Abstract
This study aimed to investigate whether mass drug administration (MDA) intervention has an equivalent effect on reducing the prevalence and intensity of Schistosoma haematobium infection regardless of the baseline values. A repeated cross-sectional survey was performed targeting students of 12 primary schools in Al Jabalain and El Salam districts of White Nile State, Sudan, at both 1 week before and 8 months after the MDA. Prior to the baseline survey, school-aged children in Al Jabalain had received MDA interventions twice in 4 years, while those in El Salam had not. The baseline prevalence was 9.1% in Al Jabalain and 35.2% in El Salam, which were reduced to 1.8% and 5.5% at 8 months after the MDA, respectively. The corresponding reduction rates were 80.3% and 84.4%, not significant difference between both districts. However, changes in the geometric mean intensity (GMI) of egg counts were significantly different between both districts. The baseline GMIs were 14.5 eggs per 10 ml of urine (EP10) in Al Jabalain and 18.5 EP10 in El Salam, which were reduced to 7.1 and 11.2 EP10 after treatment, respectively. The corresponding reduction rates were 51.0% and 39.5%. In conclusion, MDA interventions were found to bring about similar relative reduction in prevalence regardless of the baseline value; however, the relative reduction in infection intensity was more salient in the district with a low baseline value for both prevalence and intensity. This clearly points to the importance of repeated MDA interventions in endemic areas, which will eventually contribute to schistosomiasis elimination.
Keywords: Schistosoma haematobium, prevalence, infection intensity, mass drug administration, Sudan
INTRODUCTION
Schistosomiasis is a parasitic disease caused by a blood fluke of the Schistosoma species. Humans are usually infected when they come into contact with contaminated freshwater and experience hematuria, anemia, enlargement of the liver and spleen, and growth retardation [1]. Schistosomiasis is endemic in 78 countries and is a major public health problem in many tropical countries–particularly in Africa, where>90% of the global burden of schistosomiasis occurs [2]. The global burden of schistosomiasis was conservatively estimated at 1.43 million disability-adjusted life years in 2017 [3]. More than 220.8 million people required preventive chemotherapy for schistosomiasis in 2017, and 102.3 million of them were treated [4]. Sudan has one of the highest schistosomiasis prevalence rates in the world [5–8]. About 15% of the total population (~5.8 million people) require treatment, with the majority being children [9].
Mass drug administration (MDA) refers to the delivery of preventive chemotherapy to targeted populations irrespective of individual infection status. Currently, 5 major “tool-ready” neglected tropical diseases with MDA are lymphatic filariasis, onchocerciasis, schistosomiasis, soil-transmitted helminthiasis, and trachoma [10]. MDA of praziquantel to at-risk populations has become the cornerstone of schistosomiasis control, especially for school-aged children (SACs), who have the highest risk of infection [11,12]. So far, most studies on the effects of MDA were focused on reduction rates in the prevalence and intensity of disease [5,12–17] and have not investigated as to what extent the reduction rate changes depending on the baseline value. It therefore is critical to compare changes in the prevalence and intensity of Schistosoma infection between high- and low-prevalence areas to determine the adequate frequency of MDA; however, there have been no studies in this regard. To fill this knowledge gap, this study aimed to compare the changes in the prevalence and intensity of Schistosoma haematobium in 2 districts of the White Nile State, Sudan.
MATERIALS AND METHODS
Study area
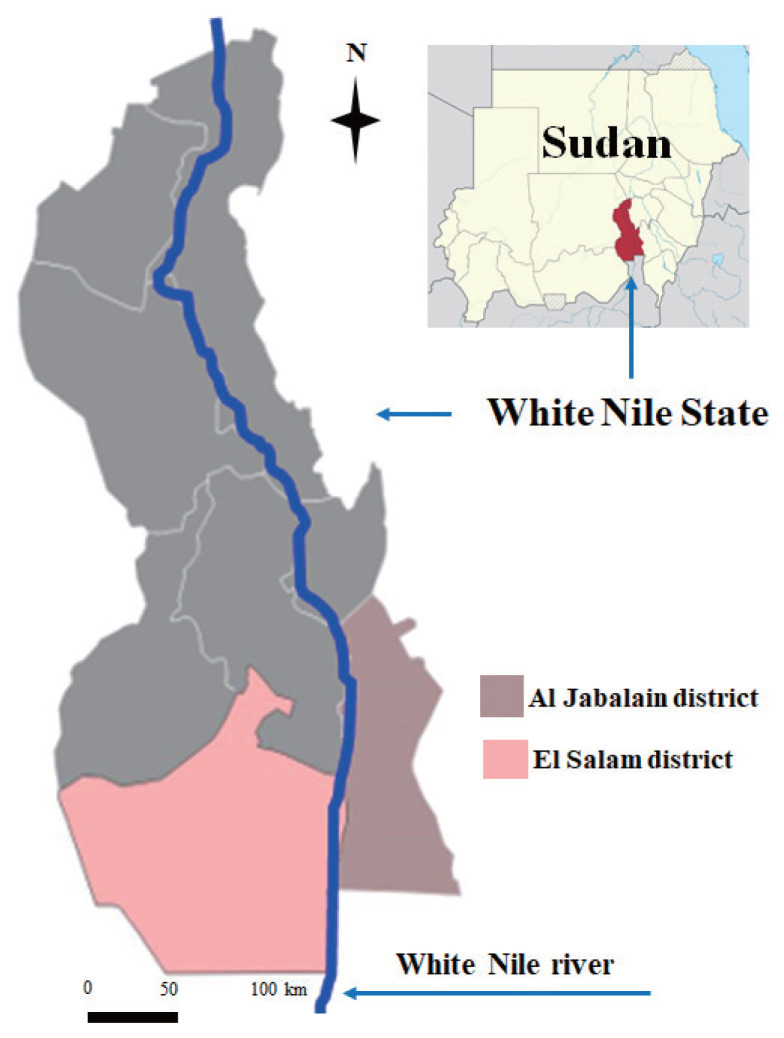
The White Nile State is located along the White Nile River in the southeastern part of Sudan. A number of water canals connecting with the river have been developed. The Al Jabalain and El Salam districts of the White Nile State are composed of 6 and 5 Administrative Units, respectively (Fig. 1). An Administrative Unit is the lowest level of the local administrative organization in Sudan and has been used as a basic structure for implementing MDA.
Fig. 1.
Location of Al Jabalain and El Salam districts in the White Nile State, Sudan.
Study design and sampling
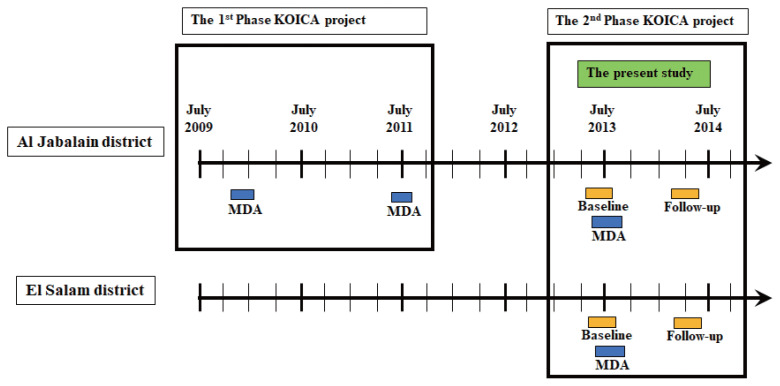
This was a repeated cross-sectional study. Two-stage cluster sampling was used. In 2013, 6 primary schools were randomly selected among 169 and 76 schools from Al Jabalain and El Salam, respectively. Of the target schools, 2,783 and 3,197 students were sampled for baseline and follow-up surveys, respectively. The baseline survey was conducted in June 2013, the MDA intervention was carried out in July 2013, and the follow-up survey was conducted in March 2014 (Fig. 2).
Fig. 2.
Schematic illustration of the study design and mass drug administration (MDA) with praziquantel to school-aged children in Al Jabalain and El Salam districts in the White Nile State of Sudan.
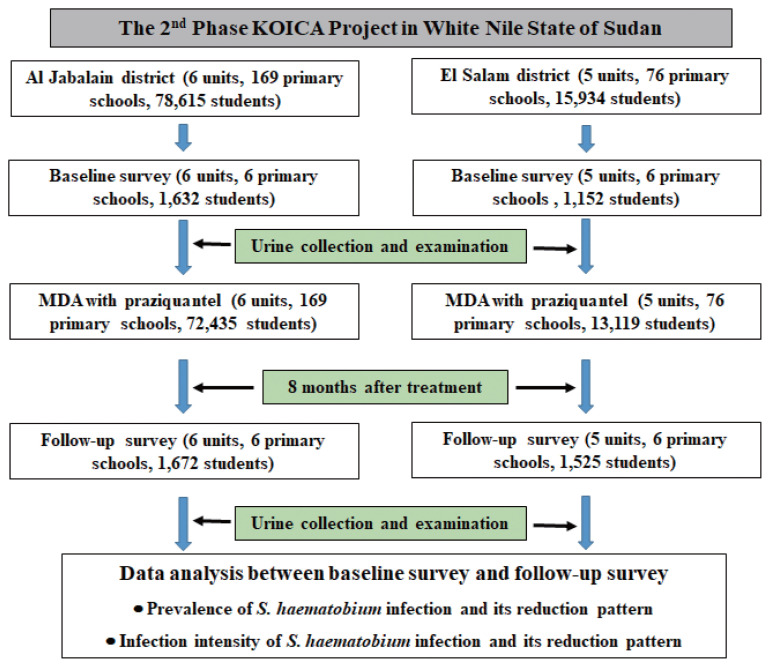
In each target school, all students in 1st, 3rd, and 5th grade were sampled. For the baseline survey, 2,784 students–1,632 from Al Jabalain and 1,152 from El Salam–were sampled. For the follow-up survey, 3,197 students–1,672 from Al Jabalain and 1,525 from El Salam–were sampled (Fig. 3). The total number of participated students were different depending on the time of the survey. The increase in the number of students at the follow-up survey was due to the rise in the enrollment and attendance rates in 2014 compared to 2013.
Fig. 3.
Flowchart of participation and study methods. This project was carried out in Al Jabalain and El Salam districts, White Nile State, Sudan 2013–2014.
Their urine samples were assessed for testing S. haematobium infection using centrifugation methods. After the baseline survey, MDA was conducted targeting schools within Administrative Units with a prevalence of ≥1% according to the Sudanese government MDA policy. Accordingly, MDA was implemented in all Administrative Units targeting SACs in the 2 districts because all Administrative Units had a schistosomiasis prevalence of ≥1%. The number of subjects for this study was estimated conveniently [18], not relying on the formula for sample size calculation mainly because the main purpose of the data collection was to assess progress and provide a report to the funder (Korea International Cooperation Agency [KOICA]). We thus had to maximize the number of samples within the given budget to assess any changes at the school level, as possible as we could.
Intervention
From 2009 until 2011, KOICA implemented an integrated schistosomiasis control project in the Al Jabalain district (1st phase of the KOICA project) [5]. The 2nd phase started in 2012, extending the target areas to the El Salam district. This study was conducted during the 2nd phase. The low baseline prevalence and intensity in Al Jabalain compared to El Salam was believed to be partially due to the repeated MDA interventions during the 1st phase. In contrast, El Salam had never received any MDA intervention from 2009 up until the baseline data collection in 2012. During the 2nd phase of the project, SACs in both districts received MDA intervention. Details of the study design and MDA during the 1st and 2nd phases of the KOICA project are illustrated in Fig. 3. Details of the MDA intervention during the 2nd phase are described in Table 1.
Table 1.
Number of target primary school children treated with praziquantel for control of schistosomiasis in Al Jabalain and El Salam districts, White Nile Sate, Sudan
| District | Administrative unit | No. of schools | No. of school children | No. of treated | Coverage rate (%) |
|---|---|---|---|---|---|
| Al Jabalain | Al Jabalain | 30 | 10,226 | 9,992 | 97.7 |
| Assalaya | 29 | 10,444 | 9,116 | 87.3 | |
| Jazeera Aba | 18 | 6,474 | 5,043 | 77.9 | |
| Joda | 10 | 4,463 | 3,644 | 81.6 | |
| Kenana | 34 | 17,750 | 17,191 | 96.9 | |
| Rabak | 48 | 29,258 | 27,449 | 93.8 | |
| Subtotal | 169 | 78,615 | 72,435 | 92.1 | |
|
| |||||
| El Salam | Al Rawat | 30 | 5,321 | 4,194 | 78.8 |
| Al Zelit | 12 | 2,602 | 2,089 | 80.3 | |
| Al Naeem | 18 | 4,313 | 3,438 | 79.7 | |
| Al Kewaik | 7 | 1,892 | 1,696 | 89.6 | |
| Al Migainis | 9 | 1,806 | 1,702 | 94.2 | |
| Subtotal | 76 | 15,934 | 13,119 | 82.3 | |
|
| |||||
| Total | 245 | 94,549 | 85,554 | 90.5 | |
The chemotherapy strategy followed the schistosomiasis control protocol of the Sudanese government, which was a modified treatment strategy recommended by the World Health Organization (WHO) [19]. Parasitology experts controlled all drug treatments. The drugs were delivered through the school-based system by health workers. All health workers were White Nile State Ministry of Health officials and were educated on drug treatment and schistosomiasis control projects by parasitology experts before the study. For the MDA of praziquantel (Distocide®, GMC Co. Ltd., Khartoum, Sudan), health workers went to schools in the morning and administered praziquantel to the SACs directly. In this study, we administered praziquantel to all primary school students regardless of the baseline prevalence of schistosomiasis in 2013, according to the schistosomiasis control protocol of the Sudanese government. The WHO dose pole was used to determine the dosage of praziquantel (40 mg/kg) for SACs [19]. The drug coverage rates among SACs were 92.1% in Al Jabalain and 82.3% in El Salam.
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of the Korea Association of Health Promotion (KAHP) (IRB approval no. 12-C-01) and received further ethical clearance from the Federal Ministry of Health of Sudan. Before the commencement of the study at each school, health workers explained the study objectives to the schoolmaster and teachers and obtained verbal informed consent from them prior to the recruitment of children. After that, verbal informed assent was obtained from each student with the presence of the schoolteachers. The requirement for written informed consent from each student was waived by the IRB. Data were collected from the primary-school students according to the IRB-approved framework.
Urine sample collection and examination
The prevalence and intensity of S. haematobium infection were assessed using urine samples collected from all students in 1st, 3rd, and 5th grade of each school. Containers were delivered early in the morning to the schools and collected on the same day (usually around 2–4 pm before children were leaving school). The collected samples were immediately transferred to Sudan-Korea Schistosomiasis Control Center established by the KOICA project (the SUKO Center) in Kosti district, White Nile State.
After collection, parasitological examinations were performed on the same day by laboratory technicians with>5 years of experience in urine and stool microscopy. S. haematobium eggs were detected in the urine samples via the urine centrifugation methods [13,20]. Specifically, 10 ml of urine in each tube was centrifuged at 1,500 rpm for 5 minutes at room temperature, and the sediments were transferred onto 2–4 glass slides to examine the whole pellet. The slides were examined via microscopy to detect and count S. haematobium eggs. The intensity of S. haematobium infection was expressed as geometric mean intensity (GMI) of eggs per 10 ml of urine (EP10) and classified into 2 categories: light intensity (EP10<50) and heavy intensity (EP10≥50) [20]. For quality control, 10% of slides were randomly selected and re-examined at the end of each day by parasitology experts who were blinded to the results of the first examination. In case of disagreement, the results were discussed with the concerned technician, and the discordant slides were re-examined until an agreement was reached.
Statistical analysis
SPSS version 24.0 software (SPSS Inc., San Diego, California, USA) was used to analyze the experimental data. Due to the deviation from a normal distribution, S. haematobium infection intensities were calculated as GMIs of EP10. Differences in continuous variables among groups were tested using the Mann-Whitney test and Student’s t-test. The reduction rate of prevalence and infection intensity was calculated by the following formula: reduction rate=(prevalence or infection intensity at baseline survey-prevalence or infection intensity at follow-up survey)/prevalence or infection intensity at baseline survey×100.
RESULTS
Reduction rate of prevalence after MDA intervention
The baseline prevalence of S. haematobium infection was 9.1% in Al Jabalain and 35.2% in El Salam. The overall prevalence was 19.9% at the baseline survey in 2013 and 3.6% at the follow-up survey in 2014, indicating an 82% reduction rate after MDA (P<0.001; 95% confidence interval [CI], 82–88%). The prevalence in Al Jabalain was reduced from 9.1% at the baseline survey to 1.8% at the follow-up survey, hence a reduction rate of 80.3% (P<0.001; 95% CI, 73–88%). In El Salam, the prevalence was 35.2% at the baseline survey, which was reduced to 5.5% at the follow-up survey, thus an 84.4% reduction rate (P<0.001; 95% CI, 86–92%). No significant differences in relative reduction of prevalence rates were observed between both districts (Table 2).
Table 2.
The prevalence rate of S. haematobium infection of children of sentinel primary schools at Al Jabalain and El Salam district at baseline and 8 months after MDA
| District | Variable | Baseline survey | Follow-up survey | Reduction rate (%) | 95% CI | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| No. exam | No. positive | % | No. exam | No. positive | % | |||||
| Al Jabalain | Unit | |||||||||
| Al Jabalain | 291 | 80 | 27.5 | 312 | 17 | 5.4 | 80.2 | 0.09–026 | <0.001 | |
| Assalaya | 250 | 28 | 11.2 | 300 | 7 | 2.3 | 79.2 | 0.08–0.44 | <0.001 | |
| Jazeera Aba | 129 | 4 | 3.1 | 148 | 0 | 0.0 | 100 | 0.996 | ||
| Joda | 300 | 3 | 1.0 | 305 | 1 | 0.3 | 67.2 | 0.03–3.15 | 0.332 | |
| Kenana | 451 | 18 | 4.0 | 300 | 2 | 0.7 | 83.3 | 0.04–0.70 | 0.015 | |
| Rabak | 211 | 16 | 7.6 | 307 | 3 | 1.0 | 87.1 | 0.04–0.42 | <0.001 | |
| Subtotal | 1,632 | 149 | 9.1 | 1,672 | 30 | 1.8 | 80.3 | 0.12–0.27 | <0.001 | |
|
| ||||||||||
| El Salam | Unit | |||||||||
| Al Rawat | 188 | 83 | 44.1 | 301 | 25 | 8.3 | 81.2 | 0.07–0.19 | <0.001 | |
| Al Zelit | 291 | 131 | 45.0 | 315 | 5 | 1.6 | 96.5 | 0.01–0.05 | <0.001 | |
| Al Naeem | 312 | 105 | 33.7 | 300 | 31 | 10.3 | 69.3 | 0.15–0.35 | <0.001 | |
| Al Kewaik | 150 | 33 | 22.0 | 304 | 2 | 0.7 | 97.0 | 0.01–0.10 | <0.001 | |
| Al Migainis | 211 | 54 | 25.6 | 305 | 21 | 6.9 | 73.1 | 0.13–0.37 | <0.001 | |
| Subtotal | 1,152 | 406 | 35.2 | 1,525 | 84 | 5.5 | 84.4 | 0.08–0.14 | <0.001 | |
|
| ||||||||||
| Total | Gender | |||||||||
| Boys | 2,127 | 424 | 19.9 | 2,328 | 88 | 3.8 | 81.0 | 0.12–0.20 | <0.001 | |
| Girls | 657 | 131 | 19.9 | 869 | 26 | 3.0 | 85.0 | 0.08–0.19 | <0.001 | |
| Age group | ||||||||||
| ≤9–year-old | 1,032 | 188 | 18.2 | 1,157 | 28 | 2.4 | 86.7 | 0.07–0.17 | <0.001 | |
| 10~12-year-old | 1,048 | 218 | 20.8 | 1,313 | 57 | 4.3 | 79.1 | 0.13–0.23 | <0.001 | |
| ≥13-year-old | 704 | 149 | 21.2 | 727 | 29 | 4.0 | 81.2 | 0.10–0.23 | <0.001 | |
|
| ||||||||||
| Total | 2,784 | 555 | 19.9 | 3,197 | 114 | 3.6 | 82.1 | 0.12–0.18 | <0.001 | |
The follow-up survey was conducted at 8 months after MDA. 95% CI; 95% confidence intervals.
Reduction Rate=(prevalence at baseline survey-prevalence at follow-up survey)/prevalence at baseline survey×100.
Reduction rate of infection intensity after MDA intervention
Table 3 shows the intensity of S. haematobium infection at the baseline and follow-up surveys in Al Jabalain and El Salam. The overall GMI for both districts was 17.3 EP10 at the baseline survey and 9.5 EP10 at the follow-up survey; thus, the overall reduction in GMI was 45%, showing a significant difference between the baseline and follow-up surveys (P< 0.001). The GMI of infection in Al Jabalain was reduced from 14.5 EP10 at baseline to 7.1 EP10 at 8 months of follow-up, accounting for 51.0% of relative reduction (P<0.001). In El Salam, the GMI of infection at baseline and at 8 months of follow-up was 18.5 and 11.2 EP10, respectively, which constituted 40% of relative reduction (P<0.001).
Table 3.
The geometric mean intensity of S. haematobium-infected children of sentinel primary schools at Al Jabalain and El Salam districts at baseline and 8 months of follow-up
| District | Variable | Baseline survey | Follow-up survey | Reduction rate | P-value | ||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| No. positive | GMI | No. positive | GMI | ||||
| Al Jabalain | Unit | ||||||
| Al Jabalain | 80 | 15.8 | 17 | 8.0 | 49.4 | <0.001 | |
| Assalaya | 28 | 10.8 | 7 | 7.8 | 27.8 | <0.001 | |
| Jazeera Aba | 4 | 22.8 | 0 | 0 | 100 | ||
| Joda | 3 | 12.6 | 1 | 2 | 84.1 | 0.31 | |
| Kenana | 18 | 8.0 | 2 | 4.9 | 38.8 | 0.01 | |
| Rabak | 16 | 28.1 | 3 | 5.2 | 81.5 | <0.001 | |
| Subtotal | 149 | 14.5 | 30 | 7.1 | 51.0 | <0.001 | |
|
| |||||||
| El Salam | Unit | ||||||
| Al Rawat | 83 | 24.8 | 25 | 10.4 | 58.1 | <0.001 | |
| Al Zelit | 131 | 17.4 | 5 | 3.5 | 79.9 | <0.001 | |
| Al Naeem | 105 | 18.7 | 31 | 19.6 | −4.8 | <0.001 | |
| Al Kewaik | 33 | 9 | 2 | 4.9 | 45.6 | <0.001 | |
| Al Migainis | 54 | 20.8 | 21 | 7.8 | 62.5 | <0.001 | |
| Subtotal | 406 | 18.5 | 84 | 11.2 | 39.5 | <0.001 | |
|
| |||||||
| Total | Gender | ||||||
| Boys | 424 | 17.8 | 88 | 12.3 | 30.9 | <0.001 | |
| Girls | 131 | 15.8 | 26 | 4.8 | 69.6 | <0.001 | |
| Age group | |||||||
| ≤9-year-old | 188 | 18.3 | 28 | 9.3 | 49.2 | <0.001 | |
| 10~12-year-old | 218 | 17.4 | 57 | 11.0 | 36.8 | <0.001 | |
| ≥13-year-old | 149 | 16.0 | 29 | 8.7 | 45.6 | <0.001 | |
|
| |||||||
| Total | 555 | 17.3 | 114 | 9.5 | 45.1 | <0.001 | |
GMI (Geometric mean intensity); Number of S. haematobium eggs per 10 ml of urine.
Reduction rate of infection intensity=(GMI at baseline survey-GMI at follow-up survey)/GMI at baseline survey×100.
As shown in Table 4, 7.7% of children had a heavy intensity of infection at the baseline survey (2.9% in Al Jabalain and 14.4% in El Salam). After MDA, the prevalence of heavy infection was significantly reduced in Al Jabalain (93.9% reduction rate, P<0.001) and El Salam (93.2% reduction rate, P<0.001) (Table 4).
Table 4.
The relative percentages of heavy and light intensities of S. haematobium infected children of sentinel primary schools at Al Jabalain and El Salam districts at baseline and 8 months of follow-up
| District | Variable | Baseline survey | Follow-up survey | Reduction rate (%) | 95% CI | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Total no. | Light infection (%) | Heavy infection (%) | Total no. | Light infection (%) | Heavy infection (%) | |||||
| Al Jabalain | Unit | |||||||||
| Al Jabalain | 291 | 18.6 | 8.9 | 312 | 4.8 | 0.6 | 92.8 | 0.06–0.30 | <0.001 | |
| Assalaya | 250 | 8.8 | 2.4 | 300 | 2.0 | 0.3 | 86.1 | 0.08–0.89 | 0.03 | |
| Jazeera Aba | 129 | 0.9 | 0.9 | 148 | 0 | 0 | 100 | |||
| Joda | 300 | 0.7 | 0.3 | 305 | 0.3 | 0 | 100 | |||
| Kenana | 451 | 3.1 | 0.9 | 300 | 0.7 | 0 | 100 | |||
| Rabak | 211 | 3.4 | 4.3 | 307 | 1.0 | 0 | 100 | |||
| Subtotal | 1,632 | 6.2 | 2.9 | 1,672 | 1.6 | 0.2 | 93.9 | 0.06–0.22 | <0.001 | |
|
| ||||||||||
| El Salam | Unit | |||||||||
| Al Rawat | 188 | 20.7 | 23.4 | 301 | 7.3 | 1.0 | 95.7 | 0.05–0.17 | <0.001 | |
| Al Zelit | 291 | 26.5 | 18.6 | 315 | 1.6 | 0 | 100 | |||
| Al Naeem | 312 | 21.2 | 12.5 | 300 | 6.3 | 4.0 | 68 | 0.31–0.69 | <0.001 | |
| Al Kewaik | 150 | 18.0 | 4.0 | 304 | 0.7 | 0 | 100 | |||
| Al Migainis | 211 | 14.7 | 10.9 | 305 | 6.9 | 0 | 100 | |||
| Subtotal | 1,152 | 20.8 | 14.4 | 1,525 | 4.5 | 1.0 | 93.2 | 0.10–0.18 | <0.001 | |
|
| ||||||||||
| Total | Gender | |||||||||
| Boys | 2,127 | 12.1 | 7.9 | 2,328 | 3.0 | 0.7 | 90.6 | 0.13–0.23 | <0.001 | |
| Girls | 657 | 12.6 | 7.3 | 869 | 2.9 | 0.1 | 98.4 | 0.02–0.08 | <0.001 | |
| Age group | ||||||||||
| ≤9-year-old | 1,032 | 10.8 | 7.4 | 1,157 | 2.2 | 0.3 | 96.5 | 0.04–0.12 | <0.001 | |
| 10~12-year-old | 1,048 | 13.0 | 7.8 | 1,313 | 3.5 | 0.8 | 89.3 | 0.14–0.29 | <0.001 | |
| ≥13-year-old | 704 | 13.2 | 8.0 | 727 | 3.4 | 0.6 | 93.1 | 0.07–0.23 | <0.001 | |
|
| ||||||||||
| Total | 2,748 | 12.2 | 7.7 | 3,197 | 3.0 | 0.6 | 92.7 | 0.11–0.18 | <0.001 | |
Light infection intensity (<50 EP10) and heavy infection intensity (×50 EP10) of S. haematobium infections.
Reduction rate=(% of heavy infection intensity at baseline survey-% of heavy infection intensity at follow-up survey)/% of heavy infection intensity at baseline survey×100.
DISCUSSION
Human schistosomiasis caused by S. haematobium is one of the major public health concerns in Sudan. Previous studies showed that the prevalence of S. haematobium infection in the White Nile State of Sudan was 28.5% [5], 45.0% [6], 21.9% [21], and 35.6% [22] in different survey areas and times. In this study, we compared changes in the prevalence and intensity of S. haematobium infection between Al Jabalain and El Salam districts of White Nile State before and after MDA intervention. Prior to the baseline survey of this study, SACs in Al Jabalain had received MDA interventions twice during the 4 years of the 1st phase of the KOICA project, while those in El Salam had not. In 2013, the baseline prevalence of S. haematobium infection was 35.2% in El Salam, which was similar to that in previous studies in the White Nile State [5,6,22], while the 2013 baseline prevalence in Al Jabalain was 9.1% due to previous MDA intervention within 4 years [5]. In this study, the reduction in the prevalence of infection after MDA was 80.3% in Al Jabalain and 84.4% in El Salam. Although both districts had different MDA histories, the chemotherapeutic effect of a single praziquantel MDA was both quite satisfactory based on the observed reduction rates of prevalence in both districts. Such reduction in the prevalence rate after MDA represents the proportion of cure among the infected population, and similar findings were observed across all sex and age categories. The reduction rate of prevalence after a single dose of praziquantel was similar to that of previous studies of SACs in Sudan and Burkina Faso [14,15].
Infection intensity–which is quantified by egg counts (GMI of EP10 in this study)–is an important index of schistosomiasis epidemiology. Egg counts can estimate the burden of infecting worms and represent the degree of morbidity by eggs in the bladder [23]. In this study, we used urine sedimentation method to detect and quantify the S. haematobium eggs. That is why urine filtration system is blocked easily due to many foreign substances in the urine collected at the survey sites due to the fallen bladder cells, crystals and so on [24]. Also, urine sedimentation method is higher detectability even if low number of parasites and economic than urine filtration method [20]. Our results showed that the reduction rates of infection intensity after MDA were 51.0% in Al Jabalain and 39.5% in El Salam. Unlike the results for reduction rates of prevalence, this study suggests relatively less reduction in infection intensity observed among the populations with heavier infection burdens. El Salam demonstrated a higher prevalence rate of urogenital schistosomiasis and higher EP10 counts than Al Jabalain. A single MDA produced a similar efficacy of reduction in the prevalence rate (i.e., cure rate) in El Salam, but a lower efficacy of worm reduction in the human body; this suggests that most of the children with a light burden of infection were cured by MDA and the proportion was similar in both districts, but heavy-burden cases remained uncured with lowered EP10 counts after MDA. Our findings indicate that a single MDA of a 40 mg/kg dose is less effective to cure a heavy burden of schistosomiasis and that repeated MDAs are recommended for control programs.
When we broke down the prevalence rates and egg counts by administrative unit in the districts, we found wide variations in findings in both localities. Even in Al Jabalain, there were administrative units with a low reduction rate of prevalence, such as the Joda and Al Naeem Administrative Units. A possible explanation might be an ongoing refugee immigration from South Sudan. Immigrants may influence the prevalence of schistosomiasis, so precautionary measures should be taken during refugee immigration and settlement. In interpreting the effects of MDA between the 2 districts, we also had to consider reinfection. We examined the urine microscopy results at 8 months after MDA, which was long enough to evaluate reinfection after MDA. A single 40 mg/kg dose of praziquantel is known to produce a 73.6% cure rate and a 94.7% egg reduction rate for S. haematobium infection [25]. The reduction in prevalence rate in our study was >80%, which is similar to the known cure rate [14,15]. However, the reduction in intensity rate (39.5% in El Salam and 51.0% in Al Jabalain) was much lower than the known 90% egg reduction rate. The egg passers after the MDA included treatment failure and reinfection cases without clear identification. In heavily endemic areas, children are more rapidly and heavily reinfected after chemotherapy because they are more exposed. The reinfection force is determined by the egg seeding amount within the local area [25]. In this study, the follow-up survey was conducted 8 months after the MDA–after the hot and humid rainy season and long summer vacation had passed. Thus, SACs might have come into contact with water (e.g., during swimming) more frequently, resulting in reinfection. This study also confirmed that the reduction in infection intensity was much less in Sudan than as expected. Therefore, repeated MDAs may diminish the reinfection force by reducing the egg seeding population and the total amount of egg production in a community. Once repeated MDAs start to effectively keep the egg seeding amount under the reinfection threshold, schistosomiasis may finally be eliminated.
This study has a few limitations. Although the follow-up data at 8 months after the MDA included both treatment failure and reinfection cases after medication, it was impossible to differentiate their impacts. The other limitation was the influence of immigrants from South Sudan who were included in the study population. This aspect warrants further study.
In conclusion, we compared the effects of MDA with praziquantel in regions that are geographically adjacent but profoundly different in terms of the baseline infection status of urogenital schistosomiasis. This study showed that praziquantel administration was equally effective in reducing the prevalence of S. haematobium infection regardless of the baseline prevalence levels in endemic areas; however, one MDA with a single dose of praziquantel was not sufficient to reduce a heavy intensity of infection. Thus, this study provides real site information about the reduction patterns of prevalence and infection intensity after praziquantel treatment in endemic regions with different baseline prevalence levels. Our findings clearly point to the importance of repeated MDA interventions in endemic areas, which will eventually contribute to schistosomiasis elimination.
ACKNOWLEDGMENTS
This study was funded by the Korea International Cooperation Agency (KOICA). The views, opinions, assumptions, or any other information set out in this article should not be attributed to KOICA or any person connected with them. This work was partly supported by research fund of Chungnam National University.
We appreciate all the staffs involved in “The Project for Combating Schistosomiasis in Sudan,” carried by Korea Association of Health Promotion (KAHP) and the Ministry of Health (MoH) of the White Nile State, Sudan. We are indebted to several colleagues at Ministry of Health of Sudan and Embassy of the Republic of Korea in Sudan. Also, we thank all primary school children and teachers of Al Jabalain and El Salam loclaities of White Nile State, Sudan. This project was supported by the Korea International Cooperation Agency (KOICA project no. P2015-00146-2) and implemented by the Korea Association of Health Promotion. This work was partly supported by research fund of Chungnam National University.
Footnotes
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
REFERENCES
- 1.Gryseels B. Schistosomiasis. Infect Dis Clin North Am. 2012;26:383–397. doi: 10.1016/j.idc.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Hotez PJ, Kamath A. Neglected tropical diseases in sub-Saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Negl Trop Dis. 2009;3:e412. doi: 10.1371/journal.pntd.0000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Fact Sheet on Schistosomiasis [Internet] Available from: http://www.who.int/mediacentre/factsheets/fs115/en/
- 5.Lee YH, Jeong HG, Kong WH, Lee SH, Cho HI, Nam HS, Ismail HA, Alla GN, Oh CH, Hong ST. Reduction of urogenital schistosomiasis with an integrated control project in Sudan. PLoS Negl Trop Dis. 2015;9:e3423. doi: 10.1371/journal.pntd.0003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ismail HA, Hong ST, Babiker AT, Hassan RM, Sulaiman MA, Jeong HG, Kong WH, Lee SH, Cho HI, Nam HS, Oh Ch, Lee YH. Prevalence, risk factors, and clinical manifestations of schistosomiasis among school children in the White Nile River basin, Sudan. Parasit Vectors. 2014;7:478. doi: 10.1186/s13071-014-0478-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abou-Zeid AH, Abkar TA, Mohamed RO. Schistosomiasis infection among primary school students in a war zone, Southern Kordofan State, Sudan: a cross-sectional study. BMC Public Health. 2013;13:643. doi: 10.1186/1471-2458-13-643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hajissa K, Muhajir AEMA, Eshag HA, Alfadel A, Nahied E, Dahab R, Ali SM, Mohammed M, Gaafar M, Mohamed Z. Prevalence of schistosomiasis and associated risk factors among school children in Um-Asher Area, Khartoum, Sudan. BMC Res Notes. 2018;11:779. doi: 10.1186/s13104-018-3871-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cha SM, Elhag MS, Lee YH, Cho DS, Ismail HA, Hong ST. Epidemiological findings and policy implications from the nationwide schistosomiasis and intestinal helminthiasis survey in Sudan. Parasit Vectors. 2019;12:429. doi: 10.1186/s13071-019-3689-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang Y, MacArthur C, Mubila L, Baker S. Control of neglected tropical diseases needs a long-term commitment. BMC Med. 2010;8:67. doi: 10.1186/1741-7015-8-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . Helminth Control in School Age Children: A Guide for Managers of Control Programmes. 2nd ed. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 12.Atalabi TE, Adubi TO. The epidemiology and chemotherapeutic approaches to the control of urinary schistosomiasis in school-age children (SAC): a systematic review. BMC Infect Dis. 2019;19:73. doi: 10.1186/s12879-018-3647-y. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 13.Atalabi TE, Adoh SD, Eze KM. The current epidemiological status of urogenital schistosomiasis among primary school pupils in Katsina State, Nigeria: An imperative for a scale up of water and sanitation initiative and mass administration of medicines with Praziquantel. PLoS Negl Trop Dis. 2018;12:e0006636. doi: 10.1371/journal.pntd.0006636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed AM, Abbas H, Mansour FA, Gasim GI, Adam I. Schistosoma haematobium infections among school children in central Sudan one year after treatment with praziquantel. Parasit Vectors. 2012;5:108. doi: 10.1186/1756-3305-5-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Touré S, Zhang Y, Bosqué-Oliva E, Ky C, Ouedraogo A, Koukounari A, Gabrielli AF, Bertrand S, Webster JP, Fenwick A. Two-year impact of single praziquantel treatment on infection in the national control programme on schistosomiasis in Burkina Faso. Bull World Health Organ. 2008;86:780–787. doi: 10.2471/BLT.07.048694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.King CH, Kittur N, Binder S, Campbell CH, N’Goran EK, Meite A, Utzinger J, Olsen A, Magnussen P, Kinung’hi S, Fenwick A, Phillips AE, Gazzinelli-Guimaraes PH, Dhanani N, Ferro J, Karanja DMS, Mwinzi PNM, Montgomery SP, Wiegand RE, Secor WE, Hamidou AA, Garba A, Colley DG. Impact of different mass drug administration strategies for gaining and sustaining control of Schistosoma mansoni and Schistosoma haematobium infection in Africa. Am J Trop Med Hyg. 2020;103(suppl):14–23. doi: 10.4269/ajtmh.19-0829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dejon-Agobé JC, Edoa JR, Honkpehedji YJ, Zinsou JF, Adégbitè BR, Ngwese MM, Mangaboula A, Lell B, Grobusch MP, Mordmüller B, Adegnika AA. Schistosoma haematobium infection morbidity, praziquantel effectiveness and reinfection rate among children and young adults in Gabon. Parasit Vectors. 2019;12:577. doi: 10.1186/s13071-019-3836-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayes RJ, Bennett S. Simple sample size calculation for cluster-randomized trials. Int J Epidemiol. 1999;28:319–326. doi: 10.1093/ije/28.2.319. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization . Prevention and Control of Schistosomiasis and Soil-Transmitted Helminthiaisis: WHO Tech Report Series No. 912. Geneva, Switzeland: World Health Organization; 2002. [PubMed] [Google Scholar]
- 20.World Health Organization . Basic laboratory methods in Medical Parasitology. Geneva, Switzeland: World Health Organization; 1991. pp. 33–35. [Google Scholar]
- 21.Ahmed ES, Daffalla A, Christensen NO, Madsen H. Patterns of infection and transmission of human schistosomiasis mansoni and schistosomiasis haematobium in White Nile Province, Sudan. Ann Trop Med Parasitol. 1996;90:173–180. doi: 10.1080/00034983.1996.11813041. [DOI] [PubMed] [Google Scholar]
- 22.Lee YH, Lee JS, Jeoung HG, Kwon IS, Mohamed AAWS, Hong ST. Epidemiological survey on schistosomiasis and intestinal helminthiasis among village residents of the rural river basin area in White Nile State, Sudan. Korean J Parasitol. 2019;57:135–144. doi: 10.3347/kjp.2019.57.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrade G, Bertsch DJ, Gazzinelli A, King CH. Decline in infection-related morbidities following drug-mediated reductions in the intensity of Schistosoma infection: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2017;11:e0005372. doi: 10.1371/journal.pntd.0005372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim MJ, Ryu K, Jin Y, Lee YH, Jeoung HG, Saeed AA, Kim SH, Hong ST. Significance of echogenic snow sign as an ultrasonography finding for diagnosis of urogenital schistosomiasis. Am J Trop Med Hyg. 2016;95:842–848. doi: 10.4269/ajtmh.16-0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zwang J, Olliaro P. Efficacy and safety of praziquantel 40 mg/kg in preschool-aged and school-aged children: a meta-analysis. Parasit Vectors. 2017;10:47. doi: 10.1186/s13071-016-1958-7. [DOI] [PMC free article] [PubMed] [Google Scholar]