Abstract
Purpose
Telemedicine was rapidly and ubiquitously adopted during the COVID-19 pandemic. However, there are growing discussions as to its role postpandemic.
Methods and Materials
We surveyed patients, radiation oncology (RO) attendings, and RO residents to assess their experience with telemedicine. Surveys addressed quality of patient care and utility of telemedicine for teaching and learning core competencies. Satisfaction was rated on a 6-point Likert-type scale. The quality of teaching and learning was graded on a 5-point Likert-type scale, with overall scores calculated by the average rating of each core competency required by the Accreditation Council for Graduate Medical Education (range, 1-5).
Results
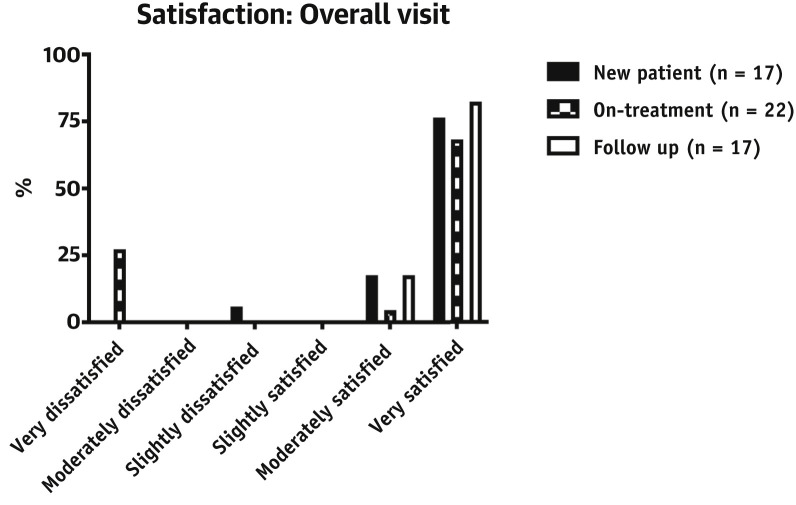
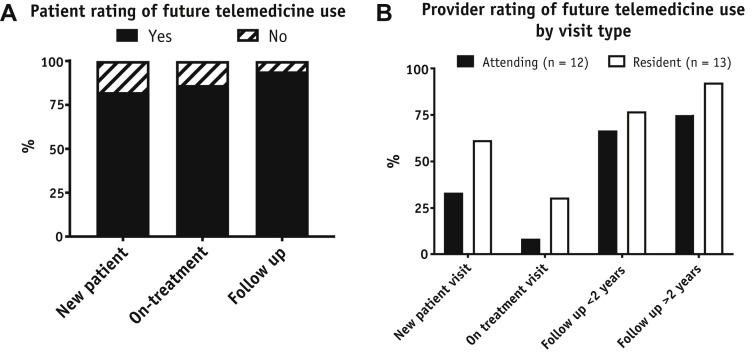
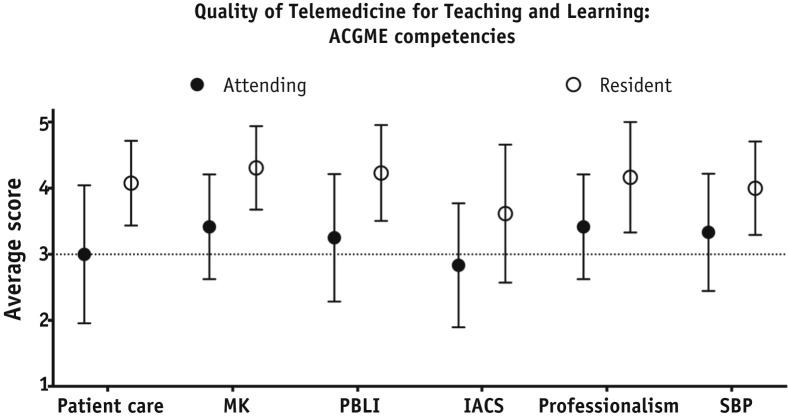
Responses were collected from 56 patients, 12 RO attendings, and 13 RO residents. Patient feedback was collected at 17 new-patient, 22 on-treatment, and 17 follow-up video visits. Overall, 88% of patients were satisfied with virtual visits. A lower proportion of on-treatment patients rated their virtual visit as “very satisfactory” (68.2% vs 76.5% for new patients and 82.4% for follow-ups). Only 5.9% of the new patients and none of the follow-up patients were dissatisfied, and 27% of on-treatment patients were dissatisfied. The large majority of patients (88%) indicated that they would continue to use virtual visits as long as a physical examination was not needed. Overall scores for medical training were 4.1 out of 5 (range, 2.8-5.0) by RO residents and 3.2 (range, 2.0-4.0) by RO attendings. All residents and 92% of attendings indicated they would use telemedicine again; however, most indicated that telemedicine is best for follow-up visits.
Conclusions
Telemedicine is a convenient means of delivering care to patients, with some limitations demonstrated for on-treatment patients. The majority of both patients and providers are interested in using telemedicine again, and it will likely continue to supplement patient care.
Introduction
Telemedicine delivers secure virtual health care and has been selectively adopted over the past several years.1 Virtual visits are particularly useful for patients who are immobile, live in remote locations, or are immunocompromised. Telemedicine is typically billed at a lower cost than in-person visits, offering accessible health care for disadvantaged populations.2 As a result of COVID-19 and physical distancing requirements, telemedicine has been rapidly adopted throughout all medical specialties.
The Centers of Medicaid and Medicare Services temporarily expanded coverage for telemedicine services during the COVID-19 pandemic, enabling radiation oncologists to transition to virtual communication for nearly all visit types. Before the virus outbreak, telemedicine was piloted for select patients in radiation oncology (RO) at our institution, with anticipated department-wide launch in February 2020 for follow-up visits (FUVs) only. Since the pandemic began, expansion of telemedicine was expedited to cover new-patient visits (NPVs) and on-treatment visits (OTVs) in efforts to mitigate disease transmission. Although adopted out of necessity, telemedicine in RO may continue as an option for select patients.
In this quality-improvement initiative, we explore the impact of telemedicine at our institution by evaluating patient satisfaction during various visit types, physician/resident satisfaction in delivering patient care, and resident education. We anticipate that these preliminary findings may inform the future use and impact of telemedicine encounters in RO.
Methods and Materials
We anonymously surveyed patients seen through telemedicine in the Department of Radiation Oncology at our institution, specifically in the breast and gastrointestinal clinics. This study was approved by our institutional review board (IRB-45782). Patients were approached after their NPV, OTV, or FUV. Patients using telemedicine for NPVs and FUVs joined remotely from a phone or computer, and OTV patients were on site and seen virtually throughout the day, logged on by a medical assistant. Telephone encounters without video were excluded. Patients reported satisfaction with their visit on a 6-point Likert-type scale, ranging from “very dissatisfied" to “very satisfied.” Similarly, patients evaluated the statement “I feel comfortable being examined through telemedicine” with answers ranging from “disagree strongly” to “agree strongly.” They were also asked about prior use of telemedicine, whether technical difficulties arose, and the likelihood they would use telemedicine after the COVID-19 pandemic.
RO attendings and residents assessed general satisfaction, efficiency, and appropriateness of telemedicine on a 6-point Likert-type scale. They also assessed the types of visits they would recommend telemedicine for in the future. The quality of telemedicine for teaching/learning was assessed on a 5-point Likert-type scale for core competencies defined by the Accreditation Council for Graduate Medical Education. Overall score for resident education was the average rating for each competency, ranging from “very poor” (1) to “excellent” (5).
Results
Fifty-six patient responses were collected on 17 NPVs, 22 OTVs, and 17 FUVs over 2 weeks. Eight patients had no previous telemedicine experience. Although patients were overall satisfied with telemedicine, satisfaction varied by visit type (Fig. 1 ). A greater proportion of NPV and FUV patients were “very satisfied” with telemedicine metrics, compared with OTV patients (Table 1 ). Correspondingly, patient dissatisfaction was higher in OTV patients (27% vs 5.9% for NPV and 0% for FUV).
Fig. 1.
Patient satisfaction with telemedicine by visit type.
Table 1.
Patients who were very satisfied with telemedicine by visit type
| Visit characteristic | Proportion of patients who were “very satisfied” (%) |
||
|---|---|---|---|
| New-patient visit (n = 17) | On-treatment (n = 22) | Follow-up (n = 17) | |
| Overall visit | 76.5 | 68.2 | 82.4 |
| Length of time spent with physician | 82.4 | 63.4 | 100 |
| How physician answered questions | 88.2 | 72.7 | 100 |
| Ease of asking questions | 70.6 | 59.1 | 94.1 |
Virtual examination of skin occurred for 22 patients. Regarding whether they felt comfortable with their examination, 1 NPV with gastrointestinal cancer “disagreed moderately,” 16 of 17 (94%) OTV patients with breast cancer agreed “moderately” or “strongly,” and 3 of 4 (75%) FUV patients with breast cancer agreed “strongly.” Technical difficulties were experienced by 28.6% patients, including faulty Internet connection, audio disconnection, and subjective lack of technological knowledge.
In total, 49 of 56 (88%) patients indicated that, if given the choice, they would use virtual visits again. Reasons included convenience of location, saving time, and avoiding traffic/parking. Seventeen percent of NPV, 13% of OTV, and 6% of FUV patients would not use telemedicine again (Fig. 2 A). Patients preferred in-person appointments for visits anticipated to be long, complex, emotionally distressing, or requiring a physical examination.
Fig. 2.
Assessment of the future use of telemedicine. (A) Patient ratings as “yes” or “no,” categorized by their visit type. (B) Percent of radiation oncology attendings and residents who answered “yes” for using telemedicine, by visit type.
RO attending (n = 12) and resident (n = 13) ratings of telemedicine experience for patient care are shown in Table 2 . More than 50% of respondents, on average, agreed that telemedicine was satisfactory for patient care, was efficient, and provided enough time to address patient needs. Contrarily, 52% of respondents disagreed that telemedicine was sufficient to deliver physical examination. Technical difficulties were experienced by all, but “often” for 58.3% attendings versus 8% residents. All residents and 91.7% of attendings would use telemedicine again; most indicated that telemedicine is best suited for FUVs (Fig. 2B).
Table 2.
Radiation oncology attending (n = 12) and resident (n = 13) ratings of telemedicine
| General rating of telemedicine for clinical duties, no. (%) |
||||||
|---|---|---|---|---|---|---|
| Disagree strongly | Disagree moderately | Disagree slightly | Agree slightly | Agree moderately | Agree strongly | |
| Telemedicine is a satisfactory way to deliver patient care | ||||||
| Attendings | 0 (0) | 1 (8.3) | 2 (16.7) | 3 (25) | 6 (50) | 0 (0) |
| Residents | 0 (0) | 1 (7.7) | 2 (15.4) | 5 (38.5) | 6 (46.2) | 4 (30.8) |
| Seeing patients via telemedicine allows me to accomplish more with my day | ||||||
| Attendings | 0 (0) | 1 (8.3) | 1 (8.3) | 4 (33.3) | 5 (41.7) | 1 (8.3) |
| Residents | 0 (0) | 0 (0) | 1 (7.7) | 0 (0) | 3 (23.1) | 8 (61.5) |
| A telemedicine visit provides enough time to address my patient’s needs | ||||||
| Attendings | 1 (8.3) | 0 (0) | 1 (8.3) | 2 (16.7) | 5 (41.7) | 6 (50) |
| Residents | 0 (0) | 0 (0) | 1 (7.7) | 0 (0) | 3 (23.1) | 8 (61.5) |
| Examination via telemedicine is sufficient to deliver appropriate care | ||||||
| Attendings | 2 (16.7) | 3 (25) | 4 (33.3) | 2 (16.7) | 1 (8.3) | 0 (0) |
| Residents | 0 (0) | 2 (15.4) | 2 (15.4) | 1 (7.7) | 6 (46.2) | 2 (15.4) |
Attendings rated telemedicine lower than residents did for teaching/learning the Accreditation Council for Graduate Medical Education competencies: Overall scores were 3.2 out of 5 by attendings (standard deviation, 0.81) and 4.1 by residents (standard deviation, 0.64; Fig. 3 ). Between virtual visits, attendings and residents were able to share screens to review scans and discuss learning points with lecture slides/papers, providing an additional avenue for education. Residents commented that navigating and conducting patient care through telemedicine are necessary skills and believed that continued use of telemedicine, when in the best interest of the patient, is beneficial.
Fig. 3.
The dotted line represents the “fair” quality. Scores: 1, very poor; 2, poor; 3, fair; 4, good; 5, excellent. Abbreviations: ACGME = Accreditation Council for Graduate Medical Education; IACS = interpersonal and communication skills; MK = medical knowledge; PBLI = practice-based learning and improvement; SBP = system-based practices.
Discussion
Telemedicine was convenient and efficient, with 88% of patients indicating they would use it in the future. Although telemedicine is not novel,3 the pandemic triggered an immediate adoption of telemedicine at many institutions for all encounter types.4 The propulsion toward universal telemedicine by removing reimbursement limitations and establishing infrastructure has created the opportunity for providers and patients to broadly adopt its implementation.
The continued use of telemedicine postpandemic is enticing, given the convenience, efficiency (eliminating rooming time, reducing clinic overflow and patient wait times), and potential to reduce health care costs. Most patients were very satisfied with their visits and would continue using telemedicine as long as a physical examination is not necessary. We observed differences in the satisfaction of patients by visit type, suggesting that patients seen for FUVs may be more amenable to telemedicine, compared with NPVs or OTVs. Telemedicine may thus be most advantageous for FUVs, when the visit is focused on reviewing imaging or symptom management, or for second-opinion NPVs, which mainly focus on patient education.
The challenges of telemedicine must be considered when assessing the feasibility of postpandemic use. Technical issues have been pervasive from the onset, creating frustrating impediments in communication for both patients and physicians. Although some technical issues have been resolved with software upgrades, others are more inherent, including connection disruptions and a disparity of technological capabilities and access among patients. Lower-income patients may not have access to the Internet or devices with video capabilities. Additionally, navigating telemedicine must be learned and is constantly changing with software upgrades, which may be particularly burdensome for elderly patients. It will be important to develop new workflows to identify which patients are ideal candidates for telemedicine. Continued support from staff is also essential to aid patients/providers in navigating telemedicine and ensure a smooth patient experience. Lastly, the economics of telemedicine implementation are not trivial. Although cost is generally beneficially lower for patients,5 , 6 institutions will need to account for lower net revenue.
One of the biggest arguments against telemedicine is the potential loss of humanistic aspects of medicine. This includes the loss in ability to build strong rapport with new patients and to optimally address a patient’s emotional state. Although physical presence was restricted during the pandemic, it remains an integral aspect of holistic care.
Small sample size limits the generalizability of our findings. Additionally, disease characteristics could not be evaluated given the anonymity of patient responses. Because surveyed patients were treated for breast and gastrointestinal cancers, results may differ for other disease sites, such as head and neck cancers and lymphomas, for which in-person physical examination may be more integral for workup and follow-up care.
Radiation oncologists are responsible for assessing patients’ side effects weekly during treatment. Telemedicine may be sufficient for patient-reported acute toxicities and superficial skin checks; however, in-person physical examination will likely remain an important aspect of care for patients actively undergoing treatment. At our institution, only 3 of 12 providers conducted virtual OTVs, reflecting the unlikelihood of virtual OTVs persisting post-COVID. Reasons are multifactorial: (1) technical difficulties easily bypassed by visiting the patient, (2) the need to continue relationship-building when patients feel most vulnerable, and (3) the need for close examination. During COVID-19, virtual OTVs were beneficial by enabling physical distancing; post-COVID, it seems there is not much to be gained. It is thus not surprising that a proportion of OTV patients felt unsatisfied by the virtual visit, which may reflect the need for facetime.
Finally, consideration of telemedicine’s impact on trainee education is paramount at academic institutions. Attendings generally rated telemedicine as worse for teaching than did residents, who generally did not believe it detracted from their education. Both groups found that telemedicine lacked the opportunity for teaching/learning interpersonal and communication skills. Thus, future transition to a solely telemedicine platform may not be ideal.
Conclusion
Although telemedicine is unlikely to fully replace in-person visits in RO, it will likely supplement patient care. Both patients and radiation oncologists indicated that telemedicine will be more ideal for FUVs rather than for NPVs, OTVs, or visits with anticipated distressing news. Telemedicine visits maintained good clinical care. The impact on resident education must be further explored.
Footnotes
Disclosures: none
References
- 1.Lewis G, Hatch S, Wiederhold L, et al. Long-term institutional experience with telemedicine services for radiation oncology: A potential model for long-term utilization [e-pub ahead of print]. Adv Radiat Oncol. https://doi.org/10.1016/j.adro.2020.04.018. Accessed July 1, 2020. [DOI] [PMC free article] [PubMed]
- 2.Uscher-Pines L., Mehrotra A. Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Aff (Millwood) 2014;33:258–264. doi: 10.1377/hlthaff.2013.0989. [DOI] [PubMed] [Google Scholar]
- 3.Field M.J., editor. Telemedicine: A Guide to Assessing Telecommunications in Health Care. National Academies Press; Washington, DC: 1996. Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine. [PubMed] [Google Scholar]
- 4.Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: Evidence from the field [e-pub ahead of print]. J Am Med Inform Assoc. https://doi.org/10.1093/jamia/ocaa072. Accessed July 1, 2020. [DOI] [PMC free article] [PubMed]
- 5.Finkelstein S.M., Speedie S.M., Potthoff S. Home telehealth improves clinical outcomes at lower cost for home healthcare. Telemed J E Health. 2006;12:128–136. doi: 10.1089/tmj.2006.12.128. [DOI] [PubMed] [Google Scholar]
- 6.Cryer L., Shannon S.B., Van Amsterdam M. Costs for “hospital at home” patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood) 2012;31:1237–1243. doi: 10.1377/hlthaff.2011.1132. [DOI] [PubMed] [Google Scholar]