Dear Editor,
We read the recent article published in KJR titled “Prediction of the Development of Pulmonary Fibrosis Using Serial Thin-Section CT and Clinical Features in Patients Discharged after Treatment for COVID-19 Pneumonia” with great interest (1). The authors assessed the predictors of pulmonary fibrosis using clinical data and followup chest computed tomography (CT) in patients with coronavirus disease (COVID-19) pneumonia (1). The most common CT findings in COVID-19 pneumonia have been described as ground-glass opacities (GGOs) with or without consolidation, crazy-paving pattern, interstitial thickening, irregular interface, and parenchymal band mainly bilateral and lower lobes predilection with peripheral locations (1). Authors found evidence of fibrosis, i.e., irregular interface and parenchymal bands, in nearly half of the patients on initial CT, and in about 85–92% of the patients on follow-up CT, and they speculated that interstitial thickening, irregular interface, coarse reticular pattern and parenchymal band, manifesting in the process of the disease, might be predictors of pulmonary fibrosis in patients who recovered from COVID-19 pneumonia (1,2). An irregular interface and parenchymal band might be two early predictors of pulmonary fibrosis (1). From the clinical point of view, fibrosis can be usually seen in elderly patients with severe clinical conditions, especially in patients with higher level of C-reactive protein and interleukin-6 (1). We are not sure whether the authors detected typical pulmonary fibrosis and honeycomb appearances during the follow-up of COVID-19 patients. We encountered a typical pulmonary fibrosis during the follow-up of one COVID-19 patient, whose initial CT examination showed only GGO. Interstitial thickening, irregular interface, or parenchymal bands were not detected on initial CT examination.
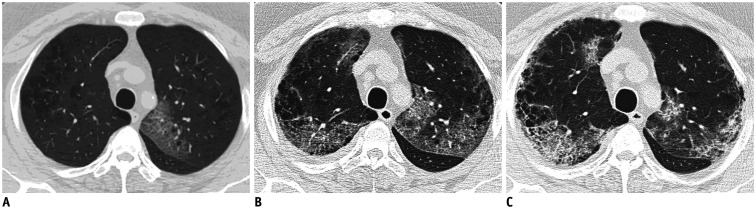
A 59-year old man was admitted to the chest department with a one-week history of dry cough and acute onset of fever and dyspnea. Unenhanced CT revealed focal GGOs in the left upper lobe of the lung (Fig. 1A). Laboratory results showed elevated C-reactive protein, D-dimer, lactate dehydrogenase, and ferritin levels, and decreased leukocyte, and lymphocyte counts. Oxygen saturation level was 85% at room air. COVID-19 infection was suspected; antiviral treatment (oseltamivir 75 mg 2 × 1, favipiravir 2 × 1600 mg first two days, then 2 × 600 mg) and supportive treatment were started. At admission, reverse transcriptase-polymerase chain reaction test (RT-PCR test) result was negative. One week later, control chest CT was obtained and chest CT showed bilateral multifocal mixed GGOs and crazy-paving pattern (Fig. 1B). A repeat RT-PCR test result was positive. Five days later, fever decreased, oxygen saturations levels improved and control chest CT showed decreased GGOs and crazy-paving patterns with peripheral cystic changes and interlobulary septal thickening causing the typical ‘honeycomb’ appearances due to pulmonary fibrosis (Fig. 1C). Respiratory rehabilitations were started and four days later, all symptoms including fever, cough, and dyspnea improved. The patient was discharged and recommended to continue respiratory rehabilitations.
Fig. 1. 59-year old man with one-week history of dry cough and acute onset of fever and dyspnea.
A. Unenhanced chest CT obtained on day 7 after onset of symptoms reveals focal ground-glass opacities in left upper lobe of lung. B. Chest CT was obtained one week later and shows bilateral multifocal mixed ground-glass opacities and crazy-paving pattern. C. Chest CT obtained on day 19 shows decreased ground-glass opacities and crazy-paving patterns with peripheral cystic changes and interlobulary septal thickening causing typical ‘honeycomb’ appearances due to pulmonary fibrosis.
In conclusion, although some fibrosis indicators such as irregular interfaces, parenchymal bands, and fibrotic changes during the follow-up of COVID-19 patients have been described in the literature, typical honeycomb appearances and typical pulmonary fibrosis have not been described before, to the best of our knowledge (1,3). Irregular interface and parenchymal bands, which were described as two early predictors of pulmonary fibrosis may not be seen on initial CT examination.
References
- 1.Yu M, Liu Y, Xu D, Zhang R, Lan L, Xu H. Prediction of the development of pulmonary fibrosis using serial thin-section CT and clinical features in patients discharged after treatment for COVID-19 pneumonia. Korean J Radiol. 2020;21:746–755. doi: 10.3348/kjr.2020.0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ward PA, Hunninghake GW. Lung inflammation and fibrosis. Am J Respir Crit Care Med. 1998;157:S123–S129. doi: 10.1164/ajrccm.157.4.nhlbi-10. [DOI] [PubMed] [Google Scholar]
- 3.Wei J, Yang H, Lei P, Fan B, Qiu Y, Zeng B, et al. Analysis of thin-section CT in patients with coronavirus disease (COVID-19) after hospital discharge. J Xray Sci Technol. 2020;28:383–389. doi: 10.3233/XST-200685. [DOI] [PMC free article] [PubMed] [Google Scholar]