Abstract
Thrombotic complications associated with coronavirus disease 2019 (COVID-19) have been described; these have mainly included venous thromboembolic events. Limited literature is available regarding arterial thrombosis. Acute limb ischemia is associated with severe complications that can result in significant morbidity and mortality. Herein, we report 3 cases of COVID-19 infection complicated by arterial thrombosis in the form of acute limb ischemia. Our case series adds to the limited literature regarding arterial thrombosis.
Case Report
The novel coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS COV-2) was declared a worldwide epidemic by the World Health Organization on March 11, 2020. Patients with COVID-19 usually present with respiratory symptoms like cough, fever, and shortness of breath, with 20% of cases being severe or critical.1 The data collected from multiple medical centers suggest a very high incidence of thromboembolic complication in patients hospitalized with COVID-19 including but not limited to pulmonary embolism, ischemic stroke, acute limb ischemia, and ischemic myocardial injury.1, 2, 3 Patients with abnormal coagulation studies at presentation are associated with worse outcomes. We report 3 cases of COVID-19 infection complicated by acute limb ischemia who presented to our institution over a span of 3 weeks (April 20–May 11, 2020).
Case 1
A 71-year-old female patient with history of Parkinson's disease, depression, and dementia who presented to the emergency department from long-term care facility with shortness of breath, cold painful lower extremities, and acute change in mental status. Vital signs on presentation were as follows: temperature, 36.8ºC; heart rate, 123 beats/min; blood pressure, 118/67 mm Hg; respiratory rate, 24 breaths/min; and oxygen saturation, 98% on supplemental oxygen. On examination, her bilateral lower extremities were mottled and cold, and her bilateral posterior tibial, popliteal arteries, and dorsalis pedis were not palpable. Her nasopharyngeal swap was positive for COVID-19 infection. On laboratory testing the following values were noted: white blood cells, 25.6K/mm3 (reference, 4.5–11K/mm3); hemoglobin, 12.7 g/dL (reference, 12–16 g/dL); hematocrit, 39.4% (reference, 36–46%); platelets, 191 (reference, 140–440K/mm3); glucose, 356 mg/dL (reference, 70–105 mg/dL); creatinine 1.32 mg/dL (reference, 0.6–1.30 mg/dL); blood urea nitrogen, 9.1 mg/dL (reference, 7–23 mg/dL); D-dimer, 9.9 (reference, <0.5); prothrombin time, 16.7 sec (reference, 12.2–14.9 sec); International Normalized Ratio (INR), 1.3 (reference, <1); partial thromboplastin time, −20.0 sec (reference, 21.3–35.1 sec); lactic acid, 4.6 mmol/L (reference, 0.5–2.2 mmol/L); C-reactive protein, 53.6 mg/L (reference, <10 mg/L); and erythrocyte sedimentation rate, 93 mm/hr (reference, 0–32 mm/hr). Computed tomography angiography showed complete occlusion above the level of the aortic bifurcation with no arterial flow to the lower extremities bilaterally (Fig. 1 ). The patient was started on heparin drip. Given the comorbidities and poor performance status, after discussion with the patient's family, no surgical intervention was done, and comfort care measures were initiated, and the patient expired.
Fig. 1.
Computed tomography angiography showed complete occlusion above the level of the aortic bifurcation with no arterial flow to the lower extremities bilaterally.
Case 2
A 70-year-old male patient with past medical history of hypertension presented to emergency department with right leg pain and swelling. COVID-19 was diagnosed on the basis of reverse transcription polymerase chain reaction testing in the prior week before presentation at a clinic. Vital signs on presentation were as follows: heart rate, 71 beats/min; blood pressure, 121/66 mm Hg; oxygen saturation, 100% on room air; and temperature, 36ºC. On examination, patient's right foot was cold, swollen, and absent right dorsalis pedis pulse. On initial laboratory evaluation, the following values were noted: hemoglobin, 12.9 g/dL (reference, 12–16 g/dL); hematocrit, 38.2% (reference, 36–46%); white blood cells, 6.9K/mm3 (reference, 4.5–11K/mm3); platelets, 178 (reference, 140–440K/mm3); potassium 4 mEq/L (reference, 3.5–5 mEq/L); glucose, 128 mg/dL (reference, 70–105 mg/dL); creatinine, 0.87 mg/dL (reference, 0.6–1.30 mg/dL); blood urea nitrogen, 9.1 mg/dL (reference, 7–23 mg/dL); D-dimer, 1.62 (reference, <0.5); prothrombin time, 13.5 sec (reference, 12.2–14.9 sec); INR, 1 (reference, <1); partial thromboplastin time, −32 sec (reference, 21.3–35.1 sec); and calcium, 8.5 mg/dL (reference, 8.6–10.3 mg/dL). Anticardiolipin IgM 15 MPL units/mL (reference, 0–12 MPL units/mL) was slightly increased and anticardiolipin IgG was within normal. Anti–β2-glycoprotein IgA, IgM, and IgG antibodies were within normal and lupus anticoagulant antibody was not done.
Peripheral angiogram showed 100% occlusion of right popliteal artery and organized clot in the tibioperoneal arteries (Fig. 2 ). The patient underwent thrombolysis with tissue plasminogen activator and next day stenting of the right tibioperoneal trunk was done (Fig. 3 ). The patient was discharged home in stable condition.
Fig. 2.
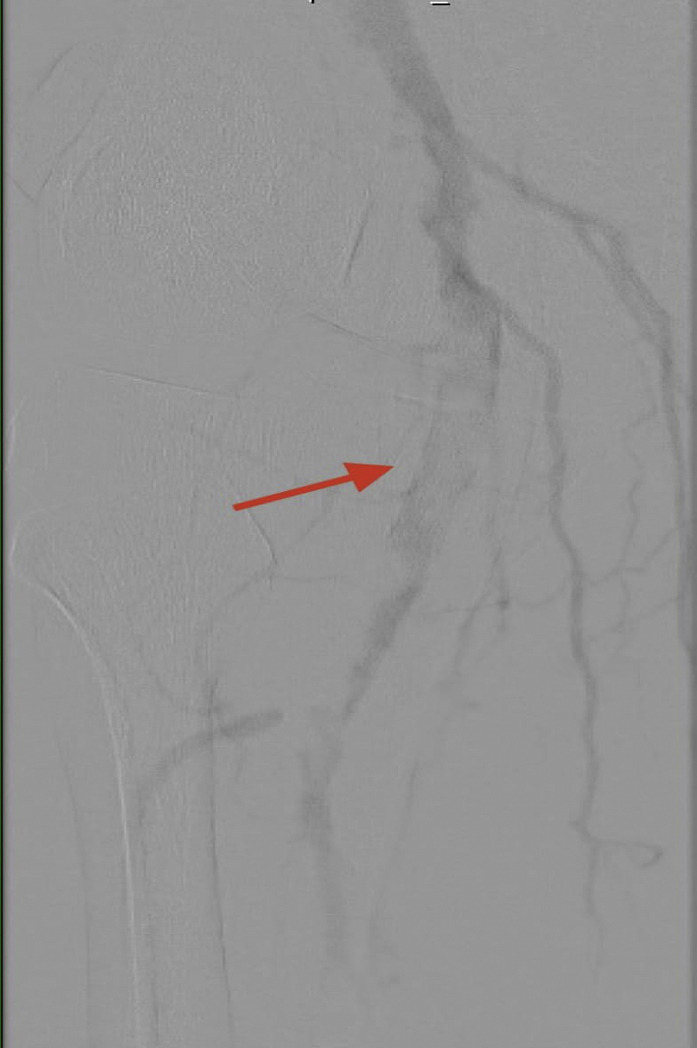
Peripheral angiogram showing clot in tibioperoneal trunk.
Fig. 3.
Peripheral angiogram before stenting of tibioperoneal trunk.
Case 3
A 70-year-old female patient with medical history significant for diabetes mellitus and hypertension who presented to the emergency department complaining of right lower extremity pain that had started 1 week prior and has been getting progressively worse. On review of systems the patient reported shortness of breath. Vital signs on presentation were significant for heart rate of 66 beats/min, blood pressure of 113/63 mm Hg, oxygen saturation of 85% on room air, and temperature of 35.9ºC. On examination, the right lower extremity was discolored, mottled, and cold to touch and right leg peripheral pulses were unpalpable. The rest of her physical examination was unremarkable. Laboratory evaluation showed the following results: hemoglobin, 9.9 g/dL (reference, 12–15.5 g/dL); white blood cell count, 22 × K/mm3 (reference, 4.5–11 × K/mm3); platelets, 195 (reference 140–440 K/mm3); Na, 133 mmol/L (reference, 135–145 mmol/L); potassium, 3.4 mmol/L (reference, 3.6–5.2 mmol/L); blood urea nitrogen, 45 mg/dL (reference, 6–23 mg/dL); creatinine, 0.94 mg/dL (reference, 0.5–1.04 mg/dL); aspartate transaminase, 132 U/L (reference, 10–50 U/L); alanine transaminase, 116 U/L (reference, 10–50 U/L); glucose, 600 mg/dL (reference, 70–99 mg/dL); anion Gap, 29 mmol/L (reference 10–19 mmol/L); and bicarbonate, 14 mmol/L (reference, 22–29 mmol/L). Chest X-ray showed bilateral ground glass opacities. A nasopharyngeal swap was positive for COVID-19. The patient underwent computed tomography angiography of the aorta and iliofemoral arteries, which showed complete occlusion of the right external iliac artery, right common femoral artery, right superficial artery, right deep femoral, and right popliteal artery (Fig. 4 ). She was hospitalized for critical right lower limb ischemia and was started on therapeutic heparin infusion. She underwent emergency right lower extremity anterior and lateral compartment fasciotomy, embolectomy of right iliac artery, superficial femoral artery, profunda femoris artery, and popliteal artery, right lower extremity through-knee guillotine amputation, and right common femoral and deep femoral artery endarterectomy. The patient had a complicated hospital course and had cardiac arrest because of hypoxia.
Fig. 4.
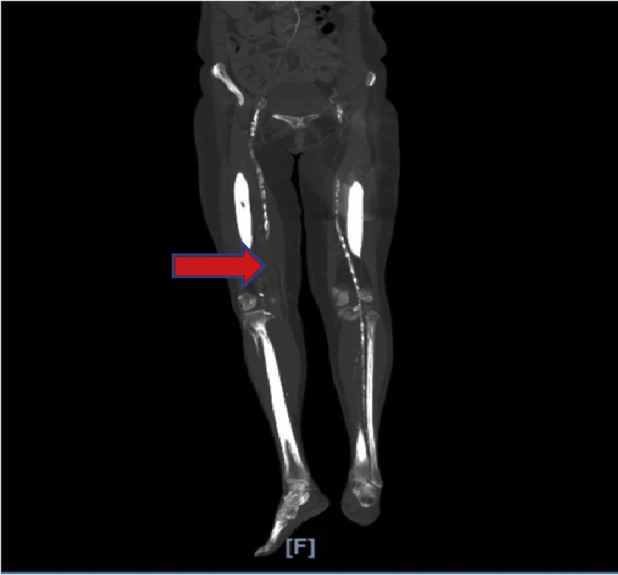
Computed tomography angiography of the aorta and iliofemoral arteries, which showed complete occlusion of the right common femoral artery, right superficial artery, right deep femoral artery, and right popliteal artery.
Discussion
Most patients hospitalized with COVID-19 who had thromboembolic complications developed deep vein thrombosis and pulmonary embolism. Arterial thrombosis has also been reported but less frequent.1 Patients with COVID-19 have abnormal levels of D-dimer, decreased prothrombin time, and increased activated partial thromboplastin time. Moreover, Tang et al.4 in their study found that 74% of patients who died of COVID-19 had disseminated intravascular coagulopathy. The incidence of acute lower limb ischemia in patients with COVID-19 is not well studied and limited data are available.
Acute limb ischemia is a vascular emergency and can result in severe morbidity, including chronic pain, limb loss, and severe disability. A prompt diagnosis is a prerequisite for successful treatment. An observational study done in Italy revealed increased incidence of acute limb ischemia in patients with COVID-19 infections, they have noted the number of patients with acute limb ischemia during the peak of the pandemic has increased by almost 8-fold compared with the same period of time in 2019.5 There is an overwhelming consensus to start patients hospitalized with COVID-19 infection on therapeutic or prophylactic dose of low-molecular-weight heparin or unfractionated heparin to prevent these complications.
The mechanism of thromboembolic complications associated with COVID-19 infection is not fully understood. COVID-19–related hypercoagulability is likely multifactorial—direct viral infection of the endothelial cell leading to diffuse endothelial inflammation, increased procoagulant factors such as factor VIII, von Willebrand factor, fibrinogen, and high inflammatory state associated with the cytokine storm leading to coagulation and fibrinolysis activation.6 Antiphospholipid antibodies were also detected in a number of patients with COVID-19; however, it is unclear if they play a role in the thromboembolic complications associated with the disease.2 , 7 As the cases of COVID-19 continue to increase throughout the world, there is an increasing need for more studies, to form guidelines for the prevention and treatment of thromboembolic complications of COVID-19.
Conclusions
We report 3 cases of arterial thrombosis in patients with COVID-19. Our cases and review of the literature reveal that health care providers should be aware of the life-threatening manifestation of COVID-19 so that appropriate measures could be taken.
Footnotes
Conflict of interests: None of the authors have any conflict of interests to report.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Kaur P., Qaqa F., Ramahi A. Acute upper limb ischemia in a patient with COVID-19. Hematol Oncol Stem Cel Ther. 2020 doi: 10.1016/j.hemonc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helms J., Tacquard C., Severac F. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaur P., Posimreddy S., Singh B. COVID-19 presenting as acute limb Ischaemia. Eur J Case Rep Intern Med. 2020;7:001724. doi: 10.12890/2020_001724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang N., Li D., Wang X. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellosta R., Luzzani L., Natalini G. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panigada M., Bottino N., Tagliabue P. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18:1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh B., Kaur P., Ajdir N. Covid-19 presenting as acute limb ischemia. Cureus. 2020;12:e9344. doi: 10.7759/cureus.9344. [DOI] [PMC free article] [PubMed] [Google Scholar]




