Abstract
Background and aims:
The long term population health impact of nicotine vaping products (NVPs) use among smokers is unknown and subject to a range of plausible assumptions about the use and health consequences of NVPs. While NVPs use may substitute for cigarette smoking and thereby aid in quitting cigarette use, it is also possible that smokers who would have otherwise quit would instead delay quitting cigarettes. We aimed to develop a cohort-specific simulation model of the impact of NVPs on smoking cessation by adult smokers and resulting premature deaths (PD) and life-years lost (LYL).
Design:
A cohort-specific simulation model of the impact of NVPs on smoking cessation by adult smokers and resulting premature deaths (PD) and life-years lost (LYL) was developed by gender for two birth-cohorts, age 30 and age 50 in 2012. Extensive sensitivity analyses were conducted.
Setting:
United States
Participants:
Smokers in two birth-cohorts, age 30 and age 50 in 2012
Measurements:
Data were from the 1965–2012 National Health Interview Surveys and the 2014/5 Tobacco Use Supplement of the Current Population Survey. The model incorporated a range of plausible assumptions from published literature about transition rates from regular smoking to exclusive NVP and dual use, from dual use to exclusive NVP use and from exclusive NVP use to no use.
Findings:
Compared with the No-NVP scenario, the male (female) model projected 17.8% (19.3%) fewer PDs and 22.9% (26.6%) fewer LYL for the 1982 cohort and 5.4% (7.3%) fewer PDs and 7.9% (11.4%) fewer LYL for the 1962 cohort. These gains were sensitive to NVP use over time, age of initial NVP use, transitions from smoking to dual, exclusive NVP and no use, and relative NVP mortality risks.
Conclusions:
Nicotine vaping product (NVP) use in the US is projected to have a net positive impact on population health over a wide range of plausible levels of NVP use, transitions to dual, exclusive NVP and no use, and NVP risks. However, net impact is sensitive to parameter estimates.
Keywords: e-cigarettes, public health, cessation, model, vaporized nicotine products, cohort analysis
INTRODUCTION
Nicotine vaping products (NVPs), including e-cigarettes, represent a new generation of nicotine delivery products. While the long-term health risks of NVPs remain to be characterized, NVPs appear to be much safer than tobacco cigarettes based on studies of their chemical composition and exposure biomarkers (1–4). With newer generations of products shown to be progressively more efficient in delivering nicotine to the user (2, 5, 6), NVPs appear to have increasingly greater potential to be useful aids to help smokers to stop smoking (7–10). However, the effects of NVPs on population health will depend on how they are used in relationship to cigarettes.
Since August 2016 in the U.S., NVPs have been subject to the Tobacco Control Act and are under the jurisdiction of the Food and Drug Administration (11, 12). To guide policy, the evaluation of NVPs toxicity and their effect on the uptake and cessation of existing tobacco products is needed. To accomplish this aim, modeling has been shown to be a useful method to synthesize and integrate the best available evidence (13–21). In a previous paper (18), a decision-theoretic model was employed to evaluate the public health impact of NVP use (“vaping”) at an age when initiation into cigarette use (”smoking”) generally takes place. Unlike previous models of NVP use, that model was developed for a specific birth cohort.
Cohort-specific analyses may be particularly important in gauging the role of vaping in cessation. While NVP use at any point in time depends on perceived product characteristics, product availability, and current tobacco control policies, current use is also likely to depend on the past experiences of each cohort with smoking and vaping. For example, in the absence of significant innovation in NVPs, future use is likely to decline if cigarette smokers or their friends have tried NVPs and found them unappealing (e.g., due to perceived harms or other characteristics of the product) or found that they did not yield anticipated effects, i.e. the ability to quit cigarette use. These experiences will depend on the evolution of NVP products, the characteristics of those who have previously used NVPs (e.g., younger aged smokers), and past policies, e.g., older smokers will have experienced changes in tobacco control policies (such as media campaigns) not experienced by those younger.
In this paper, we adopt a public health framework (22) to consider the impact of vaping on smoking cessation and its population health impact within two birth cohorts of smokers. The focus is on the modeling of cohort-specific effects and on the relevant parameters necessary to gauge population health outcomes. Since current information on use rates and transition rates is limited, the focus of this paper is heuristic, i.e., on the development of the model, rather than the predictions of future outcomes.
METHODS
To analyze the potential effects of vaping, we consider two cohorts: the 1982 birth cohort, i.e., those age 30 in 2012, an age when smoking patterns have been well-established, and the 1962 birth cohort, i.e., those age 50 in 2012, an age when cessation rates are typically high (24, 25). The models begin in 2012, when the prevalence of vaping was still quite low (23). We first project smoking rates over each cohort’s life cycle in the absence of vaping. We then consider the effects of vaping on smoking rates, incorporating cohort-specific patterns, and the resulting impact on mortality.
The No-NVP Scenario
To model counterfactual smoking patterns in the absence of vaping, we projected smoking rates using data prior to significant vaping. An age-period-cohort statistical technique (26) was applied to yearly data from National Health Interview Surveys from 1965 through 2012 to estimate the implied initiation and cessation rates. Cessation was defined as smokers who quit for at least two years, a long enough cessation period so that relapse was unlikely. Age- and cohort-specific cessation and initiation rates were used to project future smoking rates in the absence of NVPs.
NVP Scenario
Conceptually, the public health impact of NVP use ultimately depends on whether vaping is by cigarette smokers who would have otherwise quit smoking (22). Public health is improved if those who would not have otherwise quit smoking actually do quit or those who would have remained smokers become dual users and smoke fewer cigarettes or exclusively vape. Conversely, public health is worsened if smokers who would have otherwise quit smoking instead become dual users or long-term vapers.
In the model, ‘otherwise quitters’ are defined as those who would have quit in the No-NVP scenario, and ‘otherwise smokers’ are defined as those who would have remained smokers. Just as smoking cessation in the No-NVP scenario is modelled as a period long enough to incorporate relapse to smoking, we assume no relapse from dual or exclusive vaping back to exclusive smoking. Relapse to smoking may increase or decrease with vaping, but to simplify the analyses the model does not specifically consider these transitions.
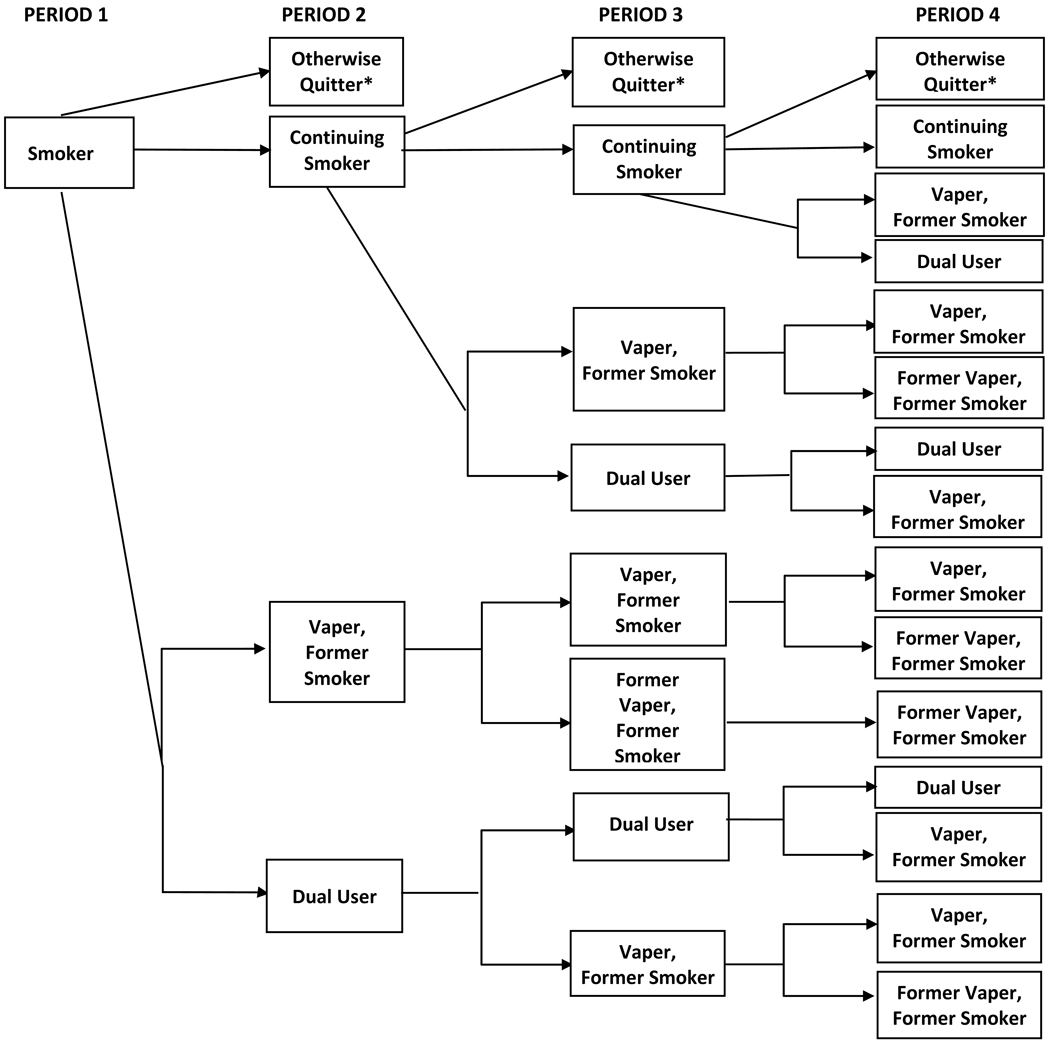
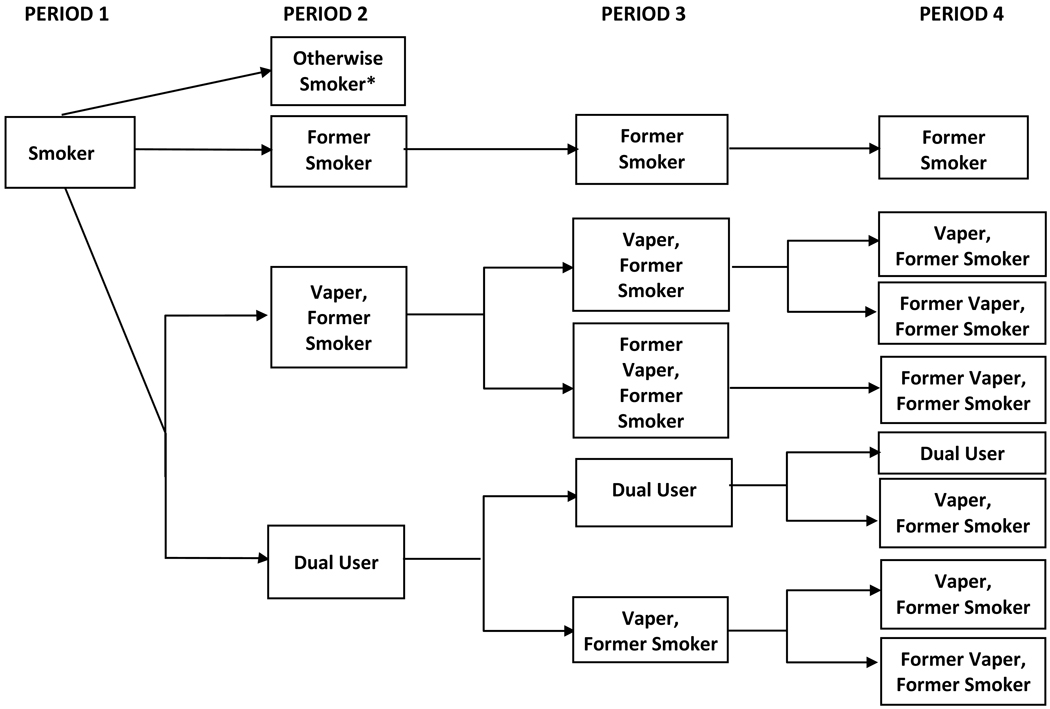
The potential transitions for otherwise smokers are illustrated in Figure 1 and the transitions for otherwise quitters are shown in Figure 2. We make a set of assumptions about potential transitions each year, which depend on transitions by the cohort in the previous year. In the first year of NVP use, both otherwise smokers and otherwise quitters who use NVPs become either dual users or former smokers who currently use NVPs. Under these assumptions, no smokers use NVPs and quit smoking in the first year of vaping. In the second year of vaping, dual users may transition to former smokers who currently vape or remain dual users, and exclusive vapers may quit and become former smokers who previously vaped or remain vapers Under these conditions, vaping-induced transitions to former smoker with no NVP use take at least two years; more immediate cessation from both smoking and vaping would accelerate the timing, but have little impact on overall results within this relatively narrow time window.
Figure 1.
Transitions with Nicotine Vaping Product Use Among Otherwise Smokers
*Otherwise quitter may use NVPs in the next period
Figure 2.
Transitions with Nicotine Vaping Product Use Among Otherwise Quitters
*Otherwise smoker may use NVPs in the next period
Over time, use rates and transitions for a particular cohort may depend on past perceptions, experience and policies as well as recent changes in these factors. Accordingly, vaping rates may vary by age and cohort over time. We focus on cohort-specific variations in use, but transitions to dual use, exclusive vaping and no use may also vary over time for each cohort. A mathematical formulation incorporating the different possibilities is presented in the Supplement.
NVP Parameters
In operationalizing the model, a measure of regular use is first defined that becomes the basis for initial transitions to exclusive and dual (with cigarette) NVP use, followed by transitions from dual and exclusive NVP use to no use. For simplicity, these transitions are assumed constant. The vaping rates and transition parameters are shown in Table 1.
Table 1.
Model Parameters for NVP Scenarios with the Same Parameters for Both Otherwise Smokers and Otherwise Quitters for Cohort 30 and 50 in 2012 by Gender and Measure
| Gender & Use | Male 25 day use | Female 25 day use | Male 10 day use | Female 10 day use | ||||
|---|---|---|---|---|---|---|---|---|
| Cohort age in 2012 | Age 30 | Age 50 | Age 30 | Age 50 | Age 30 | Age 50 | Age 30 | Age 50 |
| NVP Use Rate by Exclusive Smokers Each Year | ||||||||
| % NVP use by smokers in the initial year | 6.0%* | 4.0%* | 4.0%* | 4.0%* | 8.5%* | 5.5%* | 6.5%* | 6.5%* |
| Decay rate of NVP use in each of the following years | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% |
| % dual use among NVP users** | 75%* | 65%* | 65%* | 65%* | 65%* | 55%* | 75%* | 75%* |
| Transitions After the First Year of NVP Use | ||||||||
| Exclusive NVP to no use | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% |
| Dual to exclusive NVP | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% | 5%, 20% |
| Relative Risks with NVP Use Relative to Exclusive Cigarette Use | ||||||||
| Exclusive NVP use | 5%, 10% | 5%, 10% | 5%, 10% | 5%, 10% | 5%, 10% | 5%, 10% | 5%, 10% | 5%, 10% |
| Dual NVP Use | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% | 80%, 100% |
Scenarios were also considered where NVP use rates and the percent dual are halved for otherwise quitters.
The percent dual use is measured as the number of dual users (current smokers using NVPs) divided by the number of smokers one year ago from Table 2. The percent of exclusive NVP use (as former smokers) is estimated as 100% minus the percent dual use.
NVP Use
While current NVP use is often measured as any use in the last 30 days (2), the public health impact of vaping ultimately depends on regular use of NVPs compared to cigarettes, which is conceptualized as sufficient time for the accumulation of measureable harms (27). Based on a recent analysis of vaping (28) and its interrelationship with smoking cessation (9), we focus on those who vaped in at least 25 of the past 30 days (implying daily use) as a meaningful measure of regular use.
Data is from the 2014/15 Tobacco Use Supplement of the Current Population Survey, around the time when the percentage of adults who switched from cigarettes to NVPs doubled (29) and when vaping devices with more efficient nicotine delivery were introduced (30, 31). Initial NVP use (either dual or exclusive) was estimated using a sample of individuals who were smokers one year ago, thereby including those who were still smoking and those who quit in the past year. We note that this measure excludes those who may have used NVPs and quit both NVPs and cigarettes, but includes some regular vapers who may have begun their vaping in earlier years. The initial vaping rates were measured by 25-day use among those ages 25–44 for the 1982 cohort and ages 45–54 for the 1962 cohort, but we considered vaping in the younger and older age groups. Based on Table 2, we approximated male vaping rates of 6.0% for the 1982 cohort and of 4.0% for the 1962 cohort. For females of both cohorts, 25-day rates were 4.0%. We initially assume that these use rates remained constant each year.
Table 2.
Estimated NVP Use by Age and Gender from 2014/15 CPS-TUS
| Male | Smokers One Year ago | Current Smokers Only | Quit in the Last Year | Percent Dual | |||
|---|---|---|---|---|---|---|---|
| Ages | N | 25 of last 30 days | N | 25 of last 30 days | N | 25 of last 30 days | 25 of last 30 days |
| 18–24 | 911 | 7.0% | 747 | 4.7% | 164 | 17.7% | 55% |
| 25–34 | 2411 | 5.5% | 2011 | 3.8% | 400 | 14.3% | 57% |
| 35–44 | 2199 | 5.4% | 1909 | 3.7% | 290 | 16.2% | 60% |
| 45–54 | 2323 | 3.0% | 2133 | 2.0% | 190 | 14.7% | 60% |
| 55–64 | 2440 | 3.8% | 2188 | 2.7% | 252 | 13.5% | 63% |
| 65+ | 1410 | 2.8% | 1247 | 2.3% | 163 | 6.1% | 74% |
| Total | 11694 | 4.4% | 10235 | 3.0% | 1459 | 14.1% | 60% |
| FEMALES | Smokers One Year ago | Current Smokers Only | Quit in the Last Year | Percent Dual | |||
| Ages | N | 25 of last 30 days or daily | N | 25 of last 30 days | N | 25 of last 30 days | 25 of last 30 days |
| 18–24 | 802 | 3.9% | 648 | 2.9% | 154 | 7.8% | 61% |
| 25–34 | 2359 | 4.2% | 2018 | 3.4% | 341 | 9.4% | 68% |
| 35–44 | 2246 | 4.0% | 1976 | 2.5% | 270 | 14.8% | 56% |
| 45–54 | 2664 | 4.5% | 2422 | 3.5% | 242 | 14.5% | 71% |
| 55–64 | 2419 | 3.8% | 2168 | 2.9% | 251 | 11.6% | 68% |
| 65+ | 1533 | 3.6% | 1349 | 3.0% | 184 | 8.2% | 73% |
| Total | 12023 | 4.1% | 10581 | 3.1% | 1442 | 11.3% | 67% |
Transitions
As shown in Figure 1, vaping by smokers may lead to either dual or exclusive vaping (i.e., quit smoking). The percent that transition to dual use (i.e., who continue vaping as smokers) was measured by the number of smokers who currently vape as a percent of all smokers one year ago who currently vape. From Table 2, we calculate the percent that become dual users as (Ns*NVPs)/(Ns*NVPs +NQ*NVPQ), where Ns is the number of smokers and NVPs and NVPQ are the prevalence of NVP use among smokers and among those who quit smoking. We estimate that 65% of the 1982 male cohort and 55% of the 1962 male cohort became dual users. For females, 65% of users for both cohorts became dual users. The percent that quit smoking and exclusively vape is 100% minus the percent that transition to dual use.
Dual users may transition to former smokers who continue to vape or stay dual users. To quantify the likelihood of these transitions longitudinal studies gauging transitions from dual to exclusive NVP use are needed. Such studies are limited (33), but as many as 30% of regular smokers successfully quit when regularly vaping (9), consistent with other studies on smoking cessation (2, 34–36). A recent longitudinal study (32) found that 5% of dual users transitioned to exclusive use and another 7% transitioned to no use within a year. In addition, intention to quit is high among smokers who vape (2, 37, 38). Based on this evidence, we conservatively estimate that 5% of dual users transition to exclusive vaping each year.
Once individuals become exclusive vapers, they may remain exclusive vapers or transition to former smokers who no longer vape. A longitudinal study (32) found that 19% of former established smokers quit vaping within the year, but did not distinguish regular from occasional vaping. A longitudinal study (39) found that most daily vapers were still vaping one year later, while a randomized controlled trial (40) found that more than 70% of vapers quit vaping as well as smoking after one year (9). Vapers have also been found to be less dependent than smokers (2, 41, 42).
Calculation of Premature Deaths and Life Years Lost and Gained
For the No-NVP scenario, the number of premature deaths (PDs) at each age for current and former smokers was calculated by multiplying their excess risks by the corresponding population (prevalence rate x projected US population (43)). Excess risk for current (former) smokers was calculated as the current (former) smoker mortality rate minus the never smoker mortality rate. Mortality rates are derived from all-cause mortality cohort life tables (44). Life years lost (LYL) at each age were estimated by multiplying PDs by the expected life years remaining for a never smoker.
In the NVP scenarios, while smoker PDs decline, PDs also result from dual use, former smokers who vape, and former smokers who quit vaping. With substantially lower levels of toxic substances (1, 45–47), a multi-criteria decision analysis estimated NVP risks at 5% those of cigarette risks (46). Former smokers who use NVPs are assumed to have 5% higher excess risk relative to former exclusive smokers, but their risk reverts to that of former smokers if they quit NVPs. Dual users may also have lower mortality risk than exclusive cigarette smokers, because vaping is associated with fewer cigarettes smoked (48). We estimate excess risk of dual use as 80% of the difference between the risks of former and current smokers.
By cohort, the public health impact of NVP use is evaluated as the difference in PDs and LYLs between the No-NVP and NVP scenarios summed from initial age through age 99. Life years gained per smoker was obtained by dividing life years gained by the smoking population in 2012.
Sensitivity Analysis
We conducted sensitivity analysis on the above parameters. Instead of assuming a 5% NVP quit rate among dual users and former smokers who vape, we consider a 20% NVP quit rate each year. Instead of assuming constant use rates, we consider where use rates declined at a rate of 20% each year. Relative to cigarette use, we also consider an excess mortality risk of 10% for former smokers who vape together with 100% risk for dual use.
We assumed common use and transition rates for otherwise quitters and otherwise smokers. However, studies have found more past quit attempts and use of other cessation methods among users compared with non-users of NVPs (2, 37, 49, 50), and US (51) and England (7) studies also indicate increasing smoking quit rates in recent years, again suggesting heavier vaping by otherwise smokers relative to otherwise quitters. To incorporate these findings, we consider scenarios with initial NVP use and dual use levels of otherwise quitters at 50% those of otherwise smokers.
Instead of the 25-day measures of NVP use, we considered at least 10 of the last-30 days. Using the same data source as above, we approximated male vaping rates of 8.5% and 5.5% for the 1982 and 1962 cohorts respectively, and 6.5% for both female cohorts. Of these, 65% and 75% of the 1982 and 1962 male cohorts and 75% of both female cohorts became dual users.
RESULTS
Tables 3 and 4 are for each cohort and contain the male and female smoking and NVP prevalence, PDs and LYL by age under the No-NVP and the different NVP scenarios.
Table 3.
Prevalence of Smoking and NVP Use, Premature Deaths and Life Years Lost for the 1982 Birth Cohort by Gender, NVP Use
| MALE | FEMALE | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SCENARIO | Outcome | Age 30 | Age 50 | Age 70 | Age 30–99 | % Change from No-NVP | Age 30 | Age 50 | Age 70 | Age 30–99 | % Change from No-NVP |
| Smoker | 32.7% | 18.9% | 7.4% | 24.5% | 14.8% | 5.4% | |||||
| Former smoker | 11.6% | 26.3% | 35.4% | 9.3% | 20.0% | 28.4% | |||||
| Premature deaths | - | 1,777 | 8,670 | 390,632 | - | 398 | 3,037 | 135,468 | |||
| Life years lost | - | 60,040 | 138,753 | 4,577,882 | - | 14,604 | 55,134 | 1,628,491 | |||
| Smoker | 32.7% | 5.6% | 0.8% | 24.5% | 6.7% | 1.1% | |||||
| Former smoker | 11.6% | 21.2% | 23.5% | 9.3% | 17.3 | 20.3% | |||||
| Dual user | 0.0% | 8.1% | 3.6% | 0.0% | 4.3% | 2.3% | |||||
| FS-NVP | 0.0% | 7.3% | 5.2% | 0.0% | 4.6% | 3.6% | |||||
| FS-Former NVP | 0.0% | 3.1% | 8.5% | 0.0% | 1.9% | 5.5% | |||||
| Premature deaths | - | 1,224 | 6,713 | 321,047 | 17.8% | - | 278 | 2,136 | 109,364 | 19.3% | |
| Life years lost | - | 41,358 | 107,435 | 3,529,119 | 22.9% | - | 10,192 | 38,789 | 1,194,619 | 26.6% | |
| Scenario 2 | Premature deaths | - | 785 | 5,173 | 281,401 | 28.0% | - | 209 | 1,427 | 91,576 | 32.4% |
| Life years lost | - | 26,534 | 82,789 | 2,752,223 | 39.9% | - | 7,650 | 25,905 | 881,808 | 45.9% | |
| Scenario 3 | Premature deaths | - | 1,558 | 7,975 | 362,182 | 7.3% | - | 357 | 2,796 | 126,915 | 6.3% |
| Life years lost | - | 52,654 | 127,619 | 4,177,392 | 8.7% | - | 13,082 | 50,768 | 1,500,438 | 7.9% | |
| Scenario 4 | Premature deaths | - | 1,388 | 7,076 | 331,582 | 15.1% | - | 307 | 2,351 | 114,972 | 15.1% |
| Life years lost | - | 46,921 | 113,231 | 3,754,234 | 18.0% | - | 11,264 | 42,679 | 1,295,836 | 20.4% | |
| Scenario 5 | Premature deaths | - | 1,212 | 6,686 | 320,568 | 17.9% | - | 276 | 2,119 | 108,969 | 19.6% |
| Life years lost | - | 40,964 | 107,001 | 3,513,781 | 23.2% | - | 10,121 | 38,470 | 1,186,946 | 27.1% | |
| Scenario 6 | Never smoker | 55.6% | 54.7% | 58.7% | 66.2% | 65.2% | 67.8% | ||||
| Smoker | 32.7% | 3.3% | 0.3% | 24.5% | 4.0% | 0.4% | |||||
| Former smoker | 11.6% | 20.4% | 22.0% | 9.3% | 16.1% | 17.9% | |||||
| Dual user | 0.0% | 8.0% | 3.1% | 0.0% | 6.5% | 3.0% | |||||
| FS-NVP | 0.0% | 9.3% | 5.6% | 0.0% | 5.8% | 4.1% | |||||
| FS-Former NVP | 0.0% | 4.2% | 10.2% | 0.0% | 2.4% | 6.8% | |||||
| Premature deaths | - | 1,035 | 6,228 | 301,025 | 22.9% | - | 254 | 2,056 | 105,076 | 22.4% | |
| Life years lost | - | 34,968 | 99,670 | 3,226,301 | 29.5% | - | 9,327 | 37,323 | 1,138,418 | 30.1% | |
Notes: Scenario 1 uses the at least 25 of last 30-day vaping measure with NVP use risks at 5% and dual use risk at 80% those of smoking, assuming the same NVP and dual use rates by otherwise smokers and otherwise quitters with new NVP use remaining the same each year (6.0% male; 4.0% female) and most users become dual users (75% male; 65% female) and 5% of dual users transitioning exclusively to NVPs and 5% of NVP users quitting vaping. Scenario 2 assumes 20% NVP and dual use quit rate with parameters otherwise the same as Scenario 1. Scenario 3 assumes NVP use declines by 20% each year with parameters otherwise the same as Scenario 1. Scenario 4 assumes NVP/dual use mortality risk at 10%/100% those of cigarette with parameters otherwise the same as Scenario 1. Scenario 5 assumes the rate of smokers using NVP and dual use rate for otherwise quitters at half the rates of otherwise smokers with parameters otherwise the same as Scenario 1. Scenario 6 uses the at least 10 of last 30-day NVP use measure with new NVP use remaining the same each year (8.5% male; 6.5% female) and most users become dual users (65% male; 75% female), with parameters otherwise the same as Scenarios 1.
Table 4.
Prevalence of Smoking and NVP Use, Premature Deaths and Life Years Lost for the 1962 Birth Cohort by Gender, NVP Use
| MALE | FEMALE | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SCENARIO | Outcome | Age 50 | Age 70 | Age 99 | Age 50–99 | % Change from No-NVP | Age 50 | Age 70 | Age 99 | Age 50–99 | % Change from No-NVP |
| Smoker | 21.5% | 8.2% | 0.3% | 18.6% | 6.6% | 0.1% | |||||
| Former smoker | 25.4% | 35.8% | 21.1% | 22.1% | 32.7% | 30.7% | |||||
| Premature deaths | 2,462 | 9,948 | 1,366 | 395,699 | 604 | 4,139 | 1,294 | 170,737 | |||
| Life years lost | 75,336 | 137,063 | 755 | 4,103,572 | 20,578 | 67,093 | 756 | 1,918,021 | |||
| Scenario 1 | Smoker | 21.5% | 3.6% | 0.3% | 18.6% | 2.9% | 0.0% | ||||
| Former smoker | 25.4% | 32.5% | 17.9% | 22.1% | 29.4% | 25.9% | |||||
| Dual user | 0.0% | 2.7% | 0.1% | 0.0% | 2.5% | 0.1% | |||||
| FS-NVP | 0.0% | 3.3% | 0.6% | 0.0% | 2.9% | 0.9% | |||||
| FS-Former NVP | 0.0% | 2.1% | 2.3% | 0.0% | 1.8% | 3.2% | |||||
| Premature deaths | 2,462 | 8,887 | 1,357 | 374,229 | 5.4% | 604 | 3,470 | 1,286 | 158,314 | 7.3% | |
| Life years lost | 75,336 | 122,437 | 750 | 3,780,239 | 7.9% | 20,578 | 56,244 | 752 | 1,699,571 | 11.4% | |
| Scenario 2 | Premature deaths | 2,462 | 8,038 | 1,436 | 357,810 | 9.6% | 604 | 2,812 | 1,325 | 141,874 | 16.9% |
| Life years lost | 75,336 | 110,737 | 794 | 3,552,404 | 13.4% | 20,578 | 45,586 | 775 | 1,489,257 | 22.4% | |
| Scenario 3 | Premature deaths | 2,462 | 9,586 | 1,358 | 387,036 | 2.2% | 604 | 3,913 | 1,285 | 165,815 | 2.9% |
| Life years lost | 75,336 | 132,071 | 751 | 3,965,065 | 3.4% | 20,578 | 63,426 | 751 | 1,828,483 | 4.7% | |
| Scenario 4 | Premature deaths | 2,462 | 9,192 | 1,350 | 380,743 | 3.8% | 604 | 3,715 | 1,284 | 164,094 | 3.9% |
| Life years lost | 75,336 | 126,647 | 746 | 3,877,624 | 5.5% | 20,578 | 60,208 | 750 | 1,783,783 | 7.0% | |
| Scenario 5 | Premature deaths | 2,462 | 8,857 | 1,359 | 373,578 | 5.6% | 604 | 3,443 | 1,287 | 157,618 | 7.7% |
| Life years lost | 75,336 | 122,029 | 751 | 3,771,081 | 8.1% | 20,578 | 55,810 | 753 | 1,690,369 | 11.9% | |
| Scenario 6 | Never smoker | 53.1% | 55.6% | 78.8% | 59.3% | 60.4% | 70.4% | ||||
| Smoker | 21.5% | 2.7% | 0.3% | 18.6% | 1.7% | 0.0% | |||||
| Former smoker | 25.4% | 31.5% | 17.2% | 22.1% | 28.0% | 24.3% | |||||
| Dual user | 0.0% | 2.8% | 0.1% | 0.0% | 3.7% | 0.2% | |||||
| FS-NVP | 0.0% | 4.4% | 0.7% | 0.0% | 3.8% | 1.0% | |||||
| FS-Former NVP | 0.0% | 3.0% | 3.0% | 0.0% | 2.3% | 4.1% | |||||
| Premature deaths | 2,462 | 8,459 | 1,361 | 364,768 | 7.8% | 604 | 3,414 | 1,275 | 157,945 | 7.5% | |
| Life years lost | 75,336 | 116,548 | 752 | 3,635,555 | 11.4% | 20,578 | 55,333 | 746 | 1,676,018 | 12.6% | |
Notes: Scenario 1 uses the at least 25 of last 30-day vaping measure with NVP use risks at 5% and dual use risk at 80% those of smoking, assuming the same NVP and dual use rates by otherwise smokers and otherwise quitters with new NVP use remaining the same each year (4.0% male; 4.0% female) and most users become dual users (65% male; 65% female) and 5% of dual users transitioning exclusively to NVPs and 5% of NVP users quitting vaping. Scenario 2 assumes 20% NVP and dual use quit rate with parameters otherwise the same as Scenario 1. Scenario 3 assumes NVP use declines by 20% each year with parameters otherwise the same as Scenario 1. Scenario 4 assumes NVP/dual use mortality risk at 10%/100% those of cigarette with parameters otherwise the same as Scenario 1. Scenario 5 assumes the rate of smokers using NVP and dual use rate for otherwise quitters at half the rates of otherwise smokers with parameters otherwise the same as Scenario 1. Scenario 6 uses the at least 10 of last 30-day NVP use measure with new NVP use remaining the same each year (5.5% male; 6.5% female) and most users become dual users (55% male; 75% female), with parameters otherwise the same as Scenarios 1.
Cohort of Smokers Born in 1982
In the absence of vaping, male (female) smoking prevalence is initially 32.7% (24.5%) decreasing to 18.9% (14.8%) at age 50, and 7.4% (5.4%) at age 70. Annual LYL of current male (female) smokers increases to 90,372 (50,876) at age 65 and then decreases. Over the lifespan (ages 30–99) of the cohort, 390,632 (135,468) PDs and 4,577,882 (1,628,491) LYL are attributed to male (female) smoking.
Scenario 1 assumes applies 25-day vaping, transitions of 5% from dual and exclusive each year, and vaping risks at 5% of smoking. Exclusive smoking is reduced to 5.6% (6.7%) for males (females) by age 50, but health gains are partially offset through 8.1% (4.3%) dual use and 7.3% (4.6%) former smokers who vape. A cumulative total of 321,047 (109,364) PDs and 3,529,119 LYL (1,194,619 LYL) are projected for males (females). Compared to the No-NVP scenario, 69,585 (26,104) fewer PDs and 1,048,763 (433,872) fewer LYL are projected for males (females), representing 17.8% (19.3%) fewer PDs and 22.9% (26.6%) fewer LYL. On average, 1.5 (0.8) life-years are gained per male (female) smoker. With 20% of dual users quitting smoking and 20% of vapers quitting vaping each year (Scenario 2), 39.9% (45.9%) fewer LYL are projected for males (females). The absolute number of deaths is less for females than males, due to the lower initial smoking and smoking excess death rates, but the relative gains are comparable. With 20% of dual users quitting smoking and 20% of vapers quitting vaping each year (Scenario 2), the gains increase to 39.9% (45.9%) fewer LYL for males (females).
Modifying Scenario 1, the gain decreases to 8.7% (7.9%) fewer male (female) LYL with NVP use declining by 20% each year (Scenario 3), and to 18.0% (20.4%) fewer male (female) LYL with NVP mortality risks at 10% (Scenario 4). With overall and dual use rates by otherwise quitters at half the rates of otherwise smokers (Scenario 5), 23.2% (27.1%) fewer male (female) LYL are projected, only slightly lower than Scenario 1.
Using the 10-day vaping measure for Scenario 1, exclusive smoking is reduced to 3.3% (4.0%) for males (females) by age 50 (Scenario 6), with 22.9% (22.4%) fewer PDs and 29.5% (30.1%) fewer LYL and 1.9 (1.0) life-years saved. Compared to the estimates using the 25-day measure, there are 8.6% (4.7%) fewer LYLs. Commensurate changes to the 25-day measure are also projected when the transition and risk parameters are varied.
Cohort of Smokers Born in 1962
The 1962 birth cohort begins at age 50. With no NVPs, male (female) smoking prevalence is initially 21.5% (18.6%) decreasing to 8.2% (6.6%) at age 70. A cumulative total of 395,699 (170,737) PDs and 4,103,572 (1,918,21) LYL are attributed to smoking.
Scenario 1 applies the 25-day use measures for the 1962 cohort, but otherwise applies the same assumptions as Scenario 1 for the 1982 birth cohort. Exclusive smoking is reduced to 3.6% (2.9%) for males (females) by age 70, but health gains are partially offset through increased 2.7% (2.5%) dual use and 3.3% (2.9%) former smokers who vape. Compared to the No-NVP scenario, the model projects 5.4% (7.3%) fewer PDs and 7.9% (11.4%) fewer LYL, or 0.7 (0.5) life-years gained per smoker. The gains increase to 13.4% (22.4%) if 20% of dual users quit smoking and 20% of vapers quit vaping (Scenario 2).
Changing parameters in Scenario 1, LYL for males (females) are reduced by 3.4% (4.7%) with NVP use declining each year by 20% (Scenario 3), 5.5% (7.0%) with NVP mortality risks of 10%, (Scenario 4), 13.4% (11.4%) and 8.1% (11.9%) with vaping and dual use rates by otherwise quitters at half the rates of otherwise smokers (Scenario 5). Using the 10-day vaping measure with other parameters the same as in Scenario 1 (Scenario 6), exclusive smoking is reduced to 2.7% (1.7%) for males (females) by age 70, with 11.4% (12.6%) fewer LYL and 1.0 (0.6) life-years gained per smoker.
DISCUSSION
With NVP use, population health gains are projected in terms of in terms of fewer PDs and LYLs. These gains accrue as a result of replacing cigarette by NVP use or complete cessation from both NVPs and cigarettes. These gains outweigh any losses from dual or exclusive NVP use by the smaller percentage of smokers who have otherwise quit smoking cigarettes. While other studies (13–21) have found gains through cessation, we applied a cohort approach and considered a wide range of plausible parameters, due to the limited information available. While net population health gains were projected over plausible parameters, the extent of gains was sensitive to the choice of parameters.
Unlike previous analyses, our analysis specifically considers regular NVP use based on at least 25 of the last-30 days. Nevertheless, we did not incorporate duration of use. In developing improved models, it will be important to distinguish measures of use that are relatively stable over time, e.g., at least one year. We considered NVP use declining over time, but use may continue at relatively high rates or even increase with innovations in NVP products, such as the introduction of Juul.
Our focus was on NVP use within specific cohorts to highlight the importance of cohort-level analysis, but we assumed common age and cohort transitions. In developing better estimates of public health impacts, it will be important to consider age-specific and cohort-specific transitions to and from dual use and exclusive vaping (see Supplement). In gauging these transitions, sufficient time will be needed to allow for further transitions, e.g., transitions from dual use to exclusive vaping or no use may take longer than a year. However, short-term use may also result in smokers quitting both smoking and vaping. In addition, transitions may vary over time for individual cohorts. As individuals within a cohort age, their vaping patterns may depend not only on current use and public policies, but also previous use and policies (37, 52–55). Longitudinal studies will be needed to track these cohort-specific patterns.
We considered different use patterns and transitions by otherwise smokers and otherwise quitters. The offsetting impact of use by those who would otherwise quit plays less of a role at younger ages, because a relatively small percentage of smokers quit at these ages, but this distinction becomes more important at later ages when many smokers have tried quitting and failed. Most studies examining adult vaping have been cross-sectional, and do not distinguish reasons for use, types of use, degree of dependence and history of past quit attempts (2, 33). The distinction between otherwise smokers and quitters is central to distinguishing public health impacts (22).
This study focuses on transitions from smoking. Vaping may increase or reduce relapse back to smoking by former smokers and initiation into VNP and cigarette use smoking by never smokers (22). We also did not consider the use of other products tobacco products (e.g., smokeless tobacco, cigars or heated-tobacco products).
Finally, we considered the mortality risks of vaping relative to smoking. Regulations that reduce NVP risks can yield population health gains provided that they do not markedly discourage vaping. However, if vaping risks are found to be higher than our estimates, population health gains will be reduced. Further, we do not consider the impact of vaping on morbidity, health care, costs, work loss and quality of life. In addition, vaping may lead to acute injuries, such as accidental burns (56, 57). Finally, the impact of passive vaping and passive smoking should be considered (58).
Our approach to modeling focused on cohort-specific NVP use and the transitions from smoking and vaping. Among adult cohorts, we found substantial population health gains from NVP use leading to increased smoking cessation, resulting in reduced premature deaths and life years lost. To further refine this modeling approach, evaluations of the population impact of vaping will depend on well-validated measures of regular use as well as longitudinal evaluations of transitions to and from smoking and vaping.
Supplementary Material
ACKNOWLEDGMENTS:
We would like to thank Ron Borland for comments on an earlier draft.
FUNDING: Funding was received by Drs. Levy, Alberg and Cummings from the National Cancer Institute under grant P01CA200512.
Footnotes
Declaration of Interests: KMC has received funding from Pfizer to advise on ways to improve the delivery of tobacco cessation interventions to patients in health care settings He has also received payments as an expert witness in litigation against tobacco companies. Other authors have no conflicts of interest to declare.
References
- 1.Royal College of Physicians. Nicotine without smoke: Tobacco harm reduction, London: RCP; 2016. [Google Scholar]
- 2.Glasser AM, Collins L, Pearson JL, Abudayyeh H, Niaura RS, Abrams DB et al. Overview of Electronic Nicotine Delivery Systems: A Systematic Review, Am J Prev Med 2017: 52: e33–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shahab L, Goniewicz ML, Blount BC, Brown J, McNeill A, Alwis KU et al. Nicotine, Carcinogen, and Toxin Exposure in Long-Term E-Cigarette and Nicotine Replacement Therapy Users: A Cross-sectional Study, Ann Intern Med 2017: 166: 390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shahab L, Goniewicz ML, Blount BC, Brown J, West R. E-Cigarettes and Toxin Exposure, Ann Intern Med 2017: 167: 525–526. [DOI] [PubMed] [Google Scholar]
- 5.Farsalinos KE, Spyrou A, Tsimopoulou K, Stefopoulos C, Romagna G, Voudris V. Nicotine absorption from electronic cigarette use: comparison between first and new-generation devices, Sci Rep 2014: 4: 4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wagener TL, Floyd EL, Stepanov I, Driskill LM, Frank SG, Meier E. et al. Have combustible cigarettes met their match? The nicotine delivery profiles and harmful constituent exposures of second-generation and third-generation electronic cigarette users, Tob Control 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beard E, West R, Michie S, Brown J. Association between electronic cigarette use and changes in quit attempts, success of quit attempts, use of smoking cessation pharmacotherapy, and use of stop smoking services in England: time series analysis of population trends, BMJ 2016: 354: i4645. [DOI] [PubMed] [Google Scholar]
- 8.Caraballo RS, Shafer PR, Patel D, Davis KC, McAfee TA Quit Methods Used by US Adult Cigarette Smokers, 2014–2016, Prev Chronic Dis 2017: 14: E32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levy DT, Yuan Z, Luo Y, Abrams DB The Relationship of E-Cigarette Use to Cigarette Quit Attempts and Cessation: Insights From a Large, Nationally Representative U.S. Survey, Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel D, Davis KC, Cox S, Bradfield B, King BA, Shafer P. et al. Reasons for current E-cigarette use among U.S. adults, Prev Med 2016: 93: 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Register Federal. Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Regulations on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products; 2014. [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services F.a. D. A. Extension of Certain Tobacco Product Compliance Deadlines Related to the Final Deeming Rule: Guidance for Industry. In: Products C.f. T., editor, Washington DC; 2017. [Google Scholar]
- 13.Cherng ST, Tam J, Christine PJ, Meza R. Modeling the Effects of E-Cigarettes on Smoking Behavior: Implications for Future Adult Smoking Prevalence, Epidemiology 2016: 27(6): 819–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobb CO, Villanti AC, Graham AL, Pearson JL, Glasser AM, Rath JM et al. Markov Modeling to Estimate the Population Impact of Emerging Tobacco Products: A Proof-of-Concept Study, Tobacco Regulatory Science 2015: 1: 129–141. [Google Scholar]
- 15.Kalkhoran S, Glantz SA Modeling the Health Effects of Expanding e-Cigarette Sales in the United States and United Kingdom: A Monte Carlo Analysis, JAMA internal medicine 2015: 175: 1671–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bachand AM, Sulsky SI A dynamic population model for estimating all-cause mortality due to lifetime exposure history, Regul Toxicol Pharmacol 2013: 67: 246–251. [DOI] [PubMed] [Google Scholar]
- 17.Chen X, Yu B, Chen DG Probabilistic Discrete Event Systems Modeling of Nonlinear Transitions between Electronic and Combustible Cigarette Smoking with the 2014 National Youth Tobacco Survey Data, Nonlinear Dynamics Psychol Life Sci 2018: 22: 289–312. [PubMed] [Google Scholar]
- 18.Levy DT, Borland R, Villanti AC, Niaura R, Yuan Z, Zhang Y. et al. The Application of a Decision-Theoretic Model to Estimate the Public Health Impact of Vaporized Nicotine Product Initiation in the United States, Nicotine Tob Res 2017: 19: 149–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bachand AM, Sulsky SI, Curtin GM Assessing the Likelihood and Magnitude of a Population Health Benefit Following the Market Introduction of a Modified-Risk Tobacco Product: Enhancements to the Dynamic Population Modeler, DPM(+1), Risk Anal 2018: 38: 151–162. [DOI] [PubMed] [Google Scholar]
- 20.Poland B, Teischinger F. Population Modeling of Modified Risk Tobacco Products Accounting for Smoking Reduction and Gradual Transitions of Relative Risk, Nicotine Tob Res 2017: 19: 1277–1283. [DOI] [PubMed] [Google Scholar]
- 21.Soneji SS, Sung HY, Primack BA, Pierce JP, Sargent JD Quantifying population-level health benefits and harms of e-cigarette use in the United States, PLoS One 2018: 13: e0193328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levy DT, Cummings KM, Villanti AC, Niaura R, Abrams DB, Fong GT et al. A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products, Addiction (Abingdon, England) 2017: 112: 8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.King BA, Patel R, Nguyen K, Dube SR Trends in awareness and use of electronic cigarettes among U.S. adults, 2010–2013, Nicotine Tob Res 2014: [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. In: U.S. Department of Health and Human Services C. f. D. C. a. P., National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, editor, Atlanta, GA; 2014. [Google Scholar]
- 25.U.S. DHHS. The Health Benefits of Smoking Cessation: a report of the Surgeon General, Atlanta Georgia: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Office on Smoking and Health; 1990. [Google Scholar]
- 26.Holford TR, Levy DT, McKay LA, Clarke L, Racine B, Meza R. et al. Patterns of Birth Cohort–Specific Smoking Histories, 1965–2009, American Journal of Preventive Medicine 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pirie K, Peto R, Reeves GK, Green J, Beral V, Million Women Study C. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK, Lancet 2013: 381: 133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levy DT, Yuan Z, Li Y. The Prevalence and Characteristics of E-Cigarette Users in the U.S, International journal of environmental research and public health 2017: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park SH, Duncan DT, Shahawy OE, Lee L, Shearston JA, Tamura K. et al. Characteristics of Adults Who Switched From Cigarette Smoking to E-cigarettes, Am J Prev Med 2017: 53: 652–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lechner WV, Meier E, Wiener JL, Grant DM, Gilmore J, Judah MR et al. The comparative efficacy of first- versus second-generation electronic cigarettes in reducing symptoms of nicotine withdrawal, Addiction (Abingdon, England) 2015: 110: 862–867. [DOI] [PubMed] [Google Scholar]
- 31.Wagener TL, Floyd EL, Stepanov I, Driskill LM, Frank SG, Meier E. et al. Have combustible cigarettes met their match? The nicotine delivery profiles and harmful constituent exposures of second-generation and third-generation electronic cigarette users, Tob Control 2017: 26: e23–e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coleman B, Rostron B, Johnson SE, Persoskie A, Pearson J, Stanton C. et al. Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) Study, Waves 1 and 2 (2013–2015), Tob Control 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Villanti AC, Feirman SP, Niaura RS, Pearson JL, Glasser AM, Collins LK et al. How do we determine the impact of e-cigarettes on cigarette smoking cessation or reduction? Review and recommendations for answering the research question with scientific rigor, Addiction (Abingdon, England) 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rahman MA, Hann N, Wilson A, Mnatzaganian G, Worrall-Carter L. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis, PLoS One 2015: 10: e0122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Polosa R, Caponnetto P, Cibella F, Le-Houezec J. Quit and smoking reduction rates in vape shop consumers: a prospective 12-month survey, Int J Environ Res Public Health 2015: 12: 3428–3438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Polosa R, Caponnetto P, Maglia M, Morjaria JB, Russo C. Success rates with nicotine personal vaporizers: a prospective 6-month pilot study of smokers not intending to quit, BMC Public Health 2014: 14: 1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nayak P, Pechacek TF, Weaver SR, Eriksen MP Electronic nicotine delivery system dual use and intention to quit smoking: Will the socioeconomic gap in smoking get greater?, Addict Behav 2016: 61: 112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simonavicius E, McNeill A, Arnott D, Brose LS What factors are associated with current smokers using or stopping e-cigarette use?, Drug and alcohol dependence 2017: 173: 139–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Etter JF, Bullen C. A longitudinal study of electronic cigarette users, Addict Behav 2014: 39: 491–494. [DOI] [PubMed] [Google Scholar]
- 40.Caponnetto P, Campagna D, Cibella F, Morjaria JB, Caruso M, Russo C. et al. EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study, PLoS One 2013: 8: e66317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fagerstrom K, Eissenberg T. Dependence on tobacco and nicotine products: a case for product-specific assessment, Nicotine Tob Res 2012: 14: 1382–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu G, Wasserman E, Kong L, Foulds J. A comparison of nicotine dependence among exclusive E-cigarette and cigarette users in the PATH study, Preventive medicine 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.US Census Bureau. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States, States, and Puerto Rico Commonwealth: April 1, 2010 to July 1, 2012; 2013.
- 44.Holford TR, Meza R, Warner KE, Meernik C, Jeon J, Moolgavkar SH et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964–2012, JAMA 2014: 311: 164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J. et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes, Tob Control 2014: 23: 133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nutt DJ, Phillips LD, Balfour D, Curran HV, Dockrell M, Foulds J. et al. Estimating the harms of nicotine-containing products using the MCDA approach, European addiction research 2014: 20: 218–225. [DOI] [PubMed] [Google Scholar]
- 47.Hecht SS, Carmella SG, Kotandeniya D, Pillsbury ME, Chen M, Ransom BW et al. Evaluation of Toxicant and Carcinogen Metabolites in the Urine of e-Cigarette Users Versus Cigarette Smokers, Nicotine Tob Res 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee PN Health risks related to dual use of cigarettes and snus - a systematic review, Regul Toxicol Pharmacol 2014: 69: 125–134. [DOI] [PubMed] [Google Scholar]
- 49.Huang J, Kim Y, Vera L, Emery SL Electronic Cigarettes Among Priority Populations: Role of Smoking Cessation and Tobacco Control Policies, Am J Prev Med 2016: 50: 199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pearson JL, Stanton CA, Cha S, Niaura RS, Luta G, Graham AL E-Cigarettes and Smoking Cessation: Insights and Cautions From a Secondary Analysis of Data From a Study of Online Treatment-Seeking Smokers, Nicotine Tob Res 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys, BMJ 2017: 358: j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abrams DB Promise and peril of e-cigarettes: can disruptive technology make cigarettes obsolete?, JAMA 2014: 311: 135–136. [DOI] [PubMed] [Google Scholar]
- 53.Branston JR, Sweanor D. Big tobacco, E-cigarettes, and a road to the smoking endgame, Int J Drug Policy 2016: 29: 14–18. [DOI] [PubMed] [Google Scholar]
- 54.Kozlowski LT, Sweanor D. Withholding differential risk information on legal consumer nicotine/tobacco products: The public health ethics of health information quarantines, Int J Drug Policy 2016: 32: 17–23. [DOI] [PubMed] [Google Scholar]
- 55.Stimson GV, Thom B, Costall P. Disruptive innovations: The rise of the electronic cigarette, Int J Drug Policy 2014. [DOI] [PubMed] [Google Scholar]
- 56.Corey CG, Chang JT, Rostron BL Electronic nicotine delivery system (ENDS) battery-related burns presenting to US emergency departments, 2016, Inj Epidemiol 2018: 5: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Treitl D, Solomon R, Davare DL, Sanchez R, Kiffin C. Full and Partial Thickness Burns from Spontaneous Combustion of E-Cigarette Lithium-Ion Batteries with Review of Literature, J Emerg Med 2017: 53: 121–125. [DOI] [PubMed] [Google Scholar]
- 58.Torjesen I. E-cigarette vapour could damage health of non-smokers, BMJ 2014: 349: g6882. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.