Introduction
The current pandemic has resulted in unprecedented demands on health care systems overloaded with COVID-19–afflicted patients, with the challenges of an insufficient number of beds and insufficient equipment and personal protective equipment for staff. In an effort to spare resources and to minimize exposure of patients and personnel, a shift to limit access only to patients needing essential services was undertaken. This invariably led to decreased access to many routine hospital services. Furthermore, patients themselves were not accessing hospital services because house confinement, social distancing, limitation of gatherings, and general business lockdowns to flatten the curve came into effect. Under these unique circumstances, the move to telemedicine resources became a natural solution to pressing health care needs constrained by the disruptive crisis.
Current telemedicine use
Telemedicine, or the electronic transmission of medical information via digital communications, has become an essential tool. It has led to a significant increase in the utilization of remote telemedicine and telehealth interventions, with many physicians in some regions using these technologies to manage patients remotely. Expanded use of telemedicine in medical care and teleradiology occurred in tandem with the increased need for social distancing. Telemedicine tools are more commonly used for remote treatment, particularly in the United States, where 63% of health care practitioners have used it. Among physicians currently using telemedicine for consultation, nearly half (48%) are using it for the first time. When the outbreak ends, one-fifth of physicians using telemedicine tools expect to use them significantly more than before the pandemic.1 The COVID-19 pandemic has shone a spotlight on the innovative degree to which eHealth can empower health systems to avoid cross-infection of COVID-19 patients and ensure continuity of essential health services.
Inequitable access
This approach has not been possible in all countries. An overall global digital divide marginalizes many. Regional discrepancies are stark, with 78% of European households reporting basic Internet access in 2014 compared with 11.2% in Africa.2 The International Telecommunications Union publishes both an information and communications technology (ICT) development index rank and the Global Digital Health Index, an interactive map of countries that “tracks, monitors, and assesses the enabling environment for digital health throughout the world.”3 , 4 These country-by-country comparisons of digital infrastructure serve as the bedrock for strategically planning remote coordination of both radiation oncology and medical imaging, including nuclear medicine (both diagnostic and therapeutic), especially during a pandemic.
Worldwide, a gender gap in ICT also exists: 48% of women versus 58% of men use the Internet.5 Furthermore, even in countries with access to digital technologies, there may be pockets of underserved and rural communities that have a lack of training, infrastructure, or opportunity to use these services.
Thus, many essential services that depend on digital infrastructure risk grinding to a halt during a pandemic due to lack of robust digital foundations in many countries. Forty-three percent of 125 countries surveyed by the World Health Organization in 2015 reported “established” teleradiology and 26% Picture Archiving and Communication System.6
Support of patient care through telemedicine
Telehealth provides an effective method of accessing patients from rural and other underserved locales, as long as the infrastructure is available. Overall patient feedback has been favorable, suggesting patient satisfaction and a high level of acceptance, especially given the savings in travel expenses and time.7 , 8
Telemedicine has also proved very useful in several medical specialties where the combination of real-time image and sound can replace physical presence. These include telepathology,9 teleradiology,10 teledermatology,11 telepsychiatry,12 telepharmacy,13 and telesurgery.14 Some examples of success in telemedicine have been seen in the fields of dermatology and psychiatry.15 Several small studies exhibit the advantages of telemedicine interventions in the management of chronic disease. Studies show that telemedicine in office- and hospital-based settings is most beneficial for specialties requiring greater verbal communication in diagnosis and treatment, such as in psychiatry and neurology.16
Of note are recent success stories in advanced therapy contexts. For example, in Singapore, telemedicine throughout the crisis enabled patients to undergo Y90 selective internal radiation therapy, where ICT tools facilitated the coordination of interventional radiologists for arteriography and nuclear medicine physicians and radiopharmacists for both dosimetry and procedural aspects of therapy. This included guaranteeing a continued supply chain, dose verification, and administration of the dose conjointly with the interventional radiologist.17
Telemedicine tools also offer considerable opportunities to bring high-quality medical care to scenarios where it is not readily available on site. These include sailing ships, refugee camps, migrant assistance, native communities, prison facilities, remote dwellers, and rural areas in developed and developing countries. In addition, ICTs can enhance global collaborations such as those described in radiation oncology.18
Radiation oncology and telemedicine
During the COVID-19 pandemic, the challenge in radiation oncology was to protect patients, families, and health professionals while continuing activities. Radiation oncology centers in hospitals that were the first to confront the pandemic gained expedited practical experience and began collecting relevant data early. They published their preliminary experience and put together tentative guidelines.19, 20, 21
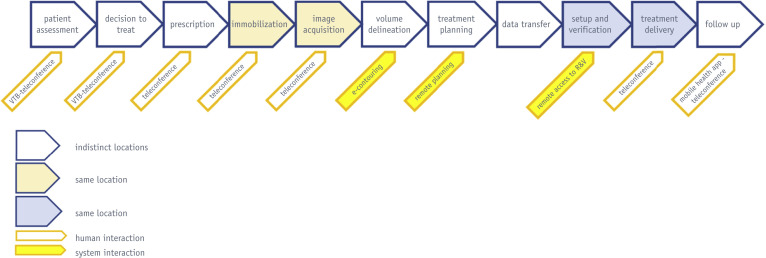
The main areas of change where telemedicine tools support or replace routine practice are communications among center staff, interactions between patients and hospital staff, meetings, working from home, radiation therapy treatment planning, and patient follow-up (Fig. 1 ). Some of the radiation therapy processes that can be supported by telemedicine include patient assessments, decision to treat and prescription,22, 23, 24, 25, 26 and immobilization and image acquisition.27 In addition, volume delineation,28 treatment planning,29, 30, 31 setup, verification, treatment delivery,27 and follow-up32, 33, 34, 35, 36 can be supported. Furthermore, telemedicine applications can also be used for education and training of health care professionals37 and in support of research and enhancing access to clinical trials.38 Management of patient care has become significantly easier with the easing of some pre-COVID-19 limiting factors, such as Centers for Medicare & Medicaid Services’ expansion of health care benefits for Medicare beneficiaries and greater flexibility in state telemedicine medical licensing regulations.39 , 40
Fig. 1.
Telemedicine interventions in the radiation therapy processes.
International Atomic Energy Agency Initiatives
The International Atomic Energy Agency (IAEA) has long supported the initiation or expansion of new radiation therapy centers, providing technical assistance, education, and training as well as conducting clinical and applied research in radiation oncology, nuclear medicine, and radiology and radiation physics worldwide.41, 42, 43 One of the most significant findings highlighted by this experience is the insufficient and inequitable access to radiation therapy services by large sectors of the population in developing countries, as well as by underserved communities in developed countries.44 In many states, a few well-developed radiation therapy centers are located in large metropolitan capitals or cities, although a large proportion of the population dwells in distant and rural regions or islands, even in high-income countries.45 In this scenario, tele-radiation therapy networks appear a feasible and effective solution to connect these centers so that expertise is shared and reaches all corners of the country. Tele-radiation therapy networks are not new and continue to be very useful. In this model, a referral radiation therapy center connects with a variable number of smaller radiation therapy centers or units in the country or region.46, 47, 48, 49, 50, 51 Telemedicine facilitates decentralized radiation therapy services and helps break professional isolation.
With currently available technologies, a course of radiation therapy cannot be delivered remotely. However, many steps in the radiation therapy process can be implemented, taking advantage of telemedicine solutions. Seeing the potential of telemedicine to address some of these steps, the IAEA has applied it in many areas. Examples are given in the following.
Research and contouring
The IAEA is conducting a coordinated research project to assess the impact of blended distance learning on standardizing radiation therapy contouring in low- and middle-income countries (LMICs). The objective of this study is to determine whether any of the benefits noted from the learning interventions that are based on local imaging are sustainable. The purpose of this 3-dimensional conformal radiation therapy coordinated research project is to improve target and organ-at-risk contouring in LMICs using web-based workshops.52 Another ongoing project in LMICs explores treatment planning in radiation therapy for nasopharyngeal carcinoma.53
Tumor boards and education
In 2012, the IAEA initiated a pilot project to support medical professionals in African countries.54 In this Africa Radiation Oncology Network project, an international network was established for a monthly virtual tumor board discussion in which challenging radiation oncology cases were reviewed. During these videoconferences, the group attempts to reach a treatment consensus or recommendation. Videoconferencing discussions contribute to the strengthening of clinical decision-making, benefiting individual oncology patients. Regularly scheduled webinars on cancer care and radiation oncology are also delivered through the platform, and a future e-contouring platform is being prepared for use in this setting as well. These activities enhance resident education in participating centers, both in Africa and in North America.55 This ongoing initiative showed the feasibility of using telemedicine tools to create a radiation oncology community for case discussions and education. In light of the success of the Africa Radiation Oncology Network, the IAEA is expanding to South America, Asia, Russian-speaking regions, and francophone Africa.
In radiation oncology education, current continuous developments in e-learning and mobile technologies are allowing learning to be more learner-centered, facilitating interactions between learners and significantly transforming the role of the educator.56, 57, 58 Distance learning was already accessible before the COVID-19 pandemic. The changes introduced by the present circumstances make it probable that all forms of distance and e-learning will be even more relevant in the future.
The IAEA has been active in producing and facilitating distance learning courses and workshops in radiation medicine and produces a wealth of online educational materials.59 In addition, the IAEA offers distance learning packages, training in remote contouring, and e-learning professional training.60 , 61 Development of remote quality assurance and remote quality assurance missions of Quality Assurance Team for Radiation Oncology is underway, as are future plans for training in remote planning through a new interactive platform.
Consensus building and information sharing amid the uncertainty
As a consequence of the COVID-19 pandemic, radiation oncology departments accelerated the adoption of telemedicine tools to implement social distancing and minimize the risk of viral spread. The use of these tools will likely continue for the foreseeable future.
During the COVID-19 crisis, the IAEA conducted a series of international webinars in various languages with experts from different regions to share experiences and collate recommendations. The primary objective of these webinars was to share experiences and help radiation therapy departments navigate these unchartered waters worldwide.62 Telemedicine and other areas were addressed by an international IAEA panel that included representatives of 10 professional societies. The panel provided insight into how the changes implemented to control the spread of the COVID-19 pandemic would affect the new normal of the radiation oncology profession.63
Radiation oncology practice should adapt to the new normal by reducing time in hospital and patient contact with health care workers while maintaining quality of care.64 , 65 Best practices include the use of information technology solutions that allow multidisciplinary team meetings, staff meetings, and discussions with patients to take place remotely, as well as radiation therapy processes such as remote contouring, quality assurance, and planning.
What are the conditions for telemedicine implementation?
Health care organizations should develop and implement a strategy for the use of telemedicine technologies and relevant task groups of health care professionals to enhance the continued integration of routine digitally enabled care. The regular assessment of newly introduced digital technologies should be conducted using monitoring and auditing tools, including feedback from all users.25 The conditions for telemedicine implementation are multifactorial66 and should be carefully considered to achieve success in a telemedicine program (Table 1 ).
Table 1.
Conditions for telehealth implementation (modified from Gagnon et al66)
| Dimension | Condition |
|---|---|
| Individual | Perceived ease of use Technology integrated within the daily practice Health care professionals' motivation |
| Professional | System based on the needs of health care professionals Adequate remuneration for professionals at both sites Defining clear rules for professional liability Participation of physicians in telehealth decision-making |
| Organizational | Availability of resources dedicated to telehealth (eg, specialized nurses, technicians) Specific schedules for telehealth consultations Referrals based on existing collaboration networks Availability of up-to-date equipment |
| Sociopolitical/systemic | Initial investments in technologies and infrastructure Regional agreements and local development plans for health care services delivery based on a combination of local expertise, outreach services, and access to specialists with telehealth |
| Technological | Reliable, mobile, ergonomic, and user-friendly systems Image quality to allow diagnosis |
| Ethical/legal | Ensuring data confidentiality |
For patient follow-up, teleconsultations appear to be safe and effective. Mobile applications can be used in the remote monitoring of radiation therapy patients, not as a replacement for in-person visits but more as a triaging and planning tool. Videoconferencing-based tumor boards should replace in-person meetings. Current Web-based videoconferencing platforms are available and allow the sharing of documents. Sharing of radiation therapy treatment plans require a higher level of technology and cost. Remote radiation therapy planning, including the use of cloud-based platforms, will become a more robust and routine tool.30 , 67 , 68
The immediate future requires that research be conducted to discern the best practices in how best to deploy telemedicine resources in health care in general and for radiation oncology in particular. All new telemedicine solutions that will become routine in future practice will need to be fine-tuned and subject to monitoring and objective evaluation. The safety and ethical/legal implications of their use will need to be better regulated.
Footnotes
Disclosures: none.
References
- 1.Sermo COVID-19 HCP Sentiment Surveys. Part 1: Physician engagement with patients and remote/telehealth experiences. https://www.sermo.com/hcp-sentiment-study-series/ Available at:
- 2.International Telecommunication Union Measuring the information society report 2014. https://www.itu.int/en/ITU-D/Statistics/Documents/publications/mis2014/MIS2014_without_Annex_4.pdf Available at:
- 3.Global Digital Health Index State of digital health around the world. http://index.digitalhealthindex.org/map Available at:
- 4.ITUICT-Eye Development index (IDI): Conceptual framework and methodology. http://www.itu.int/ITU-D/ICTEYE/Indicators/Indicators.aspx Available at:
- 5.ITU Measuring digital development: ICT facts and figures 2019. https://www.itu.int/en/ITU-D/Statistics/Pages/publications/mis/methodology.aspx Available at:
- 6.Atlas of eHealth country profiles. The use of eHealth in support of universal health coverage. https://apps.who.int/iris/bitstream/handle/10665/204523/9789241565219_eng.pd;jsessionid=3F7FC8C774CF4A9A8C9BDEE08AAAB038?sequence=1 Available at:
- 7.Sabesan S., Kelly J., Evans R. A tele-oncology model replacing face-to-face specialist cancer care: Perspectives of patients in North Queensland. J Telemed Telecare. 2014;20:207–211. doi: 10.1177/1357633X14529237. [DOI] [PubMed] [Google Scholar]
- 8.Kessel K.A., Vogel M.M.E., Schmidt-Graf F. Mobile apps in oncology: A survey on health care professionals’ attitude toward telemedicine mHealth and oncological apps. J Med Internet Res. 2016;18:e312. doi: 10.2196/jmir.6399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farahani N., Pantanowitz L. Overview of telepathology. Surg Pathol Clin. 2015;8:223–231. doi: 10.1016/j.path.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Barneveld Bynkhuysen F.H., Ranschaert E.R. Teleradiology: Evolution and concepts. Eur J Radiol. 2011;78:205–209. doi: 10.1016/j.ejrad.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 11.Eedy D.J., Wootton R. Teledermatology: A review. Br J Dermatol. 2001;144:696–707. doi: 10.1046/j.1365-2133.2001.04124.x. [DOI] [PubMed] [Google Scholar]
- 12.Hilty D.M., Luo J.S., Morache C. Telepsychiatry: An overview for psychiatrists. CNS Drugs. 2002;16:527–548. doi: 10.2165/00023210-200216080-00003. [DOI] [PubMed] [Google Scholar]
- 13.Schneider P.J. Evaluating the impact of telepharmacy. Am J Health Syst Pharm. 2013;70:2130–2135. doi: 10.2146/ajhp130138. [DOI] [PubMed] [Google Scholar]
- 14.Melvin W., Needleman B., Krause K. Computer-enhanced robotic telesurgery. Initial experience in foregut surgery. Surg Endosc. 2002;16:1790–1792. doi: 10.1007/s00464-001-8192-9. [DOI] [PubMed] [Google Scholar]
- 15.Hersh W., Helfand M., Wallace J. A systematic review of the efficacy of telemedicine for making diagnostic and management decisions. J Telemed Telecare. 2002;8:197–209. doi: 10.1258/135763302320272167. [DOI] [PubMed] [Google Scholar]
- 16.Hersh W.R., Hickam D.H., Severance S.M. Diagnosis, access and outcomes: Update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(Suppl 2):S3–S31. doi: 10.1258/135763306778393117. [DOI] [PubMed] [Google Scholar]
- 17.Quek L., Kannivelu A., Pua U. 90 Y radioembolization: Telemedicine during COVID-19 outbreak, opportunity for prime time. J Nucl Med. 2020;61:780. doi: 10.2967/jnumed.120.246389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ngwa W., Sajo E., Ngoma T. Potential for information and communication technologies to catalyze global collaborations in radiation oncology. Int J Radiat Oncol Biol Phys. 2015;91:444–447. doi: 10.1016/j.ijrobp.2014.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Filippi A.R., Russi E., Magrini S.M. Letter from Italy: First practical indications for radiation therapy departments during COVID-19 outbreak. Int J Radiat Oncol Biol Phys. 2020;107:597–599. doi: 10.1016/j.ijrobp.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simcock R., Thomas T.V., Estes C. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68. doi: 10.1016/j.ctro.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NICE National Institute for Health and Care Excellence. COVID-19 rapid guideline: Delivery of radiotherapy. NICE guideline 162, March 2020. [PubMed]
- 22.Datta N.R., Heuser M., Bodis S. A roadmap and cost implications of establishing comprehensive cancer care using a teleradiotherapy network in a group of Sub-Saharan African countries with no access to radiation therapy. Int J Radiat Oncol Biol Phys. 2016;95:1334–1343. doi: 10.1016/j.ijrobp.2016.03.030. [DOI] [PubMed] [Google Scholar]
- 23.Datta N.R., Heuser M., Samiei M. Teleradiotherapy network: Applications and feasibility for providing cost-effective comprehensive radiotherapy care in low- and middle-income group countries for cancer patients. Telemed J E Health. 2015;21:523–532. doi: 10.1089/tmj.2014.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fitzpatrick D., Grabarz D., Wang L. How effective is a virtual consultation process in facilitating multidisciplinary decision-making for malignant epidural spinal cord compression? Int J Radiat Oncol Biol Phys. 2012;84:e167–e172. doi: 10.1016/j.ijrobp.2012.03.057. [DOI] [PubMed] [Google Scholar]
- 25.O'Cathail M., Sivanandan M.A., Diver C. The use of patient-facing teleconsultations in the National Health Service: Scoping review. JMIR Med Inform. 2020;8 doi: 10.2196/15380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stevens G., Loh J., Kolbe J. Comparison of recommendations for radiotherapy from two contemporaneous thoracic multidisciplinary meeting formats: Co-located and video conference. Intern Med J. 2012;42:1213–1218. doi: 10.1111/j.1445-5994.2012.02817.x. [DOI] [PubMed] [Google Scholar]
- 27.Ju H., Kim S., Read P. Development of a novel remote-controlled and self-contained audiovisual-aided interactive system for immobilizing claustrophobic patients. J Appl Clin Med Phys. 2015;16:5359. doi: 10.1120/jacmp.v16i3.5359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mailhot Vega R.B., Ishaq O.F., Ahmed I. Novel pilot curriculum for international education of lymphoma management using e-contouring. J Glob Oncol. 2018;4:1–9. doi: 10.1200/JGO.2016.008755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Belard A., Dolney D., Zelig T. Improving proton therapy accessibility through seamless electronic integration of remote treatment planning sites. Telemed J E Health. 2011;17:370–375. doi: 10.1089/tmj.2010.0199. [DOI] [PubMed] [Google Scholar]
- 30.Norum J., Bruland Ø.S., Spanne O. Telemedicine in radiotherapy: A study exploring remote treatment planning, supervision and economics. J Telemed Telecare. 2005;11:245–250. doi: 10.1258/1357633054471858. [DOI] [PubMed] [Google Scholar]
- 31.Zellmer D., Klein E., Orton C.G. Point/counterpoint. The shortage of radiation oncology physicists is addressable through remote treatment planning combined with periodic visits by consultant physicists. Med Phys. 2008;35:1167–1169. doi: 10.1118/1.2841935. [DOI] [PubMed] [Google Scholar]
- 32.Cox A., Illsley M., Knibb W. The acceptability of e-technology to monitor and assess patient symptoms following palliative radiotherapy for lung cancer. Palliat Med. 2011;25:675–681. doi: 10.1177/0269216311399489. [DOI] [PubMed] [Google Scholar]
- 33.Cunha C.E., Fernandes R., Santos C.X. Viability of mobile applications for remote support of radiotherapy patients. Rev Assoc Med Bras (1992) 2019;65:1321–1326. doi: 10.1590/1806-9282.65.10.1321. [DOI] [PubMed] [Google Scholar]
- 34.Galiano-Castillo N., Cantarero-Villanueva I., Fernández-Lao C. Telehealth system: A randomized controlled trial evaluating the impact of an internet-based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer. 2016;122:3166–3174. doi: 10.1002/cncr.30172. [DOI] [PubMed] [Google Scholar]
- 35.Kessel K.A., Vogel M.M., Alles A. Mobile app delivery of the EORTC QLQ-C30 questionnaire to assess health-related quality of life in oncological patients: Usability study. JMIR Mhealth Uhealth. 2018;6:e45. doi: 10.2196/mhealth.9486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kock A.K., Kaya R., Müller C. A mobile application to manage and minimise the risk of late effects caused by childhood cancer. Stud Health Technol Inform. 2015;210:798–802. [PubMed] [Google Scholar]
- 37.IAEA E-learning tool helps boost medical physics expertise in Asia and the Pacific. https://iaea.org/newscenter/news/e-learning-tool-helps-boost-medical-physics-expertise-in-asia-and-the-pacific Available at:
- 38.Clark J., Heifetz L., Palmer D. Telehealth allows for clinical trial participation and multimodality therapy in a rural patient with stage 4 non-small cell lung cancer. Cancer Treat Res Commun. 2016;9:139–142. doi: 10.1016/j.ctarc.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.CMS expands telehealth benefits for medicare beneficiaries during COVID-19 pandemic. https://www.astro.org/News-and-Publications/What-is-Happening-in-Washington/2020/CMS-Expands-Telehealth-Benefits-for-Medicare-Benef Available at:
- 40.AMA Key changes made to telehealth guidelines to boost COVID-19 care. https://www.ama-assn.org/delivering-care/public-health/key-changes-made-telehealth-guidelines-boost-covid-19-care Available at:
- 41.Abdel-Wahab M., Zubizarreta E., Polo A. Improving quality and access to radiation therapy—an IAEA perspective. Semin Radiat Oncol. 2017;27:109–117. doi: 10.1016/j.semradonc.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 42.Rosenblatt E., Zubizarreta E., Wondergem J. The International Atomic Energy Agency (IAEA): An active role in the global fight against cancer. Radiother Oncol. 2012;104:269–271. doi: 10.1016/j.radonc.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 43.Rosenblatt E., Acuña O., Abdel-Wahab M. The challenge of global radiation therapy: An IAEA perspective. Int J Radiat Oncol Biol Phys. 2015;91:687–689. doi: 10.1016/j.ijrobp.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 44.Abdel-Wahab M., Fidarova E., Polo A. Global access to radiotherapy in low- and middle-income countries. Clin Oncol (R Coll Radiol) 2017;29:99–104. doi: 10.1016/j.clon.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 45.Chan J., Polo A., Zubizarreta E. Access to radiotherapy and its association with cancer outcomes in a high-income country: Addressing the inequity in Canada. Radiother Oncol. 2019;141:48–55. doi: 10.1016/j.radonc.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 46.Mueller B.A., Obcemea C., Lee J. Pilot study of a radiation oncology telemedicine platform. J Radiat Oncol Inform. 2010;2:20–30. [Google Scholar]
- 47.Lewis GD, Hatch SS, Wiederhold LR, et al. Long-term institutional experience with telemedicine services for radiation oncology: A potential model for long-term utilization [e-pub ahead of print]. Adv Radiat Oncol. https://doi.org/10.1016/j.adro.2020.04.018. Accessed June 24, 2020. [DOI] [PMC free article] [PubMed]
- 48.Huh S.J., Shirato H., Hashimoto S. An integrated service digital network (ISDN)-based international telecommunication between Samsung Medical Center and Hokkaido University using telecommunication helped radiotherapy planning and information system (THERAPIS) Radiother Oncol. 2000;56:121–123. doi: 10.1016/s0167-8140(00)00179-1. [DOI] [PubMed] [Google Scholar]
- 49.Zou L., Chen X., Xu C. Design and preliminary experience of a tele-radiotherapy system for a medical alliance in China. Telemed J E Health. 2020;26:235–243. doi: 10.1089/tmj.2018.0323. [DOI] [PubMed] [Google Scholar]
- 50.Datta N.R., Mishra S.K. Indian Institute of Technology; Kharagpur, India: 2005. Teleradiotherapy network in Uttar Pradesh to provide a comprehensive radiation therapy care for cancer patients. ICMIT (Indian Conference on Medical Informatics & Telemedicine) 2005 proceedings; pp. 22–26. [Google Scholar]
- 51.Stitt J.A. A system of tele-oncology at the University of Wisconsin Hospital and Clinics and regional oncology affiliate institutions. WMJ. 1998;97:38–42. [PubMed] [Google Scholar]
- 52.IAEA New CRP: A study of e-learning for teaching and assessing competency in contouring (E33041) https://www.iaea.org/newscenter/news/new-crp-a-study-of-e-learning-for-teaching-and-assessing-competency-in-contouring-e33041 Available at:
- 53.IAEA Improving radiotherapy treatment planning for patients with nasopharyngeal carcinoma in low- and middle-income countries. https://www.iaea.org/es/projects/crp/e33039 Available at:
- 54.Rosenblatt E., Prasad R.R., Hopkins K. Africa Radiation Oncology Network (AFRONET): an IAEA telemedicine pilot project. J Int Soc Telemed eHealth. 2018;6:1–7. [Google Scholar]
- 55.Consult QD Telemedicine program broadens access to radiation oncology in Africa. https://consultqd.clevelandclinic.org/telemedicine-program-broadens-access-to-radiation-oncology-in-africa/ Available at:
- 56.Ruiz J.G., Mintzer M.J., Leipzig R.M. The Impact of e-learning in medical education. Acad Med. 2006;81:207–212. doi: 10.1097/00001888-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Agrawal S., Maurya A.K., Shrivastava K. Training the trainees in radiation oncology with telemedicine as a tool in a developing country: A two-year audit. Int J Telemed Appl. 2011;2011 doi: 10.1155/2011/230670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tan L.T. Radiotherap-e. An e-learning programme in advanced radiotherapy techniques. Radiography. 2012;18:3–4. [Google Scholar]
- 59.IAEA Human Health Campus Radiation oncology. https://humanhealth.iaea.org/HHW/RadiationOncology/index.html Available at:
- 60.IAEA Your doctor is now connected: Telemedicine helps to improve access to radiation medicine. https://www.iaea.org/newscenter/news/your-doctor-now-connected-telemedicine-helps-improve-access-radiation-medicine Available at:
- 61.Barton M.B., Thode R.J. Distance learning in the Applied Sciences of Oncology. Radiother Oncol. 2010;95:129–132. doi: 10.1016/j.radonc.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 62.IAEA COVID-19: Webinars. https://www.iaea.org/topics/health/infectious-diseases/covid-19/webinars Available at:
- 63.IAEA COVID-19 related changes in radiotherapy practice: Defining the new normal for radiation oncology departments. https://iaea.mediasite.com/Mediasite/Play/f6796808581a4528983543d5c179338d1d Available at:
- 64.Slotman B.J., Lievens Y., Poortmans P. Effect of COVID-19 pandemic on practice in European radiation oncology centers. Radiother Oncol. 2020;150:40–42. doi: 10.1016/j.radonc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zaorsky NG, Yu JB, McBride SM, et al. Prostate cancer radiotherapy recommendations in response to COVID-19 [e-pub ahead of print]. Adv Radiat Oncol. https://doi.org/10.1016/j.adro.2020.03.010. Accessed June 24, 2020.
- 66.Gagnon M.P., Duplantie J., Fortin J.P. Implementing telehealth to support medical practice in rural/remote regions: What are the conditions for success? Implement Sci. 2006;1:18. doi: 10.1186/1748-5908-1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Olsen D.R., Bruland S., Davis B.J. Telemedicine in radiotherapy treatment planning: Requirements and applications. Radiother Oncol. 2000;54:255–259. doi: 10.1016/s0167-8140(99)00185-1. [DOI] [PubMed] [Google Scholar]
- 68.Ogawa Y., Nemoto K., Kakuto Y. Construction of a remote radiotherapy planning system. Int J Clin Oncol. 2005;10:26–29. doi: 10.1007/s10147-004-0446-9. [DOI] [PubMed] [Google Scholar]