Abstract
Background
The situation of coronavirus disease 2019 (COVID-19) pandemic in the Indian subcontinent is worsening. In Bangladesh, rate of new infection has been on the rise despite limited testing facility. Constraint of resources in the health care sector makes the fight against COVID-19 more challenging for a developing country like Bangladesh. Vascular surgeons find themselves in a precarious situation while delivering professional services during this crisis. With the limited number of dedicated vascular surgeons in Bangladesh, it is important to safeguard these professionals without compromising emergency vascular care services in the long term. To this end, we at the National Institute of Cardiovascular Diseases and Hospital, Dhaka, have developed a working guideline for our vascular surgeons to follow during the COVID-19 pandemic. The guideline takes into account high vascular work volume against limited resources in the country.
Methods
A total of 307 emergency vascular patients were dealt with in the first 4 COVID-19 months (March through June 2020) according to the working guideline, and the results were compared with the 4 pre–COVID-19 months. Vascular trauma, dialysis access complications, and chronic limb-threatening ischemia formed the main bulk of the patient population. Vascular health care workers were regularly screened for COVID-19 infection.
Results
There was a 38% decrease in the number of patients in the COVID-19 period. Treatment outcome in COVID-19 months were comparable with that in the pre–COVID-19 months except that limb loss in the chronic limb-threatening ischemia patients was higher. COVID-19 infection among the vascular health care professionals was low.
Conclusions
Vascular surgery practice guidelines customized for the high work volume and limited resources of the National Institute of Cardiovascular Diseases and Hospital, Dhaka were effective in delivering emergency care during COVID-19 pandemic, ensuring safety of the caregivers. Despite the fact that similar guidelines exist in different parts of the world, we believe that the present one is still relevant on the premises of a deepening COVID-19 crisis in a developing country like Bangladesh.
Introduction
We are living in an unprecedented time. An outbreak of the novel coronavirus disease 2019 (COVID-19; also dubbed as SARS-CoV-2) has dramatically changed the landscape of human behavior all over the world. This highly contagious disease has come to challenge the capability of the most advanced health care systems of the world. Starting from the city of Wuhan, China, in December 2019, the novel coronavirus infection has literally swept across Europe and America where thousands of lives have been lost.1 , 2 To this point in time, more than 13 million people have been infected by the virus globally and more than 580,000 have succumbed to it, most of them in Europe and the Americas.3 The World Health Organization has correctly labeled this disease a pandemic that has now spread in every major country and region of the world4 with shifting epicenters. Although the wave of infection seems to have waned in Europe, it continues to rise in other parts of the world including South America and the Indian subcontinent. Medical and surgical patient care has dramatically changed in the time of COVID-19. Developed nations have adopted policies of rendering only the essential services postponing all nonessential issues. The idea behind such a policy is to reduce burden on the health care system and conserve resources to ensure continuity of essential services in the long term. In line with such policy, different professional bodies of the world including the surgical associations have laid down working guidelines for their respective specialty.
Situation of COVID-19 Pandemic in Bangladesh
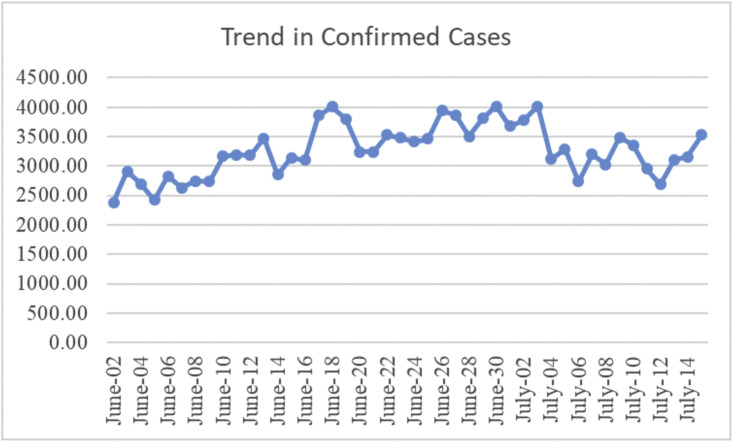
In Bangladesh, the first case of COVID-19 was detected on March 8, 2020. Since then, the country has seen a steady increase in the number of infections with a rapid surge in the recent few weeks.5 Known infection is now nearly 200,000 (Fig. 1 ) with official mortality figures close to 2,500 making it one of the worst hit countries in Asia. Even with the limited number of tests being performed (10,000–15,000/day), new infections in 24 hr are now consistently exceeding 3,000. Test versus case ratio has steadily increased since April 2020, which now ranges between 21% and 25%.6 The rate of infection is also increasing in neighboring India, which has a population of over 1,350 million. Given the current trend of infection, it may not be too far-fetched to think that the Indian subcontinent may be the next epicenter of COVID-19 pandemic. Although the case fatality rate (about 1.28%) is still somewhat low in Bangladesh,6 the number of moderate to severely ill patients requiring hospital-based care is increasing.
Fig. 1.
Trend in confirmed COVID-19 cases in Bangladesh.
COVID-19 Management Strategy in Bangladesh
Bangladesh being a developing country with limited resources is facing a challenge of unknown proportion in the fight against COVID-19 pandemic. Here, the strategy for the fight against COVID-19 has been quite unique. The government had initially set aside a number of COVID-designated hospitals, where only the confirmed cases were being housed and cared. These were mainly smaller facilities and not the main large volume public hospitals of the country, which remained non-COVID hospitals, and were meant to be out of bounds for proven patients with COVID-19. Privately owned hospitals were also not allowed to treat known patients with COVID-19 in the initial period. The idea behind such a strategy was to limit spread of infection in the community. However, infection continues to increase for a variety of reasons that include the socioeconomic ones.
Health care workers (HCWs), as expected, are in the forefront of the fight against COVID-19 all over the world. They have shown tremendous courage and resilience in facing the crisis head on. It should not come as a surprise that physicians and nurses are contracting the infection at a disproportionately higher rate and are even dying in significant numbers while providing care to the patients with COVID-19.7 In Bangladesh, infection among HCWs has also been rising steadily threatening the continuity of essential health care services. More than 2,000 physicians have become COVID-19 positive by the end of June, and there have already been more than 80 casualties. Therefore, protecting HCWs has become a priority in the health care system of Bangladesh as it is all over the world.
National Institute of Cardiovascular Diseases and Hospital (NICVD), Dhaka, is the largest tertiary care cardiovascular center in Bangladesh. It is also the only government-funded referral center for emergency vascular care. At the Department of Vascular Surgery of NICVD, we perform about 2,500 vascular operations and endovascular procedures a year, more than 60% of which are vascular emergencies. We also perform more than 3,000 Duplex imaging at our vascular laboratory and provide outdoor consultation to more than 10,000 patients/year. However, the aforementioned vascular care services rendered in ordinary times cannot continue in the COVID-19 crisis for obvious reasons. Rather, we need to adapt to the changing situation. To this end, we on behalf of the Vascular Surgery Department of NICVD have formulated a working guideline for our vascular surgeons to adhere to. The purpose of the guideline is 2-fold: to safeguard working manpower against COVID-19, and to continue essential vascular services over a long period of time. The strategic mainstay of this guideline is deferral of the elective procedures and nonessential vascular services to focus only on emergency vascular care. To protect HCWs, we have instituted a protocol of duty roster using minimum manpower in such a way that allows for a sufficiently long period of isolation in between duties. There have been confusions regarding the selection of vascular procedures to be judged for different urgency levels. The present guideline formulated on the principles being followed worldwide and also taking into consideration the health care structure and available resources of Bangladesh is expected to eliminate such confusions and make vascular patient care relatively seamless during the ongoing COVID-19 pandemic.
Vascular Services: Working Definitions of Different Urgency Levels
At NICVD, Dhaka, we have categorized vascular diseases that require one or more procedures for evaluation and management into different priority levels mentioned below and assigned one or more recommendations to every one of them (Table I ). The basic recommendations are as follows:
1. Must do
-
2.
Should not be deferred
-
3.
Consider deferral
-
4.
Should be deferred
-
5.
Consider aggressive medical management instead
Table I.
Working guidelines for vascular procedures and other services
| Disease | Description | Intended procedure(s) | Recommendation |
|---|---|---|---|
| Limb/visceral ischemia | |||
| ALI | Deteriorating sensory/motor function Tissue loss Dry/wet gangrene, ascending cellulitis Compartment syndrome |
Fasciotomy Embolectomy Catheter-directed thrombolysis Peripheral angiogram Endovascular therapy Surgical revascularization Amputation |
Must do |
| Vascular injury | Bleeding/expanding hematoma/hemodynamic derangement/potential life/limb loss situation | Hemostasis/vascular repair | Must do |
| CLI | CLTI—rest pain | Peripheral angiogram Endovascular therapy Surgical revascularization |
Consider aggressive medical management instead |
| CLTI—tissue loss | Peripheral angiogram Endovascular therapy Surgical revascularization Amputation |
Must do | |
| Intermittent claudication | Peripheral angiogram and endovascular therapy | Should be deferred | |
| Mesenteric vascular ischemia | Stable | Visceral angiogram and endovascular therapy | Should be deferred |
| Disabling symptoms | Visceral angiogram and endovascular therapy | Consider deferral/consider aggressive medical management instead | |
| TOS | Arterial/venous | Surgery | Consider deferral |
| Neurogenic | Surgery | Should be deferred | |
| Arterial aneurysm/dissection | |||
| Arterial aneurysm | Stable, not rapidly increasing in size | Repair by surgical/endovascular means | Should be deferred |
| Stable but rapidly increasing in size/ruptured/impending rupture (clinical/Doppler/CT/angiographic evidence) | Repair by surgical/endovascular means | Should not be deferred | |
| AAA/TAAA/aortic dissection | Stable, not rapidly increasing in size (clinical/Doppler/CT/angiographic evidence) | Repair by surgical/endovascular means | Should be deferred |
| Stable but rapidly increasing in size/ruptured/impending rupture (clinical/Doppler/angiographic evidence) | Repair by surgical/endovascular means | Should not be deferred | |
| Carotid atherosclerotic disease | |||
| Carotid atherosclerotic disease | Stable, asymptomatic, mild to moderate symptoms | Duplex evaluation | Should be deferred/consider aggressive medical management instead |
| Moderate to severe symptoms directly attributable to carotid pathology | Duplex evaluation/DSA/CAS/CEA | Consider deferral/consider aggressive medical management instead | |
| Venous diseases | |||
| Acute DVT | Iliofemoral with phlegmasia | Thrombolysis/medical management | Consider aggressive medical management instead |
| Femoropopliteal | Thrombolysis/medical management | Consider aggressive medical management instead | |
| High risk of PE | IVC filter insertion/removal | Consider deferral | |
| Chronic DVT/PTS | Swelling/blackening/ulcer | Venous intervention | Should be deferred/consider aggressive medical management instead |
| Varicose vein | C0–C5 | Medical management/surgery/EVLA/RFA | Should be deferred |
| C6 | Medical management/surgery/EVLA/RFA | Should be deferred/consider aggressive medical management instead | |
| Hemodialysis access | |||
| AVF | ESRD with no other means of HD | Elective creation of AVF/tunneled catheter | Should not be deferred |
| ESRD having other means of HD | Elective creation of AVF/tunneled catheter | Should be deferred | |
| ESRD with access complications (thrombosis/infection/pseudoaneurysm/bleeding) | Surgical correction | Should not be deferred | |
| ESRD with failing AVF with no other means of HD | Fistulogram/fistuloplasty | Should not be deferred | |
| ESRD with failing/failed AVF with other available means of HD | Fistulogram/fistuloplasty | Should be deferred | |
| Vascular malformations | |||
| AVM | Arterial/venous with major bleeding | Surgical/endovascular hemostasis (e.g., embolization) | Should not be deferred |
| Vascular outpatient services | |||
| Vascular duplex study | Should be deferred (unless deemed mandatory for evaluation of urgent cases) | ||
| OPD | Should be deferred (encourage telemedicine) | ||
AAA, abdominal aortic aneurysm; ALI, acute limb ischemia; AVF, arteriovenous fistula; AVM, arteriovenous malformation; CAS, carotid artery stenting; CEA, carotid endarterectomy; CLI, chronic limb ischemia; CLTI, chronic limb-threatening ischemia; CT, computed tomography; DSA, digital subtraction angiography; DVT, deep vein thrombosis; ESRD, end-stage renal disease; HD, hemodialysis; OPD, outpatient department; TAAA, thoracoabdominal aortic aneurysm; TOS, thoracic outlet syndrome; PTS, post thrombotic syndrome; IVC, inferior vena cava; EVLA, endovenous laser ablation; RFA, radio frequency ablation.
Results
Table II depicts the number of cases in each major disease category during the first 4 COVID-19 months (March through June 2020) against the number in the 4 pre–COVID-19 months (November 2019 through February 2020). The total number of emergency procedures performed in the first 4 COVID-19 months was 307, whereas procedures performed in the preceding 4 months that included elective procedures were 498 accounting for a decrease of 38% in the number of procedures. Limb salvage defined as freedom from major amputation (below knee or above knee) was similar for emergency procedures in the acute limb ischemia (ALI) disease category (83.8% vs. 87.5%). However, there was a decrease in the rate of limb salvage in the COVID-19 months for patients with chronic limb-threatening ischemia compared with pre–COVID-19 months (72.4% vs. 83.6%). The 2 stated goals of the guideline continue to be fulfilled; emergency vascular services continue unhindered and to this point, number of infection among staff at the Department of Vascular Surgery was limited to 8, only 1 of them doctor.
Table II.
Early results of the working guideline at NICVD
| Disease | Strategy/procedure | COVID-19/pre–COVID-19 months (N) | Outcome (limb salvage), n (%) | Outcome (procedural success), n (%) |
|---|---|---|---|---|
| ALI including vascular injury | Repair/embolectomy/amputation | 204/296 | 171 (83.8)/259 (87.5) | |
| CLTI with tissue loss | Revascularization with or without amputation | 29/98 | 21 (72.4)/82(83.6) | |
| HD access creation | Radiocephalic, brachiocephalic, brachiobasilic transposition, and so forth | 44/66 | 41(93.2)/61 (92.8) | |
| HD access care | Repair of pseudoaneurysm, fistuloplasty | 21/16 | 20 (95.2)/16 (100) | |
| Arterial aneurysm/pseudoaneurysm | Surgical repair | 09/22 | 09 (100)/22 (100) | |
| Total | 307/498 |
COVID-19 months, March through June 2020; pre–COVID-19 months, November 2019 through February 2020.
ALI, acute limb ischemia; CLTI, chronic limb-threatening ischemia; HD, hemodialysis.
Discussion
Bangladesh is a small Southeast Asian country, which has drawn international attention in the recent times for giving shelter to more than 1 million Rohingya refugees driven out from neighboring Myanmar. Despite all the adversities, Bangladesh has made significant strides in key socioeconomic indicators over the last decade to get rid of the status of least developed country and is now officially acknowledged as a developing country. Its present population is 164.5 million with an average population density8 of 1,265/km2 making it one of the most densely populated countries in the world. Dhaka, the capital of Bangladesh, is one of the most densely populated megacities of the world. As apprehended, the city has been hit very hard by COVID-19 infection with more than half of the country's total infection recorded here.9 Bangladesh initially pursued a strategy of managing patients with COVID-19 only in specific facilities. A system of triage along with clear demarcation of red, orange, yellow, and green areas is still mostly lacking in the major hospitals. A lack of quick screening for COVID-19 also stands in the way of efficient handling of patients, particularly those requiring emergency surgical procedures. The previously mentioned strategy is fundamentally different from that pursued in the developed countries.10 , 11 Realizing the pitfalls of this strategy, the government of Bangladesh has now changed its policy to accommodate patients both with COVID-19 and without COVID-19 in the same facility.12 However, it is still not clear how effective this will be in delivering patient care without compromising safety.
As number of infection continues to rise in Bangladesh, the situation will likely become worse. A constraint of resources can be predicted in the coming months. At this point, the COVID-19 treatment facilities all over the country, both public and private, are full to their capacity. With a very limited number of intensive care unit (ICU) beds and ventilators, there may be a need for makeshift ICUs. Operating theaters (OTs) may also need to be repurposed and used as ICU. Similar constraints can also be foreseen for HCWs. At NICVD, the number of HCWs infected with COVID-19 has now exceeded 150, 30 of whom are physicians. The number of dedicated vascular surgeons in Bangladesh is only about 30, which is clearly inadequate for the large population of the country. About one-third of these professionals work at the NICVD. Therefore, it is imperative that vascular surgeons of Bangladesh be protected while rendering essential vascular care services. We strongly believe that the proposed working guideline can greatly facilitate the execution of this policy.
Vascular surgical bodies all over the world have put in place such guidelines and adjustments for their members to follow. A large cardiovascular center in Turkey has recently published its own guideline, where different vascular procedures have been assigned a certain level of priority.10 The American College of Surgeons has also published a similar working guideline for the vascular surgeons.13 Melo and Pedro14 from Portugal reported their departmental adjustments in the time of COVID-19. Similar COVID-19–driven practice restructuring has been reported from a tertiary hospital in Singapore.11 The present guideline although fundamentally in line with these previously published principles is based on the unique situation in Bangladesh. We have taken into account the availability of not only vascular surgeons but also the supporting staff including anesthesiologists and those who have access to the OT and catheterization laboratories. The guideline also foresees the issues of affordability in addition to availability of surgical materials and hardware for endovascular procedures, which will be inevitable in the near future as a consequence of the COVID-19–related economic downturn. To this end, we have included in this guideline an additional recommendation of “consider aggressive medical management instead,” which if judiciously applied could help further reduce procedural burden at this time of crisis.
It is to be noted that since the implementation of the countrywide lockdown from early April, routine outdoor patient pool had dried, which is yet to return to normal despite the easing of lockdown. However, the pattern of vascular emergency cases has remained essentially the same. Vascular trauma resulting from violence or road traffic accidents is being encountered regularly. Complications related to ALI and dialysis access have remained more or less similar in number. Vascular surgeons have the moral and professional responsibility to serve these patients irrespective of their COVID-19 status, which places them at a high risk of contracting the infection. Our roster-based emergency services involving minimum number of HCWs minimize risk of exposure. To further minimize this risk, we have brought in a few adjustments in our anesthetic practices. Regional or locoregional anesthesia is being preferred over general anesthesia with endotracheal intubation whenever possible to reduce aerosol generation in the OT. Availability of personal protective equipment (PPE) has become a key issue for HCWs worldwide. In Bangladesh, quality PPE and masks, as well as proper donning and doffing practices, has been a matter of great concern. Physicians have been infected even when donning PPE and masks. We believe that accountability of the health administrators and training for HCWs can greatly improve the situation. The early outcome of our proposed guideline has been satisfactory in the sense that emergency vascular care services continue to be provided without significant negative impact on safety of the caregivers. Results of ALI and chronic limb-threatening ischemia treatment during pandemic have also been comparable with the pre–COVID-19 months. The slightly higher number of limb loss in the COVID-19 months may be explained by late presentation largely because of the countrywide lockdown.
Conclusions
We propose a working guideline for the vascular practices in Bangladesh during the COVID-19 pandemic. The guideline is basically in line with those being practiced elsewhere. However, it is unique in the sense that it takes into account the different reality of a developing country with significant constraint of resources in the face of a rapidly worsening crisis.
Acknowledgments
We acknowledge Professor Dr Ramapada Sarker and Dr Asraful Hoque Sium from the Department of Cardiac Surgery, NICVD, for their advisory help with the preparation of the guideline.
Conflict of interest: None to report.
Author contributions: A.H.M.B. contributed toward concept, writing, and data analysis. M.E.H. and N.C.M. contributed toward concept. M.Mo.R., M.Mu.R., M.F.I., and M.S.J. did data collection and data analysis. N.K.D. and S.M.M.H.C performed data analysis. M.M.I. contributed toward concept and data analysis.
References
- 1.World Health Organization Coronavirus disease (COVID19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at.
- 2.Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf?sfvrsn=fce87f4e_2 Available at.
- 3.Coronavirus disease (COVID-19) situation report – 174. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200712-covid-19-sitrep-174.pdf?sfvrsn=5d1c1b2c_2 Available at.
- 4.Coronavirus Disease 2019 (COVID-19) Situation Report - 51. World Health Organisation (WHO); 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid 19.pdf?sfvrsn=1ba62e57_10 Available at. [Google Scholar]
- 5.Coronavirus disease (Covid-19) situation in Bangladesh. https://www.worldometers.info/coronavirus/country/bangladesh/Date Available at.
- 6.Coronavirus disease (Covid-19) situation in Bangladesh. https://www.iedcr.gov.bd/index.php/component/content/article/73-ncov-2019 Available at.
- 7.Lai X., Wang M., Qin C. Coronavirus disease 2019 (COVID-2019) infection among health care workers and Implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Netw Open. 2020;3:e209666. doi: 10.1001/jamanetworkopen.2020.9666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bangladesh population 2020. https://worldpopulationreview.com/countries/bangladesh-population/Date Available at.
- 9.Covid-19 situation in Dhaka City. https://www.iedcr.gov.bd/website/images/files/nCoV/Case_dist_26_May_upload.pdf Available at.
- 10.Ünal E.U., Mavioğlu H.L., Iscan H.Z. Vascular surgery in the COVID-19 pandemic. J Vasc Surg. 2020;72:752–754. doi: 10.1016/j.jvs.2020.04.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng J.J., Gan T.R., Niam J.Y. Experience from a Singapore tertiary hospital with restructuring a vascular surgery practice in response to national and institutional policies during the COVID-19 pandemic. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National guidelines on clinical management of coronavirus disease 2019 (COVID-19) https://dghs.gov.bd/images/docs/Guideline/COVID_Guideline_2.pdf. Version 6.0. 18 May 2020 Available at.
- 13.COVID-19 guidelines for triage of vascular surgery patients. https://www.facs.org/covid-19/clinical-guidance/elective-case/vascular-surgery Available at.
- 14.Melo R.G., Pedro L.M. Vascular surgery department adjustments in the era of the COVID-19 pandemic. J Vasc Surg. 2020;72:375–376. doi: 10.1016/j.jvs.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]