Abstract
In Duchenne muscular dystrophy (DMD) patients, absence of dystrophin causes muscle wasting by impacting both the myofiber integrity and the properties of muscle stem cells (MuSCs). Investigation of DMD encompasses the use of MuSCs issued from human skeletal muscle. However, DMD-derived MuSC usage is restricted by the limited number of divisions that human MuSCs can undertake in vitro before losing their myogenic characteristics and by the scarcity of human material available from DMD muscle. To overcome these limitations, immortalization of MuSCs appears as a strategy. Here, we used CDK4/hTERT expression in primary MuSCs and we derived MuSC clones from a series of clinically and genetically characterized patients, including eight DMD patients with various mutations, four congenital muscular dystrophies and three age-matched control muscles. Immortalized cultures were sorted into single cells and expanded as clones into homogeneous populations. Myogenic characteristics and differentiation potential were tested for each clone. Finally, we screened various promoters to identify the preferred gene regulatory unit that should be used to ensure stable expression in the human MuSC clones. The 38 clonal immortalized myogenic cell clones provide a large collection of controls and DMD clones with various genetic defects and are available to the academic community.
Keywords: human muscle stem cells, immortalization, degenerative myopathies, Duchenne muscular dystrophy, congenital myopathies
1. Introduction
Muscular dystrophies are a group of inherited incurable myopathies characterized by ongoing rounds of skeletal muscle degeneration and regeneration. Duchenne muscular dystrophy (DMD) is caused by mutations in the dystrophin gene, which lies on the X chromosome, where the loss of a functional dystrophin protein causes muscle wasting with an incidence of 1 in 5000 to 1/6000 boys [1]. In these patients, dystrophin protein deficiency causes recurring myofiber lesions, leading to the continuous activation of the regeneration process that is sustained by muscle stem cells (MuSCs). The ongoing regeneration eventually leads to the exhaustion of MuSC capacities to repair the muscle. Over time, progressive muscle wasting and increased fibrosis lead to skeletal muscle loss of function [2]. In order to understand the cellular and molecular mechanisms involved in DMD, mouse models are commonly used. The mdx mouse model, which bears a mutation in the dystrophin gene, presents a mild clinical phenotype when compared to the human pathology due to several factors, including compensation by the related subsarcolemmal protein utrophin and the presence longer telomeres in murine MuSCs [3,4]. Past studies have used human MuSCs isolated from skeletal muscle of DMD patients to understand the mechanisms leading to MuSC exhaustion. Indeed, MuSCs isolated from healthy muscle biopsies recapitulate adult myogenesis in vitro, including activation, proliferation, differentiation and eventual myoblast fusion [5]. Initial attempts to characterize the behavior of DMD-derived MuSCs encountered two major issues. The first is that MuSC cultures were not pure, as they also contained non-myogenic cells. This issue has been overcome by the use of cell sorting techniques to obtain pure populations of myogenic cells. For this purpose, primary human MuSCs are usually sorted based on their expression of CD56 (NCAM) on their cell surface. In human skeletal muscle, CD56 is expressed by quiescent satellite cells, activated myoblasts and young regenerating myofibers [6]. The second issue, still unresolved, is the limited number of cell divisions that human MuSCs can undertake in vitro before losing their myogenic characteristics and/or entering into replicative senescence [7]. To overcome this limitation, along with the scarcity of human material available from DMD muscle, immortalization of MuSCs appears to be a good solution to obtain sufficient material for investigating the molecular mechanisms at work in human dystrophic cells.
Over the past decades, various strategies have been used to bypass the senescence state of human MuSCs. In a first approach, transduction of cells with the viral oncogene simian SV40 large T antigen was able to extend the maximum number of cell divisions by an additional 20 rounds [8]. However, this approach often leads to abnormal chromosomal recombination and to an impaired expression of the myogenic program [8,9,10]. In an alternate approach, ectopic expression of the reverse transcriptase unit of human telomerase (hTERT) further increases the maintenance of MuSCs in vitro, while preserving their differentiation potential. Expression of hTERT was also shown to improve cell survival by counteracting telomere shortening [11,12]. However, the hTERT-expressing MuSCs could not be immortalized due to their propensity to undergo cycle arrest [13]. In an effort to prevent cell cycle arrest, an alternative method was developed that consists of transducing MuSCs with cyclin-dependent kinase 4 (CDK4) or cyclin D1 (CCND1) genes to ensure their proliferative capacity [14,15,16]. Building on these various approaches, the field has adopted a technology whereby the expression of cell cycle drivers CDK4 or CCND1 is combined with that of hTERT to allow the immortalization of human MuSCs that maintain both their differentiation potential and normal karyotype [14,17]. Immortalization of CD56pos purified primary human MuSCs with hTERT and CDK4 transgenes has been performed by several groups [15,18,19]. Transcriptomic analysis showed that immortalized lines retain the myogenic expression patterns of their parent primary populations during myogenic differentiation [19]. Since the development of the immortalization technology, a series of studies have confirmed that this approach can be applied to a variety of neuromuscular diseases, including DMD, myotonic dystrophy 1, congenital muscular dystrophy type 1A, facioscapulohumeral muscular dystrophy, limb-girdle muscular dystrophy type 2B and oculopharyngeal muscular dystrophy [15,18,19,20,21].
In the present study, we used CDK4/TERT expression in primary MuSCs to derive novel MuSC clones from a series of DMD, congenital muscular dystrophies (that can serve as non-DMD myopathic samples) and age-matched control muscles. Several clones were established and characterized for each patient. Previous works have cloned immortalized hMuSCs using low cell density culture and/or a clonal ring [14,15,22], which cannot prevent the presence of cell doublets. Here, we used FACS-derived single-cell cultures to establish several genetically homogeneous immortalized MuSC clones from the same donor, in order to circumvent any impact of the insertion site of the lentiviruses in the genome. All clones were tested to ensure they retained their myogenic characteristics and differentiation potential while ensuring their genomic integrity. Finally, as studies utilizing these cell clones will surely encompass over expression/inhibition of genes of interests, we screened a panel of promoters to identify the preferred gene regulatory unit that should be used in plasmids to ensure expression in these human MuSC clones. The 38 clonal immortalized myogenic cell lines issued from genetically and clinically characterized patients provide a large collection of DMD clones with various genetic defects that are available to the academic community.
2. Materials and Methods
2.1. Patients
Biopsies were obtained from deltoideus medialis of 8 DMD patients, 4 patients suffering from congenital muscular dystrophies (CMD) and 3 controls (patients showing after investigation no clinical signs of neuromuscular diseases and for whom all the diagnosis workup was normal) used as age-matched control. Biopsies were obtained after institutionally approved protocol and parents or legal representatives gave their written informed consent for the children’s participation to the study (protocol registered at the Ministère de la Recherche and Cochin Hospital Cell Bank, Paris, agreement n°DC-2009-944).
2.2. Immortalization of Primary Human MuSCs
After mechanic dissociation of the muscle, enzymatic digestion was performed in DMEM medium (Gibco #10566, Thermofischer Scientific, Waltham, MA, USA) containing 6000 UI/mL Collagenase IA (Sigma-Aldrich#C2674, Merck KGaA, Darmstadr, Germany) for 60–90 min at 37 °C under gentle stirring. Primary cells were cultured and expanded in HAM-F10 medium (Gibco #11550), containing 15% foetal bovine serum (FBS) (Abcys, EurobioScientific, Les Ullis, France, #S1810-500), 100 U/mL penicillin, 100 µg/mL streptomycin (Gibco #15140) and 1% HEPES 1M. Cells were seeded at 5000 cells per cm2 in 6-well plates and 6 h later (once the cells are adherent), the medium was replaced by transduction medium (DMEM:M199 medium (Invitrogen #41150, Thermofischer Scientific,) (4:1) containing 10% FBS, 2.5 ng/mL HGF (Sigma-Aldrich, Merck, #H9661), 40 ng/mL Dexamethasone (Sigma-Aldrich #D4902)) containing CDK4 and HTERT lentiviruses. Two lentiviruses for CDK4 and HTERT expression were produced and titrated by the Viral Vectors and Gene Transfer facility at Université René Descartes, Paris. pTrip-CMV-CDK4-DeltaU3 and pTrip-PGK-puromycin-polyA CMV-hTERT variant 1–2 plasmids were used to produce ∆U3 SIN lentiviruses in HEK293T and were purified by ultracentrifugation. Titration was performed in HTC116 cells. Transduction was performed overnight with the 2 lentiviruses to a final concentration of 3 lentiviral particles/cell and medium was replaced by selection medium composed of transduction medium containing 1 µg/mL puromycin (Sigma-Aldrich #P8833). After selection, cells were expanded for about 3 weeks, and supernatants were tested for the presence of HIV-derived p24 using ELISA (INNOTEST, Fujirebio Inc., Courtaboeuf, France), and all the 15 cultures were shown to be negative.
2.3. Clonal Isolation and Selection of Clones
After puromycin selection, immortalized human MuSCs (iHMuSCs) were labelled with anti-CD56 APC-conjugated antibodies (BD Pharmingen #555518, BD Biosciences, Franklin Lakes, NJ, USA) and were sorted using a BD FACSAria II to be seeded at one cell per well in 96-well plates. Cells were cultured in growth medium (skeletal muscle basal medium (PromoCell GmbH #C23260, Heidelberg, Germany), containing skeletal muscle supplemental mix (PromoCell #C39365), 10% FBS, 100 U/mL penicillin and 100 µg/mL streptomycin). All along the culture procedure, expression of CD56 was monitored using anti-CD56 APC-conjugated antibodies and a FACSCantoII flow cytometer (BD Biosciences). Growth curves for each clone were built using the number of cells over time of culture. The population doubling was measured as
| (1) |
The population doubling time (PDT) was also calculated, using the population doubling over the number of days between T0 and T1, where T0 is the day of seeding and T1 the day of the next trypsinization. T0 was the time of seeding and T1 the time when the culture was stopped.
2.4. Assessment of the Myogenic Nature of iHMuSCs
IHMuSCs were seeded at 3000 cells per cm2 in 12-well plates containing glass coverslips and were grown in growth medium. After 48 h, cells were washed with phosphate-buffered saline solution (PBS), fixed in formaldehyde 4% for 10 min at room temperature (RT) and were permeabilized in triton X-100 0.1% for 10 min at RT. Immunolabeling was carried out using mouse anti-Pax7 (1:50, Developmental Studies Hybridoma Bank, #PAX7) and rabbit anti-desmin (1:200, Abcam #ab32362) antibodies labelled with donkey anti-mouse IgG and anti-rabbit IgG antibodies (1:200, Jackson ImmunoResearch #715-095-150 and #711-095-152). Nuclei were labeled with Hoechst (Sigma-Aldrich #B2261) for 10 sec at RT, and mounting was performed in Fluoromount (Sigma-Aldrich #F4680).
2.5. Two-Dimensional Differentiation Assays
iHMuSCs were seeded at 12,000 cells per cm2 in 12-well plates containing glass coverslips and were grown in growth medium for 4 days. Growth medium was replaced by differentiation medium (skeletal muscle basal medium containing 100 µg/mL transferrin (Sigma-Aldrich #T3309), 10 µg/mL human insulin (Sigma-Aldrich #I2643), 100 U/mL penicillin and 100 µg/mL streptomycin) and cells were further incubated for 5 days. Cells were washed with PBS, fixed in formaldehyde 4% for 10 min at RT and were permeabilized in triton X-100 0.1% for 10 min at RT. Immunolabeling was carried out using rabbit anti-desmin (1:200, at 4 °C overnight, Abcam #ab32362, Cambridge, UK) and/or rabbit anti-dystrophin (1:50, at 4 °C overnight, Abcam #15277) antibodies revealed with donkey anti-rabbit IgG and/or anti-mouse IgG antibodies. Nuclei were labeled with Hoechst for 10 sec at RT, and mounting was performed in Fluoromount.
2.6. Three-Dimensional Differentiation Assays
Twelve-well plates were coated with 500 µL of diluted Matrigel (Matrigel:Growth medium [1v:9v]) for 30 min at 37 °C. Wells were washed twice with PBS, and iHMuSCs were seeded at 30,000 cells per cm2 in growth medium. After 6 h of incubation, medium was replaced with differentiation medium. One day later, medium was removed and cells were covered with a thin layer of diluted Matrigel without serum (Matrigel:skeletal muscle basal medium without serum [1v:2v]). Covered cells were incubated for 30 min at 37 °C, and following Matrigel solidification, 500 µL of differentiation medium were added and cells were further incubated for 4 days. Cells were washed twice with PBS, fixed in formaldehyde 4% for 10 min at RT and permeabilized in triton X-100 0.1% at RT. Immunolabeling was performed using mouse anti-myosin heavy chain (MHC) antibodies (1:100, Developmental Studies Hybridoma Bank #MF20, Iowa city, IA, USA) revealed with donkey anti-rabbit IgG antibodies. Phalloidin conjugated with Atto 488 (Sigma #49409) was added to label actin. Nuclei were labeled with Hoechst for 10 sec at RT, and cells were mounted in Fluoromount.
2.7. Propidium Iodide Staining
iHMuSCs were seeded in proliferation condition at 3000 cells per cm2 for 3 days. Cells were trypsinated, washed with PBS and fixed with 66% of cold ethanol overnight at −20°C. Fixed cells were washed with PBS and stained for 30 min with 50 µg/mL propidium iodide (Sigma-Aldrich #P4864) and 10 µg/mL RNAse A (ThermoFisher Scientific #12091-021). Cells were washed with PBS and were analyzed using a FACSCantoII flow cytometer.
2.8. Plasmid Construction
The pLenti-GIII-CMV-mCherry plasmid was built by insertion of a PCR-amplified mCherry gene in pLenti-GIII-CMVplasmid (ABMgood #LV587), digested at cutting sites NheI-XhoI, using a T4 ligase (Invitrogen #15224025). The pLenti-GIII-EF1α-mCherry, pLenti-GIII-PGK-mCherry and pLenti-GIII-EF1a-mCherry plasmids were built by insertion of PCR amplified EF1α, PGK or UbC promoters in the previously built pLenti-GIII-CMV-mCherry plasmid, digested at either AvrII and NheI cutting sites for EF1α or cutting sites ApaI and BamHI for PGK and UbC, using a CloneEZ® PCR Cloning Kit (GenScript #L00339) and following the manufacturer’s instructions. The PCR amplification of mCherry, EF1α, PGK and pUb were performed with Phusion® High-Fidelity DNA Polymerase (NEB #M0530S) on pN1-mCherry (Clontech, #632523), pLenti-EF1α (ABMgood #LV588), PGK-DTA-BpA 23 and Ul4-GFP-SIBR 24 plasmids respectively and following the manufacturer’s protocol. Primers used for PCR amplification are listed in Table 1.
Table 1.
Primers used for PCR amplification.
| Primer Name | Sequence | Anneling Temperature |
|---|---|---|
| mCherry NheI Forward | GAGATCGCTAGCGGGCCCGCCACCATGGTGAGCAAGGGCGAGGAG | 60.9 °C |
| mCherry XhoI CMV Reverse | GAGATCCTCGAGCTACTTGTACAGCTCGTCCATG | 60.9 °C |
| Promoter EF1ɑ Forward | TCGGGTTTTTCGAACGGCTCCGGTGCCCGTCAG | 60 °C |
| Promoter EF1ɑ Reverse | ATGGTGGCGGGCCCGTCACGACACCTGAAATGGAAG | 60 °C |
| Promoter PGK/UBC Forward | GATCTCGACGGTATCGAAAGC | 60 °C |
| Promoter PGK Reverse | CCATGGTGGCGGGCCCGAATTCGATCTCGGATCCGAAAGCGAAGGAGCAAAGCTG | 60 °C |
| Promoter UbC Reverse | CCATGGTGGCGGGCCCGAATTCGATCTCGGATCCGTCTAACAAAAAAGCCAAAAAC | 60 °C |
| AP3D1 Forward | GGCATCCGTAACCACAAGGA | 60 °C |
| AP3D1 Reverse | TTGTCCTGCTTCAGCTCCTG | 60 °C |
| CDK4 Forward | GGCTGAAATTGGTGTCGGTG | 60 °C |
| CDK4 Reverse | CACGAACTGTGCTGATGGGA | 60 °C |
| TERT Forward | TGTACTTTGTCAAGGTGGATGTGA | 60 °C |
| TERT Reverse | GCTGGAGGTCTGTCAAGGTAGAG | 60 °C |
2.9. Test of Lentiviral Promoters
Lentiviral production was carried out by CaCl2 transfection of HEK293T cells with 3 plasmids. Transfection was performed with 1 × 106 HEK293T cells using 19.9 µg of constructed lentiviral vector or a pLenti-GIII-EF1α empty (ABMgood #LV588), 5.93 µg of MD2.G plasmid containing VSV-G envelope gene under the control of a CMV promoter (Addgene #12259) and 14.88 µg of psPax2 packaging plasmid containing HIV-gag and HIV-polymerase gene under the control of a CMV promoter (Addgene #12260) over 15 h. The supernatant containing lentivirus was collected 24 and 48 h after the end of transfection, filtered and concentrated using sucrose buffer at low centrifugation as described in [23]. Lentiviral titration was estimated by transfection of HEK293T cells with concentrated lentivirus in DMEM high glucose medium (Gibco #1196044) containing 10% FBS, 100 U/mL penicillin and 100 µg/mL streptomycin and supplemented by 6 µg/mL polybren (Sigma-Aldrich #107689). One day after transfection, cells were selected using growth medium supplemented with 2 µg/mL of puromycin. Multiplicity of infection (MOI) was calculated by counting the remaining cells 3 days after the start of selection. After transduction tests with different MOI ranges from 1 to 10 particles/cell, the more efficient concentration was defined as a MOI of 4 particles/cell. iHMuSCs were seeded at 3000 cells per cm2 with growth medium in 6-well plates. Six hours later, adherent cells were incubated with growth medium supplemented with 6 µg/mL polybren and concentrated lentivirus to a final MOI of 4 lentiviral particles/cell, based on the lentivirus infection efficacy on C2C12 cells (not shown). Medium was replaced by fresh growth medium 36 h later and cells were trypsinated 1 and 5 days later for flow cytometry analysis of the cherry fluorescence using a FACSCantoII flow cytometer. In parallel, cells were cultured on glass coverslips for 1 and 7 days of culture, cells were washed with PBS and fixed with formaldehyde 4% for 10 min at RT. Immunolabeling was carried out using primary rabbit anti-desmin antibodies as described above.
2.10. Quantitative RT-PCR
Total RNAs were extracted from growing iHMuSCs using Trizol (Invitrogen, #15596026) following the manufacturer’s protocol. Controls were 2 non-immortalized primary HMuSCs. Each sample was tested in triplicate. Cultured cells were directly treated with Trizol. One microgram of total RNA was reverse-transcripted using Superscript II Reverse Transcriptase (ThermoFisher #18064022) in 20 µL at 42 °C for 50 min prior to being diluted 10 times. Quality of RNA was checked using Nanodrop. The quantitative RT-PCR were performed using a CFX96 Real-Time PCR Detection System (Bio Rad). The 10 µL final volume of reactive mixture contained 2 µL of diluted cDNA, 0.5 µL of primer mixture, 2.5 µL of water and 5 µL of LightCycler 480 SYBR Green I Master Kit (Invitrogen, Thermofisher Scientific #04707518001). After initial denaturation of 2 min, the amplification was performed with 45 cycles of 95 °C for 10 s, 60 °C for 5 s and 72 °C for 10 s. The calculation of calibrated, normalized relative quantity (CNRQ) was performed using AP3D1 housekeeping gene (there is no variation of expression during myogenesis [24]), with an inter-run calibrator sample. The genes analyzed using quantitative RT-PCR were TERT and CDK4. Primers used for quantitative PCR are listed in Table 1.
3. Results and Discussion
3.1. Immortalized Myogenic Cell Lines Generated from Duchenne Muscular Dystrophy, Congenital Muscular Dystrophies and Control Muscles
We identified 8 DMD patients and 4 patients suffering from congenital muscular dystrophies (CMD) for which genetics and clinic characteristics have been established and 3 age-matched controls with normal muscle histology (Table 2). CMD included mutations in collagen VI, Lamin A/C, Laminin alpha-2 genes and an unknown cause. The genetic causes of DMD for the 8 patients are indicated in Table 2. Data collected for the donors included creatine kinase (CK) level at the time of biopsy collection, age at first walking, the presence or absence of cardiomyopathy and scoliosis and whether patients underwent scoliosis surgery (Table 2).
Table 2.
Clinical data of patients.
| Patient | Sex (M/F) | Age at the Time of Biopsy (m) | Diagnosis | Genetic Results | CK Blood Level at Diagnosis (IU/L) | Age at First Walking (m) | Cardiomyopathy Age at Onset (m) | ScoliosisAge at Onset (m) | Scoliosis Surgery/Age at Surgery |
|---|---|---|---|---|---|---|---|---|---|
| Control 1 | M | 41 | control | / | nl | 24 | N | N | N |
| Control 2 | M | 14 | control | / | nl | 24 | N | N | N |
| Control 3 | M | 19 | control | / | nl | 18 | N | N | N |
| CMD 1 | M | 144 | Collagen VI related myopathy | C6210 + 5G > A | nd | 72 | N | Y | Y/145 |
| CMD 2 | F | 144 | CMD | genetic unknown causes | nl | 18 | N | Y/195 | Y/231 |
| CMD 3 | F | 39 | Laminopathy LMNA | c.94–96 deletion; p.lys32 deletion | 860 | never walking | N | N | N |
| CMD 4 | F | 12 | LAMA2 related myopathy | c.1553 deletion GTT; pCys518 deletion and c.2866 deletion T | 14400 | never walking | N | N | N |
| DMD 1 | M | 54 | DMD | c.3–26 duplication | 18000 | 24 | N | N | N |
| DMD 2 | M | 87 | DMD | c.8–43 deletion | nd | 13 | Y/109 | Y/141 | Y/148 |
| DMD 3 | M | 97 | DMD | c.433 C > T substitution (p.R145X) | 12881 | 15 | N | Y/161 | Y/161 |
| DMD 4 | M | 25 | DMD | c.8562 deletion A; p.Glu2854Asp fs X2 | 19000 | 24 | N | N | N |
| DMD 5 | M | 79 | DMD | c.5758 C > T substitution; p.Gln1920X | 8041 | 15 | N | N | N |
| DMD 6 | M | nd | DMD | Exon skipping 19 / IVS 19 +1 G > C/c.2380 + 1 G >C | nd | nd | Y/82 | N | N |
| DMD 7 | M | 89 | DMD | c.50–59 dup | 47270 | 15 | N | N | N |
| DMD 8 | M | nd | DMD | nd | nd | nd | nd | nd | nd |
CMD, congenital muscular dystrophy; DMD, Duchenne muscular dystrophy; M, male; F, female; CK, creatin kinase; IU/L, international unit per liter; nl, normal; Y, yes; N, no; m, month; nd, non-determined.
MuSCs were isolated as CD56pos cells from the 15 patients, expanded, infected with lentiviruses expressing CDK4 and HTERT and selected using puromycin as previously described [20]. CDK4 overexpression blocks the p16INK4a-Rb pathway while hTERT maintains telomere length, allowing MuSC immortalization [17,20,22]. The bulk cell populations were first selected using puromycine, removing cells lacking the HTERT transgene. Then, cells were expanded, in order to deplete cells lacking the CDK4 transgene [13].
Infection of myoblasts with lentiviruses is expected to have generated cells that integrate variable copy numbers of the transgenes into different genomic loci. This is likely to cause high intercellular variability and heterogeneous cell populations. To select clones presenting a homogeneous phenotype and genotype, we carried out FACS single cell sorting of CD56pos immortalized cells and amplified these clonal cultures, referred to as iHMuSCs for immortalized human muscle stem cells. These clones were then analyzed for their expansion capacity, myogenic nature and myogenic differentiation potential.
3.2. Selection of iHMuSCs Exhibiting Efficient Growth Capacity
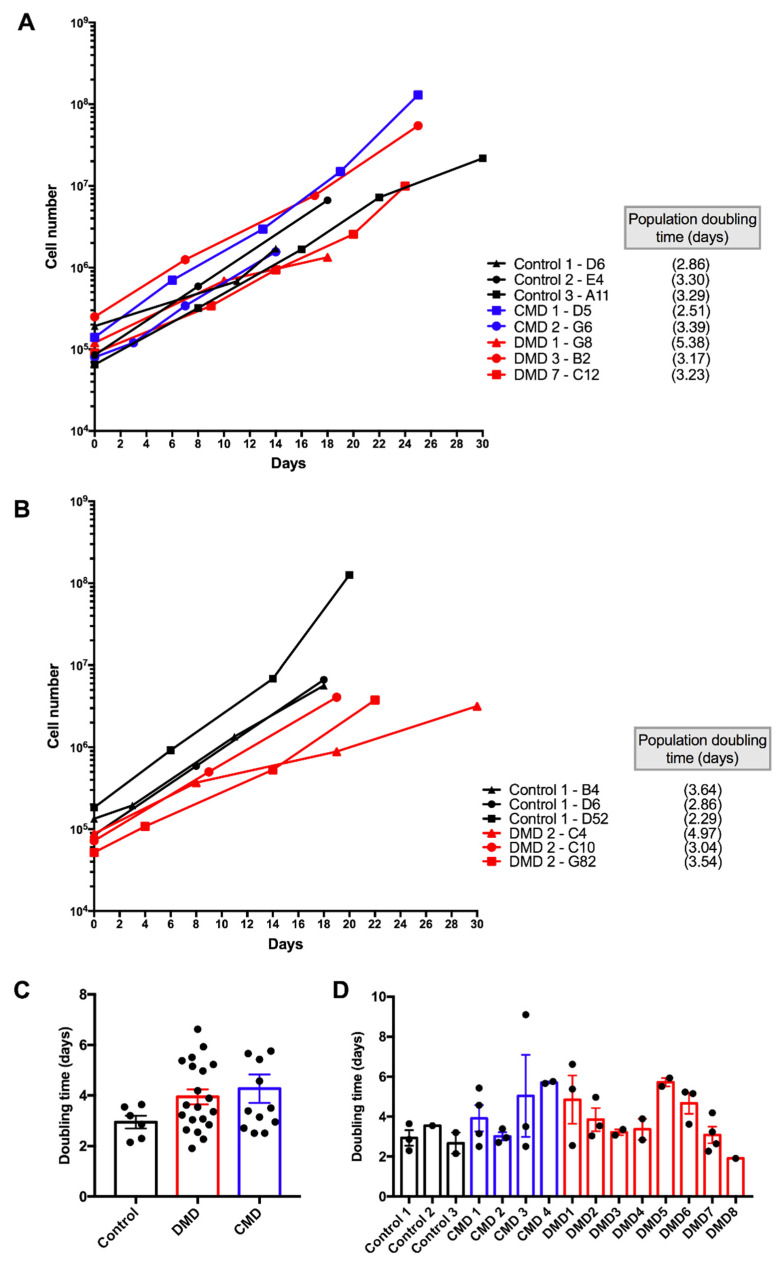
Expanding clones were first tested for their capacity to proliferate. Basically, two types of clones were observed: clones that were not capable of expansion after a few weeks, and that were discarded from further analyses, and clones that expanded efficiently and were selected. Figure 1A shows examples of clones that replicated rapidly from the time of seeding, exhibited a regular growth and showed population doubling times ranging from 2.5 to 5.4 days in growing conditions. While some variability in population doubling time was observed, no significant difference was identified when considering the pathology, i.e., controls versus DMD versus CMD (Figure 1A,C). Moreover, variability in population doubling time was observed between clones issued from the same patient, as exemplified for two patients in Figure 1B. Distribution of the population doubling time for all the selected clones is shown in Figure 1D. Therefore, the proliferative capacity was characteristic of each clone and may be related to the sites of insertion of CDK4 and HTERT genes in the genome. Thus, several clones were generated from each patient in order to allow future investigators to work on several clones from the same patient to avoid potential bias induced by the site of insertion of the lentiviral-driven genes.
Figure 1.
Growth curve of immortalized human muscle stem cell (iHMuSC) clones. IHMuSC clones were expanded in growing medium. (A) Growth of eight clones from eight different patients. (B) Growth of three different clones from the same patient (one control and one DMD patient are shown). (C) Population doubling time of control, DMD (Duchenne Muscular Dystrophy) and CMD (Congenital Muscular Dystrophy) derived iHMuSCs. (D) Comparison of population doubling time from each donor (clones from the same donor are gathered in one bar). Statistical analyses were done using one-way ANOVA.
Both control and DMD iHMuSC clones were selected for their efficient growth. The proliferation capacity of MuSCs in DMD has been a matter of debate. Earlier works reported a defect in both proliferation and differentiation of the DMD myoblasts [25,26,27,28] and others not [29], but at that time there was no method of purification of cell cultures, which contained non-myogenic cells. Later, it was shown that pure myogenic stem cells from human DMD muscle do not show alteration in their proliferative capacity as compared with cells issued from healthy muscle [20,30].
3.3. Myogenic Nature of iHMuSCs
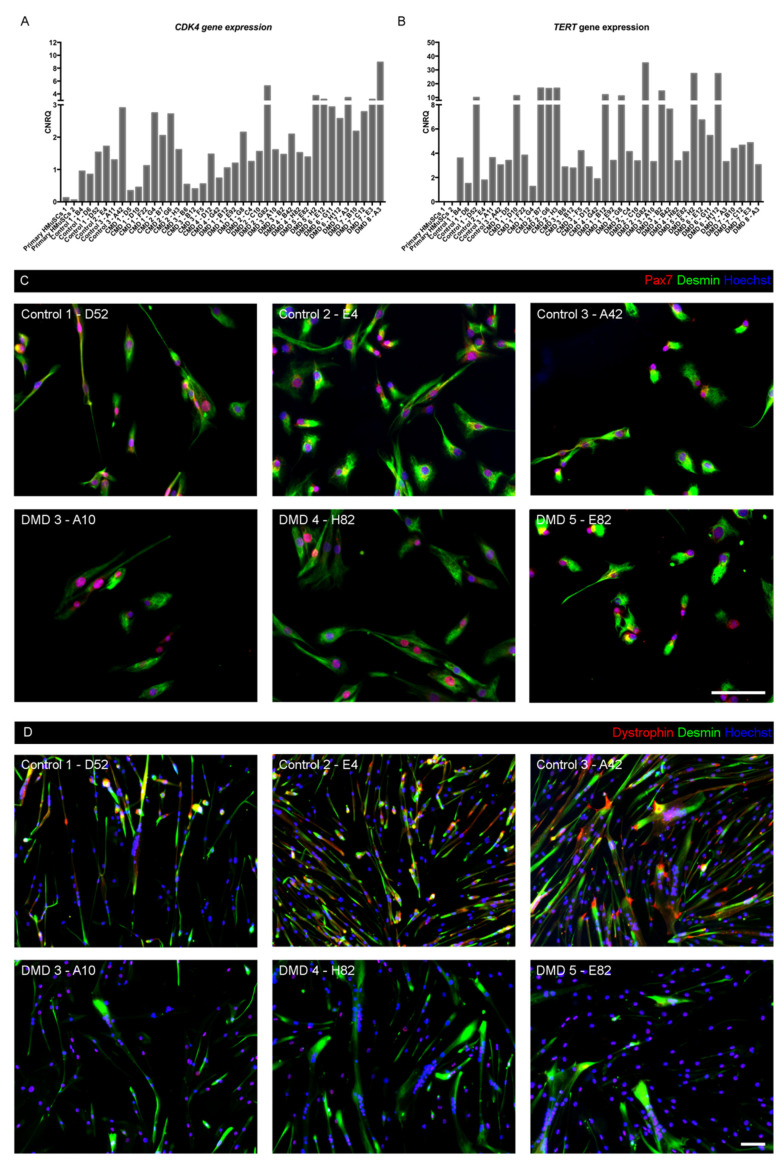
We confirmed that CDK4 and TERT transduction was efficient, through RT-qPCR of CDK4 and TERT genes in growing iHMuSCs, as compared with primary HMuSCs. The latter, issued from two healthy donors, exhibited a very low and no expression of CDK4 and TERT genes, respectively. In iHMuSCs, CDK4 expression was 3 to 35 fold higher and the expression of hTERT was triggered (minimum 1300 fold) (Figure 2A,B), confirming that the clonal cultures expanded from transduced cells.
Figure 2.
Myogenic nature of iHMuSC clones. (A,B) Primary HMuSCs and iHMuSC clones were tested for CDK4 (A) and TERT (B) gene expression using RT-qPCR. (C) Immunostaining for the myogenic markers Pax7 (Red) and desmin (green) in growing iHMuSC clones. (D) Immunostaining desmin (green) and dystrophin (red) in differentiated iHMuSC clones. Nuclei are labelled with Hoechst (blue). Bars = 100 µm.
The myogenic nature of iHMuSCs was investigated via Pax7 and desmin immunostaining on three healthy and three DMD growing iHMuSC clones issued from various donors (Figure 2C). In all six clones tested, 100% of iHMuSCs expressed both desmin and Pax7 protein, confirming that they were myogenic cells. Moreover, all 38 clones stemmed from CD56 expressing cells and then were further tested after expansion for their expression of CD56, which is a canonical marker of MuSCs in human, where cells that express CD56 invariably express Pax7 [31,32]. Additionally, we investigated the expression of dystrophin in differentiated iHMuSC clones, since in mouse, dystrophin expression is reported to be specific of satellite cells and differentiated myoblasts, but absent from growing myoblasts [33]. As expected in iHMuSCs derived from control MuSCs, differentiated myotubes expressed both the cytoplasmic and nuclear isoforms of dystrophin [34], using an antibody targeting all five isoforms (epitope between exons 77 to 79) (Figure 2D). Inversely, DMD-derived iHMuSCs displayed only the nuclear isoforms (Figure 2D), confirming the lack of muscle specific Dp427m dystrophin expression.
3.4. Selection of iHMuSCs Exhibiting Efficient Myogenic Differentiation
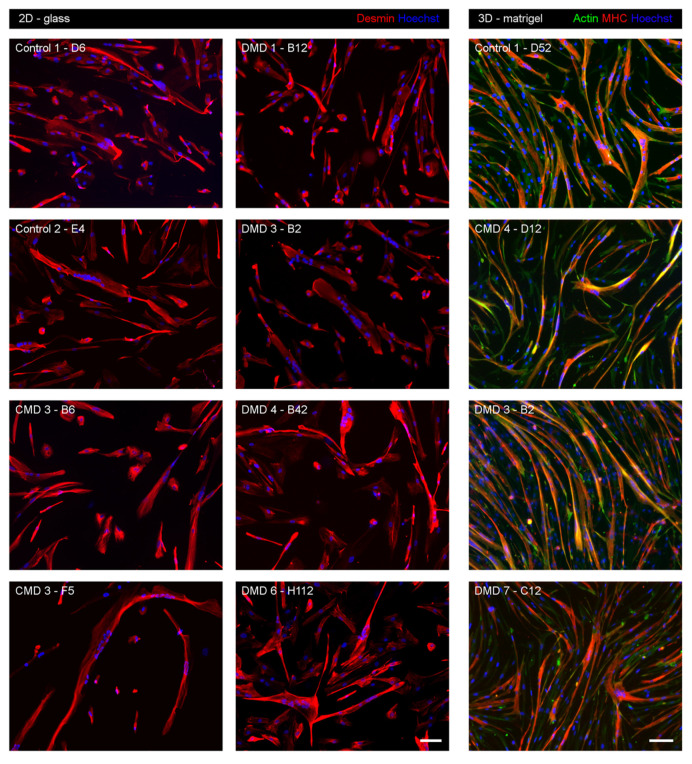
The above selected growing clones were further checked for their ability to sustain high-level expression of CD56, a specific marker of human myogenic cells [6,31,35,36]. Only clones exhibiting CD56 expression in more than 90% of the cells were retained. Previous studies showed that in bulk transduced cultures, CDK4 and HTERT overexpression triggers MuSC immortalization without interfering with their myogenicity [14,37]. We implemented a complete analysis of the differentiation capacities of each of the selected clones. Myogenic differentiation was classically triggered by culturing iHMuSCs in differentiation medium, containing low mitogen concentration and supplemented by insulin and transferrin. Myogenic differentiation capacity of the cells was assessed using immunofluorescence using desmin staining to visualize the formation of multinucleated myotubes. The formation of myotubes was estimated in a semi-quantitative manner to exclude clones showing no or poor ability to differentiate. Figure 3 (2D-glass) shows examples of iHMuSCs forming myotubes on a 2D glass culture support. We also performed a 3D culture that improves myogenic differentiation, by culturing the cells between two thin layers of Matrigel, which is a mixture of matrix proteins constitutive of basal lamina that promotes muscle cell growth and differentiation [38]. Figure 3 (3D-matrigel) shows that iHMuSCs from either control, CMD or DMD patients formed large elongated myotubes containing numerous nuclei and having developed their contractile apparatus, as assessed by MHC expression.
Figure 3.
Myogenic differentiation of iHMuSC clones. Clones selected for their good growth capacity were tested for their myogenic differentiation capacity. In the 2D glass condition (left and middle panels), clones were differentiated on glass culture supports for 5 days before the detection of desmin (red) using immunofluorescence. In the 3D-Matrigel condition (right panel), clones were differentiated between 2 thin Matrigel coats for 5 days before the detection of actin (green) and MHC (red) using immunofluorescence. Nuclei are labelled with Hoechst (blue). Bars = 100 µm.
In total, the selection process provided 38 iHMuSC clones exhibiting efficient proliferative capacity, sustained CD56 expression and showing excellent capacities for myogenic differentiation, available for 15 genetically and clinically characterized patients (Table 3).
Table 3.
Summary of characterized immortalized human myogenic stem cell clones.
| Patients | Clones | Population Doublings a | CD56 pos Cells (%) | Differentiation | Doubling Time (days) b |
|---|---|---|---|---|---|
| Control 1 | B4 | 3.33 | 99.50 | ++ | 3.64 |
| D6 | 2.80 | 99.80 | +++ | 2.86 | |
| D52 long term |
5.22 | 99.70 | +++ | 2.3 | |
| 73.23 | 99.90 | ++ | |||
| Control 2 | E4 | 4.69 | 99.40 | ++ | 3.55 |
| Control 3 | A11 | 1.82 | 98.07 | ++ | 3.2 |
| A42 long term |
3.87 | 98.20 | ++ | 2.15 | |
| 73.83 | 99.90 | +++ | |||
| CMD 1 | D5 | 6.50 | 99.00 | +++ | 2.51 |
| D10 | 8.73 | 98.90 | ++ | 5.43 | |
| F22 long term |
4.53 | 98.50 | +++ | 3.15 | |
| 69.86 | 99.80 | +++ | |||
| G4 | 5.15 | 98.91 | +++ | 4.57 | |
| CMD 2 | B7 | 4.74 | 99.80 | +++ | 2.95 |
| G6 | 4.29 | 99.80 | +++ | 3.39 | |
| H3 | 5.80 | 99.70 | +++ | 2.71 | |
| CMD 3 | B6 | 4.42 | 96.00 | ++ | 3.5 |
| B12 | 2.00 | 97.30 | +++ | 2.51 | |
| F5 | 1.96 | 90.00 | +++ | 9.1 | |
| CMD 4 | D12 | 5.40 | 93.30 | +++ | 5.76 |
| G42 | 2.51 | 91.00 | +++ | 5.66 | |
| DMD 1 | B12 long term |
5.17 | 99.00 | ++ | 2.55 |
| 66.39 | 93.40 | ++ | |||
| E92 | 3.39 | 99.00 | ++ | 6.62 | |
| G8 | 3.48 | 97.20 | +++ | 5.38 | |
| DMD 2 | C4 | 2.07 | 86.00 | +++ | 4.97 |
| C10 | 5.82 | 93.10 | ++ | 3.04 | |
| G82 | 6.18 | 98.50 | ++ | 3.54 | |
| aDMD 3 | A10 long term |
3.90 | 99.30 | ++ | 3.36 |
| 42.39 | 95.10 | + | |||
| B2 | 7.77 | 89.00 | +++ | 3.07 | |
| DMD 4 | B42 | 3.61 | 98.10 | ++ | 3.89 |
| H82 long term |
5.39 | 99.80 | ++ | 2.84 | |
| 52.30 | nd | +++ | |||
| DMD 5 | E82 | 4.32 | 98.00 | ++ | 5.93 |
| H2 | 2.56 | 100.00 | ++ | 5.51 | |
| DMD 6 | E12 | 2.65 | 96.70 | +++ | 3.62 |
| G11 | 6.45 | 93.20 | +++ | 5.23 | |
| H112 | 3.39 | 91.70 | ++ | 5.15 | |
| DMD 7 | A3 | 5.80 | 93.70 | +++ | 2.64 |
| B10 | 8.40 | 98.00 | +++ | 4.19 | |
| C12 | 6.80 | 99.30 | +++ | 3.23 | |
| E3 long term |
15.96 | 99.00 | ++ | 2.27 | |
| 119.30 | 82.90 | nd | |||
| DMD 8 | A3 long term |
5.72 | 99.20 | ++ | 1.91 |
| 63.55 | 98.00 | nd |
In italic, long term culture; +, poor fusion; ++, small myotubes; +++, large myotubes; nd, non-determined. a Population doubling of the culture at the time of analysis of CD56 expression and of differentiation. b Doubling time along the culture from the initial seeding until the indicated population doubling.
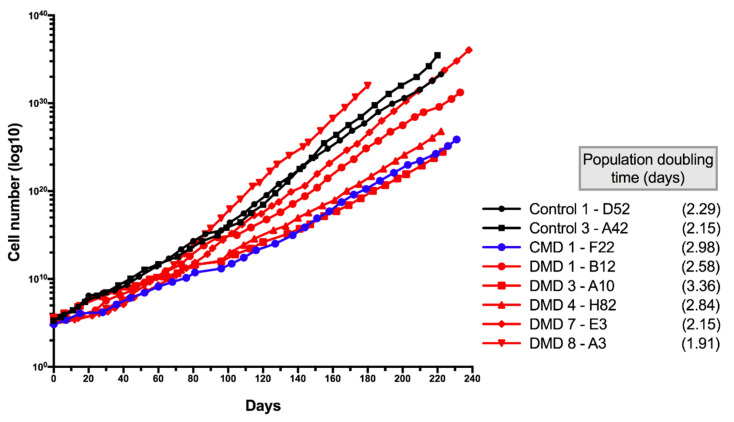
3.5. Characteristics of Long-Term Cultured iHMuSCs
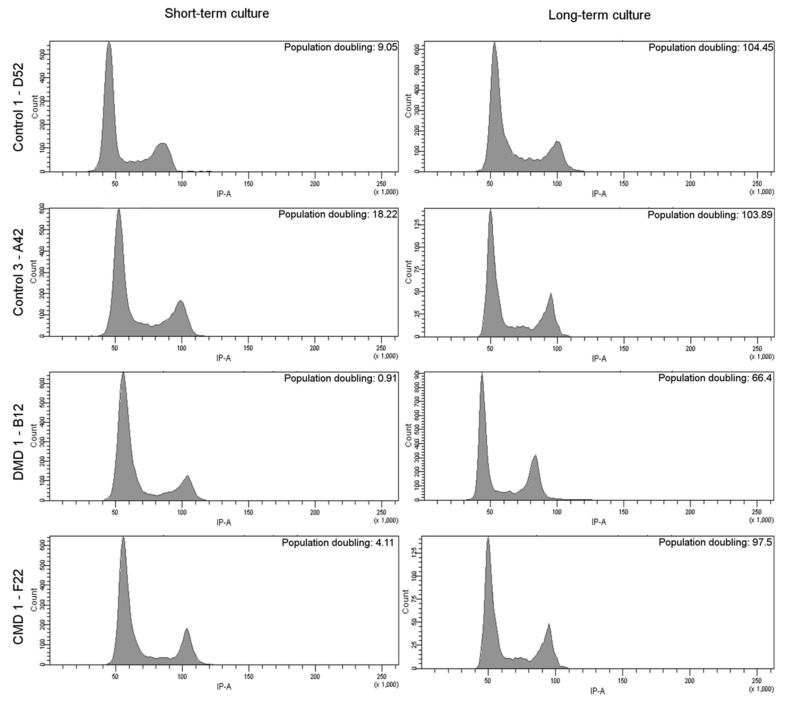
Eight clones were tested for long-term culture, up to 240 days. For all clones, regular growth was observed over time, allowing cells to perform between 60–100 population doublings after 240 days (Figure 4). CD56pos expression was maintained at a high level since all but one clone showed greater than 93% of the cell expressing the myogenic membrane protein over long-term cultures (with clone DMD7-E3 showing 82.9% of CD56pos cells) (Table 3). As for younger cultures, high CD56 expression was associated with the capacity to differentiate and to form myotubes in all clones tested but one (Table 3). It was previously shown that SV40 large T gene overexpression leads to abnormal chromosomic recombination in myoblasts and to an impaired expression of the myogenic program [8,9,10]. To estimate potential major changes in chromosomic recombination and in cell cycle, we performed cell cycle analysis using FACS with propidium iodide. Four clones were tested at early and old population doublings. Figure 5 shows that all clones presented a normal cell cycle profile during short-term cultures (left panel) that was maintained in long-term cultures (right panel). No mark of polyploidy was observed. We thus assumed that no major chromosomal abnormalities appeared in iHMuSCs, although one has to keep in mind that mutations and short chromosomal modifications may occur in cells kept for a long time in culture.
Figure 4.
Long-term culture of iHMuSC clones. Eight clones from eight patients were cultured up to 240 days.
Figure 5.
Cell cycle analysis of short-term and long-term cultured iHMuSC clones. Four randomly chosen clones were tested for cell cycle analysis at short- (left panel) and long- (right panel) term culture. Flow cytometer analysis of propidium iodide staining is shown, reflecting the amount of DNA in the cells.
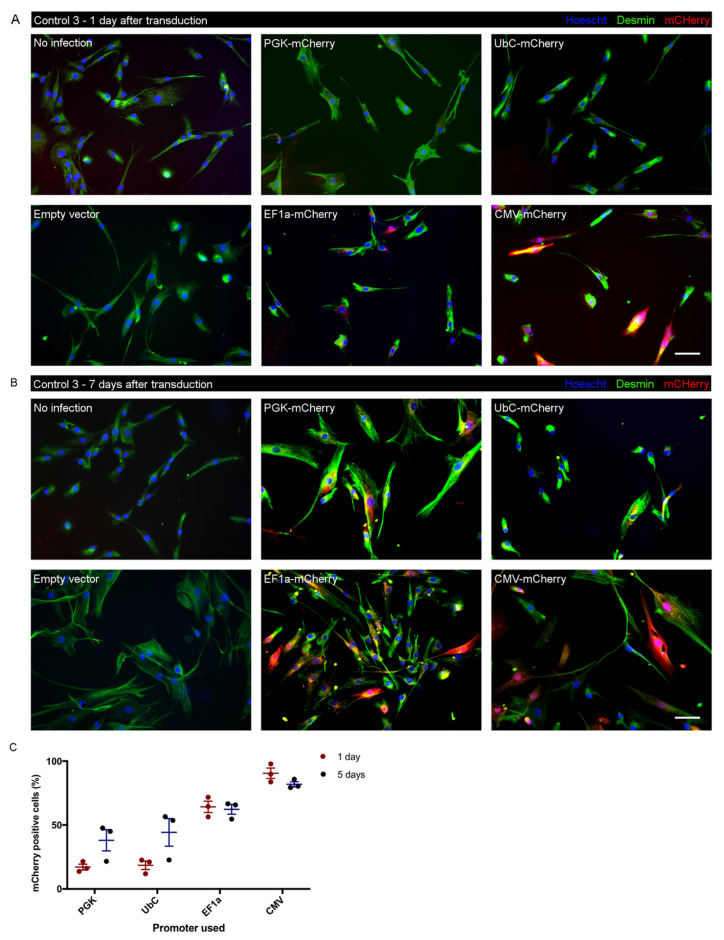
3.6. Test of Promoter Activity for Lentiviral Transduction in iHMuSCs
A potential application of iHMuSCs is gene overexpression or silencing by gene editing. To maintain either stable gene overexpression or a stable genome edition, it is necessary to carry out a lentiviral infection [39]. However, promoters may have various transcriptional efficiency depending on the cell type [40]. In order to identify promoters that are efficient for further stable gene expression in iHMuSCs, we performed lentiviral transduction with vectors expressing the mCherry reporter gene under the control of various promoters in control iHMuSCS, here considered a cell type. We tested human cytomegalovirus promoter (CMV), human elongation factor 1α promoter (EF1α), phosphoglycerate kinase promoter (PGK) and ubiquitin C promoter (UbC). Figure 6A shows that PGK and UbC promoters triggered very low level expression of mCherry in iHMuSCs, a result confirmed using flow cytometry (17.1 and 38.1% of positive cells for PGK and 18.5 and 44.3% of positive cells for UbC, at 1 and 5 days after transfection, respectively) (Figure 6C). CMV and EF1α were the most active promoters since 90.4 and 64.2% of cells were positive for mCherry expression 24 h after transduction (Figure 6A,C). However, at 5 days, the number of positive cells had declined by 10% when the promoter was driven by the CMV promoter (Figure 6C), such a decrease over time being reported in other models [41,42]. Inversely, almost no decrease (2.9%) was observed using EF1α promoter to drive mCherry expression after 5 days and an increase was noticed for PGK and UbC (21 and 26.2%, respectively) (Figure 6B,C). Thus, to alter gene expression in iHMuSCs, the CMV and EF1α promoters induced fast and strong expression of the transgene, while the PGK and UbC promoters ensured a later expression. CMV or EF1α should be preferred to obtain fast and stable expression of a transgene. In both cases, cell selection is recommended to work with cell populations expressing the transgene homogeneously in order to maintain a stable expression.
Figure 6.
Lentiviral transduction of mCherry reporter gene under the control of several promoters. iHMuSCs control 1—D52, control 2—E4 and control 3—A42 were transduced with lentiviruses containing mCherry under the control of PGK, UbC, EF1 or CMV promoters or with an empty lentivirus. (A,B) Immunostaining was performed 1 (A) and 7 (B) days after transduction for the detection of desmin (green). mCherry is red. Nuclei are labelled with Hoechst (blue). Bars = 100 µm. (C) Quantification of the expression of mCherry in iHMuSCs using flow cytometry 1 and 5 days after the lentiviral transduction. Results are given in percentage of mCherry positive cells and were done on the 3 different clones: control 1—D52, control 2—E4 and control 3—A42 (means ± SEM).
4. Conclusions
In the present study, we used the well-characterized immortalization procedure of primary human MuSCs [19,20], and we performed single cell-derived cultures to establish clones that present homogeneous genetics and cell behavior. This study provides the description of 38 clones of iHMuSCs coming from 12 patients, and including 6 clones from 3 control muscles, 12 clones from 4 CMD patients and 20 clones for 8 DMD patients, who exhibited a large variety of genetic defects. Each patient was genetically and clinically characterized, and each clone was validated for its myogenic nature (Pax7 and desmin expression), proliferative capacity, maintenance of CD56 expression and ability to differentiate/fuse. These clones provide a useful material for investigation of different aspects of DMD biology such as metabolism, gene expression, chromatin organization and membrane changes or for screening of therapeutic strategies in complement with the known animal models. The information for each patient allows choice of the clones depending on clinical features, and patient genotyping will be essential for the design of exon skipping strategies such as the recent experiments using CRISPR-Cas9ti edit the DMD gene [43,44]. Moreover, working with several clones from the same patients avoids bias due to the insertion sites of the immortalization genes. Although providing an unique material for the investigation of molecular alterations in DMD, one has to keep in mind that iHMuSCs have a slightly modified genome caused by the insertion of CDK4 and HTERT genes that may induce off-target changes depending on the insertion sites of the transgenes. Thus, it is recommended that several clones from the same parental transduced culture be used in a given experimental setup to exclude any effect due to the site of insertion of the transgenes or clone specificities.
Here, iHMuSCs were produced from DMD patients carrying eight different genetic alterations allowing the investigation of DMD mechanisms independently of—or dependent upon—a specific mutation. Similarly, iHMuSCs were produced from CMD patients of various origins allowing investigation of dystrophic cells unrelated to dystrophin loss. The 38 iHMuSCs clones will be a valuable resource for the academic scientific community and will be made available through signed material transfer agreements.
Acknowledgments
We warmly thank Jamel Chelly who made it possible to start this study in his research laboratory and his service at Hôpital Cochin and we thank Sylvie Fabrega and the Viral Vectors and Gene Transfer facility at Université René Descartes, Paris, for the hTERT and CDK4 lentiviral production.
Author Contributions
J.M.: collection and/or assembly of data, data analysis and interpretation, manuscript writing, final approval of manuscript. C.G.: provision of study material or patients, manuscript writing, final approval of manuscript. M.M.: collection and/or assembly of data, data analysis and interpretation, final approval of manuscript. S.C.: collection and/or assembly of data, data analysis and interpretation, final approval of manuscript. A.H.: provision of study material or patients, collection and/or assembly of data, final approval of manuscript. P.N.: provision of study material or patients, collection and/or assembly of data, final approval of manuscript. F.J.D.: conception and design, data analysis and interpretation, manuscript writing, final approval of manuscript. I.D.: conception and design, provision of study material or patients, final approval of manuscript. B.C.: conception and design, financial support, data analysis and interpretation, manuscript writing, final approval of manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by CNRS, Université Paris Descartes, Université Claude Bernard Lyon 1, CNRS, INSERM, and by EU FP7 Endostem (no. 241440).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Mendell J.R., Lloyd-Puryear M. Report of MDA muscle disease symposium on newborn screening for Duchenne muscular dystrophy: Issues & Opinions: Newborn Screening for DMD. Muscle Nerve. 2013;48:21–26. doi: 10.1002/mus.23810. [DOI] [PubMed] [Google Scholar]
- 2.Desguerre I., Mayer M., Leturcq F., Barbet J.-P., Gherardi R.K., Christov C. Endomysial Fibrosis in Duchenne Muscular Dystrophy: A Marker of Poor Outcome Associated With Macrophage Alternative Activation. J. Neuropathol. Exp. Neurol. 2009;68:762–773. doi: 10.1097/NEN.0b013e3181aa31c2. [DOI] [PubMed] [Google Scholar]
- 3.Deconinck A.E., Rafael J.A., Skinner J.A., Brown S.C., Potter A.C., Metzinger L., Watt D.J., Dickson J.G., Tinsley J.M., Davies K.E. Utrophin-Dystrophin-Deficient Mice as a Model for Duchenne Muscular Dystrophy. Cell. 1997;90:717–727. doi: 10.1016/S0092-8674(00)80532-2. [DOI] [PubMed] [Google Scholar]
- 4.Sacco A., Mourkioti F., Tran R., Choi J., Llewellyn M., Kraft P., Shkreli M., Delp S., Pomerantz J.H., Artandi S.E., et al. Short Telomeres and Stem Cell Exhaustion Model Duchenne Muscular Dystrophy in mdx/mTR Mice. Cell. 2010;143:1059–1071. doi: 10.1016/j.cell.2010.11.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alsharidah M., Lazarus N.R., George T.E., Agley C.C., Velloso C.P., Harridge S.D.R. Primary human muscle precursor cells obtained from young and old donors produce similar proliferative, differentiation and senescent profiles in culture. Aging Cell. 2013;12:333–344. doi: 10.1111/acel.12051. [DOI] [PubMed] [Google Scholar]
- 6.Illa I., Leon-Monzon M., Dalakas M.C. Regenerating and denervated human muscle fibers and satellite cells express neural cell adhesion molecule recognized by monoclonal antibodies to natural killer cells. Ann. Neurol. 1992;31:46–52. doi: 10.1002/ana.410310109. [DOI] [PubMed] [Google Scholar]
- 7.Renault V., Thornell L.-E., Eriksson P.-O., Butler-Browne G., Mouly V., Thorne L.-E. Regenerative potential of human skeletal muscle during aging. Aging Cell. 2002;1:132–139. doi: 10.1046/j.1474-9728.2002.00017.x. [DOI] [PubMed] [Google Scholar]
- 8.Simon L.V., Beauchamp J.R., O’Hare M., Olsen I. Establishment of Long-Term Myogenic Cultures from Patients with Duchenne Muscular Dystrophy by Retroviral Transduction of a Temperature-Sensitive SV40 Large T Antigen. Exp. Cell Res. 1996;224:264–271. doi: 10.1006/excr.1996.0136. [DOI] [PubMed] [Google Scholar]
- 9.Cudré-Mauroux C., Occhiodoro T., König S., Salmon P., Bernheim L., Trono D. Lentivector-Mediated Transfer of Bmi-1 and Telomerase in Muscle Satellite Cells Yields a Duchenne Myoblast Cell Line with Long-Term Genotypic and Phenotypic Stability. Hum. Gene Ther. 2003;14:1525–1533. doi: 10.1089/104303403322495034. [DOI] [PubMed] [Google Scholar]
- 10.Mouly V., Edom F., Decary S., Vicart P., Barbert J.P., Butler-Browne G.S. SV40 large T antigen interferes with adult myosin heavy chain expression, but not with differentiation of human satellite cells. Exp. Cell Res. 1996;225:268–276. doi: 10.1006/excr.1996.0176. [DOI] [PubMed] [Google Scholar]
- 11.Decary S., Mouly V., Butler-Browne G.S. Telomere length as a tool to monitor satellite cell amplification for cell-mediated gene therapy. Hum. Gene Ther. 1996;7:1347–1350. doi: 10.1089/hum.1996.7.11-1347. [DOI] [PubMed] [Google Scholar]
- 12.Halvorsen T.L., Leibowitz G., Levine F. Telomerase activity is sufficient to allow transformed cells to escape from crisis. Mol. Cell. Biol. 1999;19:1864–1870. doi: 10.1128/MCB.19.3.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seigneurin-Venin S., Bernard V., Tremblay J.P. Telomerase allows the immortalization of T antigen-positive DMD myoblasts: a new source of cells for gene transfer application. Gene Ther. 2000;7:619–623. doi: 10.1038/sj.gt.3301132. [DOI] [PubMed] [Google Scholar]
- 14.Shiomi K., Kiyono T., Okamura K., Uezumi M., Goto Y., Yasumoto S., Shimizu S., Hashimoto N. CDK4 and cyclin D1 allow human myogenic cells to recapture growth property without compromising differentiation potential. Gene Ther. 2011;18:857–866. doi: 10.1038/gt.2011.44. [DOI] [PubMed] [Google Scholar]
- 15.Stadler G., Chen J.C., Wagner K., Robin J.D., Shay J.W., Emerson Jr C.P., Wright W.E. Establishment of clonal myogenic cell lines from severely affected dystrophic muscles - CDK4 maintains the myogenic population. Skeletal Muscle. 2011;1:12. doi: 10.1186/2044-5040-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu C.-H., Mouly V., Cooper R.N., Mamchaoui K., Bigot A., Shay J.W., Di Santo J.P., Butler-Browne G.S., Wright W.E. Cellular senescence in human myoblasts is overcome by human telomerase reverse transcriptase and cyclin-dependent kinase 4: consequences in aging muscle and therapeutic strategies for muscular dystrophies. Aging Cell. 2007;6:515–523. doi: 10.1111/j.1474-9726.2007.00306.x. [DOI] [PubMed] [Google Scholar]
- 17.Donai K., Kiyono T., Eitsuka T., Guo Y., Kuroda K., Sone H., Isogai E., Fukuda T. Bovine and porcine fibroblasts can be immortalized with intact karyotype by the expression of mutant cyclin dependent kinase 4, cyclin D, and telomerase. J. Biotechnol. 2014;176:50–57. doi: 10.1016/j.jbiotec.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 18.Pantic B., Borgia D., Giunco S., Malena A., Kiyono T., Salvatori S., De Rossi A., Giardina E., Sangiuolo F., Pegoraro E., et al. Reliable and versatile immortal muscle cell models from healthy and myotonic dystrophy type 1 primary human myoblasts. Exp. Cell Res. 2016;342:39–51. doi: 10.1016/j.yexcr.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Thorley M., Duguez S., Mazza E.M.C., Valsoni S., Bigot A., Mamchaoui K., Harmon B., Voit T., Mouly V., Duddy W. Skeletal muscle characteristics are preserved in hTERT/cdk4 human myogenic cell lines. Skeletal Muscle. 2016;6:43. doi: 10.1186/s13395-016-0115-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mamchaoui K., Trollet C., Bigot A., Negroni E., Chaouch S., Wolff A., Kandalla P.K., Marie S., Di Santo J., St Guily J., et al. Immortalized pathological human myoblasts: towards a universal tool for the study of neuromuscular disorders. Skeletal Muscle. 2011;1:34. doi: 10.1186/2044-5040-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoon S., Stadler G., Beermann M., Schmidt E.V., Windelborn J.A., Schneiderat P., Wright W.E., Miller J. Immortalized myogenic cells from congenital muscular dystrophy type1A patients recapitulate aberrant caspase activation in pathogenesis: a new tool for MDC1A research. Skeletal Muscle. 2013;3:28. doi: 10.1186/2044-5040-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krom Y.D., Dumonceaux J., Mamchaoui K., den Hamer B., Mariot V., Negroni E., Geng L.N., Martin N., Tawil R., Tapscott S.J., et al. Generation of Isogenic D4Z4 Contracted and Noncontracted Immortal Muscle Cell Clones from a Mosaic Patient. Am. J. Pathol. 2012;181:1387–1401. doi: 10.1016/j.ajpath.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jiang W., Hua R., Wei M., Li C., Qiu Z., Yang X., Zhang C. An optimized method for high-titer lentivirus preparations without ultracentrifugation. Sci. Rep. 2015;5:13875. doi: 10.1038/srep13875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hildyard J.C.W., Wells D.J. Identification and Validation of Quantitative PCR Reference Genes Suitable for Normalizing Expression in Normal and Dystrophic Cell Culture Models of Myogenesis. PLoS Curr. 2014 doi: 10.1371/currents.md.faafdde4bea8df4aa7d06cd5553119a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blau H.M., Webster C., Pavlath G.K. Defective myoblasts identified in Duchenne muscular dystrophy. Proc. Nat. Acad. Sci. 1983;80:4856–4860. doi: 10.1073/pnas.80.15.4856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jasmin G., Tautu C., Vanasse M., Brochu P., Simoneau R. Impaired muscle differentiation in explant cultures of Duchenne muscular dystrophy. Lab. Invest. 1984;50:197–207. [PubMed] [Google Scholar]
- 27.Delaporte C., Dehaupas M., Fardeau M. Comparison between the growth pattern of cell cultures from normal and Duchenne dystrophy muscle. J. Neurol. Sci. 1984;64:149–160. doi: 10.1016/0022-510X(84)90033-9. [DOI] [PubMed] [Google Scholar]
- 28.Iannaccone S.T., Nagy B., Samaha F.J. Decreased Creatine Kinase Activity in Cultured Duchenne Dystrophic Muscle Cells. J. Child Neurol. 1987;2:17–21. doi: 10.1177/088307388700200103. [DOI] [PubMed] [Google Scholar]
- 29.Blau H. Differentiation properties of pure populations of human dystrophic muscle cells. Exp. Cell Res. 1983;144:495–503. doi: 10.1016/0014-4827(83)90431-7. [DOI] [PubMed] [Google Scholar]
- 30.Zanotti S., Saredi S., Ruggieri A., Fabbri M., Blasevich F., Romaggi S., Morandi L., Mora M. Altered extracellular matrix transcript expression and protein modulation in primary Duchenne muscular dystrophy myotubes. Matrix Biol. 2007;26:615–624. doi: 10.1016/j.matbio.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Xu X., Wilschut K.J., Kouklis G., Tian H., Hesse R., Garland C., Sbitany H., Hansen S., Seth R., Knott P.D., et al. Human Satellite Cell Transplantation and Regeneration from Diverse Skeletal Muscles. Stem Cell Rep. 2015;5:419–434. doi: 10.1016/j.stemcr.2015.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barruet E., Garcia S.M., Striedinger K., Wu J., Lee S., Byrnes L., Wong A., Xuefeng S., Tamaki S., Brack A.S., et al. Functionally heterogeneous human satellite cells identified by single cell RNA sequencing. Elife. 2020;9:e51576. doi: 10.7554/eLife.51576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dumont N.A., Wang Y.X., von Maltzahn J., Pasut A., Bentzinger C.F., Brun C.E., Rudnicki M.A. Dystrophin expression in muscle stem cells regulates their polarity and asymmetric division. Nat. Med. 2015;21:1455–1463. doi: 10.1038/nm.3990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muntoni F., Torelli S., Ferlini A. Dystrophin and mutations: one gene, several proteins, multiple phenotypes. Lancet Neurol. 2003;2:731–740. doi: 10.1016/S1474-4422(03)00585-4. [DOI] [PubMed] [Google Scholar]
- 35.Capkovic K.L., Stevenson S., Johnson M.C., Thelen J.J., Cornelison D.D.W. Neural cell adhesion molecule (NCAM) marks adult myogenic cells committed to differentiation. Exp. Cell Res. 2008;314:1553–1565. doi: 10.1016/j.yexcr.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mackey A.L., Kjaer M., Charifi N., Henriksson J., Bojsen-Moller J., Holm L., Kadi F. Assessment of satellite cell number and activity status in human skeletal muscle biopsies. Muscle Nerve. 2009;40:455–465. doi: 10.1002/mus.21369. [DOI] [PubMed] [Google Scholar]
- 37.Rokach O., Ullrich N.D., Rausch M., Mouly V., Zhou H., Muntoni F., Zorzato F., Treves S. Establishment of a human skeletal muscle-derived cell line: biochemical, cellular and electrophysiological characterization. Biochem. J. 2013;455:169–177. doi: 10.1042/BJ20130698. [DOI] [PubMed] [Google Scholar]
- 38.Gilbert P.M., Havenstrite K.L., Magnusson K.E.G., Sacco A., Leonardi N.A., Kraft P., Nguyen N.K., Thrun S., Lutolf M.P., Blau H.M. Substrate Elasticity Regulates Skeletal Muscle Stem Cell Self-Renewal in Culture. Science. 2010;329:1078–1081. doi: 10.1126/science.1191035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duchêne B.L., Cherif K., Iyombe-Engembe J.-P., Guyon A., Rousseau J., Ouellet D.L., Barbeau X., Lague P., Tremblay J.P. CRISPR-Induced Deletion with SaCas9 Restores Dystrophin Expression in Dystrophic Models In Vitro and In Vivo. Mol. Ther. 2018;26:2604–2616. doi: 10.1016/j.ymthe.2018.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zarrin A.A., Malkin L., Fong I., Luk K.D., Ghose A., Berinstein N.L. Comparison of CMV, RSV, SV40 viral and Vλ1 cellular promoters in B and T lymphoid and non-lymphoid cell lines. Biochim. Biophys. Acta. 1999;1446:135–139. doi: 10.1016/S0167-4781(99)00067-6. [DOI] [PubMed] [Google Scholar]
- 41.Ebadat S., Ahmadi S., Ahmadi M., Nematpour F., Barkhordari F., Mahdian R., Davami F., Mahboudi F. Evaluating the efficiency of CHEF and CMV promoter with IRES and Furin/2A linker sequences for monoclonal antibody expression in CHO cells. PLoS ONE. 2017;12:e0185967. doi: 10.1371/journal.pone.0185967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang Y., Chusainow J.M., Yap M.G.S. DNA methylation contributes to loss in productivity of monoclonal antibody-producing CHO cell lines. J. Biotechnol. 2010;147:180–185. doi: 10.1016/j.jbiotec.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 43.Hotta A. Genome Editing Gene Therapy for Duchenne Muscular Dystrophy. J Neuromuscul. Dis. 2015;2:343–355. doi: 10.3233/JND-150116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gee P., Xu H., Hotta A. Cellular Reprogramming, Genome Editing, and Alternative CRISPR Cas9 Technologies for Precise Gene Therapy of Duchenne Muscular Dystrophy. Stem Cells Int. 2017;2017:8765154. doi: 10.1155/2017/8765154. [DOI] [PMC free article] [PubMed] [Google Scholar]