Abstract
Purpose
In February 2020, the COVID-19 pandemic reached the United States. The impact of the pandemic on the US radiation oncology field remains unknown. The American Society for Radiation Oncology surveyed US radiation oncology practice leaders to gauge initial impact and immediate operational responses to the pandemic.
Methods and Materials
From April 16 to April 30, 2020, the American Society for Radiation Oncology surveyed US radiation oncology practice leaders by email to gauge initial impact and immediate operational responses to the COVID-19 pandemic.
Results
Two hundred twenty-two (43%) of 517 leaders responded from community and academic practices (62% and 34%, respectively), hospital-based and free-standing centers (69% and 29%), and metro and rural locations (88% and 12%). Practices reported treating an average of 1086 patients per year in 2019 (range, 0-7900) with an average daily treatment volume of 70 patients (range, 5-400). All practices reported uninterrupted operation. On average, practices were treating 68% of their typical volume (range, 10%-95%), with 92% implementing planned treatment postponement for lower risk patients. An estimated revenue decrease of 20% or more was experienced by 71% of practices. Confirmed COVID-19 patient cases were treated by 39% of practices. Seventy percent experienced staff shortages. Almost all (98%) practices implemented formal operational procedures to protect patients and staff, although personal protective equipment/infection control supply shortages were reported by 78% of practices. Seventy-four percent used telemedicine for virtual follow-up surveillance, and 15% leveraged telemedicine for on-treatment assessment.
Conclusions
The clinical and financial impacts of the COVID-19 pandemic on US radiation oncology were deep and broad. Despite reported shortages in personal protective equipment, declines in revenue, and reduced patient volumes, practices adapted quickly by refining standard processes of care, implementing recommended safety measures, and employing telemedicine to facilitate treatment continuity. Patients with higher risk disease experienced uninterrupted access to care. We plan to continue regular surveying across the lifespan of the pandemic to document the geographic and temporal impact of COVID-19 on the field and its patients.
Summary.
The American Society for Radiation Oncology surveyed US radiation oncology practice leaders to gauge initial impact and immediate operational responses to the COVID-19 pandemic. The clinical and financial impacts of the pandemic were deep and broad. Despite acute personal protective equipment supply chain shortages and sudden financial pressure, practices adapted quickly by refining their processes of care, implementing recommended safety measures, and employing telemedicine to facilitate treatment continuity.
Introduction
In February 2020, the COVID-19 pandemic reached the United States. During the initial transmission of cases, oncology practices suddenly faced the challenge of safely caring for high-risk populations with minimal evidence to guide them. On March 17, 2020, the American Society for Radiation Oncology (ASTRO) provided consensus recommendations for radiation oncology practices.1 , 2 Numerous local and multi-institutional guidelines were also published by the community.3, 4, 5, 6, 7, 8 From April 16 to April 30, ASTRO distributed a national survey to US radiation oncology practice leadership to publicly define the pandemic’s economic and clinical impact, to record the dissemination and implementation of recommended pandemic measures, and to identify new challenges to practices.
A 22-question survey was emailed directly to 517 ASTRO members identified as leaders in academic and community practices, of whOM 222 (43%) responded. Respondents were from both private practice and academic (62% and 34%, respectively), hospital-based and free-standing centers (69% and 29%), and metro and rural locations (88% and 12%). Responses were aggregated on the regional level to protect anonymity. Practices were represented from the West (20%), Midwest (25%), South (33%), and Northeast (21%).9
Practices reported treating an average of 1086 patients per year in 2019 (range, 0-7900), with an average of 69.9 patients currently under treatment (range, 5-400). Respondents reported an average of 6.2 radiation oncologists per practice (range, 1-55) and an average 15.6 radiation therapists on staff (range, 1-100).
All practices reported continuation of radiation services during the pandemic. The majority of practices experienced significant workflow changes outlined below.
Telemedicine
Nearly all (89%) centers reported that telemedicine was completely new to their practice. At the time of reporting, 74% had incorporated telemedicine for follow-up visits and surveillance, and 15% used telemedicine to assess patients under treatment in clinic. Uptake of telemedicine utilization was reported in 93%, 95%, and 92% of practices from the West, Midwest, and Northeast, respectively, but only 81% in the South. Telemedicine utilization was robust but variable across private practice versus academic (95% vs 86%), hospital-based versus free-standing centers (91% vs 86%), and metro versus rural practices (91% vs 74%).
Patient Volume
No practice reported stable patient volumes. Declines were reported by 85% of practices, largely due to reduction in referrals (81%) and delays in starting radiation therapy due to risks of the pandemic (82%). On average, practices reported treating 68% of their usual volume (range, 10%-95%). This reduction in patient volume was evenly distributed across geographic regions despite significant COVID-19 case rate heterogeneity across the United States at the time of surveying (Table 1 ).10
Table 1.
Radiation oncology practice reported patient volume and COVID-19 cases/deaths by region as of May 2, 2020
| Region | Percentage (%) patient volume compared with prepandemic (range) | COVID-19 cases (% of national total) | COVID-19 deaths (% of national total) |
|---|---|---|---|
| West | 66 (15-90) | 108,893 (10.0) | 4693 (7.3) |
| Midwest | 71 (40-90) | 184,678 (16.9) | 10,233 (15.9) |
| South | 70 (30-95) | 219,804 (20.1) | 9167 (14.3) |
| Northeast | 65 (10-90) | 577,639 (53.0) | 40,085 (62.5) |
Practice Revenue
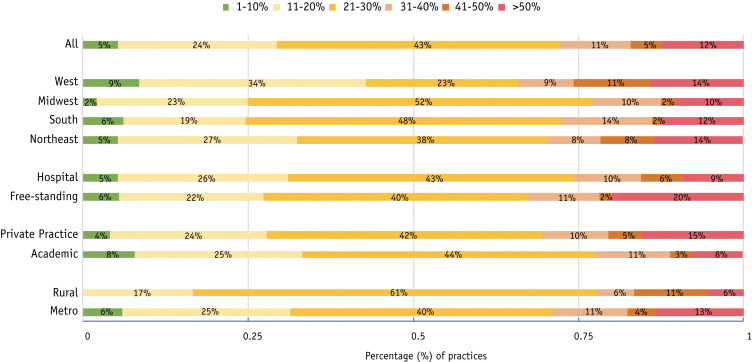
All practices reported some decrease in monthly revenue compared with the months before the pandemic. This varied modestly across practice categories and regions, as shown in Figure 1 . Overall, 71% of practices estimated revenue declines of 20% or more. Notably, revenue decline of 50% or more was reported in 12% of practices and varied between private practice versus academics (15% vs 8%), as well as free-standing and hospital-based centers (20% vs 9%).
Fig. 1.
Percentage reported revenue decrease by radiation oncology practices by location and practice type.
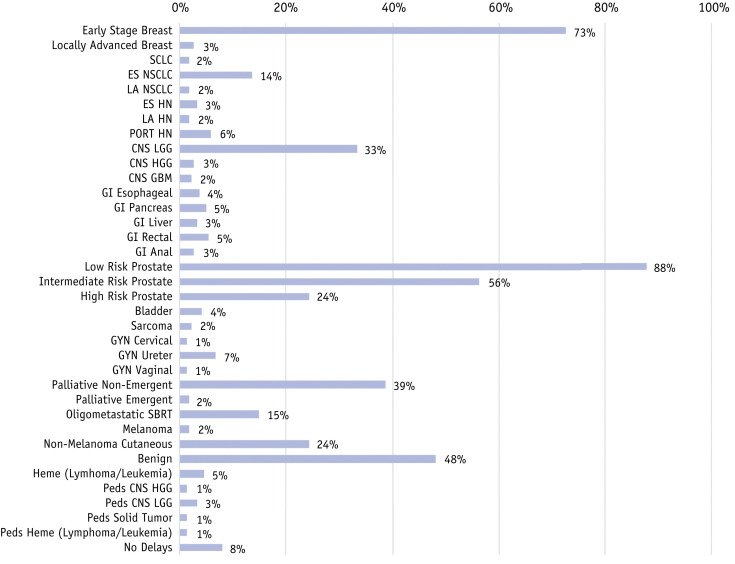
Treatment Delays
Treatment delays were reported by 92% of practices. Respondents reported planned postponement of treatment for low-risk prostate (88%), early stage breast (73%), intermediate-risk prostate (56%), benign diseases (48%), low-grade gliomas (33%), nonemergent palliative cases (39%), nonmelanoma cutaneous (24%), and high-risk prostate cancers (24%). Treatment for other types of cancers was delayed by less than 15% of practices. Full details of percentage of practices deferring radiation treatments are available by disease site in Figure 2 .
Fig. 2.
Percentage of practices reporting planned treatment postponement/delay by cancer type.
Personal Protective Equipment Shortages
Overall, 78% of practices experienced some form of shortage in personal protective equipment (PPE) or other infection control supplies. All regions of the United States experienced shortages of N95 masks, surgical masks, gowns, and/or gloves. The Northeast reported the lowest PPE shortages, in 62% of centers, compared with the South (71%), Midwest (71%), and West (67%). Rural (78%), free-standing (75%), and private (73%) practices were more heavily affected than metro (67%), hospital-affiliated (66%), and academic (61%) centers. Departments also lacked hand sanitizer (43%) and nasopharyngeal swabs (26%). Reported shortages of anticancer drugs (1%), narcotics (4%), and other supportive care drugs (4%) were infrequent.
Pandemic Procedures
Notably, 40% of practices confirmed COVID-19 patient cases within their practice at the time of this survey. Ninety-eight percent of practices reported increased measures for the protection of staff, including requiring all staff to wear masks (99%), social distancing of 6 feet while working in clinic (96%), increased cleaning (95%), screening staff at the beginning of each shift (91%), and testing symptomatic staff (93%). Some practices required gloves (72%), face shields (50%), and gowns (22%) during treatments and procedures, as well as staggered shifts of limited staff (50%).
Patient screening at the front door of the facility was reported by 98% of practices. Additional measures included social distancing of 6 feet in clinic (98%), limiting visitors (90%), requiring patients to wear masks (82%), and telehealth efforts, as mentioned.
Quarantine procedures were created for COVID-19–positive patients in 98% of centers and included treating these patients at a certain time of the day (50%) and treating them in a specific vault or satellite location (21%).
Nearly all (97%) departments stated that they increased their infection control measures by sanitizing treatment tables (91%), increasing cleaning immobilization devices (88%), and requiring patient and staff hand washing when entering and exiting treatment vaults (65%).
Staff Reductions
Many centers (70%) reported staff reductions in response to the pandemic. Practices required quarantine of staff due to a positive COVID-19 test (10%) or infection of an immediate family member (27%). As treatment loads declined, staff hours were reduced at 48% of centers. Some centers (15%) reported that hours staffed in the radiation oncology department declined to assist the staffing of other clinical services. Full details of staff reductions by region, primary employer, location, and community can be found in Table 2 .
Table 2.
Radiation oncology practice reported staff reductions distributed across US region, primary employer, practice location, and community type
| Personal infection (%) | Family infection (%) | Patient decrease (%) | Staff transfer (%) | No reductions (%) | |
|---|---|---|---|---|---|
| Region | |||||
| West | 11 | 22 | 40 | 11 | 36 |
| Midwest | 11 | 29 | 56 | 15 | 27 |
| South | 8 | 26 | 53 | 16 | 32 |
| Northeast | 13 | 30 | 36 | 19 | 28 |
| Employer | |||||
| Academic | 16 | 30 | 46 | 21 | 24 |
| Private practice | 7 | 26 | 50 | 12 | 33 |
| Location | |||||
| Free-standing | 8 | 25 | 46 | 12 | 32 |
| Hospital | 12 | 28 | 49 | 17 | 29 |
| Community | |||||
| Metro | 12 | 28 | 48 | 17 | 30 |
| Rural | 4 | 15 | 41 | 7 | 37 |
Guidance
ASTRO guidance resources were used by the majority (85%) of practices. The primary ASTRO COVID-19 information page (https://www.astro.org/Daily Practice/COVID-19-Recommendations-and-Information) was the most popular resource (66%), followed by secondary resources for clinical decision making (58%) and telehealth coding (55%).
Takeaways
Radiation therapy is an essential, nonelective treatment for many cancer types. We demonstrate durable maintenance of radiation oncology services across the United States early during the initial pandemic wave of COVID-19 despite tremendous uncertainty, challenges to staff and patient safety, limited resources, and economic loss.
Practice volumes declined nationwide, regardless of regional variations in COVID-19 prevalence. Several cancer types believed to represent lower-risk diagnoses had treatments systematically postponed across most centers. This practice was widely advised by publicized guidelines, directing providers to focus effort on time-sensitive diagnoses. Without such triage, untempered patient avoidance of health care during the early pandemic could have led to more disorganized interruption patterns. The extent and consequences of radiation therapy delays on outcomes remains uncertain, as are the long-term impacts of acute revenue loss (30% or more) across most US practices. Likewise, the exact downstream impact of PPE shortfalls on patient and provider transmission rates and perceived safety remain important topics of study.
Another significant finding was the accelerated adoption of telemedicine, likely increasing patient access to radiation therapy care nationwide. Despite many practices reporting staffing and PPE shortages, all centers were able to implement novel safety measures and maintain operations with remarkable continuity.
Our survey was shared with global leaders in Europe and Latin America, which uncovered noteworthy international distinctions. For example, the European Society for Radiotherapy and Oncology reported that only 38% of 139 surveyed centers experienced patient volume reductions, and only 52% reported PPE or supply shortages.11 In contrast, Latin American leaders reported that 80% of centers experienced reduced patient volumes and 66% experienced PPE or supply shortages (Martinez et al., COVID-19's impact on Radiation Oncology Survey: The Latin American Scenario. Unpublished data). Reduced revenue was estimated to be more than 20% in 53% of Latin American centers but only 25% of European centers. Detailed comparisons will be reported in separate manuscripts.
Our results are limited by the inherent weaknesses of a retrospective online survey using cross-sectional convenience sampling susceptible to responder bias. Nonetheless, our participation rate was relatively robust (>40%) for surveys of this type, and our results are less vulnerable to recall bias due to the near synchronous sampling of responses with the pandemic’s first wave.12
Looking toward the future, we plan to continue surveying our profession’s leadership at regular intervals across the course of the pandemic. This will guide evidence-based practice strategies, such as formal guideline-driven expansion of telemedicine into standard radiation oncology practice, that meet our patients’ needs and address the public health and financial uncertainties of the moment. ASTRO has immediately leveraged this survey data to advocate for productive professional and legislative responses to COVID-19. For example, ASTRO has collaborated directly with the American Society of Clinical Oncology (ASCO), the European Society for Radiotherapy and Oncology, and Latin American colleagues to coordinate and publish global professional survey data collection.11 ASTRO has also widely publicized its initial survey results (https://www.astro.org/ASTRO/media/ASTRO/News%20and%20Publications/PDFs/ASTROCOVID19Survey1-ExecSummary.pdf) and shared with lawmakers (Dave Adler, personal communication) to directly advocate support to maintain patient access to radiation oncology practices under acute financial stress. Future data will further characterize our role in this evolving health crisis and deepen our partnerships with public health officials, lawmakers, and the communities we serve. Our profession’s response to future large-scale public health crises will rest on a foundation of lessons learned from this wide-scale effort.
Acknowledgments
We thank all the US respondents in the survey, as well as leaders and participants from ESTRO and Latin America for their participation.
Footnotes
Disclosures: B.D.S. reports royalty and equity interest in Oncora Medical and prior research funding from Varian Medical Systems. B.J.S. reports a grant from Varian Medical Systems and grants and personal fees from ViewRay Medical Systems. G.R.S. reports grants and personal fees from Carl Zeiss Meditec AG, not related to this work.
References
- 1.American Society for Radiation Oncology COVID-19 FAQs. https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/COVID-19-FAQs#q6 Available at:
- 2.American Society for Radiation Oncology COVID-19 recommendations and information: Summary. https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/Summary Available at:
- 3.Dietz J.R., Moran M.S., Isakoff S.J. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. The COVID-19 Pandemic Breast Cancer Consortium. Breast Cancer Res Treat. 2020;181 doi: 10.1007/s10549-020-05644-z. 487-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guckenberger M., Belka C., Bezjak A. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: An ESTRO-ASTRO consensus statement. Radiother Oncol. 2020;146:223–229. doi: 10.1016/j.radonc.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Health and Care Excellence COVID-19 rapid guideline: delivery of radiotherapy. https://www.nice.org.uk/guidance/ng162/resources/covid19-rapid-guideline-delivery-of-radiotherapy-pdf-66141897390277 Available at: [PubMed]
- 6.Schwartz A., Stiegel M., Greeson N. Decontamination and reuse of N95 respirators with hydrogen peroxide vapor to address worldwide personal protective equipment shortages during the SARS-CoV-2 (COVID-19) pandemic. Appl Biosaf. 2020;25:67–70. doi: 10.1177/1535676020919932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.UW Radiation Oncology COVID-19 Approach 2020. Available at: astro.org/ASTRO/media/ASTRO/Daily%20Practice/PDFs/UWROCOVID-19ClinicalCareApproach.pdf. Accessed June 6, 2020.
- 8.Wright JL, Alcom SR, McNutt T, et al. An integrated program in a pandemic: Johns Hopkins Radiation Oncology Department [e-pub ahead of print]. Adv Radiat Oncol.https://doi.org/10.1016/j.adro.2020.03.014. Accessed June 6, 2020. [DOI] [PMC free article] [PubMed]
- 9.U.S. Census Bureau Census regions and divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf Available at:
- 10.Centers for Disease Control and Prevention United States COVID-19 cases and deaths by state. https://www.cdc.gov/covid-data-tracker/index.html Available at:
- 11.Slotman B.J., Lievens Y., Poortmans P. Effect of COVD-19 pandemic on practice in European radiation oncology centers. Radiother Oncol. 2020;150:40–42. doi: 10.1016/j.radonc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Batra P. Using organization member lists in web surveys to achieve a larger sample size. Paper presented at: 52nd Annual Meeting of the International Field Directors & Technologies Conference. May 2019; Toronto, ON.