Abstract
Coronavirus disease 2019 (COVID-19) is an infectious disease typically manifested as a respiratory infection with a range of symptoms from a mild viral illness to a severe acute respiratory syndrome with multiorgan failure and death. We report a case of a young man presenting with compartment syndrome secondary to COVID-19 viral myositis, with a protracted hospital course further complicated by extensive venous and arterial thrombosis. As the coronavirus pandemic evolves, our understanding of the virus continues to improve; however, a host of unanswered questions remain about atypical presentation and management and treatment options.
Keywords: Coronavirus, COVID-19, Viral myositis, Compartment syndrome, Arterial thrombosis
Coronavirus disease 2019 (COVID-19), caused by a highly transmissible novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has brought on a pandemic unlike any that humanity has ever seen. Primarily a respiratory disease, it has a spectrum of clinical manifestations ranging from asymptomatic carrier to multisystem organ failure. Even as the pandemic continues to unfold, the pathophysiologic mechanism of COVID-19 remains elusive with many unanswered questions. We report a case of a 33-year-old diabetic man who presented with COVID-19 viral myositis manifested with compartment syndrome and subsequently developed extensive venous and arterial thrombosis. The purpose of this case report is to better facilitate our understanding of this complex disease process with an emphasis on the vascular manifestations so that we may be better equipped to handle the next pandemic. Informed consent has been obtained from the patient to report this case and all corresponding images.
Case report
The patient presented to the emergency department with acute-onset left thigh pain starting 5 to 6 hours before presentation. The pain woke him up from sleep and was not relieved with over-the-counter pain medication. He denied any history of recent trauma. He was a former smoker but quit 2 weeks before presentation. He denied any personal or family history of hypercoagulable disorders or illicit substance use. Review of systems was negative, most importantly lacking any respiratory symptoms.
Physical examination revealed a diffusely swollen, cyanotic, tender, and tense left thigh. There was no evidence of trauma; the left leg was cool to touch, with intact motor and sensory functions. The left calf was soft. There was a palpable femoral pulse. Popliteal and posterior tibial artery signals were present with Doppler examination. On the right lower extremity, all compartments were soft, with palpable femoral, popliteal, dorsalis pedis, and posterior tibial pulses.
The patient underwent computed tomography angiography of the chest, abdomen, pelvis, and bilateral lower extremities, which revealed bilateral multifocal ground-glass opacities and consolidation in the lower lobes of the lungs concerning for COVID-19 infection, acute occlusion of the left mid-superficial femoral artery without any evidence of reconstitution, and significant swelling in the left thigh musculature (Figs 1 and 2).
Fig 1.

Computed tomography angiography of the chest. Bilateral multifocal ground-glass opacities and consolidation in the lower lobes concerning for COVID-19 infection.
Fig 2.
Computed tomography angiography of bilateral lower extremities. Occlusion of the left mid-superficial femoral artery without reconstitution and significant swelling in the left thigh musculature.
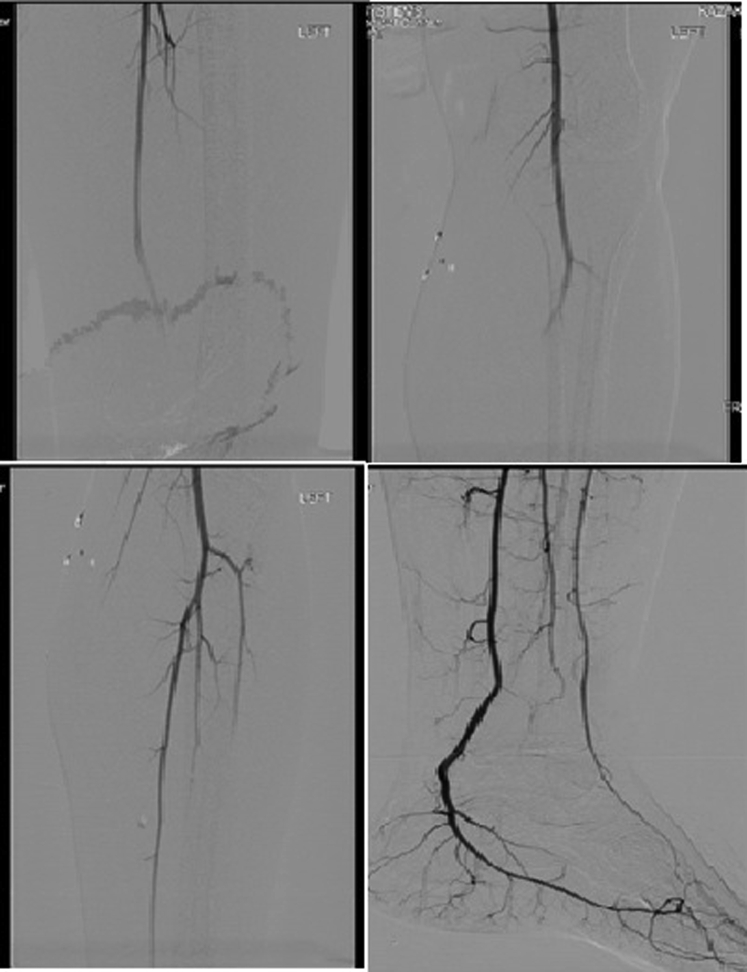
Therapeutic anticoagulation with unfractionated heparin was started, and the patient was taken to the operating room for angiography of the lower extremity and fasciotomy of the left thigh. The angiogram, obtained through a right transfemoral approach, showed no evidence of arterial thrombosis with contiguous sluggish flow down to the foot (Fig 3). The anterior and posterior compartments were found to have elevated pressures. A decompressive fasciotomy of the two compartments was performed through a lateral thigh incision. The muscles of the left thigh compartment appeared healthy, pink, and contractile. Venous duplex ultrasound examination was negative for deep venous thrombosis, and arterial flow was demonstrated to be normal on angiography; thus, viral myositis was suspected in the setting of COVID-19 presentation. However, he was kept on full-dose anticoagulation, given concern for a potential hypercoagulable state. Muscle biopsy specimens obtained were unremarkable.
Fig 3.
Left lower extremity angiogram demonstrating contiguous flow down to the foot.
Postoperatively, the patient was admitted to an intensive care unit. He was fully anticoagulated and received empirical treatment of COVID-19 infection with hydroxychloroquine and azithromycin while awaiting polymerase chain reaction test results, which later came back positive. Workup for hypercoagulable disorders was negative. Creatine kinase levels were normal on admission and remained normal until postoperative day 9. He had improved after the initial operation; the left thigh improved, and the left calf was soft and nonedematous. He did not have any respiratory symptoms during his hospitalization.
On postoperative day 9, acute-onset severe left calf pain developed with elevated compartment pressures. However, he had palpable distal pulses, and there was no concern for arterial thrombosis. He underwent an emergent four-compartment fasciotomy. The muscle in each compartment was significantly edematous. His clinical condition further deteriorated as he developed diabetic ketoacidosis, acute kidney injury, and thrombocytopenia with platelet count of 19,000/μL. In addition, extensive bilateral subsegmental pulmonary embolism and bilateral lower extremity iliofemoral and inferior vena cava thrombosis developed. Furthermore, diffuse arterial thrombosis developed in bilateral lower extremities, femoropopliteal on the right and infrapopliteal on the left leg. He was noted to have cold extremities bilaterally, with intact motor and sensory function. However, given his clinical deterioration, it was thought unsafe to attempt surgery, and he was maintained on anticoagulation.
On postoperative day 11, the patient had pain in the right calf with elevated compartment pressures. Although his clinical course improved, he was starting to demarcate at the toes bilaterally, and so a revascularization was not attempted. He was taken to the operating room for a right lower extremity four-compartment fasciotomy. The muscle was noted to be edematous and dusky.
On postoperative day 13, a right thigh compartment syndrome developed, and the patient was taken to the operating room for a three-compartment fasciotomy. These subsequent compartment syndrome occurrences were secondary to the extensive arterial and venous thrombosis. He remained on therapeutic anticoagulation and prophylactic broad-spectrum antibiotics as a precautionary measure. In addition, he received convalescent antibody plasma therapy for COVID-19 on postoperative day 16, when that became an available option. He underwent a left below-knee amputation and a right above-knee amputation after demarcation of his lower extremities and was discharged to a rehabilitation facility.
Discussion
Compartment syndrome secondary to elevated pressure within a fascial compartment of an extremity can have a variety of causes, most commonly secondary to trauma. Viral etiology of myositis, although rare, has been described in the literature with human immunodeficiency virus infection.1 The typical manifestation of COVID-19 infection revolves around respiratory symptoms. However, there has been a wide variety of atypical manifestations ranging from diffuse arterial or venous thrombosis to neurologic symptoms.2 This is an unusual case of myositis-induced thigh compartment syndrome in a patient with COVID-19.
The patient was previously diagnosed with diabetes, which has been associated with increased mortality and severity of disease in COVID-19 patients.3,4 He was started on therapeutic anticoagulation, mainly because of concern of arterial thrombosis with his initial presentation, and maintained on therapeutic anticoagulation as SARS-CoV-2 infection has been shown to be prothrombotic, probably secondary to a proinflammatory state.5 Of note, the patient had elevated D-dimer and C-reactive protein levels, suggesting a proinflammatory and hypercoagulable state. Despite this, his clinical course was complicated by diffuse arterial and venous thromboembolism, diabetic ketoacidosis, acute kidney injury, and disseminated intravascular coagulation as the septic and proinflammatory response progressed. He went on to development of compartment syndrome secondary to myositis and possibly secondary to worsening ischemic complication in both thigh and calf compartments that may have precipitated the limb amputations.
Conclusions
As the COVID-19 pandemic evolves, there remains an incredible amount of uncertainty we face as health care providers. We believe this is an atypical manifestation of acute viral myositis secondary to COVID-19 infection exhibiting diffuse bilateral, progressive compartment syndrome of the thighs and lower extremities, further complicated by diffuse arterial thrombosis and extensive venous thromboembolism. This case report unravels some complexities of SARS-CoV-2 infection that need to be managed surgically.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Lam R., Lin P.H., Alankar S., Yao Q., Bush R.L., Chen C. Acute limb ischemia secondary to myositis induced compartment syndrome in a patient with human immunodeficiency virus infection. J Vasc Surg. 2003;37:1103–1105. doi: 10.1067/mva.2003.179. [DOI] [PubMed] [Google Scholar]
- 2.Luers J., Rokohl A., Loreck N., Wawer Matos P., Augustin M., Dewald F. Olfactory and gustatory dysfunction in coronavirus disease 19 (COVID-19) Clin Infect Dis. 2020 May 1 doi: 10.1093/cid/ciaa525. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang I., Lim M.A., Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia—a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14:395–403. doi: 10.1016/j.dsx.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang F., Yang Y., Dong K., Yan Y., Zhang S., Ren H. Clinical characteristics of 28 patients with diabetes and COVID-19 in Wuhan, China. Endocr Pract. 2020;26:668–674. doi: 10.4158/EP-2020-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Long B., Brady W., Koyfman A., Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38:1504–1507. doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]