Abstract
Objectives:
Our study aims to explore the differential impact of this pandemic on clinical presentations and outcomes in African Americans (AAs) compared to white patients.
Background:
AAs have worse outcomes compared to whites while facing heart diseases, stroke, cancer, asthma, influenza and pneumonia, diabetes, and HIV/AIDS. However, there is no current study to show the impact of COVID-19 pandemic on the AA communities.
Methods:
This is a retrospective study that included patients with laboratory-confirmed COVID-19 from 2 tertiary centers in New Orleans, LA. Clinical and laboratory data were collected. Multivariate analyses were performed to identify the risk factors associated with adverse events.
Results:
A total of 157 patients were identified. Of these, 134 (77%) were AAs, whereas 23.4% of patients were Whites. Interestingly, AA were younger, with a mean age of 63 ± 13.4 compared to 75.7 ± 23 years in Whites (P < 0.001). Thirty-seven patients presented with no insurance, and 34 of them were AA. SOFA Score was significantly higher in AA (2.57 ± 2.1) compared to White patients (1.69 ± 1.7), P = 0.041. Elevated SOFA score was associated with higher odds for intubation (odds ratio = 1.6, 95% confidence interval = 1.32–1.93, P < 0.001). AA had more prolonged length of hospital stays (11.1 ± 13.4 days vs 7.7 ± 23 days) than in Whites, P = 0.01.
Conclusion:
AAs present with more advanced disease and eventually have worse outcomes from COVID-19 infection. Future studies are warranted for further investigations that should impact the need for providing additional resources to the AA communities.
Keywords: African Americans, Corona Virus, COVID, outcomes, pandemic, racial disparities
In December 2019, a novel virus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified as a causative agent for a cluster of pneumonia detected in Wuhan City, China.1–3 In January 2020, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19), a global pandemic and a health emergency.4
The number of COVID-19 cases dramatically increased in the United States since the first case report on January 22, 2020. By May 22, 2020, the Centers for Disease Control and Prevention (CDC) reported that the total number of confirmed cases was >1,571,617, and the total number of deaths was >94,150.5 The incidence rate in Louisiana State was considered the highest per capita, with >21,000 cases reported. According to published data from the first month of the US epidemic released by the CDC, about 1 in 3 people who become infected were African American (AA). Considering that AAs constitute 13% of the US population, they were overrepresented (33%) among hospitalized COVID-19 patients in 14 states (California, Colorado, Connecticut, Georgia, Iowa, Maryland, Michigan, Minnesota, New Mexico, New York, Ohio, Oregon, Tennessee, and Utah).6
Here, in Louisiana (LA), 70% of COVID-19 related mortalities were in AAs, although AAs represent only 32% of the state population.6 Our study is the first to unveil the impact of racial disparity on outcomes in patients with COVID-19 who were admitted to 2 tertiary centers in New Orleans, LA, which is a hot epicenter for COVID-19.
METHODS
This is a retrospective study that was performed after acquiring Tulane University institutional review board (IRB) approval. Data were collected on COVID-19-positive patients, who had been admitted from March 1, 2020 to April 11, 2020 to Tulane medical center (TMC) and University Medical Center, New Orleans (UMC).
Epidemiology, demographics, medical history, underlying comorbidities, clinical, laboratory, and outcome data were extracted from the electronic medical records using a standardized data collection. Sequential Organ Failure Assessment (SOFA) score was calculated. The data were reviewed by our team of physicians including attendings, resident physicians, and post-doctoral fellows.
Data management was performed using SAS v9.4, whereas SPSS v26.0 was used for statistical analysis. χ2 and Fisher exact tests were applied for categorical variables. Student t and Mann-Whitney U tests were used for continuous variables. Two-sided P-value was set to be significant at <0.05. Multivariate Cox hazards regression analysis was used to identify predictor risk factors for mortality. Binary logistic regression analysis was used to detect independent variables for prolonged length of stay (≥7 days vs <7 days).
RESULTS
A total of 157 patients (77 men and 80 women) were identified. Of these, 134 (77%) were AAs, whereas 23.4% of patients were Whites. Interestingly, AAs were younger, with a mean age of 63 ± 13.4 compared to 75.7 ± 23 years in Whites (P < 0.001) (Table 1).
TABLE 1.
Characteristics of COVID-19 Patients
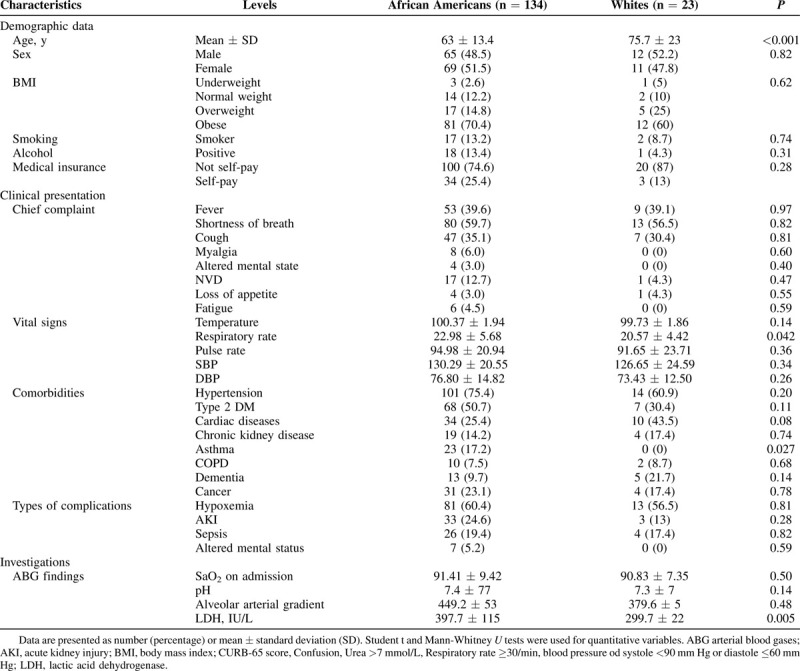
Figure 1 showed that AAs have significantly higher hospital admissions, despite that AAs represent approximately half of New Orleans’ population.5 Thirty-seven patients presented with no insurance and 34 (91.8%) of these patients were AAs (Fig. 2).
FIGURE 1.
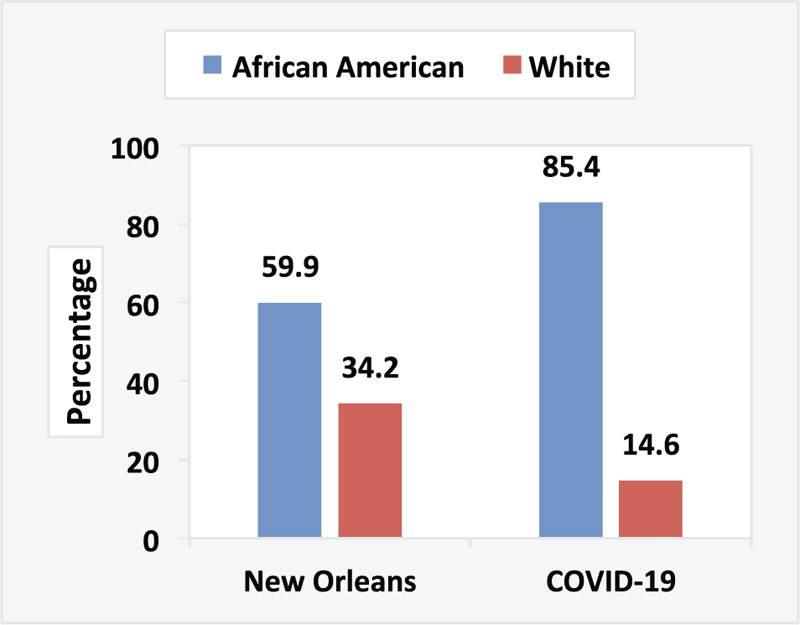
Differences in percentages between AA versus whites in state census and hospital COVID-19 infection rate in New Orleans.
FIGURE 2.
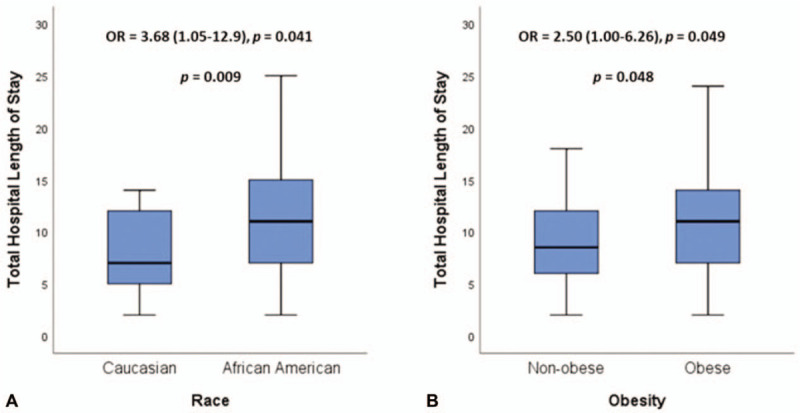
(A) Racial disparity in total hospital length of stay. (B) Influence of obesity on in total hospital length of stay.
Interestingly, hypertension (N = 115, 27%), and diabetes mellitus (N = 75, 18%) were the most frequent comorbidities. Asthma was significantly higher in AAs (N = 23, 17.2%) compared to none in White (P = 0.027). Higher rate of obesity was identified in AAs (N = 81, 70.4%) compared to whites (N = 12, 60%) (Table 1).
On examining the laboratory marker, lactate dehydrogenase (LDH) values were higher in AAs (397.7 ± 115 IU/L) than White (299.7 ± 22, P = 0.005), SOFA score was significantly higher in AAs (2.57 ± 2.1) compared to White patients (1.69 ± 1.7, P = 0.041), elevated SOFA score was associated with higher odds for intubation [odds ratio (OR) = 1.6, 95% confidence interval (CI) = 1.32–1.93, P < 0.001; Table 1].
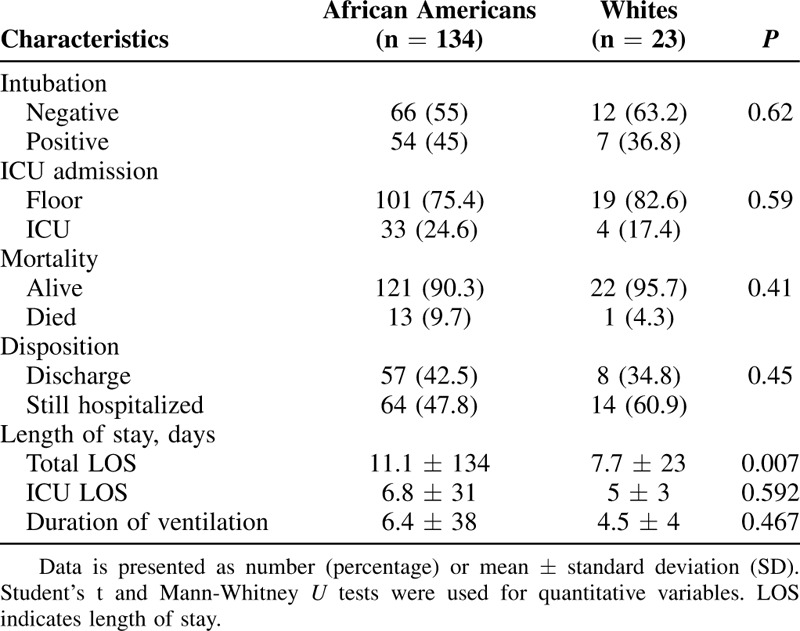
AAs had longer length of hospitalizations (mean and standard deviation of 11.1 ± 13.4 days) compared to 7.7 ± 23 days in Whites (OR = 3.68, 95% CI = 1.05–12.90, P = 0.041). Obesity was also another risk factor for longer hospitalization (OR = 2.50, 95% CI = 1.004–6.26). Mortality rate was much higher in AAs compared to whites as 13 of 14 (92.8%) COVID-19-positive patient died were AAs. AAs required more intensive care unit (ICU) admissions (14.1%) compared to 7.1% in Whites (Table 2). Of the study population, 65 (41.4%) were discharged, 14 (8.9%) were deceased, whereas 78 (49.7%) were still hospitalized (Table 3).
TABLE 2.
Predictors of Longer Hospital Stay
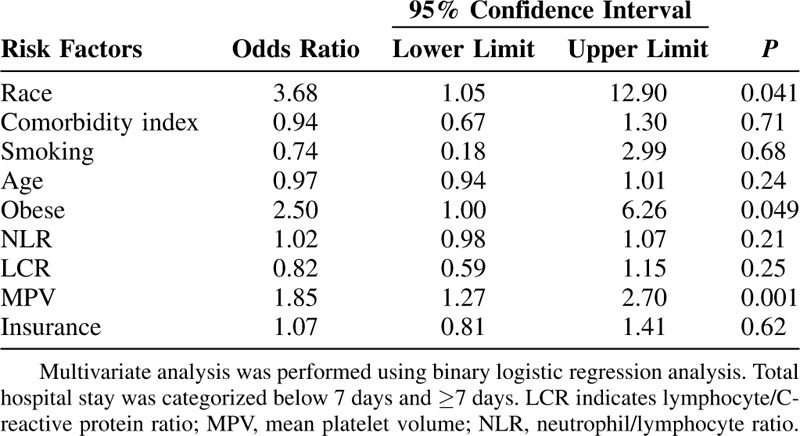
TABLE 3.
Outcomes of COVID-19 Disease
DISCUSSION
Louisiana ranked as one of the top 10 states with COVID-related deaths in the United States.6 AAs represent >30% of our state's residents.7 Nevertheless, we are showing a higher rate of COVID-19 admissions from our AA community, which highlights the higher risk of advanced disease in AAs. High blood pressure and diabetes are both risk factors that have been previously recognized for their association with severe COVID-19 infection. AAs have a higher prevalence of both those comorbidities which could explain in part the higher incidence of COVID-19.8–11
In non-COVID patients, Andre et al assessed daily repeating of SOFA score in patients who were admitted to the ICU. They showed that patients who died tended to be older (median age 74; P < 0.01) with a lower risk for AAs (9.4%; P < 0.01), and maximum SOFA score of 9 (P < 0.001).12 For the first time, our present study showed that AAs diagnosed with COVID-19 had worse outcomes correlated with SOFA scores despite that these patients presented at younger age compared to Whites.
The US Department of Health and Human Services Office of Minority Health reported a higher rate of uninsured AAs than whites. Additionally, unemployment rate for blacks was double that of non-Hispanic whites. The death rate for AAs is generally higher than whites for heart diseases, stroke, cancer, asthma, influenza and pneumonia, diabetes, HIV/AIDS, and homicide.13
AAs have the highest rates of obesity or being overweight compared to other racial groups in the United States.14 That data are consistent with our study that showed AAs also had a high rate of obesity, and herein we found that obese patients are already at high risk for severe complications of COVID-19. Obesity is associated with decreased expiratory reserve volume, functional capacity, and respiratory system compliance. In patients with increased abdominal obesity, pulmonary function is further compromised in supine patients by decreased diaphragmatic excursion, making ventilation more difficult.15
In a recent report, data were analyzed to examine the association between the coronavirus propagation, social distancing, and socioeconomic factors, The analysis showed that as the pandemic wore on, AAs were less able to stay at home and socially distance. In turn, AAs were at a higher risk of contracting and spreading COVID-19. Social distancing metrics enable us to understand how AAs have become a population with such an outsized number of COVID-19 infections and deaths. But it is crucial to note that social distancing might not be a choice for low-income AA because of work demands, transportation needs, and housing settings. The author recommends more educational program implementation should be well-established and applied immediately to raise the necessity of understanding of social distancing to limit the spread of the COVID-19, especially in AA.16
Our study adds observational data to the mounting evidence that AA are at elevated risk during the COVID-19 pandemic. Interestingly, 9.3% of New Orleans population has no insurance, but in our study 91.8% of the AAs admitted to the hospital had no insurance.7 Our study confirms the existence of significant AA in susceptibility to complications and the mortality rate. Health care workers and politicians should be aware of the impact of racial disparities during the COVID-19 pandemic. We believe these findings suggest the need to providing more resources of education and testing to the AA communities.
CONCLUSIONS
Health care workers and politicians should be aware of the effect of racial disparities during the COVID-19 pandemic. AAs are more likely to have a higher prevalence of comorbidities, which made them have more severe clinical outcomes, laboratory values (higher LDH), higher rates of ICU admissions, and higher rate of mortality. Additionally, they have higher rates of having no insurance which is usually associated with worse outcomes.
Footnotes
The authors declare there are no conflicts of interest.
REFERENCES
- 1.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; doi:10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol 2020; doi:10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; doi:10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. (2020). Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance, 28 January 2020. World Health Organization. https://apps.who.int/iris/handle/10665/330893. [Google Scholar]
- 5. Cases, Data, and Surveillance | CDC. (n.d.). Retrieved May 22, 2020, from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/index.html. [Google Scholar]
- 6. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 - COVID-NET, 14 States, March 1–30, 2020. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e3.htm#F1_down. Published April 8, 2020. Accessed April 12, 2020. [Google Scholar]
- 7. U.S. Census Bureau QuickFacts: Louisiana. Census Bureau QuickFacts. Available at: https://www.census.gov/quickfacts/LA. Accessed May 17, 2020. [Google Scholar]
- 8.Zhang J, jin, Dong X, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy Eur J Allergy Clin Immunol 2020; doi:10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 9.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020; doi:10.1056/nejmoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCormack S, Grant SFA. Genetics of obesity and type 2 diabetes in African Americans. J Obes 2013; 2013:396416.doi:10.1155/2013/396416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zilbermint M, Hannah-Shmouni F, Stratakis CA. Genetics of hypertension in African Americans and others of African descent. Int J Mol Sci 2019; 20: doi:10.3390/ijms20051081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holder AL, Overton E, Lyu P, et al. Serial daily organ failure assessment beyond ICU day 5 does not independently add precision to ICU risk-of-death prediction. Crit Care Med 2017; 45:2014–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Office of Minority Health. Black/African American - The Office of Minority Health. Available at: https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=61. Accessed May 17, 2020. [Google Scholar]
- 14. Office of Minority Health. Obesity and African Americans - The Office of Minority Health. Available at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=25. Accessed April 12, 2020. [Google Scholar]
- 15.De Jong A, Chanques G, Jaber S. Mechanical ventilation in obese ICU patients: from intubation to extubation. Crit Care 2017; 21:63.doi:10.1186/s13054-017-1641-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Henry-Nickie M, Hudak J. Social distancing in Black and white neighborhoods in Detroit: A data-driven look at vulnerable communities. Brookings. Available at: https://www.brookings.edu/blog/fixgov/2020/05/19/social-distancing-in-black-and-white-neighborhoods-in-detroit-a-data-driven-look-at-vulnerable-communities/. Published May 20, 2020. Accessed May 22, 2020. [Google Scholar]


