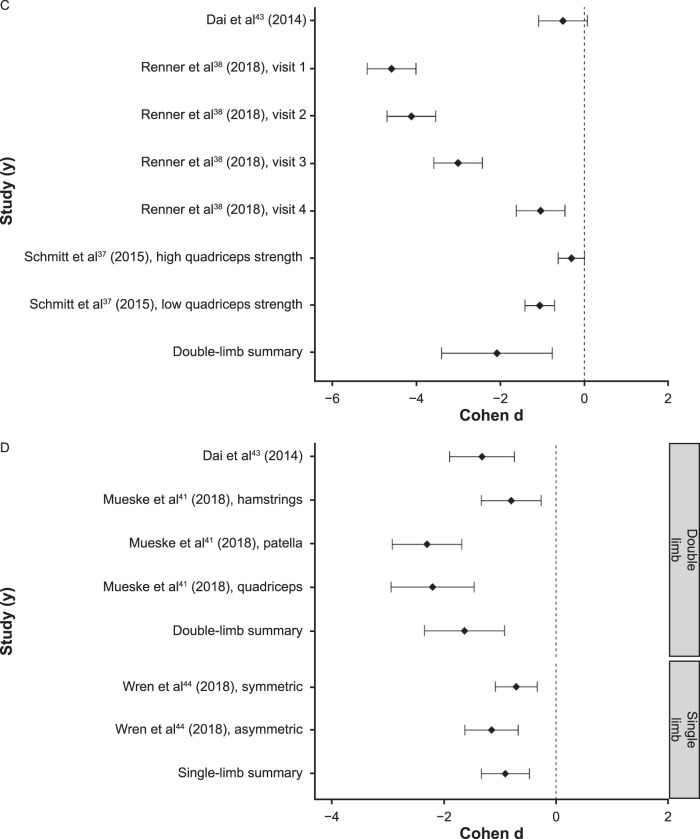
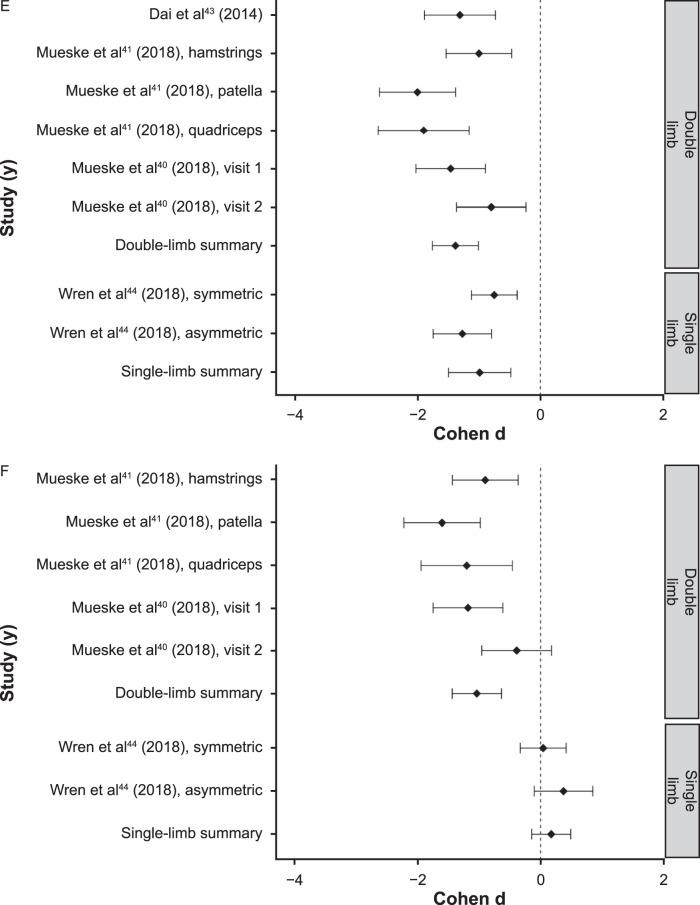
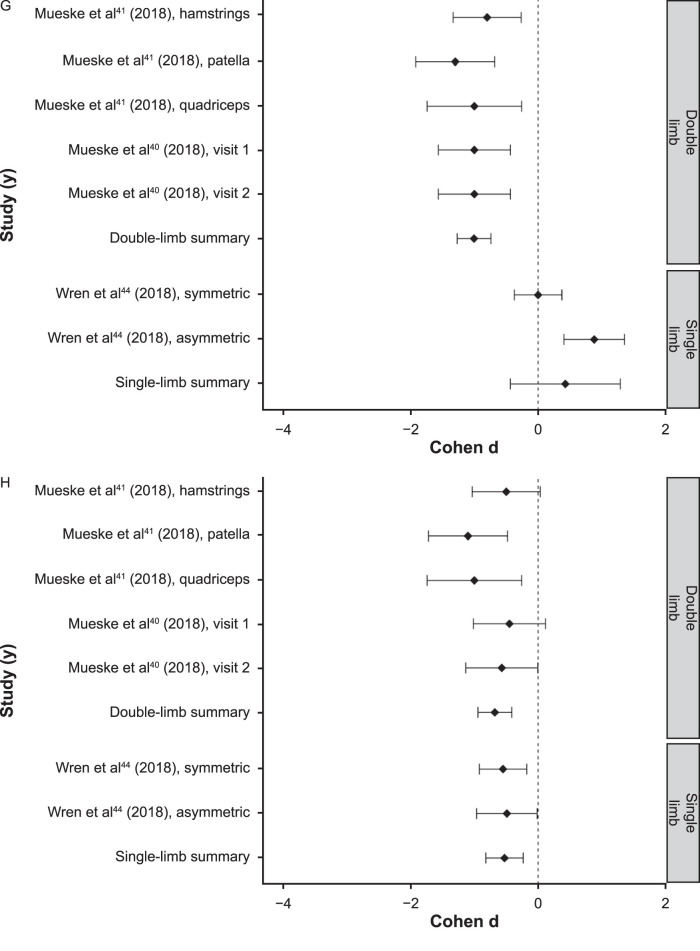
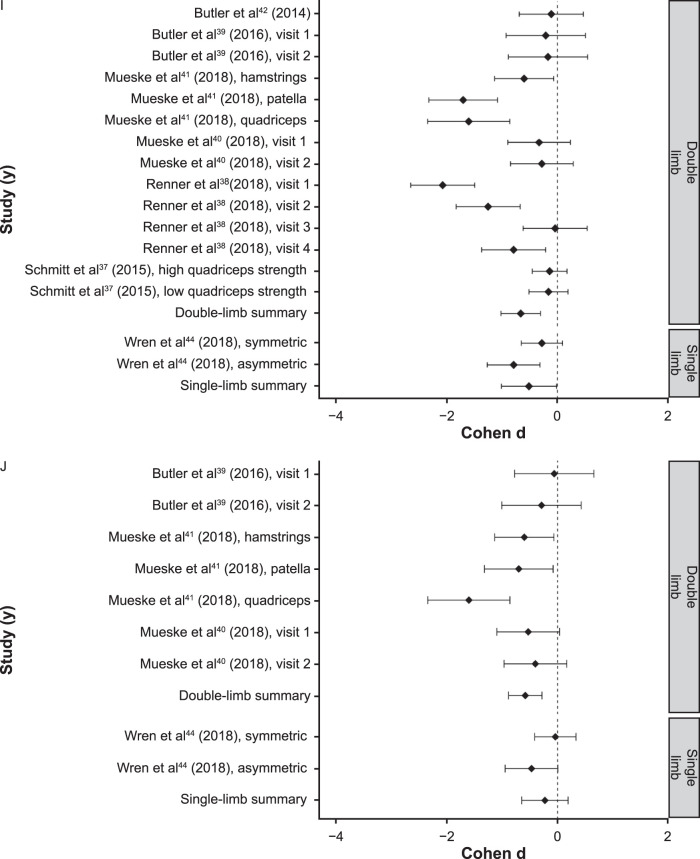
Figure 3.
Effect sizes for, A, peak vertical ground reaction force, B, peak knee-extension moment, C, loading rate, D, mean knee-extension moment, E, knee-energy absorption, F, ankle-energy absorption, G, mean ankle sagittal-plane moment, H, mean knee frontal-plane moment, I, peak knee-flexion angle, and J, peak ankle-dorsiflexion angle. Error bars represent 95% confidence intervals. Continued on next page.
Figure 3.
Continued from previous page. Continued on next page.
Figure 3.
Continued from previous page. Continued on next page.
Figure 3.
Continued from previous page. Continued on next page.
Figure 3.
Continued from previous page.
The other kinetic variables in which the meta-analyses identified asymmetry were loading rate, mean knee-extension moment, knee-energy absorption, ankle-energy absorption, mean ankle sagittal-plane moment, and mean knee frontal-plane moment. Large effect sizes were observed for loading rate during double-limb landings (b = −2.08; 95% CI = −3.39, −0.76; SE = 0.49; z = −3.58; P < .001; Figure 3C), mean knee-extension moment during double-limb (b = −1.63; 95% CI = −2.35, −0.92; SE = 0.36; z = −4.48; P < .001) and single-limb (b = −0.90; 95% CI = −1.33, −0.48; SE = 0.22; z = −4.13; P < .001) landings (Figure 3D) and knee-energy absorption during double-limb (b = −1.38; 95% CI = −1.76, −1.01; SE = 0.19; z = −7.23; P < .001) and single-limb (b = −0.99; 95% CI = −1.50, −0.48; SE = 0.26; z = −3.81; P < .001) landings (Figure 3E). Large summary effect sizes were noted during double-limb landings for ankle-energy absorption (b = −1.04; 95% CI = −1.44, −0.64; SE = 0.20; z = −5.08; P < .001 Figure 3F) and mean ankle sagittal-plane moment (b = −1.00; 95% CI = −1.27, −0.74; SE = 0.14; z = −7.42 P < .001; Figure 3G), whereas effect sizes were small or trivial and not different during single-limb landings for ankle-energy absorption (b = 0.17; 95% CI = −0.15, 0.49; SE = 0.16; z = 1.06; P = .29; Figure 3F) and mean ankle sagittal-plane moment (b = 0.43; 95% CI = −0.43, 1.29; SE = 0.44; z = 0.97; P = .33; Figure 3G). Moderate effect sizes were demonstrated for mean knee frontal-plane moment during double-limb (b = −0.68; 95% CI = −0.94, −0.41; SE = 0.14; z = −5.01; P < .001) and single-limb (b = −0.53; 95% CI = −0.82, −0.23; SE = 0.15; z = −3.52; P < .001) landings (Figure 3H).
The only kinematic variables in which the meta-analyses identified differences between the surgical and nonsurgical limbs were peak knee-flexion angle and peak ankle-dorsiflexion angle. A moderate summary effect size was observed for peak knee-flexion angle during double-limb (b = −0.66; 95% CI = −1.02, −0.30; SE = 0.18; z = −3.62; P < .001) and single-limb (b = −0.51; 95% CI = −1.01, −0.01; SE = 0.25; z = −2.02; P = .044) landings (Figure 3I) and for peak ankle-dorsiflexion angle (b = −0.58; 95% CI = −0.89, −0.28; SE = 0.15; z = −3.78; P < .001) during double-limb landings, but only a small summary effect size was detected for this variable during single-limb landings (b = −0.23; 95% CI = −0.65, 0.19; SE = 0.21; z = −1.07; P = .28; Figure 3J).
The meta-analyses indicated no asymmetry between the surgical and nonsurgical limbs for knee flexion at initial ground contact, peak hip-flexion angle, mean hip sagittal-plane moment, and hip-energy absorption during both double- and single-limb landings. Trivial summary effect sizes were present for knee-flexion angle at initial ground contact during double-limb (b = 0.04; 95% CI = −0.34, 0.42; SE = 0.19; z = 0.19; P = .85) and single-limb (b = −0.16; 95% CI = −0.45, 0.14; SE = 0.15; z = −1.05; P = .29) landings, peak hip-flexion angle during double-limb (b = 0.14; 95% CI = −0.10, 0.37; SE = 0.12; z = 1.14; P = .26) and single-limb (b = −0.20; 95% CI = −0.96, 0.57; SE = 0.39; z = −0.50; P = .62) landings, mean hip sagittal-plane moment during double-limb (b = 0.18; 95% CI = −0.08, 0.45; SE = 0.14; z = 1.36; P = .18) and single-limb (b = 0.05; 95% CI = −0.25, 0.34; SE = 0.15; z = 0.32; P = .75) landings, and hip-energy absorption during double-limb (b = −0.05; 95% CI = −0.31, 0.22; SE = 0.14; z = −0.35; P = .73) and single-limb (b = −0.15; 95% CI = −0.99, 0.70; SE = 0.43; z = −0.34; P = .73) landings.
DISCUSSION
In this systematic review and meta-analysis, we aimed to identify the common biomechanical asymmetries during landing movements reported in the literature after ACLR in adolescents. A total of 13 studies were assessed for quality, with 5 studies23,37,38,40,41 rated as high quality, 735,39,42–46 rated as moderate quality, and 19 rated as low quality (average score = 10.2/14). Sagittal-plane knee kinetics (8 studies: 4 high,37,38,40,41 3 moderate,39,42,43 and 1 low9 quality) and vertical GRF (8 studies: 5 high23,37,38–41 and 3 moderate39,42,43 quality) during double-limb landings were the most frequent variables that were both measured and shown to be asymmetric between the surgical and nonsurgical limbs. This result is supported by a recent systematic review and meta-analysis of Lepley and Kuenze,28 who also found asymmetry in these variables during landing in adults with ACLR. The close link between these factors was identified by Dai et al,43 who determined that asymmetries in GRF accurately predicted asymmetries in knee-extension moment. Anterior cruciate ligament reconstruction had a large effect on asymmetry between limbs in peak vertical GRF, peak knee-extension moment, mean knee-extension moment, knee-energy absorption, and loading rate during double-limb landing. In all cases in which asymmetries were identified for these variables, the loading of the surgical limb was less than in the nonsurgical limb. The meta-analyses more often identified asymmetries with larger effect sizes for double-limb landings than for single-limb landings. This may be partly due to the larger number of data points for double-limb landings but also suggests that during double-limb landings, athletes recovering from ACLR typically put less load on their injured limb to protect it from further injury by increasing the load on the uninjured limb. This observation is supported by Lepley and Kuenze,28 who found lower peak knee-extension moments in the surgical limb during double-limb landing but not during single-limb landing. Asymmetry in landing mechanics after ACLR has been proposed as a risk factor for secondary ACL injury9 to the surgical or nonsurgical limb, whereby increasing the load on the uninjured limb may increase the risk of injury. The only study44 (moderate quality) that measured peak vertical GRF and did not find that it was lower in the surgical than the nonsurgical limb involved a single-legged landing task in which it was not possible to unload the surgical limb by placing additional load on the nonsurgical limb. Anterior cruciate ligament reconstruction had a large effect on asymmetry during single-limb landings only for mean knee-extension moment and knee-energy absorption. This result suggests that, whereas it is not possible to unload the injured limb by increasing loading on the uninjured limb, athletes may still attempt to reduce the peak loading on the knee by spreading the loading over a longer time.
Generally, researchers reported differences far more commonly in kinetic than in kinematic variables. Lepley and Kuenze28 demonstrated no conclusive effect of asymmetry in hip or knee kinematics during landing. The only kinematic variables for which the meta-analyses identified asymmetry were peak knee-flexion angle during both double- and single-limb landings and peak ankle-dorsiflexion angle during double-limb landing, but these variables had only moderate effect sizes. In all studies, comparable 3-dimensional motion-analysis techniques were implemented to measure joint kinematics (between 8 and 10 camera systems sampling at either 120 or 240 Hz). While several different marker sets were used, it is fair to assume that the motion-analysis techniques used by all authors would elicit high-quality kinematic data. Although some investigators reported differences in sagittal-plane kinematics (9 differences at 28 times measured across 8 studies37–42,44,45: 4 high37,38,40,41 and 4 moderate39,42,44,45 quality), only once44 (moderate-quality study) did a frontal- or transverse-plane kinematic variable differ between limbs in the 13 measured cases. This is, therefore, an area for future work, particularly because frontal- and transverse-plane kinematic variables, such as knee-valgus angle and hip internal rotation, have been strongly implicated as risk factors for ACL injury.9,47–49 However, these findings relate only to asymmetry between surgical and nonsurgical limbs and not to comparisons between injured and healthy individuals or between pre- and post-ACL injury. Consensus is lacking on the extent of asymmetries in lower limb biomechanics between dominant and nondominant limbs in the general healthy population, with some groups reporting no differences50 and others reporting some differences.47,51 Of the 13 studies included in this systematic review, only 2 (1 high41 and 1 moderate43 quality) described which limb (dominant or nondominant) was injured, and no apparent control for limb dominance was included in any statistical analyses. The authors who supplied the percentage of injuries to the dominant limb provided values of 48% (11/23)43 and 54% (33/61),41 supporting previous research that showed no relationship between the side of primary ACL injury and limb dominance.52–54
Whereas kinetic variables in the frontal and transverse planes were not commonly measured, investigators in the 3 studies (2 high40,41 and 1 moderate44 quality) that did so identified asymmetry. In our review, the only frontal-plane kinetic variable that was different between limbs was mean knee frontal-plane moment (average adduction moment acting about the knee between initial ground contact and maximum knee flexion during the landing maneuver) during double- and single-limb landings, which demonstrated a moderate effect size. This highlights the need for further investigation of frontal- and transverse-plane asymmetries between surgical and nonsurgical limbs.
Although 5 groups (reflecting 3 high-38,40,41 and 2 moderate-39,44 quality studies) examined mechanical asymmetries at the hip and ankle joints, most of the asymmetric variables were at the knee joint. The only variables that were asymmetric at the ankle were ankle-energy absorption and mean ankle sagittal-plane moment during double-limb landings, with large effect sizes. No meaningful effect of asymmetry was apparent in peak hip-flexion angle, mean hip sagittal-plane moment, or hip-energy absorption after ACLR. This contrasts with the findings of Lepley and Kuenze,28 who observed large effects for peak hip sagittal-plane moment during double-limb landings in adult participants. Given that the knee was the site of the surgical reconstruction, it is perhaps to be expected that most asymmetry would occur at that joint, which emphasizes the need for rehabilitation practices to focus there, with less concern about compensatory movements in other joints of the kinetic chain.
Among adult participants after ACLR, asymmetries were present in both loading and movement patterns.11,28,39,42,55 These asymmetries included reductions in knee flexion, knee sagittal-plane moment, and vertical GRF on the surgical side compared with the nonsurgical side.11,28,56–61 We determined that these variables also affected between-limbs symmetry in adolescent participants after ACLR. Therefore, asymmetry in landing biomechanics after ACLR may be similar between adults and adolescents, and differences in secondary ACL injury prevalence between these populations do not necessarily depend on variations in landing asymmetry but may be linked to other factors, such as skeletal maturity and eagerness to return to participation in competitive sports.
For the studies included in the review, participants were tested approximately 4 to 12 months after ACLR. As expected, asymmetries were more commonly noted in participants who were tested closer to the time of surgery. However, authors of the 3 studies (2 high38,40 and 1 moderate39 quality) that involved >1 test session reported that many asymmetries were still present approximately 8 to 12 months after ACLR. When the same participants were tested on multiple occasions, the asymmetry was reduced as the time after reconstruction increased, showing that any rehabilitation practices the participants were pursuing were effectively reducing the asymmetry in landing mechanics.
Clinical Implications
Overall, asymmetries were more commonly identified in kinetic variables than in kinematic variables, which strongly supports the notion that return-to-play criteria for athletes after ACLR require assessment of between-limb loading asymmetry and should not rely on assessment of symmetry in movement patterns alone. Current criteria typically include consideration of the time since surgery, symmetry between the surgical and nonsurgical limbs in both strength and hop distance, and qualitative movement analysis during sporting tasks.25 Our review showed that some athletes were likely to exhibit symmetric movement patterns between limbs but potentially dangerous loading asymmetries. This was also supported by Orishimo et al,57 who showed that the hopping asymmetry ratio (surgical/nonsurgical limb × 100) in adult males after ACLR was 93%, whereas the peak knee-power asymmetry was 57%. Therefore, if return-to-play criteria include only a kinematic description of asymmetry between limbs, many athletes would likely be prematurely cleared to return to competition and subsequently risk secondary ACL injury. In addition, athletes returning from ACLR should focus more on achieving loading symmetry between limbs, particularly in vertical GRF and knee-extension moments, rather than on kinematic symmetry. Thus, we recommend measuring these variables during the rehabilitation process to provide feedback on the loading of each limb during landing tasks. This is a challenge for medical professionals who do not always have access to expensive equipment for measuring GRF and knee-joint loading, such as force plates and 3-dimensional motion-analysis systems. However, with the increased availability and affordability of mobile monitoring technology, such as accelerometers, that provide valid and reliable measurements of impact forces during landing,62 cutting,63 and running63,64 tasks, clinicians involved in determining return to play after ACLR should consider incorporating such technology to analyze lower limb loading.
Limitations
The limitations of our study included difficulty in formulating an inclusion criterion for adolescent athletes because many authors reported only age means and standard deviations rather than the range or information on maturity status. Researchers should consider developing improved return-to-play criteria after ACLR that include affordable techniques for analyzing lower limb loading during landing. Our study also highlighted the need for attention to asymmetric frontal- and transverse-plane mechanics after ACLR. Lastly, a small number of investigators examined single-limb landing tasks; therefore, comparisons between double- and single-limb tasks were limited for some variables.
CONCLUSIONS
Asymmetries between surgical and nonsurgical limbs were more frequently identified in kinetic than in kinematic variables. The most common asymmetries described were peak knee-extension moment and peak vertical GRF during double-limb landing, both of which were frequently less in the surgical than the nonsurgical limb. In most cases, lower limb kinematics did not display asymmetry. Our meta-analysis indicated that ACLR appeared to have a large effect on asymmetry in peak vertical GRF, peak knee-extension moment, and loading rate during double-limb landings and mean knee-extension moment and knee-energy absorption during both double- and single-limb landings. Large effect sizes were observed for asymmetry in ankle-energy absorption and mean ankle sagittal-plane moment during double-limb landings but not during single-limb landings. Moderate effect sizes were present for asymmetry in mean knee frontal-plane moment and peak knee-flexion angle during both double- and single-limb landings and peak ankle-dorsiflexion angle during double-limb landings. No meaningful asymmetry was demonstrated in peak hip-flexion angle, mean hip sagittal-plane moment, or hip-energy absorption. Our findings suggested that return-to-sport criteria after ACLR should incorporate analysis of the loading experienced by each limb rather than movement patterns alone.
Supplementary Material
REFERENCES
- 1.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 2.McNair PJ, Marshall RN, Matheston JA. Important features associated with acute anterior cruciate ligament injury. N Z Med J. 1990;103(901):537–539. [PubMed] [Google Scholar]
- 3.Linko E, Harilainen A, Malmivaara A, Seitsalo S. Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev. 2005;(2) doi: 10.1002/14651858.CD001356.pub3. CD001356. [DOI] [PubMed] [Google Scholar]
- 4.Quatman CE, Ford KR, Myer GD, Hewett TE. Maturation leads to gender differences in landing force and vertical jump performance: a longitudinal study. Am J Sports Med. 2006;34(5):806–813. doi: 10.1177/0363546505281916. [DOI] [PubMed] [Google Scholar]
- 5.Hewett TE, Myer GD, Ford KR, Slauterbeck JR. Preparticipation physical examination using a box drop vertical jump test in young athletes: the effects of puberty and sex. Clin J Sport Med. 2006;16(4):298–304. doi: 10.1097/00042752-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. N Am J Sports Phys Ther. 2009;4(1):2–12. [PMC free article] [PubMed] [Google Scholar]
- 7.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34(4):269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 8.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 9.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337–349. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 11.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258–262. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 12.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A. 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 14.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 15.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 16.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 17.Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. doi: 10.2106/JBJS.H.00539. [DOI] [PubMed] [Google Scholar]
- 18.Rauh MJ, Macera CA, Ji M, Wiksten DL. Subsequent injury patterns in girls' high school sports. J Athl Train. 2007;42(4):486–494. [PMC free article] [PubMed] [Google Scholar]
- 19.Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The Landing Error Scoring System as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50(6):589–595. doi: 10.4085/1062-6050-50.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunn KL, Lam KC, Valovich McLeod TC. Early operative versus delayed or nonoperative treatment of anterior cruciate ligament injuries in pediatric patients. J Athl Train. 2016;51(5):425–427. doi: 10.4085/1062-6050.51.5.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41(6):377–387. doi: 10.2519/jospt.2011.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 23.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE. Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2011;41(8):553–559. doi: 10.2519/jospt.2011.3591. [DOI] [PubMed] [Google Scholar]
- 24.Shelbourne KD, Klotz C. What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. J Orthop Sci. 2006;11(3):318–325. doi: 10.1007/s00776-006-1007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 26.Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente Anterior Cruciate Ligament Registry. Am J Sports Med. 2016;44(2):331–336. doi: 10.1177/0363546515614813. [DOI] [PubMed] [Google Scholar]
- 27.LaBella CR, Hennrikus W, Hewett TE. Council on Sports Medicine and Fitness, and Section on Orthopaedics. Anterior cruciate ligament injuries: diagnosis, treatment, and prevention. Pediatrics. 2014;133(5):e1437–e1450. doi: 10.1542/peds.2014-0623. [DOI] [PubMed] [Google Scholar]
- 28.Lepley AS, Kuenze CM. Hip and knee kinematics and kinetics during landing tasks after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. J Athl Train. 2018;53(2):144–159. doi: 10.4085/1062-6050-334-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Malina RM, Bar-Or O, Bouchard C. Growth Maturation and Physical Activity 2nd ed. Champagn, IL: Human Kinetics;; 2004. p. 8. [Google Scholar]
- 30.Dayanidhi S, Hedberg A, Valero-Cuevas FJ, Forssberg H. Developmental improvements in dynamic control of fingertip forces last throughout childhood and into adolescence. J Neurophysiol. 2013;110(7):1583–1592. doi: 10.1152/jn.00320.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hart HF, Culvenor AG, Collins NJ, et al. Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2016;50(10):597–612. doi: 10.1136/bjsports-2015-094797. [DOI] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical Power Analysis for Behavioral Sciences 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;; 1988. [Google Scholar]
- 34.Yeow CH, Lee PV, Goh JC. An investigation of lower extremity energy dissipation strategies during single-leg and double-leg landing based on sagittal and frontal plane biomechanics. Hum Mov Sci. 2011;30(3):624–635. doi: 10.1016/j.humov.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 35.Myer GD, Martin L, Jr, Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40(10):2256–2263. doi: 10.1177/0363546512454656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3) doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 37.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. doi: 10.1249/MSS.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Renner KE, Franck CT, Miller TK, Queen RM. Limb asymmetry during recovery from anterior cruciate ligament reconstruction. J Orthop Res. 2018;36(7):1887–1893. doi: 10.1002/jor.23853. [DOI] [PubMed] [Google Scholar]
- 39.Butler RJ, Dai B, Huffman N, Garrett WE, Queen RM. Lower extremity movement differences persist after anterior cruciate ligament reconstruction and when returning to sports. Clin J Sport Med. 2016;26(5):411–416. doi: 10.1097/JSM.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 40.Mueske NM, Patel AR, Pace JL, et al. Improvements in landing biomechanics following anterior cruciate ligament reconstruction in adolescent athletes. Sports Biomech. 2018] doi: 10.1080/14763141.2018.1510539. [published online ahead of print October 2. [DOI] [PubMed]
- 41.Mueske NM, VandenBerg CD, Pace JL, et al. Comparison of drop jump landing biomechanics and asymmetry among adolescents with hamstring, patellar and quadriceps tendon autografts for anterior cruciate ligament reconstruction. Knee. 2018;25(6):1065–1073. doi: 10.1016/j.knee.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 42.Butler RJ, Dai B, Garrett WE, Queen RM. Changes in landing mechanics in patients following anterior cruciate ligament reconstruction when wearing an extension constraint knee brace. Sports Health. 2014;6(3):203–209. doi: 10.1177/1941738114524910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dai B, Butler RJ, Garrett WE, Queen RM. Using ground reaction force to predict knee kinetic asymmetry following anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2014;24(6):974–981. doi: 10.1111/sms.12118. [DOI] [PubMed] [Google Scholar]
- 44.Wren TA, Mueske NM, Brophy CH, et al. Hop distance symmetry does not indicate normal landing biomechanics in adolescent athletes with recent anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48(8):622–629. doi: 10.2519/jospt.2018.7817. [DOI] [PubMed] [Google Scholar]
- 45.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes after anterior cruciate ligament reconstruction with single-leg landing asymmetries at the time of return to sport demonstrate decreased knee function 2 years later. Am J Sports Med. 2017;45(11):2604–2613. doi: 10.1177/0363546517708996. [DOI] [PubMed] [Google Scholar]
- 46.Schneider DK, Gokeler A, Otten E, et al. A novel mass-spring-damper model analysis to identify landing deficits in athletes returning to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2017;31(9):2590–2598. doi: 10.1519/JSC.0000000000001569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hughes G, Watkins J, Owen N. Gender differences in lower limb frontal plane kinematics during landing. Sports Biomech. 2008;7(3):333–341. doi: 10.1080/14763140802233215. [DOI] [PubMed] [Google Scholar]
- 48.Kernozek TW, Torry MR, Van Hoof H, Cowley H, Tanner S. Gender differences in frontal plane and sagittal plane biomechanics during drop landings. Med Sci Sport Exerc. 2005;37(6):1003–1012. [PubMed] [Google Scholar]
- 49.Krosshaug T, Steffen K, Kristianslund E, et al. The vertical drop jump is a poor screening test for ACL injuries in female elite soccer and handball players: a prospective cohort study of 710 athletes. Am J Sports Med. 2016;44(4):874–883. doi: 10.1177/0363546515625048. [DOI] [PubMed] [Google Scholar]
- 50.van der Harst JJ, Gokeler A, Hof AL. Leg kinematics and kinetics in landing from a single-leg hop for distance: a comparison between dominant and non-dominant leg. Clin Biomech (Bristol Avon) 2007;22(6):674–680. doi: 10.1016/j.clinbiomech.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 51.Edwards S, Steele JR, Cook JL, Purdam CR, McGhee DE. Lower limb movement symmetry cannot be assumed when investigating the stop-jump landing. Med Sci Sports Exerc. 2012;44(6):1123–1130. doi: 10.1249/MSS.0b013e31824299c3. [DOI] [PubMed] [Google Scholar]
- 52.Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med. 2010;44(10):694–697. doi: 10.1136/bjsm.2008.051243. [DOI] [PubMed] [Google Scholar]
- 53.Matava MJ, Freehill AK, Grutzner S, Shannon W. Limb dominance as a potential etiologic factor in noncontact anterior cruciate ligament tears. J Knee Surg. 2002;15(1):11–16. [PubMed] [Google Scholar]
- 54.Negrete RJ, Schick EA, Cooper JP. Lower-limb dominance as a possible etiologic factor in noncontact anterior cruciate ligament tears. J Strength Cond Res. 2007;21(1):270–273. doi: 10.1519/00124278-200702000-00048. [DOI] [PubMed] [Google Scholar]
- 55.Goerger BM, Marshall SW, Beutler AI, Blackburn JT, Wilckens JH, Padua DA. Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: the JUMP-ACL study. Br J Sports Med. 2015;49(3):188–195. doi: 10.1136/bjsports-2013-092982. [DOI] [PubMed] [Google Scholar]
- 56.Gokeler A, Hof AL, Arnold MP, Dijkstra PU, Postema K, Otten E. Abnormal landing strategies after ACL reconstruction. Scand J Med Sci Sports. 2010;20(1):e12–e19. doi: 10.1111/j.1600-0838.2008.00873.x. [DOI] [PubMed] [Google Scholar]
- 57.Orishimo KF, Kremenic IJ, Mullaney MJ, McHugh MP, Nicholas SJ. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1587–1593. doi: 10.1007/s00167-010-1185-2. [DOI] [PubMed] [Google Scholar]
- 58.Dai B, Butler RJ, Garrett WE, Queen RM. Anterior cruciate ligament reconstruction in adolescent patients: limb asymmetry and functional knee bracing. Am J Sports Med. 2012;40(12):2756–2763. doi: 10.1177/0363546512460837. [DOI] [PubMed] [Google Scholar]
- 59.von Porat A, Henriksson M, Holmström E, Roos EM. Knee kinematics and kinetics in former soccer players with a 16-year-old ACL injury—the effects of twelve weeks of knee-specific training. BMC Musculoskelet Disord. 2007;8:35. doi: 10.1186/1471-2474-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Delahunt E, Sweeney L, Chawke M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30(1):72–78. doi: 10.1002/jor.21504. [DOI] [PubMed] [Google Scholar]
- 61.Trigsted SM, Post EG, Bell DR. Landing mechanics during single hop for distance in females following anterior cruciate ligament reconstruction compared to healthy controls. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1395–1402. doi: 10.1007/s00167-015-3658-9. [DOI] [PubMed] [Google Scholar]
- 62.Tran J, Netto K, Aisbett B, Gastin P. Validation of accelerometer data for measuring impacts during jumping and landing tasks. 28th International Conference on Biomechanics in Sports; July 19–23. 2010. Paper presented at. Marquette, MI.
- 63.Wundersitz DW, Netto KJ, Aisbett B, Gastin PB. Validity of an upper-body-mounted accelerometer to measure peak vertical and resultant force during running and change-of-direction tasks. Sports Biomech. 2013;12(4):403–412. doi: 10.1080/14763141.2013.811284. [DOI] [PubMed] [Google Scholar]
- 64.Norris M, Anderson R, Kenny IC. Method analysis of accelerometers and gyroscopes in running gait: a systematic review. Proc Inst Mech Eng P J Sport Eng Technol. 2014;228(1):3–15. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.