ABSTRACT
The disease caused by the new coronavirus (SARS-CoV-2), designated COVID-19, emerged in late 2019 in China, in the city of Wuhan (Hubei province), and showed exponential growth in that country. It subsequently spread to all continents, and infection with SARS-CoV-2 is now classified as a pandemic. Given the magnitude achieved, scientific interest in COVID-19 has also grown in the international literature, including its manifestations on imaging studies, particularly on CT. To date, no case series have been published in Brazil. Therefore, our objective was to describe the CT findings in an initial series of 12 patients.
Keywords: Coronavirus infections, Coronavirus, Multidetector computed tomography
RESUMO
A doença causada pelo novo coronavírus (SARS-CoV-2) surgiu no final de 2019 em Wuhan, província de Hubei, na China, e apresentou um crescimento exponencial naquele país, alastrando-se posteriormente para todos os continentes, sendo agora classificada como uma pandemia. Dada a magnitude alcançada, o interesse científico pela doença também tem crescido na literatura mundial, incluindo suas manifestações nos exames de imagem, particularmente na TC. Até o presente momento, não existem séries de casos publicadas no Brasil, motivo pelo qual nosso objetivo foi descrever os achados tomográficos em uma série inicial de doze pacientes.
Descritores: Infecções por coronavirus, Coronavirus, Tomografia computadorizada multidetectores
In late 2019, a new coronavirus-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-was identified as the causative agent of an outbreak of pneumonia in China, in the city of Wuhan (Hubei province). An association was found between the first cases and a local food market that sold live animals, where most of such patients had been on business or visiting.
The spread of the new coronavirus was rapid, resulting in an epidemic, with the main form of transmission being person-to-person, either via the airways or by touching contaminated surfaces and then the eyes, nose, or mouth. The epidemic hit other continents, and the disease was called coronavirus disease 2019 (COVID-19). New cases started being reported in other countries, initially in individuals who had travelled to China and in people who had had contact with them, and outbreaks related to local transmission were subsequently documented. 1 - 4 COVID-19 is currently considered a pandemic.
The spectrum of clinical presentation of COVID-19 is wide, ranging from absence of symptoms to critical disease. Most respiratory infections are mild, but severe or critical forms have been also described, especially in the elderly and individuals with comorbidities, who can present with dyspnea, hypoxemia, extensive pulmonary involvement on imaging studies, respiratory failure, shock, and multiple organ failure. The estimated COVID-19 mortality in China was 2.3%, most cases having occurred in elderly patients or patients with comorbidities (cardiovascular disease, diabetes mellitus, chronic lung disease, hypertension, and cancer). 5 However, the reported mortality rates vary in different populations; in Italy, for example, where the mean age of the affected population is higher, the currently reported mortality rate is approximately 5.8%. 6
The possibility of COVID-19 should be considered in symptomatic patients who, in the past 14 days, have had close contact with a suspected or confirmed case of COVID-19, have been in areas where widespread transmission has been documented, or have had potential exposure due to participation in events or have been in places where cases of COVID-19 have been reported. Among the most commonly reported clinical manifestations of COVID-19 are fever, fatigue, dry cough, anorexia, myalgia, dyspnea, and sputum production. 7
The diagnosis of COVID-19 is confirmed through detection of SARS-CoV-2 RNA by reverse-transcriptase polymerase chain reaction (RT-PCR) from nasopharyngeal or oropharyngeal swab samples. However, if RT-PCR is negative and clinical suspicion is high, the recommendation is that RT-PCR testing be performed again, including on swabs from other respiratory sites. It is also worth highlighting the value of testing for other viruses that can clinically present in a similar way.
Multiple articles have been published reporting CT findings in COVID-19, even in patients with negative RT-PCR results, arousing interest in the role of CT in the current clinical scenario. The American College of Radiology and the Brazilian College of Radiology recommend that chest CT be used in hospitalized patients with pneumonia symptoms and with specific clinical indications for CT; it is important to point out that neither of them recommend using CT for screening of COVID-19 or as the test of choice for diagnosing COVID-19. 8 , 9
Chest CT can help in the diagnosis of COVID-19, but it cannot confirm or exclude it alone. When RT-PCR is used as a reference, chest CT has high sensitivity (97%) but low specificity (25%), given the overlap of findings with those of respiratory infections of different etiologies. 10
The most commonly observed CT findings in cases of COVID-19 are pulmonary ground-glass opacities and, occasionally, consolidations, with a predominantly peripheral distribution, sometimes associated with fine reticulation (forming the crazy-paving pattern), vascular thickening, and the reversed halo sign. Central parenchymal involvement or the presence of nodules, cavitation, lymph node enlargement, or pleural effusion are less common. 11 - 13 It has been suggested that the reversed halo sign, described by some authors, indicates that organizing pneumonia might be one of the mechanisms of lung injury. 14 , 15
The objective of the present study was to describe the major CT findings in the first case series of COVID-19 in Brazil. In this initial experience in Brazil, involving the first 12 patients with a confirmed diagnosis of COVID-19 (based on RT-PCR results) who underwent chest CT at our facility, the following CT features were observed: ground-glass opacities, in 12 patients (100%); crazy-paving pattern, in 7 (58%); alveolar consolidation, in 4 (33%); reversed halo sign, in 1 (8%); and pleural effusion, in 1 (8%). Nodules, cavitation, and lymph node enlargement were not identified in our sample.
We observed involvement of both lungs in 11 patients (92%) and a peripheral predominance in 9 patients (75%); the changes affected mainly the lower lobes in 8 patients (67%), were multilobar and relatively diffuse in 3 patients (25%), and predominated in the left lower lobe in 1 patient (8%).
Figure 1 illustrates a typical case and demonstrates the evolution of the findings, whereas Figure 2 demonstrates not only the major changes caused by the disease but also another possible but relatively uncommon finding (small pleural effusion).
Figure 1. Axial images (in A to C) and coronal reconstructions (in D) of chest CT scans of a 44-year-old man with clinical findings suggestive of COVID-19 (fever, sore throat, and frequent dry cough), demonstrating the most commonly described pattern: numerous bilateral multifocal ground-glass opacities, associated with fine reticulation and interlobular septal thickening (crazy-paving pattern), involving various lung lobes and being predominantly peripheral in distribution in the parenchyma and a little more extensive in the posterior regions of the lower lobes. The patient had a positive RT-PCR result for COVID-19 on the day he underwent the first CT scan (images on the left in each pair) and was hospitalized. A second CT scan, which was performed three days later (images on the right in each pair) because he continued to have fever spikes and dry cough, demonstrated an increase in the number and extent of pulmonary opacities.
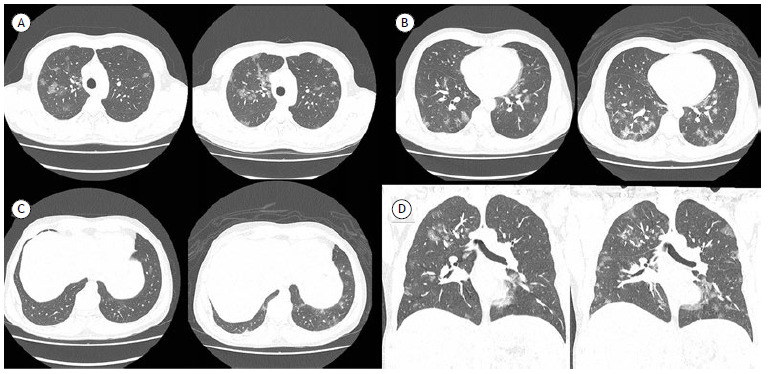
Figure 2. Chest CT scans of different patients illustrating the spectrum of findings of COVID-19 in our sample. In A, a 61-year-old male patient with peripheral and posterior ground-glass opacities in the lower lobes (blue arrows in the right lower lobe), as well as a focus of parenchymal opacification in the lingula. In B and C, a 41-year-old male patient with extensive ground-glass opacities associated with septal thickening and fine reticulation (crazy-paving) in the right upper lobe, in addition to other small scattered foci in the upper and lower left lobes. In D, an 85-year-old male patient with ground-glass opacities, associated with fine reticulation and thickening of some interlobular septa, extending mostly into the periphery of the left lower lobe, but also present in the lingula and in the right lower lobe. In E and F, a 42-year-old male patient with ground-glass opacities and bilateral foci of consolidation, predominantly in the most posterior regions of the lower lobes. The patient also had bilateral minimal pleural effusion (arrows), a relatively uncommon finding in patients with COVID-19. In addition, signs suggestive of hepatic steatosis were identified.

Because the major imaging finding in COVID-19 is ground-glass opacities, chest X-ray plays a less important role in the imaging evaluation of patients, given that the sensitivity of chest X-rays for detecting this type of opacity is low. However, of course, chest X-rays can be useful in monitoring inpatients, including those who are in the ICU, because it is a widely available, rapid, and inexpensive test that enables more frequent (often daily) monitoring of the extent of the pulmonary involvement in the disease.
It has been demonstrated that asymptomatic individuals can present with pulmonary findings (clinical-radiological dissociation), but less frequently than do symptomatic patients and, in general, with less extensive involvement and predominant ground-glass opacities. In contrast, symptomatic patients more commonly present with pulmonary findings, with predominant consolidations and more extensive parenchymal involvement. 16
Despite the variety of presentations, it has generally been reported that, in the first 4 days after symptom onset, the ground-glass opacity pattern predominates. Between days 5 and 8 after symptom onset, there is an increase in the extent of the pulmonary involvement, with the presence of crazy-paving pattern and consolidations. Between days 9 and 13 after symptom onset, when CT findings are usually at their peak, consolidations are noted to predominate; after day 14, the process of consolidation resorption begins and the crazy-paving pattern tends to resolve, although ground-glass opacities may persist. 17 The resolution of the findings is usually relatively slow, taking approximately 30 days, and scarring changes in the lung parenchyma have been described.
The major CT features identified in the first 12 Brazilian patients evaluated at our facility are very similar to those being described in the literature and fundamentally include bilateral multifocal ground-glass opacities, sometimes associated with fine reticulation and septal thickening (crazy-paving pattern), in general involving several lung lobes and being predominantly peripheral in distribution in the parenchyma. The low incidence of pleural effusion and the absence of other findings, such as lymph node enlargement, nodules, and cavitary lesions, are in line with recent international experiences. 10 - 17
The most common CT findings in COVID-19 overlap with those observed in pulmonary infections caused by other agents (particularly other viruses), and, ideally, the definitive diagnosis of COVID-19 should be based on RT-PCR results. Nevertheless, given the magnitude achieved by COVID-19 in recent months, with the disease being classified as a pandemic by the World Health Organization, it is essential that clinicians and radiologists be familiar with the most common imaging presentations of COVID-19, as well as with the expected evolution of the findings, so that they can contribute to earlier identification of cases and thus to reducing the consequences and mortality of the disease.
Footnotes
Financial support: None.
Study carried out by the Grupo de Imagem Cardiotorácica, Departamento de Diagnóstico por Imagem, Hospital Israelita Albert Einstein, São Paulo (SP) Brasil.
REFERENCES
- 1.National Health Commission of the People’s Republic of China . New coronavirus cases rise to 571 in Chinese mainland. Beijing: The Commission; 2020. http://en.nhc.gov.cn/2020-01/23/c_76004 [Google Scholar]
- 2.World Health Organization . Novel Coronavirus - Republic of Korea (ex-China) Geneva: WHO; 2020. https://www.who.int/csr/don/21-january-2020-novel-coronavirus-republic-of-korea-ex-china/en [Google Scholar]
- 3.European Centre for Disease Prevention and Control (ECDC) Geographical distribution of 2019-nCov cases. Solna, Sweden: ECDC; 2020. https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases [Google Scholar]
- 4.Centers for Disease Control and Prevention . 2019 Novel Coronavirus (2019-nCoV) in the US. Atlanta: CDC; 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention [published online ahead of print, 2020 Feb 24] JAMA. 2020 doi: 10.1001/jama.2020.2648. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Grasselli G, Pesenti A, Cecconi M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response [published online ahead of print, 2020 Mar 13] JAMA. 2020 doi: 10.1001/jama.2020.4031. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 7.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China [published online ahead of print, 2020 Feb 7] JAMA. 2020:e201585. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American College of Radiology (ACR) ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection. Reston, VA: ACR; 2020. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection [Google Scholar]
- 9.Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR) Recomendações de uso de métodos de imagem para pacientes suspeitos de infecção pelo COVID-19. São Paulo: CBR; 2020. https://cbr.org.br/wp-content/uploads/2020/03/CBR_Recomenda%C3%A7%C3%B5es-de-uso-de-m%C3%A9todos-de-imagem_16-03-2020.pdf [Google Scholar]
- 10.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases [published online ahead of print, 2020 Feb 26] Radiology. 2020:200642–200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT [published online ahead of print, 2020 Mar 10] Radiology. 2020:200823–200823. doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ng M-Y, Lee EY, Yang J, Yang F, Li X, Wang H, et al. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiol Cardiothorac Imaging. 2020;2(1):e200034. doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV) Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kong W, Agarwal PP. Chest Imaging Appearance of COVID-19 Infection. Radiol Cardiothorac Imaging. 2020;2(1):e200028. doi: 10.1148/ryct.2020200028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Y, Xie YL, Wang X. Longitudinal CT Findings in COVID-19 Pneumonia: Case Presenting Organizing Pneumonia Pattern. Radiol Cardiothorac Imaging. 2020;2(1):e200031. doi: 10.1148/ryct.2020200031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inui S, Fujikawa A, Jitsu M, Kunishima N, Watanabe S, Suzuki Y, et al. Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19) [published online ahead of print, 2020 Mar 17] Radiol Cardiothorac Imaging. 2020;2(2) doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time Course of Lung Changes On Chest CT During Recovery From 2019 Novel Coronavirus (COVID-19) Pneumonia [published online ahead of print, 2020 Feb 13] Radiology. 2020:200370–200370. doi: 10.1148/radiol.2020200370. [DOI] [Google Scholar]


