Introduction
The COVID-19 pandemic has dramatically and permanently disrupted global life. Hospitals throughout the world have experienced a surge of COVID-19 cases, requiring the rapid expansion of hospital capacity and redeployment of medical staff. Moreover, the widespread closure of nonessential businesses has led to record unemployment and a global economic downturn. As of this writing, our employer, Northwell Health in New York State, has diagnosed over 40,000 COVID-19 patients and had greater than 18,000 COVID admissions across our 19 hospitals.1 As a result, routine ambulatory medical care has slowed considerably, with a collateral impact on general health that will be significant and long lasting.
In this manuscript, we outline our thesis regarding the pandemic’s effects on our specialty. First, we believe that radiation oncology will prove clinically resilient with a potential expanding role in cancer management. Second, we are concerned about access to cancer care for reasons that include but are not limited to patients’ hesitance to interact with health care staff, delays in cancer screening and surgery, and financial limitations related to patient insurance coverage and the financial instability of radiation practices themselves. Third, we believe that the pandemic will drive rapid adoption of technology and innovations that improve access to cancer care.
Impact of Pandemic on Cancer Care
Just a few months ago, we were celebrating encouraging news about declining cancer death rates in the United States. From 2008 to 2018, the death rate for all cancers decreased annually by about 1.4% in females and 1.8% in males.2 The driver of that success was a combination of factors including prevention, screening, and treatment, representing a massive effort of health policy and advances in therapy. Despite these gains, estimated cancer deaths this year will exceed 600,000 individuals and will sit alongside cardiovascular diseases as the top 2 causes of death in the United States.
Decline in cancer clinic visits, screening, and diagnosis
On March 11, the World Health Organization declared COVID-19 a pandemic; on or around March 13, 2020, hospitals nationally started cancelling elective surgical and interventional procedures. Outpatient radiology and endoscopy suites closed. The impact of the pandemic on cancer care was immediate. Community cancer practices saw a 40% decline in new patients between February and April of 2020, with an associated 17% decline in chemotherapy use and up to an 80% rate of cancellation or no-shows for follow-up visits.3 Additionally, in March 2020 there was a precipitous drop in cancer screenings by as much as 94% for colon, cervix, and breast cancers.4
Patient fears and financial concerns
Communities throughout the country implemented strict stay at home and social distancing policies. As the pandemic spread, we learned that older patients with comorbidities were at greatest risk of complications due to COVID-19.1 The general public, including patients with cancer, understandably has become fearful of visiting hospitals and clinics for medical care.
Beyond the effects of COVID-19 on patients’ willingness to interact with health care settings, unprecedented unemployment will place added stress on oncology practices by shifting insurance coverage to exchange products or Medicaid, which have lower reimbursement rates. A shift in payer mix will undoubtedly reduce medical practice incomes. Furthermore, unemployed patients may be unable to afford out-of-pocket costs. In 1 survey of over 1200 patients with cancer conducted by the American Cancer Society, 38% of respondents reported an impact of the COVID-19 pandemic on their ability to pay for care.5 An update of this survey found that 46% of respondents reported a change to their financial situation that affected their ability to pay for care,6 23% are worried about losing health insurance, and 32% are worried about affording basic household expenses. The combination of patient fear and the financial toxicity of health care will contribute further to the delay of patients seeking cancer screening and cancer care.
Impact of delays in care
The impact of delayed cancer care is difficult to estimate. One study that attempted to calculate the impact of surgical cancellations found that 3- and 6-month delays in cancer surgery were associated with 5% and 11% increases in cancer deaths, respectively.7 Delays in diagnosis and timely treatment may lead to stage migration and ultimately lower rates of cancer cure.8 Dr Ned Sharpless, director of the National Cancer Institute, recently expressed concerns that “in 2021 or 2022 or 2023, we will have the first Annual Report to the Nation since 1993 that shows an increase in cancer mortality.”9
Immediate Impact of Pandemic on Radiation Oncology
Having worked through the New York surge of COVID-19 in March and April 2020, we have learned that radiation oncology is resilient relative to surgery and chemotherapy. Throughout this crisis, our radiation medicine department has consistently maintained safe, timely, and evidence-based standards of care with a very low staff and patient infection rate. As described earlier, surgery was all but shut down for 2 months. Systemic chemotherapy remains available, but multiple reports now show an increased risk of death from coronavirus among patients who traditionally receive more aggressive chemotherapy,10 including those with hematologic cancers,11 lung cancer, and metastatic cancer.12 Targeted therapies and immune checkpoint inhibitors do not appear to be associated with higher risk of death.13 Radiation therapy for solid tumors has not been shown to increase a patient’s risk of dying from coronavirus.
Standard fractionation remains our preferred evidence-based approach
Early in the pandemic, a number of organizations published disease-specific guidelines for radiation therapy practice modifications in the midst of this pandemic.14 Hypofractionation and decreased use of concurrent radiosensitizing chemotherapy were the focus of many of these reports. As we enter the third month of this pandemic, we have found that most patients can be safely treated with standard-of-care radiation fractionation, especially in diseases for which evidence-based use of hypofractionated regimens for curative intent do not exist. For example, most aerodigestive tract head and neck cancers require standard fractionation to doses between 60 and 70 Gy for cure, with concurrent chemotherapy. We believe that standard fractionation should continue in the appropriate patient populations wherever possible. One exception may be in lung cancer; several reports indicate increased mortality from COVID-19 in this patient population, and a change in practice to reducing the length of treatment may be beneficial.15
Where there is a high level of evidence for hypofractionation in other common disease sites, including prostate, breast, and glioblastoma, we continue to frequently employ hypofractionation, as we have previously published.16 In our experience, there is a very low rate of COVID-19 in patients undergoing weeks of radiation therapy, provided they are following recommendations for mask-wearing, hand hygiene, and physical distancing. Likewise, we have not seen any nosocomial spread despite treating COVID-19–positive patients.
Radiation prevails when hospital resources are limited
Rescheduling of delayed screenings and surgery will likely take many months, if not longer, to catch up, because ambulatory health care was operating at near-capacity before COVID-19. In an effort to triage this backlog, multidisciplinary management can guide patients toward radiation therapy for diseases where outcomes of radiation are equivalent to surgery. For example, radiation alone is appropriate for prostate and early-stage oropharynx cancers. Redirecting patients to radiation therapy will free up surgical capacity for malignancies such as colon cancer and melanomas that are surgically cured without acceptable nonsurgical alternatives.
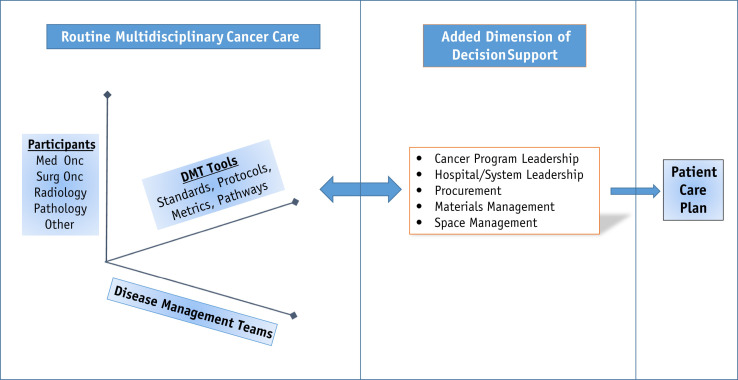
To operationalize this type of decision-making, we would suggest a 3-dimensional multidisciplinary approach to cancer treatment decisions, where unbiased leaders can take into account the patient queue and resource availability to facilitate optimal clinical outcomes (Fig. 1 ). The usual division of cancer into disease teams for multidisciplinary treatment decision-making is helpful and necessary, but it loses the broader perspective of resource availability within the health care entity. As surgery reopens, triage of the extensive backlog requires high-level awareness of available resources. Although we believe this “Resource-Allocating Multidisciplinary Approach” would be effective, we are realistic in noting that traditional issues of politics and turf within the house of medicine could prevent this model’s success. Nevertheless, if resources were to become severely limited, we believe this approach could have the greatest effect on the outcome of a large population of patients with cancer, rather than just the patient at hand.
Fig. 1.
Traditional model of multidisciplinary cancer management layered with the additional dimension of resource allocation as a driver for treatment selection.
Preparing for a value-based future helps weather the COVID-19 crisis
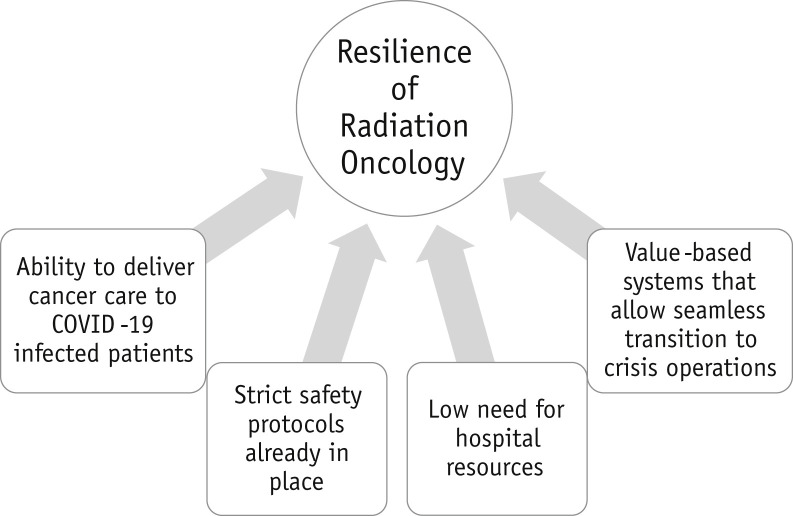
Over the past decade, our department has instituted systems and standards to prepare for a value-based future of health care.17 , 18 These include our centralized cloud-based treatment planning, remote access to programs for all physicians and physicists, evidence-based and consensus-driven treatment directives,19 an electronic whiteboard,20 and other processes to improve safety21 and efficiency.22 , 23 This structure created standards and expectations of the staff and an operating culture that served as the foundation during the current crisis (Fig. 2 ). Our crisis management team could then focus on instituting pandemic-related policies, including universal masking, screening for symptoms by phone and in person at each reception desk, cleaning routines, telehealth, and expanded work from home. Our culture of safety and teamwork allowed staff to focus on high-quality patient care.
Fig. 2.
Value of radiation oncology during COVID-19.
Communicating with patients
Telemedicine has proven its value during this crisis, and we would not be the first or last to suggest that it will have a permanent place in radiation oncology. Although we believe there is value to a face-to-face interaction with our patients, radiation oncology uniquely requires in-office patient presence for treatment simulation, thus allowing a virtual consultation as an introduction and the presimulation office visit as a built-in opportunity to address questions and to review the care plan. An added benefit of telehealth includes the participation of other colleagues as part of a multidisciplinary consult or inclusion of other family members from other parts of the country. There is still much to learn; techniques for making the most of telehealth, and establishing protocols for various cancers, are necessary to correctly assess our patients’ needs. Our department has created telehealth protocols encompassing all cancer diagnoses and types of visits (manuscript submitted).
Market research has demonstrated that patients are currently reticent about interfacing with health care settings (unpublished data). Some of this change in attitude may be transient, but it remains paramount that we share our experiences of safe cancer care to help allay these fears. Assurances that we have created a safe environment (with universal masking, physical distancing, abundant hand sanitizer, and frequent cleanings) has in a way redefined the definition of “safety” in our departments, where we generally think of risk associated with clinical treatment errors. Establishing new metrics for quality of radiation oncology care, such as rate of emergency room visits and hospitalizations during treatment that result from hypermanagement of our patients, will be key toward establishing patient trust. Another quality indicator could be the number of staff interactions associated with an office visit. Finally, basic metrics such as wait times become all the more meaningful in this new environment.
What Is the Future of US Health Care Under COVID-19?
Health care at the end of 2020 and beyond will look significantly different than it did at the end of 2019. Until a vaccine is developed and widely implemented, COVID-19 modeling shows several waves of viral persistence for some time to come,24 occupying both inpatient and outpatient resources across all of health care. We believe that radiation oncology and health care will see permanent changes as a result of this pandemic.
Radiation oncology must recommit to high value care
In the long term, we believe that radiation oncology is clinically resilient to COVID-19. We will continue to offer patients access to modern, uncompromised, evidence-based cancer care. In the short term, radiation oncology practices face significant financial risks associated with the slowing of new patient referrals secondary to lower cancer screening and surgery.
From a high-level perspective, the COVID-19 crisis has laid bare the frailties of the US health care system that will have a direct impact on radiation oncology practices. Specifically, we will see financial instability25 , 26 for practices caused by (1) delays in cancer diagnosis and treatment, (2) drastically reduced referrals, and (3) insurance shifts toward public payers. This loss of revenue, along with the macrolevel competition for capital throughout the health care system, will translate into fewer opportunities for oncology practices to make large investments. Looking ahead, there will be a need for fair and balanced resource allocation for both COVID-19 and routine health care (which includes screening and treatment of cancer).
The typical business model of capital expense depreciated over time represents a vulnerability to radiation oncology. Our machines are expensive. Medical oncology, on the other hand, has minimal capital investment requirements for infusion chairs and chemotherapy is reimbursed for each administered treatment without upfront capital. Given the new economic realities we will all be facing, we believe this pandemic presents an opportunity for our field to fully commit to the concept of high-value radiation oncology care.27 We must reconsider the marginal benefits of expensive technologies, including proton beam therapy and magnetic resonance imaging linear accelerators. High-value care requires that we stop the “technology arms race” under the guise of improved outcomes—unless and until trial data clearly identify the value of these tools. We should redirect funds and resources to other areas of our practice where they make more of an impact. Our time is better spent advocating for innovations in care delivery that maximize value. For example, after years of failed efforts, we should collectively develop policies that direct our vendors to establish interoperability requirements for the equipment and software that will tangibly lead to higher quality, efficiencies, and above all, enhanced safety. Likewise, technologies such as autosegmentation and AI-based planning software will likely prevail as winners.
Health care is at a turning point
We foresee the COVID-19 crisis creating a deeper divide in the US 2-tiered system of cancer care. Population-level cancer mortality will rise, while pockets of excellent care will continue to reflect the best cancer care available anywhere in the world. Despite the COVID-19 crisis bringing these inequalities to the front of our minds, we do not see any short-term plans for our nation to address health care disparities in a meaningful way. How much will our disease outcomes have to worsen before we make structural changes?
Out of the depths, the phoenix will rise. We foresee rapid technological adoption and innovation across the health care continuum. Technology enhances access. The pandemic has proven the value of technology in our personal lives, allowing us to successfully work from home, order food and groceries, and connect with colleagues around the world. We have seen technology’s positive impact in telemedicine as the primary and most obvious change and in virtual care tools such as mobile patient-reported outcome and symptom management applications. Technology also helps physicians access each other, through virtual tumor boards, conferences, websites, and social media that allow geographically dispersed clinicians to seek their colleagues’ expertise. We have already seen in our own multidisciplinary cancer center, for example, that work from home and video-conferencing platforms have enabled easier collaborative evaluation of imaging studies between physically distant physicians.
We believe that this pandemic will only further accelerate the rapid adoption of technology into health care. Health care has been operating in an analog era, with overreliance on in-person patient management and physician conferences and tumor boards. With the adoption of tech into health care, the natural outcome is new models of care. For example, patients can consult clinicians anywhere in the country; physicians can then connect with one another, and that patient’s care can be delivered locally without ever physically meeting the prescribing or treating doctor.
We also anticipate that technology adoption will force new payment models. The Center for Medicare and Medicaid Services has already significantly modified payments for evaluation and management visits to facilitate telemedicine. CMS and commercial payers should similarly appreciate the role of virtual nonaudio/video care in high-value medicine. Payers would be wise to incorporate tech-enabled virtual patient management, virtual tumor boards and conferences, and physician-to-physician “telemedicine” in their payment structures. Virtual care allows patients anywhere to have access to expert clinicians, ancillary staff, evidence-based guidelines for care and efficient systems that have worked in specific centers. In addition, virtual care allows greater access to clinical trials that are currently unavailable to the vast majority of Americans.
We believe that technology-enabled patient care and clinician communication can improve access to all forms of medical care, including radiation therapy. We have a moral imperative to come out of this crisis with innovative ways of improving the glaring disparities in health care in this country. Will our specialty remain complacent with the status quo of access to radiation therapy, where low-income inner-city and rural communities have disproportionally less access to care and significantly worse outcomes? Will we stay silent amid a 2-tiered health system where city- and state-run systems cannot afford the basic technology requirements needed to meet certain standards of care? The lack of innovation with regard to care delivery perpetuates inequalities and a system where some patients are only offered outdated forms of cancer care.
The unknowns still remain. As in other times of crisis, larger health systems are more likely to weather the financial setbacks and emerge stronger in the long run. Will there be further health care market consolidation under the umbrella of large health care entities or private equity firms? How many Americans will lose access to employer-based health insurance? Furthermore, how will the nationwide lockdown and lack of recreational arenas affect the general health of populations? Will we see an increase in diseases associated with sedentary lifestyles? What will be the impact on mental health?28
Conclusions
The COVID-19 pandemic will have a long-lasting effect on cancer care. In the immediate short term, we must inspire confidence in our patients that health care is safe and that they continue with routine care, including health screenings. Although the immediate crisis management discussions in radiation oncology revolved around how to shorten treatment courses, we now appreciate that such compromises are not necessary. Standard evidence-based care outside of clinical trials can be used safely without the need to improvise new treatments. Radiation oncology is well positioned to continue curative care and to help load balance when considering health care resource limitations. Our participation at multidisciplinary conferences, advocating for the opportunity that our specialty provides for safe treatments, is vital if we are to maintain the success of lower cancer mortality over time. This pandemic has revealed major shortcomings in our public health infrastructure and health care at large. We have a responsibility as a specialty to think big. We must innovate so that cancer care and radiation therapy in particular remain widely available and accessible.
Footnotes
Disclosures: none.
References
- 1.Richardson S., Hirsch J.S., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 3.IQVIA Shifts in healthcare demand, delivery, and care during the COVID-19 era. https://www.iqvia.com/insights/the-iqvia-institute/covid-19/shifts-in-healthcare-demand-delivery-and-care-during-the-covid-19-era Available at:
- 4.Epic Health Research Network Preventive cancer screenings during COVID-19 pandemic. https://ehrn.org/wp-content/uploads/Preventive-Cancer-Screenings-during-COVID-19-Pandemic.pdf Available at:
- 5.American Cancer Society COVID-19 pandemic impact on cancer patients and survivors: Survey findings summary. https://www.fightcancer.org/sites/default/files/National%20Documents/Survivor%20Views.COVID19%20Polling%20Memo.Final_.pdf Available at:
- 6.American Cancer Society COVID-19 pandemic ongoing impact on cancer patients and survivors: Survey findings summary. https://www.fightcancer.org/sites/default/files/National%20Documents/COVID19-Ongoing-Impact-Polling-Memo.pdf Available at:
- 7.Sud A, Jones ME, Broggio J, et al. Collateral damage: The impact on cancer outcomes of the COVID-19 pandemic [e-pub ahead of print]. medRxiv.https://doi.org/10.1101/2020.04.21.20073833, accessed May 28, 2020.
- 8.Rosenbaum L. The untold toll — the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 9.Ong MBH Sharpless: COVID-19 threatens to reverse long-running trend of decreasing cancer mortality. https://cancerletter.com/articles/20200515_3/ Available at:
- 10.Dai M., Liu D., Liu M. Patients with cancer appear more vulnerable to SARS-COV-2: A multi-center study during the COVID-19 outbreak. Cancer Discov. 2020;10:783–791. doi: 10.1158/2159-8290.CD-20-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He W., Chen L., Chen L. COVID-19 in persons with haematological cancers. Leukemia. 2020;34:1637–1645. doi: 10.1038/s41375-020-0836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehta V., Goel S., Kabarriti R. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov. 2020;10:935–941. doi: 10.1158/2159-8290.CD-20-0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mei H., Dong X., Wang Y. Managing patients with cancer during the COVID-19 pandemic: Frontline experience from Wuhan. Lancet Oncol. 2020;21:634–636. doi: 10.1016/S1470-2045(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simcock R., Thomas T.V., Estes C. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68. doi: 10.1016/j.ctro.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burki T.K. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 2020;21:629–630. doi: 10.1016/S1470-2045(20)30217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilbo P., Potters L., Lee L. Implementation and utilization of hypofractionation for breast cancer. Adv Radiat Oncol. 2018;3:265–270. doi: 10.1016/j.adro.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Potters L., Kapur A. Implementation of a “No Fly” safety culture in a multicenter radiation medicine department. Pract Radiat Oncol. 2012;2:18–26. doi: 10.1016/j.prro.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 18.Cox B.W., Kapur A., Sharma A. Prospective contouring rounds: A novel, high-impact tool for optimizing quality assurance. Pract Radiat Oncol. 2015;5:e431–e436. doi: 10.1016/j.prro.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Potters L., Raince J., Chou H. Development, implementation, and compliance of treatment pathways in radiation medicine. Front Oncol. 2013;3:105. doi: 10.3389/fonc.2013.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cox BW, Teckie S, Kapur A, et al. Prospective peer review in radiation therapy treatment planning: Long-term results from a longitudinal study [e-pub ahead of print]. Pract Radiat Oncol.https://doi.org/10.1016/j.prro.2019.10.008. Accessed October 18, 2019. [DOI] [PubMed]
- 21.Potters L., Bloom B. Our pledge to achieve safety. Int J Radiat Oncol Biol Phys. 2012;82:1310–1311. doi: 10.1016/j.ijrobp.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 22.Kapur A., Potters L. Six sigma tools for a patient safety-oriented, quality-checklist driven radiation medicine department. Pract Radiat Oncol. 2012;2:86–96. doi: 10.1016/j.prro.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 23.Kapur A., Adair N., O’Brien M. Improving efficiency and safety in external beam radiation therapy treatment delivery using a Kaizen approach. Pract Radiat Oncol. 2017;7:e499–e506. doi: 10.1016/j.prro.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 24.CIDRAP COVID-19: The CIDRAP viewpoint. https://www.cidrap.umn.edu/sites/default/files/public/downloads/cidrap-covid19-viewpoint-part1_0.pdf Available at:
- 25.Kliff S. Hospitals knew how to make money. Then coronavirus happened. The New York Times. https://www.nytimes.com/2020/05/15/us/hospitals-revenue-coronavirus.html Available at:
- 26.Harvard Business Review What will U.S. health care look like after the pandemic? https://hbr.org/2020/04/what-will-u-s-health-care-look-like-after-the-pandemic?utm_content Available at:
- 27.Teckie S., McCloskey S.A., Steinberg M.L. Value: A framework for radiation oncology. J Clin Oncol. 2014;32:2864–2870. doi: 10.1200/JCO.2014.55.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rogers J.P., Chesney E., Oliver D. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]