The SARS-CoV-2 virus has caused a worldwide pandemic, affecting nearly every aspect of the lives of individuals, communities, and nations. For radiation oncology (RO) departments, the need for social distancing has translated into policies limiting in-person interactions and restricting companions. These restrictions have been distressing for many but may take a particular toll on patients with low health literacy (LHL) and limited English proficiency (LEP). As the world of medicine after COVID-19 comes to rely more heavily on technology to connect patients and providers, disparities in access and barriers to use of health information technology may create an additional layer of complexity for patients receiving radiation. Thus, if telemedicine technology becomes the new post–COVID-19 normal, it is important that we approach these new processes with a health equity lens. We may otherwise compound the already disproportionate effects that the virus has had on underserved minority racial and ethnic communities.
Although cancer treatments within the United States have improved over the past decade through advances in radiation, surgical, and systemic treatments, not all patients have benefited equally. Ethnic and racial minorities underrepresented in medicine (UIM) continue to experience worse outcomes compared with their white counterparts.1 This problem is deepened by the higher levels of LHL and LEP found among UIM, factors that negatively affect health care use, patient–provider relationships, self-care, and quality of life (QoL) among patients with cancer.2 In the United States, the consequences will be further amplified as the proportion of UIM within the population is projected to increase to 40.1% in 2030 and 50.4% in 2060.3
Many studies have highlighted inequalities faced by UIM communities owing to diminished access to radiation therapy and the need for systematic changes to address these inequities. When focusing on Hispanic Americans, it has been reported that those born outside the United States or those with LEP were more likely to experience difficulties seeking appropriate care.4 LEP patients with head and neck cancer treated by radiation were less likely to undergo chemoradiation (60% vs 83.8%; P = .028) and had lower locoregional control (58.3% vs 82.2%; P = .098) than English-proficient patients, regardless of race or ethnicity.5 In the 2013 World Health Organization report “Health Literacy: The Solid Facts,” the authors warned of LHL among immigrant populations, with the US Department of Health and Human Services recommending LHL interventions be evidence based, culturally adapted, and led by health professionals.6 During the COVID-19 pandemic, it has similarly become clear that the social determinants of health are intimately intertwined with the higher incidence and mortality for Black and Hispanic communities, unmasking disparities that cannot be ignored in the post–COVID-19 world.
COVID-19 and the urgent need for physical distancing pushed the medical world to rapidly adopt virtual technologies. Digital platforms, in the short term, enable patients and providers to stay safe and connected and may also benefit patients and health care teams in the years to come. Virtual platforms may reduce time off work and transportation costs. Similarly, they may decrease the burden on those with diminished ability to travel owing to caregiving responsibilities or cancer-related symptoms and increase access for those who live farther from urban areas.
However, not all may benefit equally because we also face a “digital divide.” Older Black and Hispanic patient populations in particular are less likely to use technology for health-related purposes, even when taking demographics and education into account.7 Such patients are also less likely to supplement their knowledge by using publicly available online resources.8 For these patients, going “virtual” risks making their understanding of radiation and the management of treatment-related adverse effects even more difficult, particularly for those with LEP or LHL.9
RO departments will have to be conscious of this problem to prevent exacerbation of existing disparities as they develop their post–COVID-19 telemedicine processes. By acting early and proactively, we can prioritize patient-centered care through shifting the responsibility of navigating LEP and LHL from individuals to institutions. Organizations will need to identify and target those needing LHL and LEP interventions. Studies in cancer care have shown that addressing LHL translates into better QoL, perhaps through improved self-care practices.2
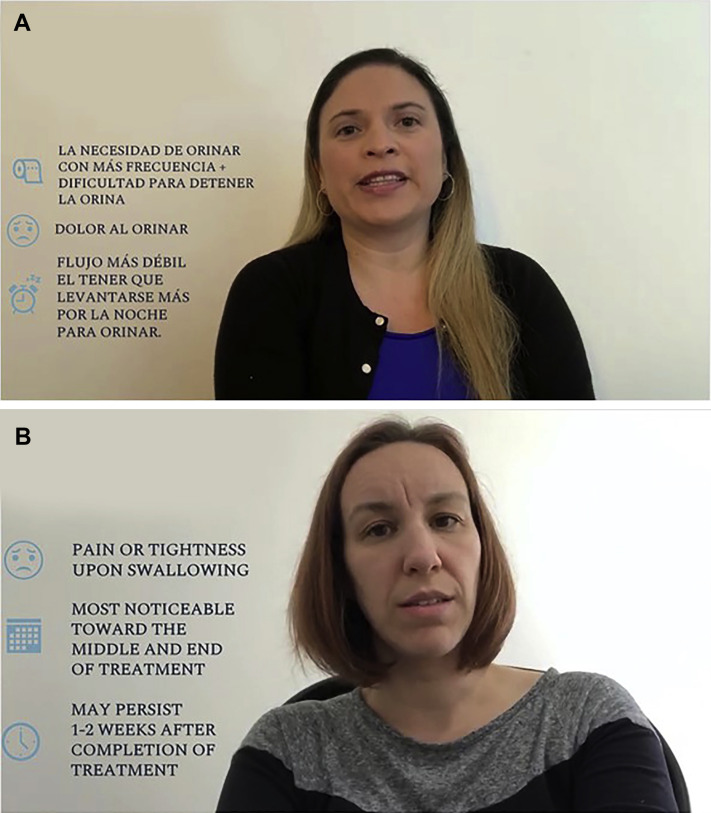
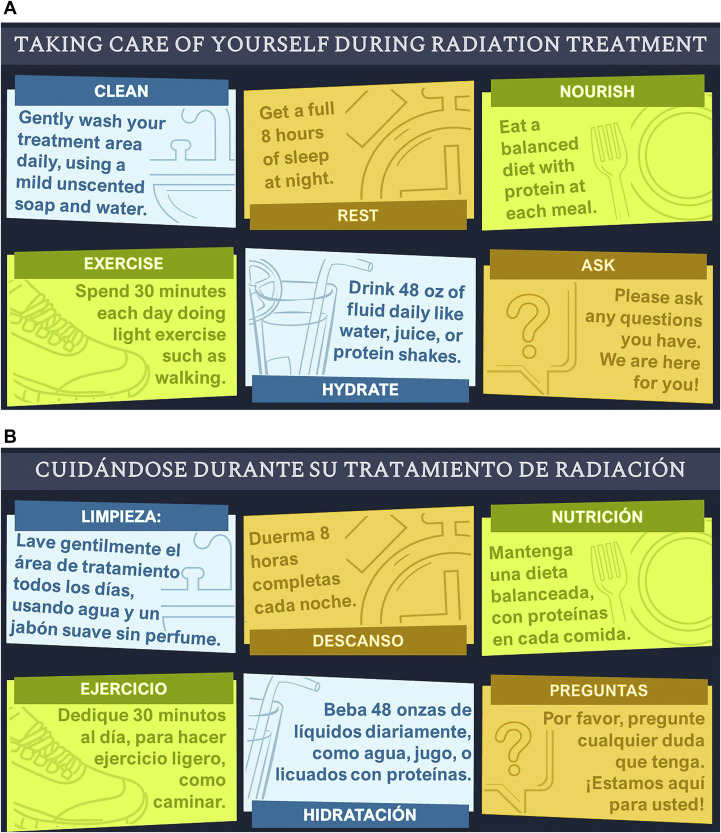
In our own department, as the COVID-19 pandemic surge occurred, we formed a multidisciplinary patient education task force composed of a nurse practitioner, nurse director, RO resident, communications manager, and the administrative director of finance and business operations. The objective was to develop simple and comprehensible patient education tools to assist patients through radiation. Videos (Fig. 1 ) and infographics (Fig. 2 ) in both English and Spanish were created describing expected side effects of radiation and providing guidance about symptom management. Infographics outlined key topics in self-care during treatment and symptoms to report to the treatment team. Videos included the most common side effects reported during radiation: (1) fatigue, weakness, dizziness, and lightheadedness; (2) urinary symptoms; (3) skin care; (4) esophagitis and difficulty swallowing; (5) diarrhea; and (6) pain. The infographics were displayed on a large digital screen in the waiting room, and videos were embedded within a virtual patient treatment guide, accessible from the hospital website. Video transcripts were developed by nursing staff and translated into Spanish by a native Spanish-speaking resident. Pictures and key words were added to increase patient engagement and understanding.
Fig. 1.
Patient educational videos on self-care during radiation. (A, top) In Spanish, done by a radiation oncology resident. (B, bottom) In English, done by a radiation oncology nurse practitioner.
Fig. 2.
Patient infographics depicting self-care during radiation, developed by a multidisciplinary radiation oncology team, displayed on a large digital screen in the treatment waiting area. (A, top) English. (B, bottom) Spanish.
These, however, are small first steps. Multidisciplinary task forces will be vital in instituting a number of other interventions, including expanding the menu of readable consent forms and patient educational materials using multiple platforms in a variety of languages. Beyond this, multidisciplinary efforts to recognize and intervene on inequities in digital literacy are required. Many departments are screening patients for SARS-CoV-2 infections, but screening for LHL, LEP, and telemedicine access is also essential in improving patient care. For patients who are identified as having access to a computer and quality Internet but low technological proficiency, “telemedicine navigators” can help walk them through use of telemedicine platforms, allowing more patients to be “seen” via video. Dedicated telemedicine support and training focused on providers can also increase provider comfort, efficiency, and quality of care and assist in integrating available services, such as interpretation. Providing both patients and providers with early access to preemptive troubleshooting can allow for the successful adaptation of telemedicine to everyday practice. Addressing these issues may allow those who would traditionally be seen as “late adopters” of technology to embrace telemedicine more quickly by providing them the tools to deal with the technical difficulties associated with use of new technology.
Nevertheless, the deepest systemic problems lie furthest from the reach of the medical professionals. Video telemedicine, no matter how good it is for many of our patients, cannot work for those who have no access to the Internet, private spaces, or technology. Our siloed effort must expand beyond the walls of our hospitals to affect the policies needed to support access to telemedicine for patients, including federal and state efforts to expand and decrease the cost of broadband access. As intermediate measures, we should work to improve patient access to telemedicine via vouchers for broadband access, analogous to ongoing hospital provision of parking, transportation, and lodging assistance. Social workers could also help identify suitable public Internet-equipped spaces, providing a list to patients in the way that they currently provide lists of affordable lodging resources. Other innovative, multidisciplinary solutions tailored to specific contexts will prevent patients from being left behind during the telemedicine transition.
We must also not forget that a subgroup of patients, regardless of provider, hospital, and system-wide efforts, will still be unable to access new technologies. Overlooking the possibility of integrating existing technologies, such as text messaging systems, or disincentivizing use of telephone encounters through lack of reimbursement parity systematically prioritizes patients with access to newer technology. Regular mobile phones are often more widely accessible than smartphones, particularly for those with LEP and LHL, and should be used to their full potential. Innovative strategies using existing technologies are possible. One such solution is the creation of an “on-call messaging” platform that patients can access via text messages from their mobile phones. Providers might be able to sign into such a system and receive texts from patients in their native languages, using already available text-translation services, to facilitate communication. Text messaging can also be used for patients who may not feel comfortable with patient portal platforms to provide reminders, self-care tips, and other instructions to improve patient engagement, awareness, and QoL.
Disparities in access to radiation therapy were a pervasive problem before COVID-19. Without active and deliberate steps to incorporate equity into the innovations and technologies that are implemented during and after the pandemic, the gap in access to care and cancer outcomes will only continue to perpetuate the inequities that have so clearly become apparent in the world we live in today.
Acknowledgments
We thank Tiffany Koolakian, Gregory Conklin, Cynthia Bowes, Brenda Silvia, and all the nurses and nurse practitioners at the Massachusetts General Hospital Department of Radiation Oncology for their assistance in creating the educational materials used in the patient videos.
Footnotes
Idalid Franco and Subha Perni made equal contributions to this study.
Disclosures: none
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Halverson J.L., Martinez-Donate A.P., Palta M. Health literacy and health-related quality of life among a population-based sample of cancer patients. J Health Commun. 2015;20:1320–1329. doi: 10.1080/10810730.2015.1018638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vespa J., Armstrong D.M., Medina L. US Department of Commerce, Economics and Statistics Administration, US Census Bureau; Washington, DC: 2018. Demographic turning points for the United States: Population projections for 2020 to 2060. [Google Scholar]
- 4.McClelland S., III, Perez C.A. The pervasive crisis of diminishing radiation therapy access for vulnerable populations in the United States—part 3: Hispanic-American patients. Adv Radiat Oncol. 2018;3:93–99. doi: 10.1016/j.adro.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qureshi M.M., Romesser P.B., Jalisi S. The influence of limited English proficiency on outcome in patients treated with radiotherapy for head and neck cancer. Patient Educ Couns. 2014;97:276–282. doi: 10.1016/j.pec.2014.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernández-Gutiérrez M., Bas-Sarmiento P., Albar-Marín M.J. Health literacy interventions for immigrant populations: A systematic review. Int Nurs Rev. 2018;65:54–64. doi: 10.1111/inr.12373. [DOI] [PubMed] [Google Scholar]
- 7.Levy H., Janke A.T., Langa K.M. Health literacy and the digital divide among older Americans. J Gen Intern Med. 2015;30:284–289. doi: 10.1007/s11606-014-3069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell U.A., Chebli P.G., Ruggiero L. The digital divide in health-related technology use: The significance of race/ethnicity. Gerontologist. 2019;59:6–14. doi: 10.1093/geront/gny138. [DOI] [PubMed] [Google Scholar]
- 9.Williams R., Moeller L., Willis S. Barriers and enablers to improved access to health information for patients with low health literacy in the radiotherapy department. Radiography (Lond) 2018;24:S11–S15. doi: 10.1016/j.radi.2018.06.010. [DOI] [PubMed] [Google Scholar]