Abstract
Objective
The novel coronavirus SARS-CoV-2 (COVID-19) pandemic has posed significant changes to physician workflow and healthcare delivery. This national survey investigated the impact of the pandemic on burnout and career satisfaction among U.S. attending neurosurgeons.
Methods
A 24-question survey was sent electronically to all American Association of Neurological Surgeons (AANS) attending members. The abbreviated Maslach Burnout Inventory (aMBI) was used to measure the following burnout and career satisfaction indices: emotional exhaustion, depersonalization, and personal accomplishment. Bivariate analyses were conducted and multivariate analyses were performed using logistic regression models.
Results
407 attending neurosurgeons were included in the present study, with an overall response rate of 17.7 %. The majority of respondents were male (88.7 %), White (84.3 %), and in practice for 15 years or more (64.6 %). The majority reported a decrease in work hours due to the pandemic (82.6 %), uncertainty about future earnings (80.3 %), and uncertainty regarding future healthcare reform (84.5 %). Burnout was identified in 83 (20.4 %) respondents, whereas career satisfaction was identified in 316 (77.6 %) respondents. Rate of burnout was decreased when compared to rates reported in the pre-COVID era.
In multivariate analysis, burnout was associated with working in a hostile or difficult environment since the rise of COVID-19 (OR = 2.534, p = 0.008), not having children (OR = 3.294, p = 0.011), being in practice for 5−15 years (vs. < 5 years) (OR = 4.568, p = 0.014), spending increased time conducting non-neurosurgical medical care due to COVID-19 (OR = 2.362, p = 0.019), feeling uncertain about future earnings due to COVID-19 (OR = 4.031, p = 0.035), and choosing not to pursue or feeling uncertain about pursuing neurosurgery again if given the choice (OR = 7.492, p < 0.001). Career satisfaction was associated with cerebrovascular subspecialty training (OR = 2.614, p = 0.046) and a willingness to pursue neurosurgery again if given the choice (OR = 2.962, p < 0.001).
Conclusion
Factors related to the novel COVID-19 pandemic have contributed to changes in workflow among U.S. attending neurosurgeons. Despite these changes, we report decreased burnout and high career satisfaction among U.S. neurosurgeons. Understanding modifiable stressors among neurosurgeons during the pandemic may help to identify effective future interventions to mitigate burnout and improve career satisfaction.
Keywords: COVID-19, Pandemic, Burnout, Career satisfaction, Neurosurgery, Attending
1. Introduction
The COVID-19 pandemic has disrupted surgical practice globally. A decrease in surgical case volumes, increased utilization of telemedicine, and increased redeployment of surgical specialists for non-surgical medical care are among the many impacts the pandemic has had on surgical practice [1,2]. Neurosurgical practice has been particularly impacted, leading to centers reporting significant financial losses, changes in call schedules, and increased use of virtual education [2,3]. Outside of structural changes to surgical care, the pandemic has also been associated with the physical, mental, and emotional exhaustion of healthcare workers [4,5]. With more than three million cases in the U.S. alone, COVID-19 has placed increased physical and psychological burdens on health care workers, and these stressors may be associated with exacerbation of physician career dissatisfaction and burnout [6].
Physician burnout has been defined as a syndrome of work-related emotional exhaustion, feelings of depersonalization, detachment from patients, and low sense of personal accomplishment [7,8]. Physician burnout has been associated with increased rates of medical errors, involvement in malpractice lawsuits, substance use, and suicidal ideation [9,10]. The association between the impact of COVID-19 on changes in neurosurgical practice and physician wellbeing, including physician burnout and career satisfaction, has yet to be studied. The rates of burnout among attending neurosurgeons has been studied prior to the COVID-19 pandemic. McAbee et al. conducted a survey of 783 neurosurgeons and discovered an overall burnout rate of 57%, with anxiety regarding future earnings and healthcare reform associated with increased burnout [10]. Klimo et al. conducted a pilot survey of 85 neurosurgeons and discovered an overall burnout rate of 27%, with low salary and uncertainty regarding future earnings and healthcare reform identified as stressful factors by the majority of participants [11]. As neurosurgical care resumes, it will be important to identify which factors are associated with decreased career satisfaction and increased burnout among attending neurosurgeons. This study aims to report the rates of burnout and career satisfaction among attending neurosurgeons during the COVID-19 pandemic while identifying potential areas for intervention. We aimed to capture a “snapshot” of burnout at a single time point during the pandemic in order to inform potential interventions in the event of future pandemics or recurrences.
2. Materials and methods
2.1. Study population
An online survey assessing burnout among attending neurosurgeons was created using the Qualtrics platform (Qualtrics, Provo, UT). An email describing the study purpose and containing the survey link was sent to all current attending neurosurgeon members of the American Association of Neurological Surgeons (AANS) on behalf of the AANS Young Neurosurgeons Committee in May 2020. The attending neurosurgeons included in the present study were comprised of AANS non-resident neurosurgeons from both academic and non-academic institutions. Attending neurosurgeons were invited to complete the voluntary survey within 2 weeks, and a follow-up request was sent via email 1 week after the initial request. Survey responses were collected anonymously, and responses with incomplete data were excluded from analysis. All survey recipients were U.S. neurosurgeons with membership in AANS. This study was exempt from institutional review board approval due to lack of identifiable participant information. The survey was reviewed for content validity and piloted to 4 independent faculty neurosurgeons (D.D., W.S., J.J., D.M) to ensure ease of use and comprehension prior to distribution.
2.2. Survey design
The 24-item survey consisted of questions about demographics, workflow changes related to COVID-19, personal and professional stressors, career satisfaction, and burnout (Appendix). Questions related to COVID-19 ascertained the effect of the pandemic on respondents’ workload, personal and professional lives, uncertainty regarding future earnings and changes in healthcare, and state of mind. Additional questions focused on ascertaining which stressors were most affecting respondents’ practice since the rise of COVID-19 and how respondents had spent their time since the rise of the pandemic. Finally, an optional open-ended question allowed respondents to report what they found to be the most challenging aspect of their role during the COVID-19 pandemic.
The effect of COVID-19 on respondents’ personal and professional lives was scored along a 5-point Likert scale. Responses were collapsed into three categories (“Improved,” “No change,” and “Worsened”) for the purposes of statistical interpretation. Impact of COVID-19 on weekly work hours and uncertainty about future earnings and healthcare reform as a result of the pandemic were also scored along a 5-point Likert scale; responses were similarly collapsed into three categories for statistical analysis. Responses regarding the alteration of vacation schedules due to COVID-19 were converted into a dichotomous variable with the following categories: “Altered schedule at least once” and “Did not alter schedule.” Responses regarding whether individuals would pursue neurosurgery again if given the choice were also converted to a dichotomous variable, with responses of “No” and “Do not know” combined into a single category (“No/Unsure”).
Burnout was assessed using the previously-validated abbreviated Maslach Burnout Inventory (aMBI) [12,13], which uses a 9-item questionnaire to assess three indices related to burnout: emotional exhaustion (EE; 3 questions), depersonalization (DP; 3 questions), and personal accomplishment (PA; 3 questions). Each question was scored on a 7-point Likert scale, and the total score for each aMBI index was categorized as low (0−6 points), intermediate (7−12 points), or high (13−18 points). Burnout was defined as a high score in either EE or DP as consistent with previously published studies assessing physician burnout [8,9]. Respondents were classified as being satisfied with their career if they selected “Every day” or “A few times a week” in response to Question 6 of the aMBI (“I feel I’m positively influencing other people’s lives through my work”).
2.3. Statistical analysis
Demographic information and information regarding the effect of COVID-19 on various aspects of respondents’ lives was compiled using descriptive statistics. As mentioned previously, select survey responses using 5-point Likert scales were collapsed into dichotomous or trichotomous variables for the purpose of statistical analysis. Descriptive statistics were also used to describe the proportion of neurosurgery attendings receiving low, intermediate, and high scores for each of the 3 aMBI indices (EE, DP, PA) as well as to assess the proportion of attending neurosurgeons that scored positive for burnout and career satisfaction. Low, intermediate, and high scores for each aMBI index were reported as mean ± standard deviation (SD). All descriptive data were summarized into tables displaying the number and proportion of respondents in each category.
Bivariate analysis was performed to look for factors associated with EE, DP, PA, burnout, and career satisfaction. A Shapiro-Wilk test to assess normality revealed that numerical scores for the 3 burnout indices did not follow a normal distribution. Comparisons between groups of categorical variables were performed using chi-square tests and Fisher’s exact tests. Any factor found to have a p-value ≤ 0.1 in bivariate analysis was placed in a multivariate binary logistic regression analysis using a forward stepwise approach to investigate predictors of burnout and career satisfaction. The binary logistic regression models generated in multivariate analysis were internally validated using bias-corrected bootstrapping with 1000 samples, and the accuracy of the regression models at predicting burnout or career satisfaction was assessed using area under receiver operating characteristic (AUROC) scores. Results were reported with p-values, odds ratios (OR), and corresponding 95% confidence intervals (CI). P-values ≤ 0.05 were considered statistically significant. All data analysis was conducted using IBM SPSS Statistics software (Version 25.0; IBM Corp., Armonk, NY).
3. Results
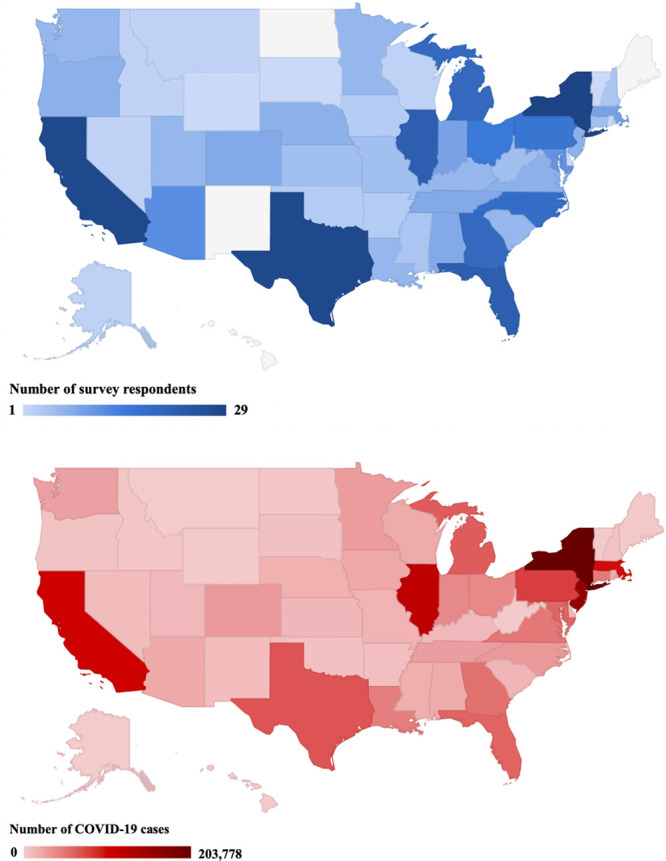
Of the 3000 attending neurosurgeons invited to complete the survey, 671 clicks to the survey link were logged and 531 total survey responses were received. The overall response rate was 17.7% among all AANS attending neurosurgeons and 79.1% among those who accessed the survey link. Among the total responses received, 124 were excluded on the basis of incomplete responses, yielding 407 complete responses to be included in the final analysis. The majority of attending neurosurgeons who responded were male (88.7%), White (84.3%), between the ages of 40 and 60 (65.4%), had children (89.4%), and were in practice for >15 years (64.6%). Most attendings worked between 50−70 hours per week (58.9%), had at least 6 on-call days per month (71.8%), and performed at least 200 operative cases annually on average (64.9%). All summary of respondent demographic data and practice characteristics can be found in Table 1 , and a heat map visualization of respondents by U.S. state has also been provided (Supplementary Figure 1).
Table 1.
Demographic Information and Practice Characteristics of AANS Attending Neurosurgeon Survey Respondents (N = 407).
| Characteristic | N (%) | |
|---|---|---|
| Age | ||
| 30−40 | 42 (10.3) | |
| 40−50 | 118 (29.0) | |
| 50−60 | 148 (36.4) | |
| 60−70 | 90 (22.1) | |
| >70 | 9 (2.2) | |
| Gender | ||
| Male | 361 (88.7) | |
| Female | 46 (11.3) | |
| Race | ||
| White | 343 (84.3) | |
| Asian | 42 (10.3) | |
| Black or African American | 4 (1.0) | |
| American Indian or Alaska Native | 1 (0.2) | |
| Other | 17 (4.2) | |
| Ethnicity | ||
| Not of Hispanic, Latino, or Spanish Origin | 382 (93.9) | |
| Hispanic, Latino, or Spanish Origin | 25 (6.1) | |
| Relationship Status | ||
| Stable Partner | 365 (89.7) | |
| Single | 42 (10.3) | |
| Have Children | ||
| Yes | 364 (89.4) | |
| No | 43 (10.6) | |
| Region | ||
| Northeast | 73 (17.9) | |
| Northwest | 115 (28.3) | |
| Southeast | 132 (32.4) | |
| Southwest | 87 (21.4) | |
| Number of Years in Practice | ||
| <5 | 47 (11.5) | |
| 5−15 | 97 (23.8) | |
| >15 | 263 (64.6) | |
| Formal Subspecialty Training | ||
| None | 150 (36.9) | |
| Spine/Peripheral Nerve | 87 (21.4) | |
| Cerebrovascular | 55 (13.5) | |
| Pediatrics | 53 (13.0) | |
| Neuro-oncology | 37 (9.1) | |
| Functional/Stereotactic | 35 (8.6) | |
| Endovascular | 26 (6.4) | |
| Critical Care | 15 (3.7) | |
| Avg. Number of Weekly Work Hours Prior to COVID-19 | ||
| <30 | 10 (2.5) | |
| 30−40 | 22 (5.4) | |
| 41−50 | 54 (13.3) | |
| 51−60 | 134 (32.9) | |
| 61−70 | 106 (26.0) | |
| 71−80 | 40 (9.8) | |
| >80 | 41 (10.1) | |
| Avg. Number of Monthly On-Call Days Prior to COVID-19 | ||
| <3 | 33 (8.1) | |
| 3−5 | 82 (20.1) | |
| 6−10 | 168 (41.3) | |
| >10 | 124 (30.5) | |
| Avg. Number of Yearly Operative Cases Prior to COVID-19 | ||
| <100 | 12 (2.9) | |
| 100−200 | 119 (29.2) | |
| 200−300 | 138 (33.9) | |
| 300−400 | 85 (20.9) | |
| >400 | 41 (10.1) | |
| Number of Times Named in Malpractice Lawsuits in Last Five Years | ||
| 0 | 259 (63.6) | |
| 1−5 | 146 (35.9) | |
| >5 | 2 (0.5) | |
| Practice Type | ||
| University | 134 (32.9) | |
| Group | 115 (28.3) | |
| Private with academic affiliation | 66 (16.2) | |
| Solo | 35 (8.6) | |
| City/county hospital | 26 (6.4) | |
| Health management organization | 15 (3.7) | |
| Veterans Affairs/government hospital | 4 (1.0) | |
| Other | 12 (2.9) | |
Among the attending neurosurgeons surveyed, the majority expressed uncertainty regarding future changes in healthcare (84.5%) and earnings (80.3%) due to COVID-19. Most neurosurgeons reported a decrease in weekly work hours due to COVID-19 (82.6%) and stated that their vacation schedules had been altered at least once due to the pandemic (82.1%). A large percentage also perceived that their professional life would worsen due to COVID-19 (60.2%). When asked whether they would pursue neurosurgery again if given the choice, 24.3% of attending neurosurgeons indicated that they would not pursue, or were unsure about pursuing, neurosurgery again. Since the rise of the pandemic, the majority of attendings surveyed spent increased time interacting with family members (71.0%). A notable proportion also reported spending increased time participating in remote didactic lectures held by their program or national organizations (e.g. AANS, CNS) (36.6%). Respondents indicated that the three stressors most affecting their practice due to COVID-19 were too few cases (78.6%), uncertainty of future earnings or healthcare reform (78.1%), and low salary/income (43.5%). These and other perceptions related to COVID-19 have been summarized in Table 2 .
Table 2.
Attending Neurosurgeons' Perceptions and Stressors Related to COVID-19.
| Perception | N (%) |
|---|---|
| Uncertainty about future changes in healthcare due to COVID-19 | 344 (84.5) |
| Decreased weekly work hours due to COVID-19 | 336 (82.6) |
| Altered vacation schedule due to COVID-19 | 334 (82.1) |
| Uncertainty about future earnings due to COVID-19 | 327 (80.3) |
| Professional life will worsen due to COVID-19 | 245 (60.2) |
| Personal life will worsen due to COVID-19 | 143 (35.1) |
| Unsure or would not pursue neurosurgery again | 99 (24.3) |
| Stressors most affecting practice due to COVID-19: | |
| Too few cases | 320 (78.6) |
| Uncertainty of future earnings or health care reform | 318 (78.1) |
| Low salary/income | 177 (43.5) |
| Hostile or difficult work environment | 86 (21.1) |
| Too little vacation time | 58 (14.3) |
| Too much call | 53 (13.0) |
| Loss of coworker/faculty | 49 (12.0) |
| Inadequate teaching time | 33 (8.1) |
| Demands of senior faculty members | 27 (6.6) |
| Surgery-related complications | 27 (6.6) |
| Inadequate administrative time | 23 (5.7) |
| Tenure/promotion issues | 18 (4.4) |
| Inadequate research time | 15 (3.7) |
| Malpractice issues | 14 (3.4) |
| Too many cases | 3 (0.7) |
| Since rise of COVID-19, I have spent increased time: | |
| Interacting with my family members | 289 (71.0) |
| Participating in remote didactic lectures | 149 (36.6) |
| Working on clinical research studies | 93 (22.9) |
| Conducting non-neurosurgical medical care | 79 (19.4) |
| Conducting neurosurgical medical care | 57 (14.0) |
| Engaging with other residents or faculty | 43 (10.6) |
| Partaking in board preparation | 21 (5.2) |
| In the cadaver/anatomy lab | 3 (0.7) |
| None of the above | 45 (11.1) |
Abbreviations: COVID-19 (Coronavirus Disease 2019).
3.1. Burnout and career satisfaction among attending neurosurgeons
The overall burnout rate among attending neurosurgeons was 20.4%, whereas the overall rate of career satisfaction was 77.6% (Table 3 ). The majority of respondents reported low levels of emotional exhaustion (51.6%), low levels of depersonalization (87.5%), and high levels of personal accomplishment (81.1%).
Table 3.
Burnout and Career Satisfaction Indices Among 407 Attending Neurosurgeons.
| Burnout Index | Mean Score (SD) | N (%) |
|---|---|---|
| Burnout | 83 (20.4) | |
| Emotional Exhaustion | 7.05 (5.12) | |
| Low score (0−6) | 210 (51.6) | |
| Intermediate score (7−12) | 119 (29.2) | |
| High score (13−18) | 78 (19.2) | |
| Depersonalization | 2.73 (3.46) | |
| Low score (0−6) | 356 (87.5) | |
| Intermediate score (7−12) | 41 (10.1) | |
| High score (13−18) | 10 (2.5) |
| Career Satisfaction Index | Mean Score (SD) | N (%) |
|---|---|---|
| Career Satisfaction | 316 (77.6) | |
| Personal Accomplishment | 15.06 (2.71) | |
| Low score (0−6) | 3 (0.7) | |
| Intermediate score (7−12) | 74 (18.2) | |
| High score (13−18) | 330 (81.1) |
Abbreviations: SD (Standard Deviation).
In bivariate analysis, factors strongly associated with burnout since the rise of COVID-19 included working in a hostile or difficult work environment (p < 0.001), spending increased time conducting non-neurosurgical medical care (p < 0.001), feeling uncertain about future earnings (p = 0.005), not having children (p = 0.013), and performing too few cases (p = 0.013). Respondents who were burned out were less likely to have spent increased time interacting with family members (p = 0.007), less likely to pursue neurosurgery again if given the choice (p < 0.001), and more likely to feel that their professional (p < 0.001) and personal (p < 0.001) lives had worsened due to COVID-19. Factors strongly associated with career satisfaction since the rise of COVID-19 included Hispanic, Latino, or Spanish ethnic origin (p = 0.023), cerebrovascular subspecialty training (p = 0.028), and having children (p = 0.037). Attending neurosurgeons who were satisfied with their career were less likely to have received spine/peripheral nerve subspecialty training (p = 0.028) and were less likely to feel that their professional life had worsened due to COVID-19 (p = 0.045). Neurosurgeons satisfied with their career were also more likely to pursue neurosurgery again if given the choice (p < 0.001).
In multivariate analysis, burnout was associated with working in a hostile or difficult environment since the rise of COVID-19 (OR = 2.534, 95% CI: 1.273−5.046, p = 0.008), not having children (OR = 3.294, 95% CI: 1.307−8.299, p = 0.011), being in practice for 5−15 years (vs. < 5 years) (OR = 4.568, 95% CI: 1.354−15.414, p = 0.014), spending increased time conducting non-neurosurgical medical care due to COVID-19 (OR = 2.362, 95% CI 1.153−4.839, p = 0.019), feeling uncertain about future earnings due to COVID-19 (OR = 4.031, 95% CI: 1.103−14.728, p = 0.035), and choosing not to pursue, or feeling uncertain about pursuing, neurosurgery again if given the choice (OR = 7.492, 95% CI: 4.003−14.021, p < 0.001). Career satisfaction was associated with cerebrovascular subspecialty training (OR = 2.614, 95% CI: 1.015−6.731, p = 0.046) and a willingness to pursue neurosurgery again if given the choice (OR = 2.962, 95% CI: 1.721−5.097, p < 0.001). All significant predictors of burnout maintained statistical significance after bias-corrected bootstrapping. The AUROC score for the regression model predictive of burnout was 0.857 (95% CI: 0.814−0.900), whereas the score for the regression model predictive of career satisfaction was 0.741 (95% CI: 0.687−0.796). The results of the multivariate analysis are provided in Table 4 .
Table 4.
Multivariate Binary Logistic Regression Analysis of 407 Attending Neurosurgeons.
| Characteristic | Factor | OR | 95% CI | p-value | Bootstrap p-value |
|---|---|---|---|---|---|
| Burnout | |||||
| Would not choose to pursue Neurosurgery again | 7.492 | 4.003−14.021 | <0.001 | <0.001 | |
| In practice for 5−15 yearsa | 4.568 | 1.354−15.414 | 0.01 | 0.01 | |
| Uncertainty about future earnings due to COVID-19 | 4.031 | 1.103−14.728 | 0.04 | 0.02 | |
| No children | 3.294 | 1.307−8.299 | 0.01 | 0.01 | |
| Working in a hostile or difficult environment since rise of COVID-19 | 2.534 | 1.273−5.046 | 0.01 | 0.02 | |
| Increased time conducting non-neurosurgical medical care due to COVID-19 | 2.362 | 1.153−4.839 | 0.02 | 0.04 | |
| Career Satisfaction | |||||
| Would choose to pursue Neurosurgery again | 2.962 | 1.721−5.097 | <0.001 | <0.001 | |
| Cerebrovascular subspecialty training | 2.614 | 1.015−6.731 | 0.05 | 0.03 |
a. Reference group consisted of neurosurgeons in practice for less than five years.
Abbreviations: CI (Confidence interval), OR (odds ratio).
An optional open-ended question at the conclusion of the survey allowed respondents to report what they found to be the most challenging aspect of their role as an attending neurosurgeon during the COVID-19 pandemic. This question received 194 total responses. Common themes among the responses included an inability to contribute to administrative protocols (20.6%), difficulty scheduling operations on patients whose cases had been deemed elective (19.1%), fear of contracting COVID-19 (17.0%), lack of interaction with patients (10.8%) or colleagues (5.7%), loss of work-life balance (10.8%), concern regarding income (9.8%), and feelings of underutilization during the pandemic (7.7%). Despite these challenges, a few neurosurgeons (3.1%) noted that they appreciated spending increased time with their family.
4. Discussion
4.1. Study findings
While neurosurgery can be a rewarding profession, aspects of the vocation are also demanding of some degree of personal sacrifice. Prior to the pandemic, physician burnout and its effects have been widely documented in the neurosurgical community [10,11,14]. Our study is the first of its kind to evaluate the effects of the COVID-19 pandemic on workflow changes, personal and professional stressors, career satisfaction, and burnout in attending neurosurgeons through a survey of U.S. members of the American Association of Neurologic Surgeons (AANS). We reported a response rate of 17.7% (531 responses) among all AANS attending neurosurgeons, which is comparable to a similar study conducted over a three-month period in 2012 prior to the COVID-19 pandemic (783 responses) [10]. Our response rate is similar to other published studies surveying neurosurgeons in the U.S [9,10].
Prior to the COVID-19 pandemic, physician burnout was prevalent among attending neurosurgeons, and rates of burnout and career dissatisfaction had been documented as ranging from 16 to 57% [8,10,11,15]. Our study demonstrated a burnout rate of 20.4%, which is at the lower end of the previously reported rates among neurosurgeons, and we have reported several factors that may be protective against burnout or contribute to it.
4.2. Effects of COVID-19 on neurosurgical practice and burnout
The majority of our survey respondents reported that they felt uncertain about future earnings and changes in healthcare due to COVID-19, had decreased work hours, and felt that their professional life would worsen due to the pandemic. McAbee et al. conducted a survey of 783 attending neurosurgeons prior to the pandemic that found anxiety regarding future earnings and healthcare reform was independently associated with burnout, and that a balance between work and life outside of the hospital was protective against burnout [10]. We also found that uncertainty in future earnings was associated with burnout during the COVID-19 pandemic.
COVID-19 has indeed created unprecedented changes in hospital revenues and earnings due to decreased surgical case volumes and decreased elective procedures. One report estimated that globally, 82% of elective surgery and 38% of oncological surgeries would be cancelled or postponed due to the pandemic [16]. These projections have been corroborated in early reports published by several U.S. neurosurgery programs [2,17,18]. A recent report from Harvard Medical School’s Department of Neurosurgery described a 44% reduction in operative charges during the first week of implementation of changes due to the pandemic and projected future reductions [17]. They further report that several academic medical centers in the Boston area have planned to halt pension contributions, bonus pay, or increases in salary due to the pandemic [17]. A similar report from University Hospitals Cleveland Medical Center described the pandemic’s greatest effect upon volume as impacting functional neurosurgery cases, while the treatment of unruptured aneurysm, spine conditions, and benign tumors have also seen significant reductions. With these changes in case volume and revenue have also come changes in policies regarding call hours, resident education, and restructuring of neurosurgical care [18]. There is also concern that the furloughing of ancillary neurosurgery team members may negatively impact neurosurgical care during the COVID-19 pandemic [19]. The Coronavirus Aid, Relief, and Economic Security (CARES) act of March 2020 provided $130 billion to hospitals for COVID-19-related expenses and revenue, which may provide some relief to hospitals after the pandemic; however, it is still likely that many will continue to experience uncertainty regarding their future earnings and stress from changes in healthcare delivery models due to the pandemic [20]. As low neurosurgical case volume may contribute to greater time spent conducting non-neurosurgical care and heightened uncertainty regarding future income and earnings, we anticipate, given our predictive model of burnout, that U.S. neurosurgeons will likely experience greater burnout as the pandemic progresses.
The psychological consequences of the pandemic are well-summarized in one of the free-text responses we recorded from an attending neurosurgeon, who described the impact that loss of physician autonomy has had on their wellbeing: “We define ourselves by [our] surgical prowess, derive benefit from neurosurgical interactions with patients, and feel empowered by commanding ORs and doing surgery. That has been taken away from us and significantly affects my well-being.” This correlates with our finding that those who ranked “too few cases” as a top stressor and those who had spent increased time conducting non-neurosurgical medical care due to COVID-19 were more likely to experience burnout.
4.3. Career satisfaction and factors protective against burnout
Interestingly, despite discovering a burnout rate of 20.4% among attending neurosurgeons, we also discovered a high rate of career satisfaction. McAbee et al. posited that burnout may occur transiently, such as in times of stress, whereas career satisfaction is more resistant to change and may remain stable throughout one’s career [10]. We discovered that those who would choose to not pursue neurosurgery again had higher rates of burnout, whereas those who would pursue the field again and those who underwent cerebrovascular subspecialty training had high rates of career satisfaction. Given the decline in cerebrovascular consultations and stroke case volume during the early phase of the pandemic due to mitigations efforts, we posit that the correlation between satisfaction and cerebrovascular subspecialty training may be due to decreased emergency operative and neurointerventional frequency with secondarily increased leisure time during the pandemic [21,22]. We also discovered that both having children and spending increased time with family members during the pandemic was independently associated with less risk of burnout. Indeed, the majority of our survey respondents reported having spent more time interacting with family during the pandemic, which may have contributed to the relatively low burnout rate that we report. These findings are in line with other studies positing a link between having no children and increased burnout [23]. The increased time spent at home with children, due to a combination of decreased case volumes and social distancing measures, may be one of the silver linings of the pandemic. Many of our survey respondents also stated that they had spent increased time participating in remote didactic lectures, working on clinical research studies, or partaking in board preparation, which all may contribute to decreased burnout by allowing for more time at home during the pandemic.
4.4. Model predicting burnout and areas for intervention
Our model predicting burnout during the pandemic includes attending neurosurgeons who do not have children, those who are in practice for 5−15 years (compared to <5 years), those who would not pursue neurosurgery again, those working in a difficult/hostile environment since the start of COVID-19, those spending increased time conducting non-neurosurgical care due to COVID-19, and those who had uncertainty about future earnings due to the pandemic. Our model demonstrated an AUROC of 0.857 and was able to discriminate attending neurosurgeons who were at potential risk for burnout during the pandemic. Our finding that those who were in practice for 5−15 years (compared to <5 years) were at higher risk of burnout matches reports in the literature. Dyrbye et al. discovered that physicians in mid-career (11–20 years) worked more hours, took more overnight call, had low career satisfaction, and had the highest rates of emotional exhaustion and burnout relative to younger and older counterparts [24]. McAbee et al. discovered no association between career stage and burnout, but did report that those neurosurgeons who were in their early-to-mid-career experienced greater career satisfaction, whereas those who had practiced more than 20 years were less likely to be satisfied, potentially linked to greater administrative duties, less operating room time, or increased personal health issues [10]. Importantly, only 11.5% of our cohort reported <5 years in practice, whereas 23.8% reported 5−15 years and 64.6% reported >15 years in practice. The lower representation of younger surgeons in our cohort may have skewed our measurement of burnout, as early career neurosurgeons may have had more significant changes to their career trajectory during the pandemic due to differences in responsibilities as well as lost operative and clinic time compared to surgeons more advanced in their career. In the future, it will be important to clarify this relationship between career stage and burnout among practicing neurosurgeons, though our study and others suggest that mid- to late- career surgeons may be at particular risk for burnout.
Novel interventions should be investigated to help prevent further burnout in the wake of the pandemic. One report prior to the pandemic tracked numerous resident-level interventions meant to combat burnout, including workout sessions, lectures on wellness, scheduled primary care appointments, and teambuilding exercises [25]. Attending-level interventions have also been described, and include programs involving mindful communication, stress management, and resilience building [7,26,27]. During the pandemic, the Montefiore Medical Center detailed the psychological impact of the pandemic on residents and reported that their department holds daily videoconferences to provide departmental news and to ensure the wellbeing of residents and attendings [28]. These types of initiatives may be needed more than ever as neurosurgical care resumes following the pandemic.
4.5. Study limitations
Our study has several limitations. First, we reported a response rate of 17.7% among attending neurosurgeons. However, our study was conducted over a shorter time frame, namely during the COVID-19 pandemic, which may have contributed to our lower response rate. Furthermore, because survey respondents voluntarily completed the survey, only those who may have had available time during the pandemic may have responded. This may have led us to capture less of a selection of attending neurosurgeons who had higher demands on the job during this period, possibly leading to underreporting of burnout during the pandemic. In addition, fatigue related to increased computer usage during the pandemic and lack of financial incentive for completing the survey may have further contributed to our low response rate. Moreover, we did not ask respondents to the survey to indicate their ABNS board certification status. However, of the 3000 attending neurosurgeons invited to complete the survey, 2270 (86%) are currently ABNS board certified. We therefore approximate that a similar percentage of ABNS board-certified neurosurgeons likely responded to our survey.
Notably, this survey was confined to the membership of the AANS, which may be a potential limitation of our study. In order to prevent duplicate responses while simultaneously gauging the impact of COVID-19 on the U.S. attending neurosurgical community, the AANS was chosen as the sole professional neurosurgical organization to be surveyed in this study. As the AANS constitutes a large proportion of U.S. neurosurgeons, particularly attending neurosurgeons, we hypothesize that confining our survey respondents to the AANS membership would introduce limited bias to this study.
5. Conclusions
Our study demonstrates that uncertainty surrounding the pandemic in terms of healthcare policy reform and compensation changes are highly associated with burnout, and characterizing these changes in the coming months may aid in reducing burnout among attending neurosurgeons. To allow for healthy transitioning of neurosurgical attendings back to patient care, interventions must be implemented to decrease the risk of physician burnout. Above all, it is clear that we must support our colleagues during this challenging time as we transition back to caring for patients in the COVID era and beyond.
Reporting guidelines
We found no applicable reporting guidelines that would apply to this article. By following the EQUATOR reporting guidelines decision tree, (http://www.equator-network.org/wp-content/uploads/2013/11/20160226-RG-decision-tree-for-Wizard-CC-BY-26-February-2016.pdf), we found that none of the most popular checklists are appropriate for our study design.
The content in this manuscript has not been published or submitted for publication elsewhere. All authors have contributed significantly, and are in agreement with the content of the manuscript.
Disclosure of funding
The authors received no financial support for the research, authorship, and/or publication of this article.
CRediT authorship contribution statement
Adham M. Khalafallah: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - review & editing. Shravika Lam: Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Abhishek Gami: Investigation, Writing - original draft, Writing - review & editing. David L. Dornbos: Writing - review & editing. Walavan Sivakumar: Writing - review & editing. Jeremiah N. Johnson: Writing - review & editing. Debraj Mukherjee: Conceptualization, Supervision, Writing - review & editing.
Declaration of Competing Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Acknowledgments
We thank the AANS Young Neurosurgeons Committee and the AANS administration for their collaboration in developing and distributing the survey. We would also like to thank the AANS attending physician participants for taking the time to complete the surveys, as well as for their thoughtful free text survey responses.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.clineuro.2020.106193.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Pennington Z., Lubelski D., Khalafallah A.M., et al. Changes to neurosurgery resident education since onset of the COVID-19 pandemic. World Neurosurg. 2020;(May) doi: 10.1016/j.wneu.2020.05.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khalafallah A.M., Jimenez A.E., Lee R.P., et al. Impact of COVID-19 on an academic neurosurgery department: the johns hopkins experience. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.05.167. Published online May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Theofanis T.N., Khanna O., Stefanelli A., et al. Letter: neurosurgery residency in the COVID-19 era: experiences and insights from thomas jefferson university hospital, Philadelphia, Pennsylvania. Neurosurgery. 2020;2020 doi: 10.1093/neuros/nyaa211. 0(0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai J., Ma S., Wang Y., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rossi R., Socci V., Pacitti F., et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prevention C for DC and P. Cases in the U.S. | CDC. Accessed June 19, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
- 7.Panagioti M., Panagopoulou E., Bower P., et al. Controlled interventions to reduce burnout in physicians a systematic review and meta-analysis. JAMA Intern. Med. 2017;177(2):195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 8.Dyrbye L.N., West C.P., Satele D., et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general u.s. population. Acad. Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 9.Shakir H.J., McPheeters M.J., Shallwani H., Pittari J.E., Reynolds R.M. The prevalence of burnout among US neurosurgery residents. Clin. Neurosurg. 2018;83(3):582–590. doi: 10.1093/neuros/nyx494. [DOI] [PubMed] [Google Scholar]
- 10.McAbee J.H., Ragel B.T., McCartney S., et al. Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J. Neurosurg. 2015;123(1):161–173. doi: 10.3171/2014.12.JNS141348. [DOI] [PubMed] [Google Scholar]
- 11.Klimo P., Decuypere M., Ragel B.T., McCartney S., Couldwell W.T., Boop F.A. Career satisfaction and burnout among U.S. neurosurgeons: a feasibility and pilot study. World Neurosurg. 2013;80(5):e59–e68. doi: 10.1016/j.wneu.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 12.McManus I.C., Winder B.C., Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet. 2002;359(9323):2089–2090. doi: 10.1016/S0140-6736(02)08915-8. [DOI] [PubMed] [Google Scholar]
- 13.McManus I.C., Keeling A., Paice E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: a twelve year longitudinal study of UK medical graduates. BMC Med. 2004;2(1):29. doi: 10.1186/1741-7015-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu J., Gao J., Chen J., Sun Y. Academic versus non-academic neurosurgeons in China: a national cross-sectional study on workload, burnout and engagement. BMJ Open. 2019;9(10):1–9. doi: 10.1136/bmjopen-2018-028309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rotenstein L.S., Torre M., Ramos M.A., et al. Prevalence of burnout among physicians a systematic review. JAMA – J. Am. Med. Assoc. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nepogodiev D., Bhangu A. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020 doi: 10.1002/bjs.11746. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: adaptation under fire: two harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery. 2020:1–5. doi: 10.1093/neuros/nyaa146. 0(0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bambakidis N.C., Tomei K.L. Editorial. Impact of COVID-19 on neurosurgery resident training and education. J. Neurosurg. 2020:1–2. doi: 10.3171/2020.3.jns20965. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsermoulas G., Zisakis A., Flint G., Belli A. Challenges to neurosurgery during the coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 2020;139:519–525. doi: 10.1016/j.wneu.2020.05.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Act A. Coronavirus Aid, Relief, and Economic Security Act, H.R. 748, 116th Cong., 2nd Sess. 2020. [Google Scholar]
- 21.Hsiao J., Sayles E., Antzoulatos E., et al. Effect of COVID-19 on emergent stroke care: a regional experience. Stroke. 2020 doi: 10.1161/STROKEAHA.120.030499. Published online July 8 STROKEAHA120030499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwarz V., Mahfoud F., Lauder L., et al. Decline of emergency admissions for cardiovascular and cerebrovascular events after the outbreak of COVID-19. Clin. Res. Cardiol. 2020 doi: 10.1007/s00392-020-01688-9. Published online August 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shakir H.J., Cappuzzo J.M., Shallwani H., et al. Relationship of grit and resilience to burnout among U.S. Neurosurgery residents. World Neurosurg. 2020;134:e224–e236. doi: 10.1016/j.wneu.2019.10.043. [DOI] [PubMed] [Google Scholar]
- 24.Dyrbye L.N., Varkey P., Boone S.L., Satele D.V., Sloan J.A., Shanafelt T.D. Physician satisfaction and burnout at different career stages. Mayo Clin. Proc. 2013;88(12):1358–1367. doi: 10.1016/j.mayocp.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 25.Wolfe S.Q., West J.L., Hunt M.A., et al. A comparison of the existing wellness programs in neurosurgery and institution champion’s perspectives. Neurosurgery. 2019;84(5):1149–1155. doi: 10.1093/neuros/nyy418. [DOI] [PubMed] [Google Scholar]
- 26.West C.P., Dyrbye L.N., Shanafelt T.D. Physician burnout: contributors, consequences and solutions. J. Intern. Med. 2018;283(6):516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 27.Sotile W.M., Simonds G.R. The thriving neurosurgeon. World Neurosurg. 2019;125:532–533. doi: 10.1016/j.wneu.2019.02.088. [DOI] [PubMed] [Google Scholar]
- 28.Ammar A., Stock A.D., Holland R., Gelfand Y., Altschul D. Managing a specialty service during the COVID-19 crisis: lessons from a New York City health system. Acad. Med. 2020:1–4. doi: 10.1097/ACM.0000000000003440. XX(X) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


