Abstract
Purpose:
To characterize determinants of resident maternity leave and their effect on maternal and infant wellbeing. Among non-parents, to identify factors that influence the decision to delay childbearing
Study Design:
In 2016, a survey was sent to female residents at a large academic medical center on their experiences with maternity leave, the impact of personal and program factors on length of leave, reasons for delaying childbearing, and measures of wellbeing.
Results:
Forty-four percent (214/481) of residents responded. Fifty (23%) residents were parents and 25 (12%) took maternity leave during training. The average maternity leave length was 8.4 weeks and did not differ across program type, size, or program director gender, but was longer for programs with fewer women than men. The most common self-reported determinant of leave was financial. Residents with ≥ 8 weeks of leave were less likely to have postpartum depression or burnout and more likely to breastfeed longer, perceive support from colleagues and program directors, and be satisfied with resident parenthood. Among 104 non-parents who were married or partnered, 84 (81%) were delaying childbearing, citing busy work schedules, concern for burdening colleagues, and finances.
Conclusions:
This study suggests that multiple aspects of resident wellbeing are associated with longer maternity leaves, yet finances and professional relationships hinder length of leave and lead to delayed childbearing. These issues could be addressed at a program level with clear policies describing how work is redistributed during parental leave, and at an institutional and state level through provision of paid family leave.
Keywords: maternity leave, childbearing, wellbeing, internship and residency, graduate medical education, medical education & training
INTRODUCTION
In 1993, the results of a national survey of resident mothers showed that 36% of residents took 4 to 8 weeks of maternity leave during training, and 30% took less than 4 weeks.1 Since this survey, the number of women residents and faculty has substantially increased, 2,3 yet few studies have reexamined maternity leave practices since.4,5,6,7
Longer maternity leaves are consistently associated with better maternal and infant health outcomes. For example, studies of the general population have shown that more than 12 weeks of maternity leave is associated with fewer postpartum depressive symptoms and lower rates of self-reported poor health.8,9 Longer maternity leaves are also associated with longer duration of breastfeeding and increased early childhood checkups and immunizations.10 Despite the proven benefits of maternity leave, few residency programs provide explicit policies on the length of maternity leave permitted and how this is determined. In the absence of transparent practices, many of these decisions are determined on an ad hoc basis.11
To better understand the determinants and effects of maternity leave in residency, we examined factors that influence its length and assessed the impact of the length of maternity leave on resident and infant wellbeing. Among married or partnered residents who are not parents nor pregnant, we sought factors that influence the decision to delay childbearing during residency training.
METHODS
Study design
We conducted an anonymous survey of women residents enrolled across 24 graduate medical education (GME) programs at the University of Washington. REDCap was used to collect study data over a 2-week period (May 2016).12
Survey development
A survey tool was developed by identifying factors and survey items from current literature relating to maternity leave in GME.4,6,7,13 New items were drafted on breastfeeding duration, perceived support, and satisfaction with resident parenthood according to survey design best practices.14 Burnout was assessed using a single-item measure shown to be a reliable substitute for the Maslach Burnout Inventory domain of emotional exhaustion.15 Postpartum depression was assessed using the Edinburgh Postnatal Depression Scale, the most common and extensively validated screen for postpartum depression.16
Married and partnered participants who were nonparents were asked if they were delaying childbearing and if so, their reasons for doing so, and satisfaction with their decision. The framework for these items was based on prior literature exploring residents’ perceptions of childbearing as a career threat, and regrets of female career physicians with respect to delaying childbearing.17,18
The survey underwent content validation, followed by cognitive interviewing of volunteers representative of our target population.19 Volunteers were recent residency graduates, both parents and nonparents, who read each survey item aloud and explained their thought process in selecting their response. This reasoning was used to revise survey items to ensure that respondents would interpret the items as we intended. The final version was subsequently distributed to our study population.
Statistical Analysis
One-way analysis of variance was used to assess for differences in outcomes between maternity leaves of 8 weeks or more compared to less than 8 weeks. Eight weeks was chosen based on the distribution of reported maternity leaves among respondents. Program size was categorized as large for 40 or more residents, and small if less than 40, based on the internal distribution of participating program sizes. Program types were categorized according to medical, surgical, and hospital-based specialties.20
Outcomes were stratified by length of maternity leave. For breastfeeding duration, a target of 6 months or more was chosen per American Academy of Pediatrics recommendations.21 For satisfaction with the decision to have a child during residency, or to delay childbearing, Likert scales were used and collapsed into two groups: satisfied (“very satisfied”, “satisfied”) versus not satisfied (“neither”, “dissatisfied”, “very dissatisfied”). Likert scales were also utilized for questions on perceived support and collapsed into two groups: positive support (“well-supported”, “somewhat supported”) versus no support (“neutral”, “somewhat not supported”, and “not supported”). Although our data is presented in a dichotomous manner, we used 5-point Likert scales in anticipation of the variation among residents in their perceived satisfaction and support. By allowing for a range, we were better able facilitate residents’ assessments of their experiences.
To identify other determinants of length of maternity leave, and of delaying childbearing, respondents were asked to select up to three options from a list of choices, including a free-text response which were categorized into themes. We used SPSS Inc. version 19.0 (Chicago) for the analysis.22
At the end of the survey, participants were given the option of a free-text response for additional comments. These answers were used to provide context for our quantitative results.
RESULTS
A total of 214 residents (44%) responded with demographic data shown in Table 1. The distribution of respondents was compared to our institution’s female resident population in medical (66% versus 67%), surgical (20% versus 19%), and hospital-based programs (14% versus 14%) and found to be similar.
Table 1.
Resident demographics and response rates.
| Characteristic | All Respondents | Parents or Currently Pregnant |
||
|---|---|---|---|---|
| n | % | n | % | |
| Total | 214 | 44% | 50 | 23% |
| Age (years) - mean, sd | 31 | 3.4 | 33.7 | 3.5 |
| Program | ||||
| Medical | 141 | 66% | 30 | 60% |
| Surgical | 42 | 20% | 4 | 8% |
| Hospital-Based | 31 | 14% | 16 | 32% |
| Postgraduate Year | ||||
| PGY 1 | 47 | 22% | 6 | 12% |
| PGY 2 | 58 | 27% | 10 | 20% |
| PGY 3 | 56 | 26% | 17 | 34% |
| PGY 4 | 37 | 17% | 11 | 22% |
| PGY 5 | 8 | 4% | 3 | 6% |
| PGY 6 or more | 6 | 3% | 3 | 6% |
| Marital Status | ||||
| Married | 108 | 50% | 46 | 92% |
| Live with partner | 48 | 22% | 2 | 4% |
| Single | 54 | 25% | 0 | 0% |
| Divorced or Widowed | 4 | 2% | 2 | 4% |
| Other Graduate Education | ||||
| PhD | 13 | 6% | 7 | 14% |
| Other Masters degree or higher | 36 | 17% | 11 | 22% |
Residents with or expecting children
Among the 50 residents who are either parents or currently pregnant, 56% (28) of women had one child, and 34% (17) had two or more children. Seventy percent (35) reported pregnancy during residency, and 18% (9) reported current pregnancies.
Maternity leave
Among 25 women who reported maternity leave during residency, the mean length of leave was 8.4 weeks (standard deviation 2.6 weeks) (Figure 1). Most maternity leave lengths were less than 12 weeks, even when stratified by postgraduate year. Maternity leave tended to be longer for residents whose partners worked full time or were not in medical training (Table 2). On a program level, there was no statistically significant difference in length of leave between program type, size, or program director gender. However, resident maternity leave lengths in programs where residents were mostly men averaged nearly 2 weeks longer compared to programs where residents were mostly women.
Figure 1:
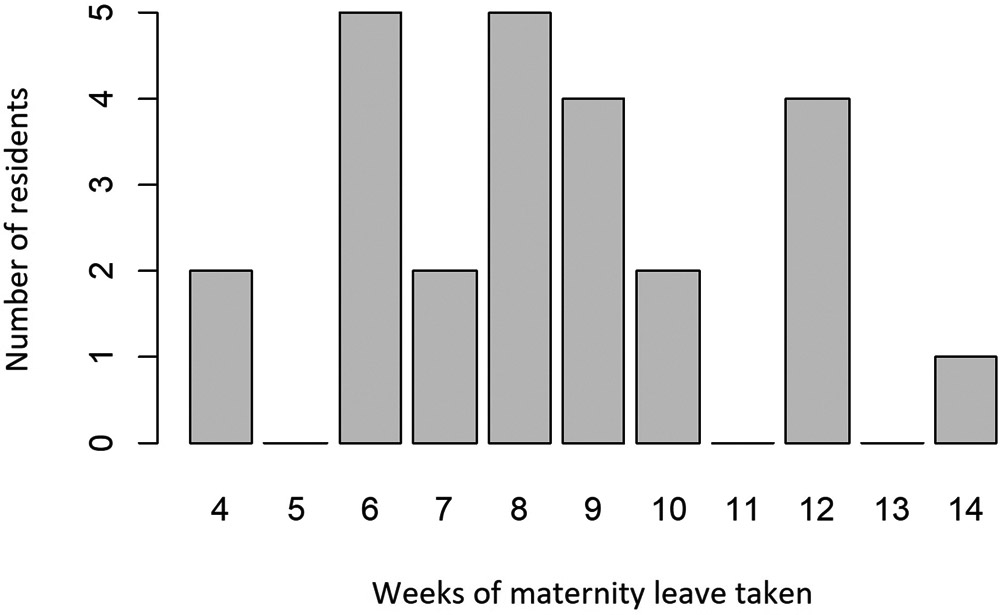
Distribution of resident maternity leave lengths.
Table 2.
Personal and program factors and their influence on length of maternity leave.
| n | Mean | Std Dev | p value | |
|---|---|---|---|---|
| Overall | 25 | 8.4 | 2.6 | |
| Partner in medical training | ||||
| yes | 4 | 8.3 | 3.3 | 0.89 |
| no | 20 | 8.5 | 2.6 | |
| Partner working full time | ||||
| yes | 18 | 8.7 | 2.7 | 0.44 |
| no | 6 | 7.7 | 2.7 | |
| Training Program | ||||
| Medical | 15 | 8.1 | 2.4 | 0.75 |
| Surgical | 2 | 9.0 | 4.2 | |
| Hospital Based | 8 | 8.9 | 2.9 | |
| Program size | ||||
| Small | 8 | 8.8 | 2.9 | 0.65 |
| Large | 17 | 8.2 | 2.5 | |
| Program Trainee majority gender | ||||
| Female | 12 | 7.4 | 2.0 | 0.07 |
| Male | 13 | 9.3 | 2.8 | |
| Program Director Gender | ||||
| Female | 13 | 9.0 | 2.1 | 0.24 |
| Male | 12 | 7.8 | 3.0 |
Self-reported factors influencing length of maternity leave are shown in Figure 2, with the most commonly cited determinant being family finances. Notably, our institution’s maternity leave policy did not specify the number of weeks. Multiple residents commented that our lack of a more detailed policy is a lack of protection that disproportionately affects women and perceived this as discriminatory toward their advancement. Another noted the conflict of interest arising from “the fact that an attending is able to control my maternity leave.”
Figure 2:
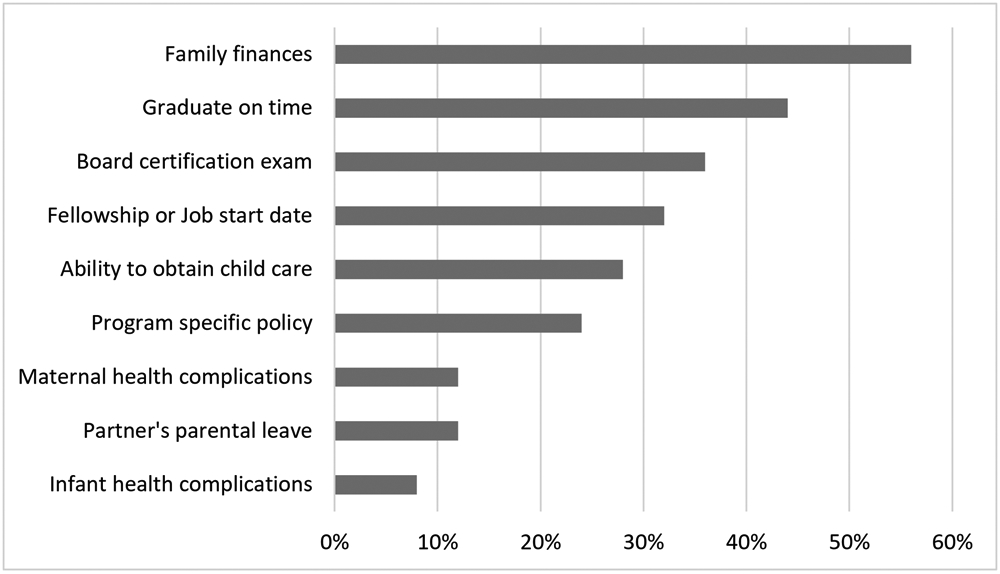
Self-reported determinants of maternity leave length (factors are not independent).
Qualitatively, there was considerable apprehension described by several residents regarding maternity leave potentially burdening their colleagues. One resident parent described feeling “like I was inconveniencing others and that my superiors were irritated that I chose to have a child in my training.”
Maternity leave outcomes
Compared to those with less than 8 weeks of maternity leave, a much higher proportion of residents with 8 weeks or more of leave reported breastfeeding for at least 6 months (Table 3). They were also more likely to have negative postpartum depression and burnout screens, greater perceptions of colleague and program director support, and greater satisfaction with childbearing during training. These findings were not statistically significant, likely due to the small sample size.
Table 3.
Maternal and infant wellbeing outcomes.
| Wellbeing outcomes | n | < 8 weeks | ≥ 8 weeks | p value |
|---|---|---|---|---|
| Breastfed ≥ 6 monthsa | 15 | 33% (2 of 6) | 89% (8 of 9) | 0.09 |
| Negative Postpartum Depression screenb | 13 | 33% (1 of 3) | 70% (7 of 10) | 0.51 |
| Negative Burnout screen | 25 | 33% (3 of 9) | 38% (6 or 16) | 1.00 |
| Positive Colleague support | 25 | 78% (7 of 9) | 88% (14 of 16) | 0.60 |
| Positive Attending support | 25 | 67% (6 of 9) | 69% (11 of 16) | 1.00 |
| Positive Program Director support | 25 | 67% (6 of 9) | 88% (14 of 16) | 0.31 |
| Satisfaction with decision to have a child during training | 25 | 56% (5 of 9) | 75% (12 of 16) | 0.39 |
Among participants who were 6 months or more postpartum.
Among participants who were 12 months or less postpartum.
Residents delaying childbearing
Among the 104 residents who were married or partnered, but not parents nor pregnant, 84 (81%) were intentionally delaying childbearing. The most commonly cited reasons were the busy work schedule of residency (81; 96%), concern that maternity leave would burden their colleagues (42; 50%), and family finances (38; 45%), followed by inability to obtain child care (35; 42%). Only 32% (27) expressed satisfaction with this decision.
Qualitatively, several residents acknowledged residency as the peak of their childbearing years, yet viewed the culture of their programs as an obstacle. A common concern among nonparents was that childbearing would negatively affect their colleagues. One participant observed contrition expressed by residents when “having to go pump breastmilk or coordinate childcare,” concluding that residencies “can do better supporting an environment that encourages people to have healthy family lives - without guilt.” This common conflict represents what another resident referred to as the “impossible choices” women are forced to make in training between risking infertility and potentially damaging their career.
DISCUSSION
We found that the majority of maternity leaves at our institution were less than the 12 weeks provided by the Family and Medical Leave Act.23 Obstacles to longer leaves, and to childbearing, appear to be tied to the financial strain of doing so and the perception of an unwelcoming environment which includes anxiety around burdening colleagues.
During the survey period, neither our institution, nor the state of Washington, provided paid family leave. Notably, this is in the setting of an already modest resident salary and medical school debt typically exceeding $100,000.24 While the financial burden of childbearing was explicitly described in our study, other results indirectly highlight this barrier. For example, the next three most frequently chosen determinants of maternity leave were related to the ability to work, suggesting an urgency in realizing anticipated income. Longer maternity leaves were also associated with a more financially stable partner. These findings suggest that finances may carry substantial weight in the decision-making process of maternity leave duration.
Concern for disrupting the training environment could explain why programs with male majorities had nearly 2 week longer maternity leaves than programs with female majorities. It is possible that maternity leaves in programs with lower ratios of women are viewed as less of an overall burden. The lack of a sufficiently detailed maternity leave policy, as pointed out by our participants, may have also contributed to this perception. Unclear expectations of how long a resident will be absent can result in uncertainty of how a colleague’s work could be affected, which was a significant concern among participants delaying childbearing.
When asked how supported a resident felt during their pregnancy, the people most affected by a resident’s absence, specifically their colleagues and the program director, were perceived as more supportive by residents with longer maternity leaves. This finding could reflect a program’s ability to plan for and accommodate maternity leaves, resulting in a culture of acceptance rather than inconvenience. Attending physician support was relatively unchanged with length of maternity leave, which may reflect the lack of an effect of maternity leave on their own work.
Based on prior literature showing that the support of coworkers toward a resident’s pregnancy could modify the resident’s perceptions of stress, we explored perceptions of support in the work environment as an indicator of wellbeing.25 The proportional differences in support, as well as our other wellbeing outcomes of postpartum depression, burnout, and length of breast feeding, suggest that, similar to studies of the general population,26 residents also see an improvement in their wellbeing from longer maternity leaves.
This study has important implications for policy at a program level. At the time of this survey, no residency program at our institution had a written, program-specific maternity leave policy. Thus, both pregnant residents and their colleagues had no information on how clinical work is shifted when a resident takes leave, nor how that work is compensated for upon their return. The lack of a transparent process resulted in anxiety on the part of pregnant residents about of peer perceptions and influenced residents who reported delaying childbearing due to the worry of burdening colleagues and extending training. For this reason, it is important that programs not only create maternity leave policies that are easily accessible to all residents, both pregnant and not pregnant, but that such policies also specify the details of how length of leave is determined, how clinical work during a leave is redistributed, if at all, and when training extension is required. The latter factor is particularly important as the desire to graduate on time determined the length of maternity leave for more than 40% of our respondents. Given that training extension is heavily influenced by the requirements of medical specialty boards, the parameters of when to extend training could be a fruitful area of collaboration between programs and medical specialty boards.
Eliminating these uncertainties can mitigate the peer discord that has been described to occur with resident pregnancies27,28 and help female residents make informed childbearing decisions. Moreover, describing clear logistics in a written policy could also benefit programs by providing a consistent blueprint for how to plan for future resident maternity leaves.
There are also implications for policy at an institutional and state level. Longer maternity leaves favored better wellbeing outcomes but were hindered by financial factors. Institutional and state policy could best address this by facilitating paid family leave. Paid family leave has been associated with better maternal and infant health outcomes29 and has the potential to close the gender presence, pay, and productivity gaps in academics.30 This effect increases with more generous leave. Given the increasing emphasis on resident wellbeing and the increasing numbers of women in medicine, the need for paid family leave has become more relevant and pressing to our field.
Our study’s primary limitation was that our survey was limited to a single center, resulting in a relatively small number of respondents who took maternity leave during training. We were likely underpowered to detect statistically significant differences due to the small size. Yet, given that only 3% of residents in the United States reported that their programs provide childcare benefits27 and only three states provided paid family leave at the time of this survey, we suspect our results are translatable to other institutions. Because our questions reviewed past experiences, there may be recall bias in the accuracy of perceptions and factors explored. Finally, given that participation was voluntary, there is likely self-selection bias toward women with personal experience in the topic at hand.
CONCLUSION
Despite the proportion of women residents steadily rising across specialties over the past twenty years, maternity leave durations remain less than ideal in this population. GME policies could start to address this issue by focusing on the financial burdens of unpaid leave and flexible schedules that allow women to meet fellowship or job start dates. Creating clear and easily accessible policies could also help programs and trainees to plan for leave, thus mitigating the stress of an unknown burden to colleagues. The potential benefits of these actions include improved resident and infant wellbeing as well as advancing a culture of medical education that does not divert women from their desired careers nor risk unintentional childlessness, but rather, creates a more supportive environment for women to advance through training.
MAIN MESSAGES.
Resident wellbeing increases and programs are perceived as more supportive when resident maternity leaves are longer.
Most female residents are dissatisfied with the decision to delay childbearing during training, citing finances and fear of damaging their careers as reasons for doing so.
Clear and detailed maternity leave policies at a residency program level can benefit residents and their colleagues by protecting them from unclear expectations, concurrently mitigating peer discord.
Institutional and state maternity leave policies can be used to promote gender equity and wellbeing in medicine by providing for paid leave and addressing the local culture that impedes maternity leave length and childbearing.
CURRENT RESEARCH QUESTIONS.
How does a resident’s decision to delay childbearing during training affect childbearing and productivity in their career?
How many graduate medical education programs have clear maternity leave policies that are easily accessible by all residents and applicants?
How does a clear and easily accessible maternity leave policy influence perceptions of resident pregnancy in that program?
Acknowledgments
FUNDING: This study was funded through a grant by the Center for Leadership and Innovation in Medical Education at the University of Washington School of Medicine and supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1 TR000423.
Footnotes
COMPETING INTERESTS: None declared.
PATIENT CONSENT: Not required.
REFERENCES
- 1.Bongiovi ME, Freedman J. Maternity leave experiences of resident physicians. J Am Med Womens Assoc. 1993;48(6):185–8,193. [PubMed] [Google Scholar]
- 2.Bickel J, et al. Women in Academic Medicine: Statistics. July 1993. Association of American Medical Colleges: Washington D.C. [Google Scholar]
- 3.Association of American Medical Colleges. AAMC data book: statistical information related to medical schools and teaching hospitals. 2017. Association of American Medical Colleges: Washington D.C. [Google Scholar]
- 4.Sandler BJ, Tackett JJ, Longo WE, Yoo PS. Pregnancy and Parenthood among Surgery Residents: Results of the First Nationwide Survey of General Surgery Residency Program Directors. J Am Coll Surg. 2016. June;222(6):1090–6. [DOI] [PubMed] [Google Scholar]
- 5.Hutchinson AM1, Anderson NS 3rd, Gochnour GL, Stewart C. Pregnancy and childbirth during family medicine residency training. Fam Med. 2011. March;43(3):160–5. [PubMed] [Google Scholar]
- 6.Holliday EB, Ahmed AA, Jagsi R, et al. Pregnancy and Parenthood in Radiation Oncology, Views and Experiences Survey (PROVES): Results of a Blinded Prospective Trainee Parenting and Career Development Assessment. Int J Radiat Oncol Biol Phys. 2015;92(3):516–524. [DOI] [PubMed] [Google Scholar]
- 7.Blair JE, Mayer AP, Caubet SL, Norby SM, O'Connor MI, Hayes SN. Pregnancy and Parental Leave During Graduate Medical Education. Acad Med. 2016. July;91(7):972–8. [DOI] [PubMed] [Google Scholar]
- 8.Dagher RK, McGovern PM, Dowd BE. Maternity Leave Duration and Postpartum Mental and Physical Health: Implications for Leave Policies. Journal of Health Politics, Policy and Law, Vol. 39, No. 2, April 2014. [DOI] [PubMed] [Google Scholar]
- 9.Gault B, Hartmann H, Hegewisch A, Milli J, Reichlin L. Paid Parental Leave in the United States: What the data tell us about access, usage, and economic and health benefits The Institute for Women’s Policy Research. U.S. Department of Labor Women's Bureau; Washington, DC: March 2014. [Google Scholar]
- 10.Ogbuanu C, Glover S, Probst J, Liu J, Hussey J. The Effect of Maternity Leave Length and Time of Return to Work on Breastfeeding. Pediatrics. 2011. June; 127(6): e1414–e1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss J, Teuscher D. What Provisions Do Orthopaedic Programs Make for Maternity, Paternity, and Adoption Leave? Clin Orthop Relat Res. 2016. September;474(9):1945–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support, J Biomed Inform. 2009. April;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sattari M, Serwint JR, Neal D, Chen S, Levine DM. Work-Place Predictors of Duration of Breastfeeding among Female Physicians. J Pediatr 2013;163:1612–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rickards G, Magee C, Artino AR Jr. You can’t fix by analysis what you’ve spoiled by design: developing survey instruments and collecting validity evidence. J Grad Med Educ. 2012;4(4):407–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dolan ED, Mohr D, Lempa M, Joos S, Fihn SD, Nelson KM, Helfrich CD. Using a Single Item to Measure Burnout in Primary Care Staff: A Psychometric Evaluation. J Gen Intern Med 30(5):582–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sit DK, Wisner KL. The Identification of Postpartum Depression. Clin Obstet Gynecol. 2009. September; 52(3): 456–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willett LL, Wellons MF, Hartig JR, et al. Do women residents delay childbearing due to perceived career threats? Acad Med. 2010;85(4):640–646. [DOI] [PubMed] [Google Scholar]
- 18.Stentz NC, Griffith KA, Perkins E, Jones RD, Jagsi R. Fertility and Childbearing among American Female Physicians. Journal of Women's Health. 2016;25(10):1059–1065. [DOI] [PubMed] [Google Scholar]
- 19.Willis GB, Artino AR Jr.. What Do Our Respondents Think We’re Asking? Using Cognitive Interviewing to Improve Medical Education Surveys. J Grad Med Educ. 2013;5(3):353–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Accreditation Council for Graduate Medical Education. Data Resource Book, Academic Year 2015–2016. http://www.acgme.org/Portals/O/PFAssets/PublicationsBooks/2015-2016_ACGME_DATABOOK_DOCUMENT_Locked.pdf. Accessed August 1, 2017.
- 21.Johnston M, Landers S, Noble L, Szucs K, Viehmann L. Breastfeeding and the use of human milk. Pediatrics. 2012. March;129(3):e827–41. [DOI] [PubMed] [Google Scholar]
- 22.IBM Corp. Released 2010. IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp. [Google Scholar]
- 23.United States Department of Labor Wage and Hour Division. Family and Medical Leave Act. Accessed May 7, 2017 Available at: http://www.dol.gov/whd/fmla/.
- 24.Chesanow N. Residents Salary & Debt Report 2016. Medscape; Accessed May 7, 2017 Available at: http://www.medscape.com/features/slideshow/public/residents-salary-and-debt-report-2016#page=1. [Google Scholar]
- 25.Phelan ST. Sources of stress and support for the pregnant resident. Acad Med. 1992. June;67(6):408–10. [DOI] [PubMed] [Google Scholar]
- 26.Avendano M, Berkman LF, Brugiavini A, Pasini G. The long-run effect of maternity leave benefits on mental health: Evidence from European countries. Social science & medicine (1982). 2015;132:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mundschenk MB, Krauss EM, Poppler LH, et al. Resident perceptions on pregnancy during training: 2008 to 2015. American Journal of Surgery. 2016;212(4):649–659. [DOI] [PubMed] [Google Scholar]
- 28.Turner PL, Lumpkins K, Gabre J, Lin MJ, Liu X, Terrin M. Pregnancy among women surgeons: Trends over time. Archives of Surgery. 2012;147(5):474–479 [DOI] [PubMed] [Google Scholar]
- 29.Heymann J, Sprague AR, Nandi A, et al. Paid parental leave and family wellbeing in the sustainable development era. Public Health Reviews. 2017;38:21. doi: 10.1186/s40985-017-0067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Waldfogel J, Higuchi Y & Abe M Family leave policies and women's retention after childbirth: Evidence from the United States, Britain, and Japan. J Popul Econ. 1999;12(4):523–45. [Google Scholar]


