ABSTRACT
Objective:
To determine the CT findings of multiple cavitary lung lesions that allow the differentiation between benign and malignant etiologies.
Methods:
We reviewed CT scans, including patients with two or more cavitary lung lesions. We evaluated the number of cavitary lesions, their location, cavity wall thickness, and additional findings, correlating the variables with the diagnosis of a benign or malignant lesion.
Results:
We reviewed the chest CT scans of 102 patients, 58 (56.9%) of whom were male. The average age was 50.5 ± 18.0 years. Benign and malignant lesions were diagnosed in 74 (72.6%) and 28 (27.4%) of the patients, respectively. On the CT scans, the mean number of cavities was 3, the mean wall thickness of the largest lesions was 6.0 mm, and the mean diameter of the largest lesions was 27.0 mm. The lesions were predominantly in the upper lobes, especially on the right (in 43.1%). In our comparison of the variables studied, a diagnosis of malignancy was not found to correlate significantly with the wall thickness of the largest cavity, lymph node enlargement, emphysema, consolidation, bronchiectasis, or bronchial obstruction. The presence of centrilobular nodules correlated significantly with the absence of malignant disease (p < 0.05). In contrast, a greater number of cavities correlated significantly with malignancy (p < 0.026).
Conclusions:
A larger number of cavitary lung lesions and the absence of centrilobular nodules may be characteristic of a malignant etiology. However, on the basis of our evaluation of the lesions in our sample, we cannot state that wall thickness is a good indicator of a benign or malignant etiology.
Keywords: Lung neoplasms/diagnosis; Lung diseases/diagnosis; Tomography, X-ray computed; Neoplasms
RESUMO
Objetivo:
Determinar os achados tomográficos de lesões escavadas pulmonares múltiplas que contribuem para a diferenciação entre etiologia benigna e maligna.
Métodos:
Foram revisados exames de TC, sendo incluídos pacientes com duas ou mais lesões pulmonares escavadas. Avaliaram-se a quantidade de lesões escavadas, sua localização, espessura parietal das lesões e achados adicionais, correlacionando as variáveis com a presença de diagnóstico de benignidade ou de malignidade.
Resultados:
Foram revisadas TCs de tórax de 102 pacientes, sendo 58 (56,9%) desses do sexo masculino. A média de idade foi de 50,5 ± 18,0 anos. Lesões benignas e malignas foram diagnosticadas em 74 pacientes (72,6%) e em 28 (27,4%), respectivamente. Quanto aos achados tomográficos, a média do número de cavidades foi 3, a da espessura média da parede da maior lesão foi de 6,0 mm, e a do diâmetro da maior lesão foi de 27,0 mm. Houve predomínio das lesões em lobos superiores, especialmente no direito (43,1%). Após a comparação das variáveis estudadas, a espessura parietal da maior escavação, assim como a presença de linfonodomegalia, enfisema, consolidação, bronquiectasias e obstrução brônquica, não apresentaram diferenças estatisticamente significativas para o diagnóstico de malignidade. A presença de nódulos centrolobulares correlacionou-se significativamente com a ausência de doença maligna (p < 0,05). Observou-se também que um número maior de cavidades se correlacionou significativamente com malignidade (p < 0,026).
Conclusões:
Um maior número de lesões pulmonares escavadas e a ausência de nódulos centrolobulares podem ser características relacionadas à etiologia maligna. Por outro lado, a espessura parietal não permitiu a diferenciação entre etiologia benigna e maligna das lesões em nossa amostra.
Descritores: Neoplasias pulmonares/diagnóstico, Doenças pulmonares/diagnóstico, Tomografia computadorizada por raios X, Neoplasias
INTRODUCTION
The differential diagnosis of multiple cavitary lung lesions is wide-ranging and includes infectious diseases such as tuberculosis, fungal infections, and parasitic infections, as well as noninfectious diseases such as malignant and rheumatic lesions. 1 A cavitary lesion may be caused by various pathological processes, including suppurative necrosis, caseous necrosis, and ischemic necrosis, and is defined as a gas-filled space, evidenced in multislice CT scans as an area of low-grade attenuation within a pulmonary consolidation, mass, or nodule. 2
The imaging characteristics of lesions may increase diagnostic accuracy, especially when the initial clinical findings are indeterminate or inconsistent. 3 , 4 Simple chest X-ray and CT are the most commonly used chest imaging modalities, CT being more widely used and more sensitive in the detection of lung diseases and their characteristics, including shape, dimensions, wall thickness, location, and other aspects. 1 , 3
The objective of the present study was to determine which CT findings of multiple cavitary lung lesions help differentiate between benign and malignant disease, on the basis of etiology.
METHODS
Study population
We retrospectively reviewed 102 consecutive chest CT scans performed at two university hospitals between 2012 and 2017. The search terms “cavitation” and “cavitary lesion” were used in searches of imaging systems and electronic reports (PACS; MV Informática, Recife, Brazil; and PixViewer; Pixeon, São Paulo, Brazil). This cross-sectional analytical study was approved by the Research Ethics Committee of the Santa Casa de Misericórdia in Porto Alegre (CAAE protocol no. 35917214.4.0000.5335).
The study included patients in whom CT scans of the chest showed two or more cavitary lung lesions during the study period. Patients without a defined etiological diagnosis and those with a single cavitary lesion were excluded.
Additional patient data, such as laboratory results, histological reports, and immune status, were obtained from electronic medical records (Tasy; Philips Clinical Informatics, Blumenau, Brazil, and Soul; MV Informática). The criteria for immunosuppression included corticosteroid therapy or chemotherapy in the four weeks prior to a CT scan, a history of organ transplantation, and a diagnosis of AIDS. Definitive diagnoses were obtained through histological study, sputum smear microscopy, or clinical/radiological follow-up. The diagnosis of tuberculosis was based on symptoms suggestive of the disease, a demonstrated response to treatment, and cultures of respiratory secretions testing positive for Mycobacterium tuberculosis, with or without lesion histology that indicated that diagnosis. Pulmonary abscesses were defined by the presence of a clinical history consistent with their diagnosis and the resolution of clinical and radiological findings after antimicrobial therapy, with or without postoperative histological analysis.
CT protocol
The images were obtained using two 64-slice multidetector CT scanners (LightSpeed VCT; GE Healthcare, Waukesha, WI, USA) with the following parameters: tube voltage: 120 kVp; tube current: 250 mA; rotation time: 0.8 s; and pitch: 1.375.
Analysis of images
The CT scans were evaluated by two radiologists with more than 10 years of experience, both of whom were blinded to the clinical status and data regarding the diagnosis of the patients. After independent analysis, the two radiologists reviewed the images with a third thoracic radiologist (with over 30 years of experience), who was likewise blinded, in order to reach a final consensus.
The number of cavitary lesions, their location, the measurement of the two largest lesions on two axes in the axial slice, and the wall thickness at its greatest point were evaluated, as were the dimensions of the largest and second largest lesions. We also evaluated associated findings such as the presence of mediastinal lymph node enlargement, centrilobular nodules, central acinar emphysema, bronchial obstruction, bronchiectasis, and parenchymal consolidation, as well as immunosuppression and the histopathological diagnosis of the lesions.
We acquired the images volumetrically and evaluated them with lung and mediastinal window settings, using specific filters. Measurements were taken in the axial plane with only a lung window setting in order to increase the reproducibility of the results. The characteristics obtained from the CT scans were then correlated with the diagnosis of malignancy.
A nodule was defined as an ill- or well-defined, round or irregularly shaped opacity with a diameter ≤ 3 cm. Mediastinal lymph node enlargement was defined as a lymph node with a short-axis diameter > 10 mm. Cavities were defined as gas-filled spaces, characterized as transparencies or areas of low-grade attenuation within pulmonary consolidations, masses, or nodules. Consolidation was defined as homogeneous opacification of the parenchyma with obscuration of the underlying blood vessels. To define these concepts, the recommendations of the Fleischner Society were used. 2
Statistical analysis
The data are expressed as absolute and relative frequencies, mean ± standard deviation, or median (interquartile range [IQR]). The normality of the data was assessed with the Shapiro-Wilk test. The Mann-Whitney test was used in order to compare the means. The proportions were compared by using the chi-square test. We developed a multivariate statistical model using logistic regression expressed in ORs in relation to the tomographic factors associated with malignancy. Values of p < 0.05 were considered statistically significant for all analyses, which were performed with the IBM SPSS Statistics software, version 22.0 (IBM Corporation, Armonk, NY, USA).
RESULTS
The study sample included 102 patients with at least two cavitary lesions on CT scans of the chest. The mean age was 50.5 ± 18.0 years, and 58 patients (57%) were male.
Benign and malignant lesions were diagnosed in 74 (72.6%) and 28 (27.4%) of the patients, respectively. Among the 74 patients with benign lesions, the diagnosis was tuberculosis in 50 (49.0%); lung abscess in 9 (8.8%); mycetoma in 6 (5.9%); septic embolism in 3 (2.9%); atypical mycobacteriosis in 2 (2.0%); atypical aspergillosis in 2 (2.0%); fusariosis in 1 (1.0%); and granulomatosis with polyangiitis in 1 (1.0%). Of the 28 patients with malignant lesions, 20 (71.4%) were diagnosed with extrapulmonary neoplasms, whereas 8 (28.6%) were diagnosed with pulmonary neoplasms. Table 1 shows the main etiological diagnoses of the lesions.
Table 1. Frequencies of the pathologies associated with multiple cavitary lesions.a .
| Pathologies | (n = 102) |
|---|---|
| Tuberculosis | 50 (49.0) |
| Neoplastic lesions of extrapulmonary origin | 20 (19.6) |
| Bacterial abscess | 9 (8.8) |
| Neoplastic lesions of pulmonary origin | 8 (7.8) |
| Mycetoma | 6 (5.9) |
| Septic embolism | 3 (2.9) |
| Atypical mycobacteriosis | 2 (2.0) |
| Atypical aspergillosis | 2 (2.0) |
| Fusariosis | 1 (1.0) |
| Granulomatosis with polyangiitis | 1 (1.0) |
Values expressed in n (%).
Of the 102 patients in the sample, 17 (16.7%) were immunocompromised. There were no statistically significant differences between the characteristics of the benign lesions and those of the malignant lesions, in the immunocompromised patients or in the immunocompetent patients (p = 0.775 for both).
Regarding the CT findings, the median number of cavities observed was 3 (IQR, 2-6), the median thickness of the largest lesion was 6 mm (IQR, 4-8 mm), and the median diameter of the largest lesion was 27 mm (IQR, 14-43 mm). With respect to the location of the lesions, they were more prevalent in the upper lobes, 44 (43.1%) being observed in the upper right lobe and 23 (22.5%) being observed in the upper left lobe. The most common imaging finding was that of centrilobular nodules, which were observed in slightly more than half of the patients (53.9%), followed by consolidation, lymph node enlargement, bronchiectasis, bronchial obstruction, and emphysema (Table 2).
Table 2. Characteristics of patients in accordance with the type of lesion.
| Parameters | Total | Benign lesions | Malignant lesions | p |
|---|---|---|---|---|
| (n = 102) | (n = 74) | (n = 28) | ||
| Male | 58 (56.9) | 43 (58.1) | 15 (53.6) | 0.680 |
| Age, years | 50 ± 18 | 47 ± 17 | 59 ± 16 | 0.001 |
| Immunosuppression | 17 (16.7) | 13 (17.6) | 4 (14.3) | 0.775 |
| Characteristics of the lesion | ||||
| Number of cavities | 3 (2-6) | 3 (2-6) | 4 (2-9) | 0.122 |
| Wall thickness of the largest lesion, mm | 6 (4-8) | 6 (4-8) | 4 (3-10) | 0.242 |
| Diameter of the largest lesion, mm | 27 (14-43) | 30 (17-48) | 18 (9-39) | 0.024 |
| Location of the largest lesion | < 0.001 | |||
| Upper right lobe | 44 (43.1) | 38 (48.6) | 8 (28.6) | |
| Upper left lobe | 23 (22.5) | 22 (29.7) | 1 (3.6) | |
| Lower right lobe | 16 (15.7) | 5 (6.8) | 11 (39.3) | |
| Lower left lobe | 9 (8.8) | 6 (8.1) | 3 (10.7) | |
| Middle lobe | 6 (5.9) | 2 (2.7) | 4 (14.3) | |
| Lingula | 4 (3.9) | 3 (4.1) | 1 (3.6) | |
| Imaging findings | ||||
| Centrilobular nodule | 55 (53.9) | 48 (64.9) | 7 (25.0) | < 0.001 |
| Consolidation | 43 (42.2) | 39 (52.7) | 4 (14.3) | < 0.001 |
| Emphysema | 15 (14.7) | 12 (16.2) | 3 (10.7) | 0.755 |
| Lymph node enlargement | 42 (41.2) | 30 (40.2) | 12 (42.9) | 0.826 |
| Bronchiectasis | 23 (22.5) | 21 (28.4) | 2 (7.1) | 0.032 |
| Bronchial obstruction | 16 (15.7) | 13 (17.6) | 3 (10.7) | 0.547 |
Values expressed in n (%), mean ± SD, or median (interquartile range).
In the univariate analysis of the variables studied, there were no significant differences between the benign and malignant etiologies in relation to the mean wall thickness of the largest lesion, lymph node enlargement, emphysema, or bronchial obstruction. The presence of a centrilobular nodule correlated significantly with the absence of malignant disease (p <0.05; Table 3).
Table 3. Univariate and multivariate analysis of factors associated with malignity.
| Parameter | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| ORs (95% CI) | p | ORs (95% CI) | p | |
| Male | 1.20 (0.49-2.89) | 0.681 | ||
| Age, years | 1.04 (1.00-1.08) | 0.013 | 1.06 (1.01-1.10) | 0.004 |
| Immunosuppression | 1.27 (0.37-4.34) | 0.693 | ||
| Characteristics of the lesion | ||||
| Number of cavities | 1.13 (1.00-1.27) | 0.036 | 1.25 (1.02-1.52) | 0.026 |
| Wall thickness of the largest lesion, mm | 1.01 (0.88-1.16) | 0.826 | ||
| Diameter of the largest lesion, mm | 0.97 (0.95-0.99) | 0.045 | 0.98 (0.96-1.01) | 0.451 |
| Location of the largest lesion | 0.792 | |||
| Upper right lobe | 1.00 | |||
| Upper left lobe | 0.20 (0.02-1.76) | |||
| Lower right lobe | 9.90 (2.66-36.7) | |||
| Lower left lobe | 2.25 (0.45-11.0) | |||
| Middle lobe | 9.00 (1.38-58.4) | |||
| Lingula | 1.50 (0.13-16.5) | |||
| Imaging findings | ||||
| Centrilobular nodule | 5.53 (2.06-14.8) | 0.001 | 3.64 (1.07-12.2) | 0.037 |
| Consolidation | 6.68 (2.09-21.2) | 0.001 | 1.99 (0.49-8.03) | 0.329 |
| Emphysema | 1.61 (0.41-6.24) | 0.489 | ||
| Lymph node enlargement | 0.90 (0.37-2.20) | 0.833 | ||
| Bronchiectasis | 5.15 (1.11-23.8) | 0.036 | 2.27 (0.40-12.9) | 0.353 |
| Bronchial obstruction | 1.77 (0.46-6.81) | 0.403 | ||
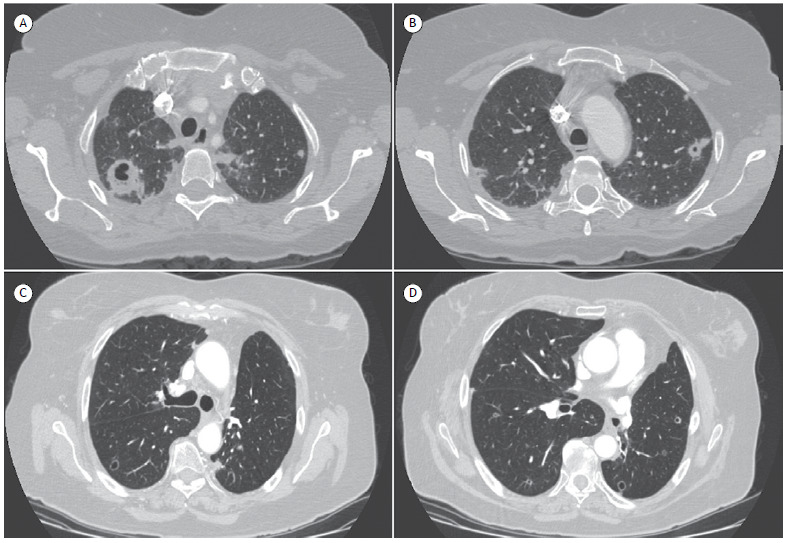
In the multivariate analysis adjusted for age, diameter of the largest lesion, centrilobular nodules, consolidation, and bronchiectasis, a larger number of cavities correlated significantly with malignancy (p < 0.026; Table 3). Figure 1 shows the CT scans of 2 patients with multiple cavitary lesions of benign and malignant etiology, respectively.
Figure 1. Axial CT scans of the chest of a 57-year-old female patient, showing two cavitary lesions with irregular walls and thickened upper lobes (in A and B). The final diagnosis was septic embolism. In C and D, CT scan of the chest of a 70-year-old female patient with multiple cavitary lesions, most of them thin-walled, apart from one thick-walled lesion in the lower left lobe. The final diagnosis was pulmonary metastases of a colorectal neoplasm.
DISCUSSION
In the present study, we showed that a larger number of cavitary lesions is associated with a malignant etiology, and that the presence of centrilobular nodules is associated with a benign etiology. In addition, we found that did not differentiate between benign and malignant lesions did not differ significantly in terms of the wall thickness of the lesion, the diameter of the largest lesion, or the location of the largest lesion. The most common benign pathology (seen in nearly 50% of the cases of benign lesion) was tuberculosis, followed by bacterial abscess, and most of the malignant lesions were extrapulmonary.
Cavitary pulmonary lesions are common in clinical practice and are widely used as a differential in diagnoses based on CT findings, including nonmalignant pathologies such as infectious processes (caused by mycobacteria, fungi, or parasites) and autoimmune diseases, as well as malignant pulmonary and extrapulmonary pathologies. 3 , 4 Clinical findings of a benign pathology can often be similar to findings common in neoplastic lesions, and the results of laboratory tests performed at symptom onset may be normal. Therefore, CT is of great value and contributes to the etiological recognition of pathologies, notably by taking into account the characteristics of lesions. 4 - 7 A previous study 8 described findings that can help differentiate between benign and malignant cavitary lesions; however, that study evaluated a population sample different than ours, in which granulomatous lesions (tuberculosis) were quite common.
Various authors have demonstrated the importance of the characteristics of cavitary lesions, together with clinical findings and imaging results, in the differential diagnosis. 1 , 4 , 9 Woodring et al. 9 , 10 found that a cutoff point for wall thickness of > 15 mm was suggestive of a malignant lesion in X-rays, whereas Nin et al. 3 defined a cutoff point of > 24 mm for CT. In our study, the average wall thickness was 6 mm, and there were no statistical differences between benign and malignant lesions, which is similar to results reported previously in the literature. 8 One of the likely causes of there being such a large difference in wall thickness measurements is that the aforementioned studies 3 , 9 , 10 evaluated single pulmonary lesions, rather than multiple lesions as in our study. There were also variations in other aspects, such as the systemic conditions and pathophysiology of the formation of the lesions. It is of note that even thin-walled lesions can be related to a malignant etiology. 11
In the present study, we observed a higher probability of malignancy in cases with a greater number of cavitary lesions, the multivariate analysis having been adjusted for age, diameter of the largest lesion, average wall thickness of the largest lesion, presence of centrilobular nodules, consolidation, and bronchiectasis. However, this is a finding that should be evaluated with caution, because, among other reasons, and as has been demonstrated in various studies, 1 , 3 malignant lesions, including secondary implants, may present as a single lesion or even as dozens of lesions.
The presence of centrilobular nodules was associated with a higher probability of nonmalignant etiology. This finding is in accordance with data in the literature, because centrilobular nodules are more commonly found in patients with mycobacteriosis, 12 as well as in those with infection caused by bacteria, fungi, parasites, or viruses, 13 , 14 than in those with malignant lesions. 8
Our study has some limitations. First, given the retrospective nature of the study, we could not include all clinical and laboratory variables, because of the inconsistency of the collected data. Second, the profile of patients at a tertiary care hospital is not the same as that of outpatients in the community, which restricts to an extent the generalizability of the findings to the general population.
In conclusion, the present study demonstrated two characteristics of cavitary lesions on CT scans of the chest that may contribute to the etiological differentiation between benign and malignant lesions. A greater number of cavitary lesions and the absence of centrilobular nodules were associated with a higher probability of malignancy. However, the parameters wall thickness and location of the lesions were not capable of differentiating between benign and malignant lesions.
Footnotes
Financial support: None.
Study carried out in the Laboratório de Pesquisa em Imagens Médicas - LABIMED - Departamento de Radiologia, Pavilhão Pereira Filho, Irmandade Santa Casa de Misericórdia de Porto Alegre, Porto Alegre (RS) Brasil.
REFERENCES
- 1.Hansell DM, Bankier AA, McMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 2.Gadkowski LB, Stout JE. Cavitary Pulmonary Disease. Clin Microbiol Rev. 2008;21(2):305–333. doi: 10.1128/CMR.00060-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nin CS, de Souza VV, Alves GR, do Amaral RH, Irion KL, Marchiori E. Solitary lung cavities CT findings in malignant and non-malignant disease. Clin Radiol. 2016;71(11):1132–1136. doi: 10.1016/j.crad.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Parkar A, Kandiah P. Differential Diagnosis of Cavitary Lung Lesions. J Belg Soc Radiol. 2016;100(1):100–100. doi: 10.5334/jbr-btr.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker CM, Abbott GF, Greene RE, Shepard JA, Vummidi D, Digumarthy SR. Imaging pulmonary infection classic signs and patterns. AJR Am J Roentgenol. 2014;202(3):479–492. doi: 10.2214/AJR.13.11463. [DOI] [PubMed] [Google Scholar]
- 6.Vourtsi A, Gouliamos A, Moulopoulos L, Papacharalampous X, Chatjiioannou A, Kehagias D. CT appearance of solitary and multiple cystic and cavitary lung lesions. Eur Radiol. 2001;11(4):612–622. doi: 10.1007/s003300000583. [DOI] [PubMed] [Google Scholar]
- 7.Li BG, Ma DQ, Xian ZY, Guan J, Luo KJ, Fan QW. The value of multislice spiral CT features of cavitary walls in differentiating between peripheral lung cancer cavities and single pulmonary tuberculous thick-walled cavities. Br J Radiol. 2012;85(1010):147–152. doi: 10.1259/bjr/79051309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Honda O, Tsubamoto M, Inoue A, Johkoh T, Tomiyama N, Hamada S. Pulmonary cavitary nodules on computed tomography differentiation of malignancy and benignancy. J Comput Assist Tomogr. 2007;31(6):943–949. doi: 10.1097/RCT.0b013e3180415e20. [DOI] [PubMed] [Google Scholar]
- 9.Woodring JH, Fried AM, Chuang VP. Solitary cavities of the lung diagnostic implications of cavity wall thickness. AJR Am J Roentgenol. 1980;135(6):1269–1271. doi: 10.2214/ajr.135.6.1269. [DOI] [PubMed] [Google Scholar]
- 10.Woodring JH, Fried AM. Significance of wall thickness in solitary cavities of the lung a follow-up study. AJR Am J Roentgenol. 1983;140(3):473–474. doi: 10.2214/ajr.140.3.473. [DOI] [PubMed] [Google Scholar]
- 11.Guo J, Liang C, Sun Y, Zhou N, Liu Y, Chu X. Lung cancer presenting as thin-walled cysts An analysis of 15 cases and review of literature. Asia Pac J Clin Oncol. 2016;12(1):e105–e112. doi: 10.1111/ajco.12126. [DOI] [PubMed] [Google Scholar]
- 12.Burrill J, Williams CJ, Bain G, Conder G, Hine AL, Misra RR. Tuberculosis a radiological review. Radiographics. 2007;27(5):1255–1273. doi: 10.1148/rg.275065176. [DOI] [PubMed] [Google Scholar]
- 13.Rossi SE, Franquet T, Volpacchio M, Giménez A, Aguilar G. Tree-in-bud pattern at thin-section CT of the lungs radiologic-pathologic overview. Radiographics. 2005;25(3):789–801. doi: 10.1148/rg.253045115. [DOI] [PubMed] [Google Scholar]
- 14.Collins J, Blankenbaker D, Stern EJ. CT patterns of bronchiolar disease what is "tree-in-bud"? AJR Am. J Roentgenol. 1998;171(2):365–370. doi: 10.2214/ajr.171.2.9694453. [DOI] [PubMed] [Google Scholar]


