Abstract
Objective:
Given that weight gain patterns in adolescents receiving outpatient Family-Based Treatment (FBT) have not been characterized, the purpose of this study was to examine trajectories of weight gain in a group of adolescent patients with a restrictive eating disorder [e.g. anorexia nervosa (AN), atypical AN] receiving FBT. This study also examined the association of patient characteristics with weight gain trajectories, including age, diagnosis, weight suppression, presenting BMI-for-age percentile, and eating pathology.
Method:
Latent growth mixture modeling was used to identify distinct weight trajectories, as defined by change in BMI-for-age percentile, for 153 adolescents with AN or atypical AN, receiving FBT.
Results:
There were five distinct weight gain trajectory profiles for adolescents receiving FBT for a restrictive eating disorder. Younger age and greater weight suppression were associated with more rapid weight gain trajectories. A pattern of slow and consistent weight gain was associated with older age and less eating pathology.
Discussion:
There was considerable variability in weight gain trajectories in youth receiving outpatient FBT for a restrictive eating disorder. This suggests that patients’ presenting information can be used to inform expectations regarding weight gain trajectories.
Keywords: Adolescent, Anorexia Nervosa, Feeding and Eating Disorders, Weight Gain, Weight Suppression
Weight restoration is a well-established requirement for the resolution of both physical and psychological symptoms in the treatment of adolescent anorexia nervosa (AN) (Coturier & Lock, 2006; Accurso, Ciao, Fitzsimmons-Craft, Lock & Le Grange, 2014). Failure to return to a healthy weight can delay normative developmental processes, as well as contribute to medical comorbidities of the eating disorder. Similarly, research on predictors of outcome in Family Based Treatment (FBT)—the gold-standard treatment for adolescent AN— has consistently found early weight gain to be associated with good prognosis (Doyle, Le Grange, Loeb, Celio Doyle & Crosby, 2010; Le Grange, Accurso, Lock, Agras & Bryson, 2014; Madden et al., 2015, Swenne, Parling & Salonen Ros, 2017).
Given the importance of rapid weight gain, the first stage of FBT is primarily focused on weight restoration. During this stage, parents are empowered to take charge of monitoring all meals, and are charged with maximizing weight gain as the main goal. Although there is general agreement that weight gain is crucial in the treatment of AN, there has been less clarity with regards to optimal or expected weight gain trajectories in this population. Very few studies have looked at weight trajectories in outpatient samples. Though early studies, largely conducted with adult inpatient samples, have found rapid weight gain was linked to poorer outcomes, which was hypothesized to be due to challenges with patients ‘assimilating’ the gain both psychologically and physically (e.g. Herzog, Zeeck, Hartmann & Nickel, 2004), recent studies have challenged the idea that slow rate of weight gain is desirable (e.g. Casteo, Gila, Puig, Rodriguez & Toro, 2004; Garber, Michihata, Hetnal, Shafer & Moscicki, 2012).
Although the optimal rate of weight gain to support recovery is an empirical question, rate of gain—even in highly-regulated residential or inpatient settings—may not be subject to control of the treatment team. Weight gain in adult patients with AN placed on a standardized inpatient refeeding protocol has been found to be highly variable (Hart, Abraham, Franklin & Russell, 2011). Research suggests that individual characteristics have a considerable influence on both the rate and absolute amount of weight gain in patients with eating disorders (e.g. Karlsson, Clinton & Nevonen, 2013).
Weight suppression is one factor that has received empirical attention as potentially influencing rate of gain in treatment. Weight suppression is defined as the difference between an individual’s highest weight and either current or lowest weight (Lowe, 1993). Compared to those with low weight suppression, adults with high weight suppression have been found to gain more weight in treatment at a faster rate, regardless of presenting BMI (Wildes & Marcus, 2012; Berner, Shaw, Witt & Lowe 2013; Carter et al., 2015). However, the relationship between the amount and rate of weight gain and treatment outcome is unclear. One of the few studies on weight suppression in adolescents found that high weight suppression was associated with higher BMI at 6- and 10-year follow-ups (Witt et al., 2014). A study of adolescents found that high weight suppression was associated with a lower likelihood of return of menses, an important indicator of treatment outcome (Seetharaman et al., 2017).
Presenting at a relatively higher BMI and meeting criteria for what DSM-5 characterizes as atypical anorexia nervosa (atypical AN), under the Other Specified Feeding and Eating Disorders (OSFED) category, may also influence rate of weight gain during treatment. Atypical AN includes individuals who have lost a significant amount of weight but have not fallen below the “average range” (American Psychiatric Association, 2013). At present, research has yet to examine whether there are unique weight gain patterns among adolescents with atypical AN as defined by the DSM-5 criteria.
Given the lack of information on weight trajectories in treatment, this study examined patterns of BMI-for-age percentile changes in adolescents with AN, atypical AN, or sub-threshold AN receiving outpatient FBT. To our knowledge, only one previous study has looked at characteristics of weight gain and loss in adolescents, using a sample of patients with AN being readmitted for inpatient hospitalization (Lay, Jennen-Steinmetz, Reinhard, & Schmidt, 2002). Although this study did not examine different weight or BMI-for-age percentile trajectory profiles, they found that specific weight curve characteristics, including velocity of BMI increase, were related to weight changes after discharge. Given that this study looked at weight gain among individuals with eating disorders in an inpatient setting, it is unclear whether these results could be useful in describing patterns of weight gain in outpatient settings. To our knowledge, this is the first study examining patterns of weight gain in a sample of adolescents with AN treated in an outpatient setting. In particular, we were interested in weight gain patterns among adolescents receiving FBT, as this modality specifically emphasizes parent-driven weight restoration as a main priority. It also is the first study looking at patient characteristics associated with patterns of weight gain.
Although this study was largely exploratory in nature, the existing literature supports several theories about weight gain trajectories. First, given evidence that higher weight suppression is linked to a faster rate of initial gain (Wildes & Marcus, 2012; Berner et al., 2013; Carter et al., 2015), it was hypothesized that patients with higher weight suppression would experience a steeper initial weight gain trajectory as compared with patients with lower weight suppression. Similarly, based on research that links higher presenting BMI to more rapid recovery during and after treatment (Strober, Freeman & Morrell, 1999), early steep weight gain trajectories were hypothesized to be more likely in adolescents with atypical AN than AN.
Method
Participants included 153 youth, up to age 18, evaluated at The University of Chicago (n = 120) and the Mayo Clinic (n = 33), two academic medical center-based outpatient eating disorder programs. All participants 1) met DSM-IV criteria for AN or Eating Disorder Not Otherwise Specified with a presentation akin to DSM-5 atypical AN, and 2) engaged in FBT at either of the two sites. Diagnoses were made during a clinic intake. At The University of Chicago, potential participants included all those seen between 2002 and 2015. At the Mayo Clinic, potential participants were those seen between 2008 and 2013. During these time frames, there were 237 youth up to age 18 who were evaluated in The University of Chicago or Mayo Clinic Eating Disorders Programs and received a DSM-IV diagnosis of AN or Eating Disorder Not Otherwise Specified with a weight gain goal in treatment. Of those, 16 (6.8%) were missing treatment data, 7 (3.0%) were referred elsewhere for treatment, and 17 (7.2%) received individual therapy. The sample for this study is comprised of the remaining 197 youth. Of those, 153 had at least three weights recorded after their baseline weight. This sample included both completers and non-completers of FBT.
Participants provided written informed assent/consent, and all protocols were approved by The University of Chicago, the University of California, San Francisco, and Mayo Clinic Institutional Review Boards.
Intervention
All participants received outpatient FBT and were excluded if they were hospitalized for their eating disorder at any time during the course of therapy.
Assessment
Basic demographic (e.g., age, gender) and clinical information (e.g., duration of illness, psychotropic medication use) were collected during the intake interview.
Weight and height.
Patient weights (without shoes in light indoor clothing) were taken on a regularly recalibrated scale at all sessions. For the purpose of this study, weights were pulled from those measured at sessions closest to the following times: baseline, sessions 1 through 6, month 3, and month 6. Height was also regularly measured. Percent of median Body Mass Index according to Center for Disease Control (CDC) norms for age and gender (Department of Health and Human Services, 2002) was calculated for each participant at each assessment time point. Weight/height history was also examined using growth charts when available and self- and parent-report in order to identify highest historical BMI-for-age percentile (to be used in determining weight suppression). For this study, participants who had received a diagnosis of Eating Disorder Not Otherwise Specified, who were above the 15th percentile BMI for age at presentation, but engaged primarily in restrictive eating and were at a low weight as defined in the context of developmental trajectory and physical health were reclassified as having atypical AN.
Eating Disorder Examination-Questionnaire (EDE-Q, Fairburn & Beglin, 1994).
Adolescents completed the EDE-Q at intake. The EDE-Q consists of 28 items assessing eating disorder attitudes and behaviors in the past month rated on a scale from 0 to 6. The self-report questionnaire has been shown to have good reliability (Rose, Vaewsorn, Rosselli-Navarra, Wilson & Weissman, 2013) and validity (Mond, Hay, Rodgers, Owen, & Beumont, 2004). The measure yields a Global scale and four subscales (Restraint, Eating Concern, Weight Concern, and Shape Concern). Higher scores indicate greater eating disorder symptom severity.
Analyses
Latent growth mixture modeling (Muthén & Khoo, 1998; Muthén & Muthén, 2000) (LGMM) was used to identify distinct weight gain trajectories, as defined by change in BMI-for-age percentile, for youth with AN or atypical AN. This statistical approach assumes that a sample is comprised of subgroups, which can be characterized by unique growth curves or trajectories (Wiesner, Weichold, & Silbereisen, 2007). All available data were included in analyses.
Mplus 3.12 software (Muthén & Muthén, 1999–2004) was used to estimate the LGMM models. Preliminary analyses revealed that models required an intercept, as well as linear, quadratic, and cubic effects to adequately characterize weight gain trajectory classes, using participant as a clustering variable to account for repeated weight observations within participants. Separate model components were estimated for each class, and individual variation within class was allowed for the intercept, linear, and quadratic components. The variance of the cubic component was set to zero to facilitate model convergence. As a result, the LGMM models estimated both mean growth curves for each class as well as individual variation around these growth curves (Muthén & Muthén, 2000).
The optimal number of classes was determined based upon four separate fit indices. The Bayesian information criterion (BIC; Schwarz, 1978) determines model fit based on log likelihood, sample size, and number of parameters in the model. The adjusted BIC (aBIC; Sclove, 1987), which is an alternative form of the BIC, includes a correction for large sample size. The Akaike information criterion (AIC; Akaike, 1987) evaluates model fit based on log likelihood and number of parameters in the model. The Consistent Akaike information criterion (cAIC; Bozdogan, 1987) is based on the AIC and includes a penalty for models with more parameters. All of the information criterion indices above were used for comparing plausible models with the lowest values indicating the best fitting model.
Chi-square tests and one-way ANOVAs were used to compare latent classes with respect to treatment center, gender, age, diagnosis (AN v. Atypical AN), duration of illness, initial BMI-for-age percentile, highest BMI-for-age percentile, and BMI-for-age percentile suppression (difference between highest and current BMI-for-age percentile), global eating disorder psychopathology, weight concern, use of atypical antipsychotics, and number of treatment sessions.
Results
Participants were primarily non-Hispanic White (n = 145, 86.3%) girls (n = 136, 88.9%) with a diagnosis of either AN (n = 84, 54.9%) or atypical AN (n = 69, 45.1%). %). A minority were Hispanic Whites (n = 21, 13.7%), Black or African American (n = 3, 2.0%), Asian (n = 2, 1.3%), or more than one race/ethnicity (n = 2, 1.3%). Mean age was 14.73 years (SD = 2.28) with a mean duration of illness of 14.59 months (SD = 15.84) and mean BMI-for-age percentile of 20.63 (SD = 22.51). Highest historical BMI-for-age percentile was 61.20 (SD = 26.50), with an average BMI-for-age percentile suppression (difference between highest and current BMI-for-age percentile) of 40.58 (SD = 23.09) percentile points. Mean scores on the EDE-Q were as follows: global score (M = 2.55, SD = 1.60), Restraint (M = 2.70, SD = 1.87), Eating Concern (M = 1.84, SD = 1.53), Weight Concern (M = 2.70, SD = 1.79), and Shape Concern (M = 2.97, SD = 1.93). Finally, youth attended an average of 15.9 (SD = 10.41) FBT sessions. Data were available for 84.3% (n = 129) of participants at 3 months and 68.6% (n = 105) of participants at 6 months. Of those for whom data were not available, 4.6% (n = 7) and 11.1% (n = 17) were missing data due to terminating treatment prior to 3 and 6 months, respectively. The remaining data were missing due to weights not being available at those time points in treatment.
Classification of weight gain trajectories
The 5-class LGMM was the best fitting model, with three of the four information criterion indices (BIC, aBIC, and AIC) at their minimum for this model compared to the models with 1 to 4 classes (see Table 1). The AIC reached its minimum for the 4-class model. Given the agreement among these three indicators and the clinical interpretability of the 5-class solution, this model was selected as the best-fitting model (see Table 2 for model parameters). As shown in Figure 1, the mean weight trajectories across time by class represent five distinct classes. Given relatively small changes in height (cm) at 3 (M = 0.29, SD = 0.96) and 6 months (M = 0.87, SD = 1.68) and the fact that mean change in height was not associated with class, height change was not accounted for in these models other than how it factored into the calculation of BMI-for-age percentile.
Table 1.
Fit indices for one-, two-, three-, four-, and five-class solutions
| Number of Classes | BIC | aBIC | AIC | cAIC | LL | |
|---|---|---|---|---|---|---|
| 1 | 8858.3 | 8807.6 | 8809.8 | 8874.3 | −4388.9 | 16 |
| 2 | 8697.7 | 8631.3 | 8634.1 | 8718.7 | −4296.0 | 21 |
| 3 | 8612.2 | 8529.9 | 8533.4 | 8638.2 | −4240.7 | 26 |
| 4 | 8568.7 | 8470.6 | 8474.8 | 8599.7 | −4206.4 | 31 |
| 5 | 8568.5 | 8454.6 | 8459.4 | 8604.5 | −4193.7 |
BIC = Bayesian information criterion; aBIC = sample-size adjusted BIC; AIC = Akaike information criterion; cAIC = consistent Akaike information criterion; LL = log likelihood.
Table 2.
Model parameters for one-, two-, three-, four-, and five-class solutions
| Class | Intercept | Linear | Quadratic | Cubic |
|---|---|---|---|---|
| Class 1 | 7.9 | 0.8 | 0.1 | 0.0 |
| Class 2 | 15.6 | 5.8 | −0.3 | 0.0 |
| Class 3 | 3.4 | 23.8 | −2.1 | 0.1 |
| Class 4 | 61.2 | 1.4 | −0.2 | 0.0 |
| Class 5 | 14.3 | 11.7 | −0.9 | 0.0 |
Figure 1.
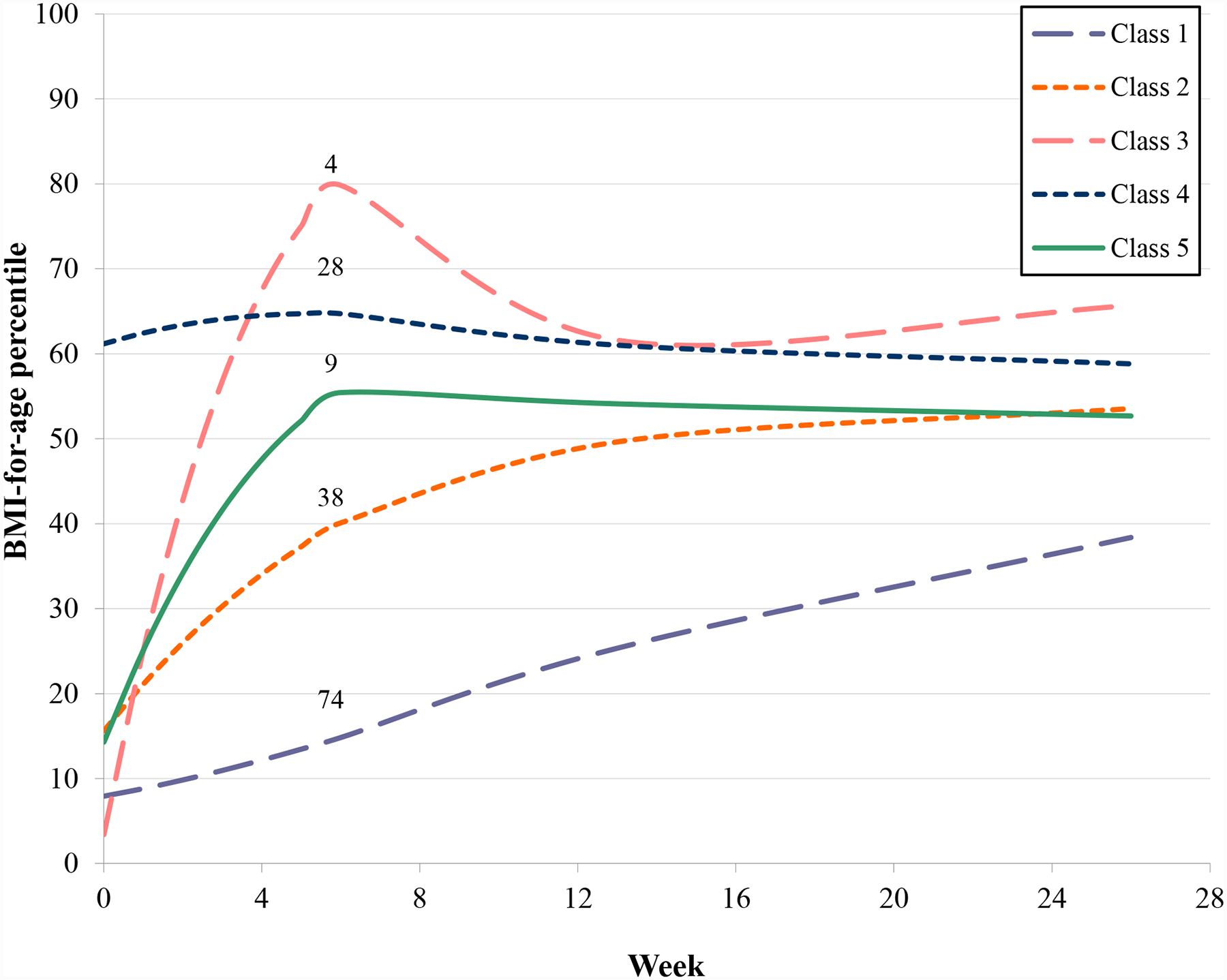
Five-class solution for weight gain trajectories
Class 1, labeled “Slow and steady gains,” is characterized by low initial BMI-for-age percentile that improves slowly and steadily; on average, youth in this class achieved a BMI-for-age percentile just below 40 after six months of FBT. This represents the largest class and accounts for approximately half of youth (48.4%, n = 74). Class 2, labeled “Moderate gains with mid-treatment maintenance,” is characterized by moderate initial gains in BMI-for-age percentile that very slowly leveled off to maintenance by three months into FBT. This class accounts for about one quarter of all youth (24.8%, n = 38). Class 3, labeled “Dramatically rapid early gains that stabilize at the 65th percentile,” is characterized by substantial gains in BMI-for-age percentile from below the 5th percentile to the 80th percentile within six sessions of FBT, followed by loss to the 60th BMI-for-age percentile by three months and ultimately stabilization around the 65th BMI-for-age percentile by six months of FBT. This trajectory is only representative of 2.6% (n = 4) of youth, but classifies a distinct—albeit rare—pattern of weight gain. Class 4, labeled “Maintenance at the 60th percentile,” is characterized by youth who have an initial BMI-for-age percentile above the median (60) and steadily gain a small amount of weight that returns to their initial BMI-for-age percentile by three months of FBT. This class accounts for 18.3% (n = 28) of youth. Finally, Class 5, labeled “Rapid gains with early stabilization,” is characterized by early rapid gains in BMI-for-age percentile that peaks at session 6 of FBT and remains very stable thereafter (5.9%, n = 9). Both Classes 2 and 5 stabilize just above median BMI-for-age.
Predictors of weight gain trajectory class
Classes differed by age (F = 3.52, p = .009), with significantly younger participants in Class 3 (M = 11.11) than Classes 1 (M = 15.07, p = .006), 2 (M = 14.45, p = .037), and 4 (M = 14.95, p ˂ .012), but not 5 (M = 14.13). Significant differences between classes were also found by diagnosis (AN v. atypical AN: Pearson χ2 = 24.58, p < .001), such that individuals with atypical AN were more likely to belong to Class 4 (82.1% membership) than to Classes 1 (31.1%), 2 (36.8%), 3 (25.0%), or 5 (22.2%). Classes were also characterized by current and prior BMI-for-age percentiles. Initial BMI-for-age percentile differed by class (F = 49.97, p ˂ .001), with Class 4 youth having a significantly higher initial BMI-for-age percentile (M = 55.93) than all other classes (M range: [9.84,17.55], all p’s ˂ .001), as well as significantly higher historical BMI-for-age percentiles (i.e., highest BMI-for-age percentile: M = 85.67) than Classes 1 (M = 49.71, p ˂ .001), 2 (M = 64.71, p = .003), and 5 (M = 57.31, p = .014), but not Class 3 (M = 77.96), and Class 2 having significantly higher historical BMI-for-age percentiles than Class 1 (p = .012). Similarly, BMI-for-age percentile suppression (difference between highest and current BMI-for-age percentile) differed by class (F = 3.59, p = .008), with Class 4 youth having relatively lower weight suppression (M = 29.74) than Classes 2 (M = 47.16, p = .018) and 3 (M = 63.83, p = .038), but not Classes 1 (M = 39.87) or 5 (M = 40.58). Finally, eating disorder psychopathology (as measured by the EDE-Q) differed by class. Global eating disorder psychopathology (F = 5.70, p < .01) was significantly higher in Class 4 (M = 3.44) than Classes 1 (M = 2.21, p = .006) and 3 (M = 0.33, p = .001) but not 2 (M = 2.77) or 5 (M = 2.13) and higher in Class 2 than 3 (p = .024). Weight concern was also higher in Class 4 (M = 3.86) than Classes 1 (M = 2.30, p = .001), 3 (M = 0.80, p = .007), 3 (M = 0.33), and 5 (M = 2.01, p = .036) but not 2 (M = 2.79). Classes did not differ with respect to treatment center, gender, duration of illness, use of atypical antipsychotics, or number of treatment sessions (ps > .10).
Early treatment response associated with weight gain trajectory class
Previous research has identified an early weight gain cut-point of 6.5 pounds by session 4 as a potent predictor of end of treatment remission (Le Grange, Accurso et al., 2014). For the 128 participants (83.7%) with session 4 data, 30.5% were classified as early responders (i.e., gaining ≥6.5 pounds from baseline to session 4). Significant differences in early treatment response were found between classes (Pearson χ2 = 44.79, p ˂ .001), such that Classes 3 and 5 were made up entirely of early responders. Early responders were also significantly more likely to belong to Class 2 (55.9%) than other classes, and there were fewer early responders in Classes 1 (9.4%) and 4 (23.8%).
Discussion
The purpose of this study was to determine patterns of weight gain, as defined by change in BMI percentile for age, in young patients with restrictive eating disorders receiving FBT. The findings suggest that weight gain is highly variable in FBT for AN. The best-fit LGMM model suggests that there are five distinct weight trajectory profiles for these adolescents. Although more research is necessary to understand predictors of weight gain trajectories in restrictive eating disorders and how they relate to treatment outcome, the identification of these trajectories has implications for clinical practice, including preparing caregivers for expected weight gain trajectories early in treatment to minimize frustration and burnout.
Interestingly, preliminary findings from this study did not support the hypothesis that individuals with atypical AN would have weight trajectories characterized by early steep weight gain. In fact, patients in Class 4, which was characterized by the shallowest slope of gain, had significantly higher rates of atypical AN as compared to other classes. Additional study is needed to clarify whether this pattern of weight gain in these patients represents treatment success or failure to establish true weight restoration.
Consistent with the literature, this study suggests that high weight suppression may be linked to early, rapid weight gain. Class 4 had less weight suppression as compared to Classes 2 and 3, but not Class 1. However, the lack of significant weight suppression in Class 5 is counter to what was expected. Regardless, patients with higher weight suppression were more likely to have a large initial surge of weight gain, as seen in Class 3, or at least have treatment and weight gain proceed in line with expectations, as seen in Class 2. In other words, highly weight suppressed adolescents have the potential for rapid and greater weight gain, and clinicians should prepare caregivers for this possibility so that when it occurs, they do not react to it as problematic and inadvertently diminish progress.
Class 1, characterized by slow yet steady rates of gain, represented the largest group of patients. Without outcome data, it is unclear whether this class is associated with treatment success or failure, though the group had significantly more patients fail to reach an early weight gain cut-off point of 6.5 pounds in 4 weeks. Because it has been well established that early weight gain within the first four weeks of treatment is strongly linked to an increased probability of success in FBT (Doyle et al., 2010; Le Grange et al., 2014; Madden et al., 2015, Swenne, et al. 2017), in addition to the potential for family burnout and diminished quality of life associated with longer treatment duration, this profile might represent a subset of adolescents who would ultimately benefit from more intensive or adapted interventions, but who advance—albeit more slowly—in FBT.
These patients tended to be a bit older and were more likely to have AN, as opposed to atypical AN. Class 1 individuals also endorsed less weight and shape concerns than other groups. It is possible that this slightly older patient group represents a more “savvy” treatment group, who, despite presenting at very low BMI percentiles, are better able to minimize symptoms and thus less likely to report all cognitive symptoms on a self-report measure. This may be linked to slower treatment progress, as this lack of expressed cognitive symptoms may impede parents’ ability to recognize the seriousness of the eating disorder. Consequently, parents might be more ambivalent about the need for aggressive refeeding, targeted weight restoration, and intensive parental meal monitoring, as is crucial in stage 1 of FBT.
Class 2, representing the second largest group, was more consistent with what might be theoretically considered a textbook treatment response. This group was characterized by initial moderate weight gain that leveled off, potentially at their set point range, though without end-of-treatment outcome data, this remains speculative. This group was marked by moderately low BMI-for-age percentiles, levels of weight suppression, and EDE-Q scores; in other words, their presentation on a range of metrics was typically in the middle of that of the larger sample. Early responders were significantly more likely to belong to this group as compared to Classes 1 and 4. It is possible that this Class was in a clinical “sweet spot”—severe and typical enough to prompt recognition and action from parents without being overly severe so as to cause disproportionate challenges to implementing FBT.
Though it represented a small group of patients, Class 5 was similar to Class 2 in its steady and steep weight gain, as would be expected from a successful course of FBT. Initial gains were followed by weight leveling off at what potentially is a set point range, though again, without outcome data, this remains speculative. As compared to Class 2, initial gains were somewhat more rapid, but overall the trajectories began and ended near the same place. Of note, this group was entirely comprised of early responders, or those who reached a threshold of 6.5 pounds in 4 weeks. Consistent with the findings that FBT is particularly effective for younger patients, members of this class were also somewhat younger, which might explain why their initial weight gain progressed so quickly.
Despite being the smallest group, Class 3 was robust across numerous models. The group was characterized by a large, rapid initial surge in weight, and then what appears to be a regression to the mean, with weight decreasing to near the 60th percentile. This was a significantly younger group, with fewer cognitive symptoms (which may be related to their younger age) as compared with other classes. This group was also entirely comprised of early responders to treatment. Although there was insufficient power to determine statistical significance, Class 3 descriptively had the highest BMI-for-age percentile of any group, a finding that requires replication in larger studies. The question of whether Class 3’s ultimate drop in BMI-for-age percentile is beneficial is complicated by irregularities in calculating target or expected body weight (Le Grange et al., 2012; Lebow, Sim & Accurso, 2017). It should also be noted that it is unclear whether the subsequent dip in BMI-for-age percentile is related to actual weight loss. Speculation that this decrease in BMI might be related to patients recouping height deficits was not borne out by data, as this class did not differ from the others in mean change to height.
Class 4 was much larger, and was characterized by weight maintenance, or a small amount of gain around the 60th percentile. Again, it is unclear whether this represents a treatment failure or if these were a group of adolescents who needed only a small amount of weight gain to reverse physical, behavioral, and cognitive eating disorder symptoms. Interestingly, this group was characterized by significantly higher rates of atypical AN and the highest scores on the EDE-Q. A recent case series by Hughes et al. (2017) found that patients with atypical AN treated with FBT experienced significant decreases in eating disorder symptoms with no significant change in percent of median BMI for age and gender. Authors concluded that these individuals may have needed less weight gain to be fully restored, suggesting that adolescents in Class 4 might represent treatment success, despite the relatively small amount of weight gain.
Conversely, however, some data suggest that individuals with atypical AN are identified later in their illness trajectory and typically have a larger decrease in BMI between illness onset and presentation for treatment (Lebow, Sim & Kransdorf, 2015), suggesting these patients do need substantial weight gain to return to baseline. It should be noted that, similar to Class 1, this group had significantly fewer early responders with regards to weight gain as compared to Classes 2, 3 and 5. It is possible that, since patients in Class 4 tracked higher than average BMI from the beginning of treatment, parents or even providers, were never wholly convinced these patients needed weight restoration consistent with their historical growth pattern, and may not have pushed FBT to a degree commensurate with other classes. In this way, the relatively flat weight trajectory might be interpreted as representing premature discontinuation of weight restoration.
A notable limitation of this study is the small sample size. Further, there were an exceedingly small number of participants in Classes 3 and 5, so the solution is not very robust. An additional limitation is the lack of long-term outcome data, which restricts our ability to draw conclusions about optimal weight trajectories. Given the sample size and statistical methods used, this exploratory study provides several possible hypotheses about factors associated with weight gain trajectories that should be tested with larger samples in future studies. Further, as this sample of adolescents was restricted in age and to those participating in FBT within two academic medical centers, it may not represent patients of a broader age span, within other types of outpatient treatment, or treatment settings. Finally, because we do not have access to data on treatment outcome, it is unclear how these weight trajectories relate to re-nourishment or remission. As a result, future research to elucidate these relationships is necessary.
Despite these limitations, this study represents the first attempt to clarify the ways in which weight restoration occurs in outpatient settings. Given that a major part of the clinician’s role in stage 1 of FBT is to assess rate of weight gain, having more information about typical rates and trajectories of weight gain in treatment for adolescent AN has substantial clinical utility.
In summary, this study found five classes of weight gain trajectories among adolescents with restrictive eating disorders treated with FBT. Although we were not able to examine post-treatment outcomes associated with these classes, younger age and weight suppression were associated with more rapid weight gain trajectories. A pattern of steady, yet slow rate of weight gain was associated with older age and lower scores on the EDE-Q. Additional research with larger samples is needed to better understand patterns associated with outcomes. Such research will have important implications for clinical decision-making, including providing families with sufficient and appropriate support during stage I of FBT, as well as the appropriateness of patients for continuing in FBT as compared to higher levels of care.
References
- Accurso EC, Ciao AC, Fitzsimmons-Craft EE, Lock JD & Le Grange D (2014). Is weight gain really a catalyst for broader recovery?: The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behaviour Research and Therapy,56, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akaike H (1987). Factor analysis and AIC InSelected Papers of Hirotugu Akaike(pp. 371–386). Springer, New York, NY. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders(5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Berner L, Shaw J, Witt A & Lowe M (2013). The relation of weight suppression and body mass index to symptomatology and treatment response in anorexia nervosa. Journal of Abnormal Psychology 122(3), 694–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozdogan H (1987). Model selection and Akaike’s information criterion (AIC): The general theory and its analytical extensions. Psychometrika,52(3), 345–370. [Google Scholar]
- Carter F, Boden J, Jordan J, McIntosh V, Bulik C & Joyce P (2015). Weight suppression predicts total weight gain and rate of weight gain in outpatients with anorexia nervosa. International Journal of Eating Disorders, 48, 912–918. [DOI] [PubMed] [Google Scholar]
- Castro J, Gila A, Puig J, Rodriguez S, & Toro J (2004). Predictors of rehospitalization after total weight recovery in adolescents with anorexia nervosa. International Journal of Eating Disorders,36(1), 22–30. [DOI] [PubMed] [Google Scholar]
- Couturier J & Lock J (2006). What is remission in adolescent anorexia nervosa? A review of various conceptualizations and quantitative analysis. International Journal of Eating Disorders,39(3), 175–183. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services. (2002). 2000 CDC growth charts for the United States: Methods and development. Vital and Health Statistics, 11(246). [PubMed] [Google Scholar]
- Doyle P, Le Grange D, Loeb K, Celio Doyle A, Crosby R (2010). Early response to Family-Based Treatment for adolescent anorexia nervosa, International Journal of Eating Disorders, 43, 659–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C & Beglin S (1994). Assessment of eating disorders: Interview or self-report questionnaire. International Journal of Eating Disorders, 16(4), 363–370. [PubMed] [Google Scholar]
- Garber A, Michihata N, Hetnal K, Shafer M & Moscicki A, (2012). A prospective examination of weight gain in hospitalized adolescents with anorexia nervosa on a recommended refeeding protocol. Journal of Adolescent Health, 50(1), 24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart S, Abraham S, Franklin R & Russell J (2011), Weight changes during inpatient refeeding of underweight eating disorder patients. European Eating Disorders Review, 19, 390–397. [DOI] [PubMed] [Google Scholar]
- Herzog T, Zeeck A, Hartmann A & Nickel T (2004). Lower targets for weekly weight gain lead to better results in inpatient treatment of anorexia nervosa: A pilot study. European Eating Disorders Review, 12, 164–168. [Google Scholar]
- Hughes EK, Le Grange D, Court A, & Sawyer SM (2017). A case series of family-based treatment for adolescents with atypical anorexia nervosa. International Journal of Eating Disorders,50(4), 424–432. [DOI] [PubMed] [Google Scholar]
- Karlsson G, Clinton D, & Nevonen L (2013). Prediction of weight increase in anorexia nervosa. Nordic Journal of Psychiatry,67(6), 424–432. [DOI] [PubMed] [Google Scholar]
- Lay B, Jennen-Steinmetz C, Reinhard I & Schmidt M (2002). Characteristics of inpatient weight gain in adolescent anorexia nervosa: Relation to speed of relapse and re-admission. European Eating Disorders Review, 10, 22–40. [Google Scholar]
- Lebow J, Sim L & Accurso E (2017). Is there clinical consensus in defining weight restoration for adolescents with anorexia nervosa? Eating Disorders The Journal of Treatment and Prevention. [DOI] [PubMed] [Google Scholar]
- Lebow J, Sim L & Kransdorf L (2015). Prevalence of a history of overweight and obesity in adolescents with restrictive eating disorders. Journal of Adolescent Health,56(1), 19–24. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Accurso EC, Lock J, Agras S & Bryson SW (2014). Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. International Journal of Eating Disorders,47(2), 124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Doyle PM, Swanson SA, Ludwig K, Glunz C & Kreipe RE (2012). Calculation of expected body weight in adolescents with eating disorders. Pediatrics,129(2), e438–e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Agras W, Moye A, Bryson S, Jo B & Kraemer H (2012). Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behaviour Research and Therapy,50(2), 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe M (1993). The effects of dieting on eating behavior: A three-factor model. Psychological Bulletin,114(1), 100. [DOI] [PubMed] [Google Scholar]
- Lund B, Hernandez E, Yates W, Mitchell j., McKee P & Johnson C (2009). Rate of inpatient weight restoration predicts outcome in anorexia nervosa. International Journal of Eating Disorders 42, 301–305. [DOI] [PubMed] [Google Scholar]
- Madden S, Miskovic-Wheatley J, Wallis A, Kohn M, Hay P & Touyz S (2015). Early weight gain in Family-Based Treatment predicts greater weight gain and remission at the end of treatment and remission at 12-month follow-up in adolescent anorexia-nervosa. International Journal of Eating Disorders, 48, 919–922. [DOI] [PubMed] [Google Scholar]
- Mond J, Hay P, Rodgers B, Owen C & Beumont P (2004). Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy,42(5), 551–567. [DOI] [PubMed] [Google Scholar]
- Muthén B & Khoo S (1998). Longitudinal studies of achievement growth using latent variable modeling. Learning and Individual Differences,10(2), 73–101. [Google Scholar]
- Muthén L & Muthén B (1998–2004). Mplus User’s Guide. Sixth Edition Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Muthén B,& Muthén L (2000). Integrating person‐centered and variable‐centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical and Experimental Research,24(6), 882–891. [PubMed] [Google Scholar]
- Rose J, Vaewsorn A, Rosselli-Navarra F, Wilson G & Weissman R (2013). Test-retest reliability of the eating disorder examination-questionnaire (EDE-Q) in a college sample. Journal of Eating Disorders,1(1), 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. Annals of Statistics,6(2): 461–464. [Google Scholar]
- Sclove S (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika,52(3), 333–343. [Google Scholar]
- Seetharaman S, Golden N, Halpern-Felsher B, Peebles R, Payne A & Carlson J (2017). Effect of a prior history of overweight on return of menses in adolescents with eating disorders. Journal of Adolescent Health, 60(4), 469–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strober M, Freeman R, & Morrell W (1999). Atypical anorexia nervosa: Separation from typical cases in course and outcome in a long‐term prospective study. International Journal of Eating Disorders,25(2), 135–142. [DOI] [PubMed] [Google Scholar]
- Swenne I, Parling T, & Salonen Ros H (2017). Family-based intervention in adolescent restrictive eating disorders: early treatment response and low weight suppression is associated with favourable one-year outcome. BMC Psychiatry,17, 333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiesner M, Weichold K & Silbereisen R (2007). Trajectories of alcohol use among adolescent boys and girls: Identification, validation, and sociodemographic characteristics. Psychology of Addictive Behaviors,21(1), 62. [DOI] [PubMed] [Google Scholar]
- Wildes J & Marcus M (2012). Weight suppression as a predictor of weight gain and response to intensive behavioral treatment in patitns with anorexia nervosa. Behaviour Research and Therapy 50, 266–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt A, Berkowitz S, Gillberg C, Lowe M, Rastam M & Wentz E (2014). Weight suppression and body mass index interactg to predict long-term weight outcomes in adolescent-onset anorexia nervosa. Journal of Consulting and Clinical Psychology, 82(6), 1207–1211. [DOI] [PubMed] [Google Scholar]


