New York City has been the epicenter for SARS-CoV-2 infections in the USA. Although symptomatic infection rates continue to rise, the presence of asymptomatic infection, though not well characterized, likely contributes to the spread of infection.2,3 To minimize transmission of SARS-CoV-2, many hospital activities including elective surgeries have paused under governmental orders. However, timely surgery remains a necessity for maximizing survival in some cancer patients.4 Unfortunately, in patients with active COVID-19, cancer surgery may be associated with higher morbidity and mortality5 and create risk for the transmission of infection to members of the perioperative team. The appropriate goal is to balance performance of essential cancer surgery with protecting the health and safety of patients and healthcare workers.
In an effort to minimize the risk of conducting surgery on patients with active COVID-19, we initiated a protocol for preoperative symptom assessment of patients 48 hours before surgery and again on the day of surgery, with delay of surgery in patients responding affirmatively. Unfortunately, patients were still diagnosed with symptomatic COVID-19 in the immediate postoperative period. As this might reflect asymptomatic or pre-symptomatic SARS-CoV-2 infection at the time of surgery, and as an added measure to enhance the safety of our patients and perioperative staff, we initiated preoperative virologic testing of all patients scheduled for surgery.
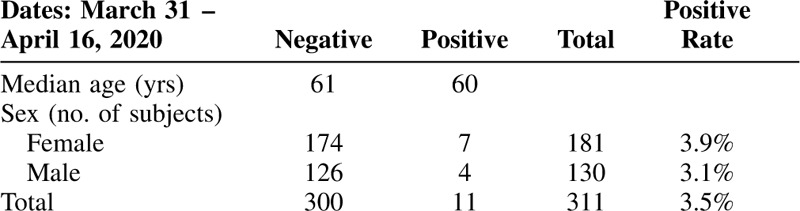
Patients who denied recent COVID-19-like symptoms 48 hours before surgery were scheduled for SARS-CoV-2 nasopharyngeal testing 1–2 days before surgery. Between March 31 and April 16, 2020, 3.5% of asymptomatic patients tested positive for SARS-CoV-2 (Table 1). Virus-positive patients had surgery postponed and were rescheduled for retesting in 3 weeks. To date, none of these patients have gone on to develop symptomatic infection. In our small series there was 1 potential false negative patient, who tested negative for SARS-CoV-2 before surgery but positive on postoperative day 1. Whether this represented a technical aspect of testing or whether the patient's preoperative test occurred before manifesting detectable virus is uncertain.
TABLE 1.
Results of Preoperative Testing for SARS-CoV-2
There is a real risk of asymptomatic SARS-CoV-2 infection among patients scheduled for essential cancer surgery in a region with a high prevalence of symptomatic infection. A protocol of preoperative screening and SARS-CoV-2 testing can substantially, but not completely, reduce the risks of operating on asymptomatic patients. Such a protocol may improve the safety of cancer patients and hospital staff.
Footnotes
1The Covid19 Subcommittee of the Operating Room Executive Committee: Laura Ardizzone, Thomas Barber, Jeffrey Drebin, Gregory Fischer, Elizabeth Jewell, Vincent Laudone, Marcia Levine, Jeannine Linder, Brett Simon, Christopher Stromblad, Viviane Tabar, Martin Weiser, and Shok-Jean Yee.
The authors declare no conflicts of interest.
REFERENCES
- 1. Covid-19 Sub-Committee of the Operating Room Executive Committee, Laura Ardizzone, Thomas Barber, Jeffrey Drebin, Gregory Fischer, Elizabeth Jewell, Vincent Laudone, Marcia Levine, Jeannine Linder, Brett Simon, Christopher Stromblad, Viviane Tabar, Martin Weiser, and Shok-Jean Yee. [Google Scholar]
- 2.Bai Y, Yao L, Wei T. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020; 323:1406–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Song JY, Yun JG, Noh JY, et al. Covid-19 in South Korea – challenges of subclinical manifestations. N Engl J Med 2020; 382:1858–1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turaga K, Girotra S. Are we harming cancer patients by delaying their cancer surgery during the COVID-19 pandemic? Ann Surg 2020; (Published on-line ahead of print). Available at: https://journals.lww.com/annalsofsurgery/Documents/Are%20we%20harming%20cancer%20patients.pdf. Accessed May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laing W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet 2020; 21:335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]


