On January 4, 2020, the World Health Organization (WHO) tweeted1:
#China has reported to WHO a cluster of #pneumonia cases —with no deaths— in Wuhan, Hubei Province. Investigations are underway to identify the cause of this illness.
The etiology of the pneumonia referred to was subsequently identified as SARS-CoV-2, the novel virus causing COVID-19. COVID-19 swept across the globe, and the WHO characterized it as a pandemic on March 11.1 In its wake, oncologists were faced with multiple challenges and few resources to help navigate new clinical realities. Who is most at risk for COVID-19? Should cancer treatment continue or be delayed? How should radiation oncology proceed?
National and international professional societies published detailed clinical guidance, including American Society of Radiation Oncology (ASTRO), American Society of Clinical Oncology (ASCO), and European Society for Radiotherapy and Oncology (ESTRO), among others. These recommendations were unique in the rapid fashion in which they were created and shared. The guidance offered was broad because its application was highly dependent on the specific location of the patient and radiation facility. For example, in the United States, locales within New York and New Jersey were overwhelmed with coronavirus cases while other states had relatively few cases.2
The ASTRO web team was extremely nimble as leadership and staff created content related to COVID-19. A new section of the website in the daily practice tab was added in March 2020 to house the rapidly evolving content. As new content was submitted, the section was reorganized for easy navigation. Overall, this section has had 58,961 page views as of June 12, 2020. The most frequently visited pages were summary (17,548 views), FAQs (14,603 views), and journal articles (11,579 views).
Social media are defined as interactive forms of electronic communication.3 During the COVID-19 epidemic, these tools were used by the radiation oncology community to connect and share information. Platforms including Twitter, Facebook, Instagram, WhatsApp, ASTRO ROHub, webinars, and podcasts were used to disseminate experiences and foster communication among oncologists worldwide. In this brief report, we share some examples of how social media filled a strong need for information-sharing during the crisis.
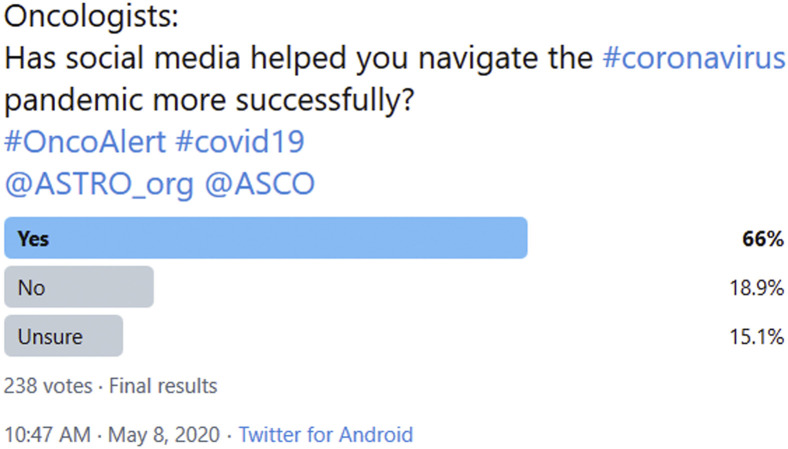
Twitter is a microblogging platform in which users can share sentences (otherwise known as tweets) of up to 280 characters. During the pandemic, oncologists from all over the world shared their experiences caring for patients during this difficult time. Practical information was exchanged, including patient scheduling, initiating telemedicine, personal protection equipment (PPE) use, on-treatment visits, remote work, SARS-CoV-2 testing procedures, and research publications. Twitter was also used by ASTRO’s journals to disseminate links to preprints of new COVID-19 research.4 Group messaging via Twitter was also used to share tweets and information globally. For example, the OncoAlert COVID-19 group messaging includes oncologists from the United States, United Kingdom, Sweden, Italy, and many other countries. Information from Europe was shared with members of this group (including author M.K.) before the COVID-19 surge in the United States. Tweets regarding how European oncologists were handling the crisis (managing COVID-19–positive patients, hospitals bed shortages, and cancer care continuation) helped US-based oncologists understand and prepare for the challenges coming their way via the US surge from COVID-19. Figure 1 shows a Twitter poll created by author M.K. asking the question: “Oncologists: Has social media helped you navigate the #coronavirus pandemic more successfully?” Sixty 6% responded “yes,” and 15% responded “unsure.”
Fig. 1.
Twitter poll by Miriam A. Knoll, MD via Twitter @MKnoll_MD on May 8, 2020.
Group Messaging: Facebook and WhatsApp
The number of Facebook groups for physicians has exploded during the past 5 years and is often organized according to member interests within medicine (ie, specialty, as in interventional radiology interest groups) or outside medicine (eg, motherhood, as in physician moms’ groups).5 The COVID-19 physician group was created on March 12, 2020, for physicians and is described on its Facebook group page as “An inclusive resource for physicians to share front line clinical information about COVID-19 as it becomes available.”6 Of note, the group was started before the US coronavirus surge but quickly grew because physicians understood the importance of gaining knowledge from their peers. As of June 1, 2020, the group had 28,287 members. There were 578 new posts in May 2020. The administrators and moderators of the group instruct members to share clinical information only and to provide references and links to articles. Many COVID-19–related posts were also shared on the radiation oncology women’s Facebook group page and on the hematology oncology women’s Facebook group page.
Many of the clinical features of COVID-19 came to be identified by physicians who communicated with each other remotely during the initial phases of the pandemic, including the dermatologic “COVID toes,” anosmia, and hypercoagulability. The crowdsourcing of information across groups via Facebook, WhatsApp, and others allowed for quick dissemination of knowledge. Authors M.K. and A.D. participated in a WhatsApp global group of radiation oncologists, in which resources were quickly shared. For example, a webinar presented at Jefferson regarding how to identify COVID-19 from computed tomography scans was recorded via Zoom and uploaded to DropBox. The DropBox link was then shared to the WhatsApp group. Another resource shared across messaging platforms was a Google Docs spreadsheet created by trainees, which listed radiation oncology programs and the residents’ roles and responsibilities during COVID-19, such as if trainees worked from home.
ASTRO’s ROhub
ROhub is an online forum hosted by ASTRO where members can discuss radiation oncology topics. During the coronavirus pandemic, many individuals shared questions, information, and ideas about radiation oncologists’ experiences with COVID-19. In particular, physician experiences from COVID-19 epicenters in New York City and New Jersey proved to be extremely helpful. These topics included the American Board of Radiology examinations, interviews, COVID-19 testing, telemedicine, provider relief funds, and much more. The online forum provided a unique space for ASTRO members to exchange ideas—arguably a space that does not exist elsewhere.
Membership engagement with the ROhub has grown considerably during the past year, especially in the open forum, member directory, and event communities. Per communication from ASTRO, in 2020 the open forum so far has had 154,828 views and the member directory has had 63,762 views.
The open forum has been a dynamic communication vehicle during the COVID-19 outbreak. Members and staff have used the open forum to share experiences, struggles, and resources during this time. The first thread on this topic appeared on March 13, before the surge in the United States; as of June 12, 2020, there were 60 threads and 149 discussions posts related to this topic. The COVID-19 conversations have had 118,238 page-views by 3843 users. Of note, these statistics count only those visitors who log in to the forum itself. All ASTRO —members receive the daily digest from the ROhub via email and can read posts from within their email as well. These discussions helped inform the expanded COVID-19 resources, FAQs, and updates that appear on the astro.org/covid webpages.
Remote Conferences
The Centers for Disease Control and Prevention recommended limiting face-to-face interactions as the most effective way to limit the spread of COVID-19.7 These measures, termed “social distancing,” required meetings to be held virtually or postponed. For example, the American Association for Cancer Research annual meeting was held virtually on April 27 and 28 in lieu of the customary in-person meeting.8 The meeting reported 61,000 registrants from 140 countries and meeting content was shared online. The second portion of the meeting took place June 22 to 24, 2020, with free registration.
In March 2020, the Annual Refresher Course was converted to a virtual meeting, and the ROhub was used to encourage conversations and as a vehicle to find resources during the meeting. The Refresher Community had 2248 views as of June 12, 2020.
Similarly, ASCO’s annual meeting took place virtually from May 29 to 31 for the first time.9 This proved to be a resounding success as a new record of 42,750 attendees from 138 countries streamed more than 2.5 million views of meeting content (and counting). ASTRO’s annual meeting will also take place virtually in October 2020 “based on our overwhelming concern for the safety and well-being of our members, their patients, exhibitors, staff and the families of all involved.”10 Notably, ESTRO will be one of the first oncology conferences hosting a hybrid in person and virtual event in November 2020, which may provide a unique look into how future meetings can be hosted.
As organizations navigate virtual platforms and online meetings, engagement with virtual attendees remains key. How will participating in a virtual meeting be different than simply watching a YouTube video? Can virtual networking be facilitated? How will organizations recoup lost revenue and funding?
Future Opportunities
The challenges faced by radiation oncology during the coronavirus pandemic were and continue to be abundant. Social media has facilitated connectivity within our community by allowing individuals from across the globe to share information in real time. Should these virtual ties be maintained when face-to-face interactions resume? If we value perspectives from outside our 6-foot circle, the answer is emphatically “yes.”
Footnotes
Disclosures: M.A.K. reports consulting fees from Bristol Myers Squibb and AstraZeneca, outside of the submitted work. A.D. receives financial support from National Cancer Institute, American Society of Clinical Oncology, NRG Oncology, and Prostate Cancer Foundation Challenge outside of the submitted work. He serves in an advisory role for Roche, Janssen, Self Care Catalysts, Oncohost, Varian, Accordant, and Envisino Health Partners outside of the submitted work. He has provided expert testimony regarding intellectual property for Wilson Soncini, outside of the submitted work.
References
- 1.World Health Organization WHO timeline-COVID-19. https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19 Available at:
- 2.Johns Hopkins University Coronavirus resource center. https://coronavirus.jhu.edu/map.html Available at:
- 3.Merriam-Webster Social media. https://www.merriam-webster.com/dictionary/social%20media Available at:
- 4.American Society for Radiation Oncology Accepted articles from ASTRO journals. https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/Journal-Articles Available at:
- 5.Shillcutt S.K., Silver J.K. Social media and advancement of women physicians. N Engl J Med. 2018;378:2342–2345. doi: 10.1056/NEJMms1801980. [DOI] [PubMed] [Google Scholar]
- 6.COVID19 physician group. https://www.facebook.com/groups/630423250840324/ Available at:
- 7.Centers for Disease Control and Prevention Social distancing. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html Available at:
- 8.American Association for Cancer Research AACR annual meeting 2020. https://www.aacr.org/meeting/aacr-annual-meeting-2020/coronavirus-information/ Available at:
- 9.American Society of Clinical Oncology ASCO20 virtual. https://meetings.asco.org/am/virtual-welcome Available at:
- 10.American Society for Radiation Oncology Annual meeting. https://www.astro.org/Meetings-and-Education/Live-Meetings/2020/Annual-Meeting Available at: