Abstract
Background
The occurrence of large-vessel occlusion in young patients with coronavirus disease 2019 (COVID-19) infection has been exceedingly rare. An extensive review of reported studies revealed a few reported cases. In the present report, we have described the clinical presentation, radiological findings, and outcome of large-vessel occlusion in a young patient with COVID-19 and reviewed the pertinent reported data on this condition.
Case Description
A 31-year-old woman was in her usual state of health until she had presented with a 3-day history of right-sided weakness, slurred speech, and decreased vision. The patient had been taken to several hospitals where she had been treated conservatively with analgesics and discharged. Shortly thereafter, her weakness had become progressive. She had become severely dysarthric and unresponsive. On arrival to the emergency department, her physical examination revealed that she was stuporous, with a Glasgow coma scale of 10 (eye response, 3; verbal response, 2; motor response, 5). The National Institutes of Health Stroke Scale score was 19 on presentation. Brain computed tomography and computed tomography venography revealed an occluded left internal carotid artery and left middle cerebral artery with subacute left middle cerebral artery territory infarction and midline shift. Computed tomography angiography revealed complete occlusion of the left common carotid artery. An emergent decompressive craniectomy was successfully performed. The patient was shifted to the intensive care unit. She was later found to be positive for COVID-19.
Conclusions
Although rare, patients with COVID-19 can present with large-vessel occlusion. Prompt identification of COVID-19–related coagulopathy is essential to assess young patients with clinical manifestations of infarction.
Key words: Common carotid artery, Coronavirus, COVID-19, Thrombotic, Virus, Young
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019
Introduction
The involvement of the central nervous system in coronavirus disease 2019 (COVID-19) infection has varied.1 The neurological manifestations of COVID-19 have included, but are not limited to, headache, altered levels of consciousness, and cerebrovascular disease.1 COVID-19 infection has been associated with a prothrombotic state, leading to cerebrovascular involvement.2 Subsequently, acute cerebrovascular disease can be the presenting symptom of COVID-19 in the absence of vascular disease.2
The development of infarction in patients with COVID-19 infection has been extremely rare. A review of the reported data revealed a few reported cases. Considering the rarity of large-vessel occlusion in young patients with COVID-19, we have outlined the clinical presentation, radiological findings, surgical intervention, and outcome of large-vessel infarction in a 31-year-old woman with COVID-19 and reviewed the pertinent reported data on this condition.
Case Description
Clinical Data
A 31-year-old woman, with hypertension and epilepsy, was in her usual state of health until she had presented with a 3-day history of right-sided weakness, slurred speech, and decreased vision. These symptoms fluctuated throughout the day and were associated with generalized fatigability, headache, and somnolence. The patient was taken to several hospitals where she had been treated conservatively with analgesics and discharged. However, during those 3 days, her right-sided weakness had worsened, she had become severely dysarthric, and she had decreased responsiveness. Thus, the patient was brought to our emergency department. She had no history of traumatic events, previous intracranial hemorrhage, bleeding disorders, rheumatologic and/or autoimmune diseases, or recurrent miscarriage.
On arrival to the emergency department, her physical examination revealed she was vitally stable but stuporous with a Glasgow coma scale of 10 (eye response, 3; verbal response, 2; motor response, 5). Her pupils were 3 mm bilaterally and reactive to light, with no gaze preference. The patient had a right-sided facial droop. Her left upper and lower limbs were localized to pain. She had no movement in her right upper and lower limbs. The National Institutes of Health Stroke Scale score was 19 on presentation to the emergency department.
Radiological Imaging Findings
A brain computed tomography scan showed large left middle cerebral artery territory hypodensity causing a mass effect and ipsilateral lateral ventricle compression and midline shift to the right of ~0.5 cm, representing subacute infarction (Figure 1 ). A computed tomography venogram revealed the absence of contrast opacification of the left internal carotid artery and M1 and A1 segments, and complete occlusion of the left common carotid artery from the origin at the aortic arch (Figure 2 ).
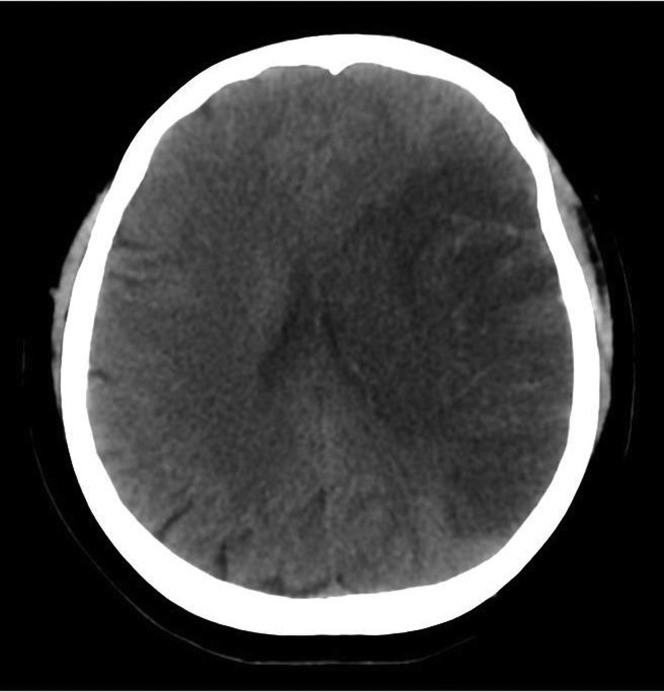
Figure 1.
Baseline non–contrast-enhanced axial computed tomography scan of the patient's head demonstrating a subacute large left middle cerebral middle cerebral artery territory infarct with a mass effect and mild midline shift.
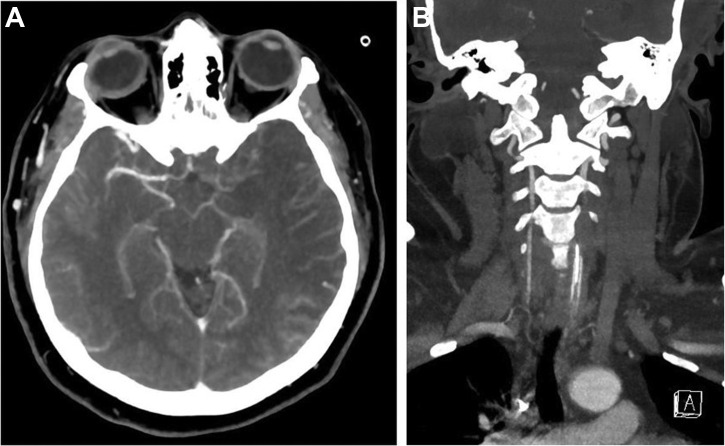
Figure 2.
(A) Computed tomography venogram demonstrating the absence of contrast opacification in the left internal carotid artery and M1 and A1 segments consistent with occlusion. The major venous sinuses were patent. (B) Subsequent computed tomography angiogram showing complete occlusion of the left common carotid artery from the origin at the aortic arch.
Surgical Intervention
The decision was made to perform emergent decompressive craniectomy, anticipating the worsening mass effect and midline shift. The decompressive craniectomy, which involved storing the bone flap in an abdominal subcutaneous pocket, was successfully performed (Figure 3 ). The patient was kept intubated and moved to the intensive care unit.
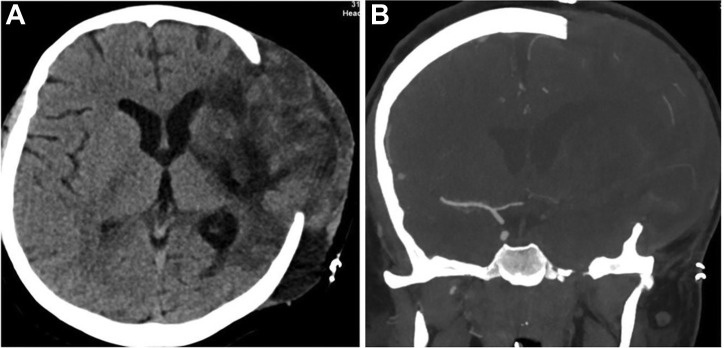
Figure 3.
(A) Non–contrast-enhanced axial computed tomography scan of the head demonstrating an evolving left middle cerebral artery territory infarction and improvement of the mass effect post decompressive craniectomy. (B) Coronal computed tomography angiogram showing persistent occlusion of the intracranial left internal carotid artery.
Outcome and Follow-Up
Postoperatively, the patient was tested for COVID-19, and the result was positive. Thus, the patient was kept in droplet isolation, in addition to contact isolation. All protocols from the infection and prevention control department were performed. Because the patient had an unremarkable medical history, except for hypertension, all investigations were performed to exclude the possible causes of infarction. The autoimmune workup findings revealed an erythrocyte sedimentation rate of 83 mm/hour (reference range, 0–20 mm/hour), C-reactive protein of 157 mg/L (reference range, <8 mg/L), anti–double-stranded DNA of 24 IU/mL, vitamin B12 of 134 pmol/L (reference range, 138–652 pmol/L), thyroid-stimulating hormone of 0.89 mIU/L (reference range, 0.35–4.94 mIU/L), and indeterminate lupus anticoagulant levels. Thrombophilia screening revealed a D-dimer of 23 mg/dL (reference range, <0.50 mg/dL), fibrinogen of 3.96 g/L (reference range, 1.5–4.1 g/L), and antithrombin III level of 103.2% (reference range, 75%–125%). Additionally, an echocardiogram showed a grossly normal left ventricle, an ejection fraction of >55%, and an intact transmitral spectral Doppler flow pattern.
Discussion
Large-vessel infarction in young patients with COVID-19 has been rare. A review of the reported studies identified only a few reported cases since the emergence of the COVID-19 pandemic. We have reported an additional case managed at our institution. To the best of our knowledge, the present patient is the youngest to develop a large-vessel occlusion as the presenting feature of COVID-19.
In a previously reported series, most of the reported cases (n = 20; 90.9%) had been diagnosed in males.3 In terms of the vascular territories, stroke involving the anterior circulation was noted in 13 patients (65%) and in the posterior circulation in 6 patients (27.3%).3 In addition, stroke as the initial clinical manifestation of COVID-19 was noted in 18 patients (81.8%).3
It is evident that patients with COVID-19 have a high risk of thromboembolic disease.4 Coagulopathy and dysfunction of endothelial cells have been implicated in contributing to the disease process.5 However, the exact pathophysiological mechanism leading to cerebrovascular disease has remained uncertain.3 Therefore, healthcare providers should keep a high level of suspicion to promptly diagnose any young patient presenting with signs and symptoms of cerebrovascular disease during the COVID-19 pandemic.4 Gunasekaran et al.4 have recommended close neuromonitoring of patients presenting with cerebrovascular disease who have COVID-19. This will allow for further investigations and establishment of an association of thrombotic events in this population.3
Oxley et al.6 recently reported their case series (n = 5) on large-vessel infarction as the initial clinical manifestation of COVID-19 in patients aged <50 years. In addition, during the pandemic, patients might be reluctant to seek medical attention because of social distancing, isolation rules, and concern of going to the hospital. Therefore, it has not been uncommon for the clinical presentation of cerebrovascular disease to be delayed for patients with COVID-19.6
The present patient had had a National Institutes of Health Stroke Scale score of 19, consistent with the occurrence of a moderate to severe stroke. All diagnostic investigations were performed to exclude autoimmune diseases that can cause cerebrovascular disease in young patients. The clinical manifestations of the present case were consistent with previously reported data. However, to the best of our knowledge, our patient is the youngest patient with COVID-19 to present with cerebrovascular disease in the form of a common carotid artery occlusion.
Conclusion
Large-vessel occlusion as the initial presentation of COVID-19 is a rare, but catastrophic, clinical manifestation. Understanding the various neurological manifestations of COVID-19 should be of paramount importance to physicians during the pandemic. Extensive evaluation should be performed to exclude predisposing factors of hypercoagulability. Further studies are required to delineate the pathogenesis of COVID-19–related coagulopathy.
Acknowledgments
The institutional review board at King Abdullah International Medical Research Center, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia, approved the present study.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Liu K., Pan M., Xiao Z., Xu X. Neurological manifestations of the coronavirus (SARS-CoV-2) pandemic 2019-2020. J Neurol Neurosurg Psychiatry. 2020;91:669–670. doi: 10.1136/jnnp-2020-323177. [DOI] [PubMed] [Google Scholar]
- 2.Cavallieri F., Marti A., Fasano A. Prothrombotic state induced by COVID-19 infection as trigger for stroke in young patients: a dangerous association. eNeurologicalSci. 2020;20:100247. doi: 10.1016/j.ensci.2020.100247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan M., Ibrahim R.H., Siddiqi S.A. EXPRESS: COVID-19 and acute ischemic stroke—a case series from Dubai, UAE. Int J Stroke. 2020;15:699–700. doi: 10.1177/1747493020938285. [DOI] [PubMed] [Google Scholar]
- 4.Gunasekaran K., Amoah K., Rajasurya V., Buscher M.G. Stroke in a young COVID-19 patient. QJM. 2020;113:573–574. doi: 10.1093/qjmed/hcaa177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oxley T.J., Mocco J., Majidi S. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]