Abstract
Since coronavirus disease 2019 (COVID-19) might circulate in the following seasons, it is essential to understand how COVID-19 influences other respiratory diseases, especially influenza. In this study, we analyzed the influenza activity from mid-November 2019 to March 2020 in Chinese mainland and found that the influenza season ended much earlier than previous seasons for all subtypes and lineages, which may have resulted from the circulation of COVID-19 and measures such as travel control and personal protection. These findings provide rudimentary knowledge of the co-circulation patterns of the two types of viruses.
Keywords: COVID-19, Chinese mainland, Influenza, Biosafety measures
Coronavirus disease 2019 (COVID-19) has been prevalent in China since the end of 2019 [1]. By May 19, 2020, COVID-19 had spread worldwide, with a total of almost five million confirmed cases [2]. During the spread of the SARS-CoV-2 virus in China, the Chinese Government established several measures to prevent the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), such as the establishment of a cordon sanitaire in Hubei Province, strict controls on travel, the quarantine of suspected cases and those in contact with confirmed cases [3]. Chinese people have also taken measures such as wearing a mask, washing hands frequently, and maintaining social distancing. Those interventions have been suggested useful in mitigating the spread of COVID-19 [4,5]. How this COVID-19 outbreak and the related unprecedented measures influence other infectious diseases, such as influenza, remains unknown. In this work, we collected the influenza-positive rate from the tested ILI cases in China in the 2019–2020 influenza season and compared the results with those from previous influenza seasons to evaluate how COVID-19 and the following measures influenced influenza activity.
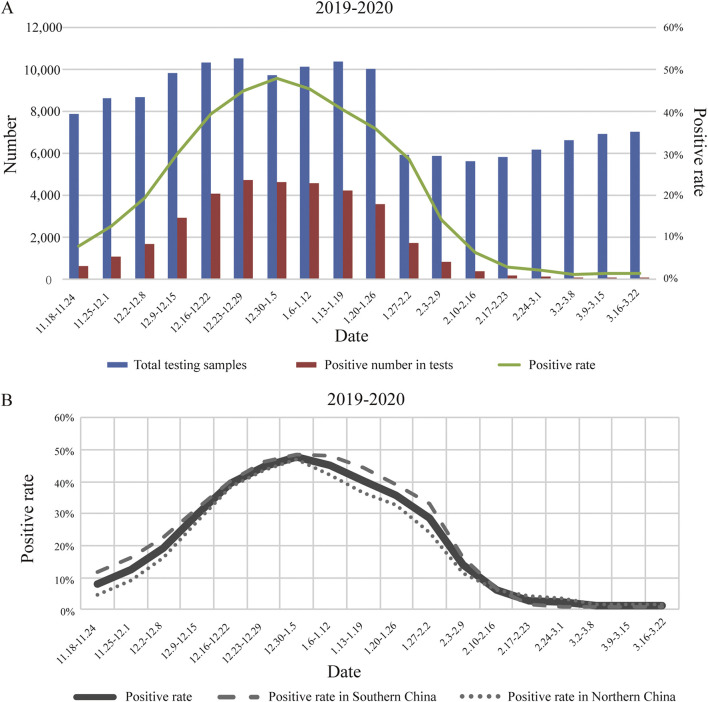
We collected surveillance data from the Chinese National Influenza Center website [6], including all the testing samples and the number of influenza-positive samples (Fig. 1A). The total sample number decreased sharply since late January, which may have been due to the great need for COVID-19 testing. The overall positive number gradually reduced from the beginning of January and reached a shallow level in March. To fairly evaluate the prevalence of influenza, we mapped the positive rate, as shown in Fig. 1A with a green line. The positive rate decreased from the beginning of 2020, approaching zero in March. We further calculated the positive rates for Southern and Northern China separately, as shown in Fig. 1B, to have found similar decreasing trends.
Fig. 1.
Influenza activity in the 2019–2020 epidemic season.
(A) All testing samples and the number of influenza-positive samples from mid-November 2019 to mid-March 2020 in China are shown with blue and red bars. The positive rate is shown with a green line. (B) The positive rates for Chinese mainland, Southern China and Northern China are shown with full lines, dashed lines and dotted lines, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
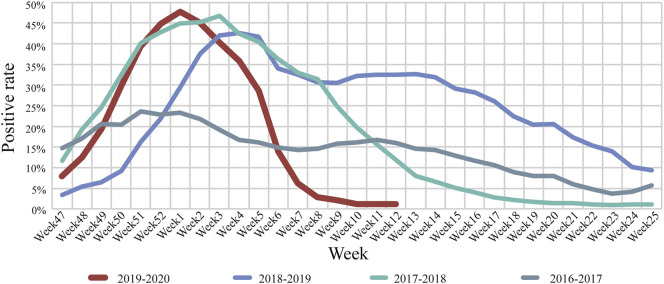
To evaluate the difference between regular influenza seasons and the influenza season under the COVID-19 outbreak, we collected surveillance data of 2016–2017, 2017–2018, and 2018–2019 seasons from the Chinese National Influenza Center website [6]. After mapping the positive rates during these influenza seasons in Fig. 2 , it was apparent that the positive rate decreased much earlier in the 2019–2020 season than in the previous three seasons. In week 7 of 2020, the positive rate was already below 10%, while for 2016–2017, 2017–2018, and 2018–2019 seasons, the positive rates decreased to below 10% at weeks 18, 13, and 25.
Fig. 2.
Positive rates of influenza in recent influenza seasons in Chinese mainland.
The influenza-positive rates in Chinese mainland during the 2016–2017, 2017–2018, 2018–2019 and 2019–2020 influenza seasons.
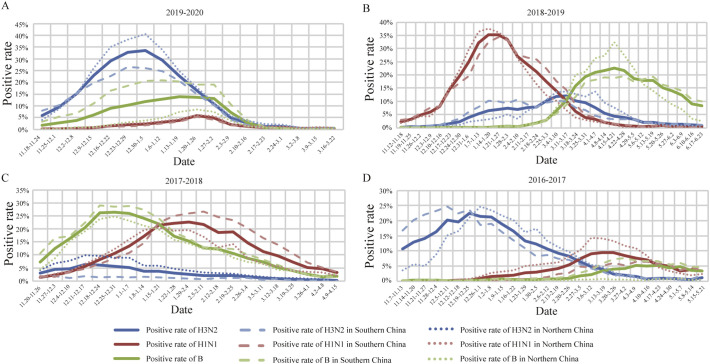
Additionally, we mapped the positive rate for subtypes H3N2, H1N1, and lineage B (Fig. 3A). Subtype H3N2 predominated from the end of 2019 to the beginning of 2020, then it rapidly decreased, beginning in the second week (Jan. 6-Jan. 12, 2020) and dropped to less than 5% by week 6. Subtype H1N1 and lineage B were at low levels during the 2019–2020 flu season and declined approximately one month later than H3N2. In Southern China, subtype H3N2 and lineage B predominated, and the positive rate of H3N2 was higher than that of lineage B from November 2019 to mid-January 2020. Then, beginning in late January 2020, lineage B dominated and declined to start in February. In Northern China, subtype H3N2 dominated in the 2019–2020 flu season and tended to start at the beginning of the year, and subtype H1N1 and lineage B were at shallow levels and declined to start in February. In the 2018–2019 influenza season (Fig. 3B), H1N1 predominated from November 2018 to early March 2019. After H1N1 declined to a low level, influenza B arose and predominated beginning in late March and declined to be below 10% in June. Influenza H3N2 was also mild in China during this season. In the 2017–2018 influenza season (Fig. 3C), lineage B arose quickly in the beginning, while H1N1 exceeded and became predominant beginning in late January 2018. H3N2 was mild in the 2017–2018 season, with a positive rate of no more than 10% in both Southern and Northern China. In the 2016–2017 influenza season (Fig. 3D), H3N2 predominated from the beginning to late February. After H3N2 declined to a low level, H1N1 exhibited a slight increase (mainly in Northern China) and dropped soon after.
Fig. 3.
Positive rates of different lineages in recent influenza seasons in Chinese mainland.
The positive rates of subtype H3N2, H1N1 and lineage B during the 2019–2020 (A), 2018–2019 (B), 2017–2018 (C) and 2016–2017 (D) influenza seasons are shown with blue, red and green lines, respectively. Meanwhile, the positive rates for Southern China and Northern China are shown with dashed lines and dotted lines, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
In conclusion, we have found that the influenza season ended much earlier in 2020 than in previous years. According to the China CDC Weekly Report [7], the confirmed cases (by date of symptom onset) of COVID-19 outside Hubei mainly arose starting in January. They reached a peak on January 27th, which is consistent with a recent work that considered different versions of the case definition [8], and this peak occurred soon after the cordon sanitaire was imposed in Wuhan city. For influenza, we observed a significant decline in the total testing samples for influenza beginning in late January, which may be due to the increased testing capacity for COVID-19. The positive rate somehow reflected the severity of influenza, which reached a peak in the first week of 2020 and then decreased. The positive rate for influenza exhibited a sharp decrease after interventions for COVID-19 were imposed in late January and reached a shallow level within several weeks. A similar phenomenon for influenza was also observed in Chinese Taiwan and Singapore [[9], [10]]. For the past three seasons, after the positive rate reached its peak, there was possibly a slight decrease, but it remained at a high level for a relatively long time.
The decrease in the influenza-positive rate at the beginning of 2020 may be due to the COVID-19 outbreak or other reasons, such as the environment [11,12] and the high level of herd immunity to influenza H3N2 viruses (since the positive rate always decreased when a subtype/lineage reached a relatively high level). Since January 23rd, China has undertaken public health interventions, the cordon sanitaire, and controls on travel, which also limited the transmission of influenza between districts. Meanwhile, the Chinese people are taking self-protection measures such as wearing masks, washing hands frequently, and staying at home. These prophylactic measures also significantly reduced the transmission of influenza and made this flu season reach a low status much earlier than regular seasons.
Some previous studies have focused on the theory of the interactions between different viruses [13,14]. Due to data limitations, we could not infer how the circulation of COVID-19 influenced influenza transmission in detail. Still, it is worth studying since they might co-circulate in the coming seasons. For influenza, once a lineage/subtype reaches the peak and then declines, the other lineage/subtype might soon arise. Whether there will be a similar phenomenon for the co-circulation of influenza and COVID-19 remains unknown.
As COVID-19 seems unlikely to disappear and might circulate with influenza in the following years, biosafety measures, including self-protection and public governance, will likely be taken for a long time and may change the circulation characteristics of seasonal influenza. For example, a low positive rate and early ending (and possibly a late start) of influenza seasons may occur, which may lead to reduced mortality, social and financial losses.
Acknowledgments
Acknowledgements
This work was supported by CAMS Initiative for Innovative Medicine (grant number 2016-I2M-1-005), National Natural Science Foundation of China (grant number 31671371, 31600750), and Central Public-Interest Scientific Institution Basal Research Fund (grant number 2017PT31026, 2018PT31016). We thank the Chinese National Influenza Surveillance Network for contributing to influenza epidemiological and laboratory surveillance. We thank Dr. Jing Meng for linguistic assistance during the preparation of this manuscript.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Author contributions
Mi Liu: Formal analysis, Data curation, Writing - original draft, Funding acquisition. Lizong Deng: Formal analysis, Writing - review & editing. Dayan Wang: Conceptualization. Taijiao Jiang: Conceptualization, Writing - review & editing, Funding acquisition.
References
- 1.Wang R., Zhang X., Irwin D.M., Shen Y. Emergence of SARS-like coronavirus poses a new challenge in China. J. Inf. Secur. 2020;80(3):350–371. doi: 10.1016/j.jinf.2020.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2020. Coronavirus disease (COVID-19) Situation Dashboard.https://www.who.int/redirect-pages/page/novel-coronavirus-(COVID-19)-situation-dashboard (accessed 19 May 2020) [Google Scholar]
- 3.Chen S., Yang J., Yang W., Wang C., Bärnighausen T. COVID-19 control in China during mass population movements at new year. Lancet. 2020;395(10226):764–766. doi: 10.1016/s0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kraemer M.U.G., Yang C.H., Gutierrez B., Wu C.H., Klein B., Pigott D.M., et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.H., McDevitt J.J., Hau B.J.P., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26(5):676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chinese National Influenza Center Influenza Weekly Report. 2020. http://www.chinaivdc.cn/cnic/zyzx/lgzb/ (accessed 2 April 2020)
- 7.The novel coronavirus pneumonia emergency response epidemiology team Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Weekly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- 8.Tsang T.K., Wu P., Lin Y., Lau E.H.Y., Leung G.M., Cowling B.J. Effect of changing case definitions for COVID-19 on the epidemic curve and transmission parameters in mainland China: a modelling study. Lancet Public Health. 2020;5(5) doi: 10.1016/s2468-2667(20)30089-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuo S.C., Shih S.M., Chien L.H., Hsiung C.A. Collateral benefit of COVID-19 control measures on influenza activity, Taiwan. Emerg. Infect. Dis. 2020;26(8):1928–1930. doi: 10.3201/eid2608.201192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soo R.J.J., Chiew C.J., Ma S., Pung R., Lee V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg. Infect. Dis. 2020;26(8):1933–1935. doi: 10.3201/eid2608.201229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dowell S.F. Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg. Infect. Dis. 2001;7(3):369–374. doi: 10.3201/eid0703.010301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sloan C., Moore M.L., Hartert T. Impact of pollution, climate, and sociodemographic factors on spatiotemporal dynamics of seasonal respiratory viruses. Clin. Transl. Sci. 2011;4(1):48–54. doi: 10.1111/j.1752-8062.2010.00257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DaPalma T., Doonan B.P., Trager N.M., Kasman L.M. A systematic approach to virus-virus interactions. Virus Res. 2010;149(1):1–9. doi: 10.1016/j.virusres.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Díaz-Muñoz S.L. Uncovering virus-virus interactions by unifying approaches and harnessing high-throughput tools. mSystems. 2019;4(3) doi: 10.1128/mSystems.00121-19. [DOI] [PMC free article] [PubMed] [Google Scholar]