Abstract
Purpose
To describe our methodology for implementing synchronous telemedicine during the 2019 novel coronavirus (COVID-19) pandemic.
Methods
A retrospective review of outpatient records at a single children's hospital from March 21 to April 10, 2020, was carried out to determine the outcome of already-scheduled face-to-face outpatient appointments. The week leading up to the March 21, all appointments in the study period were categorized as follows: (1) requiring an in-person visit, (2) face-to-face visit that could be postponed, and (3) consultation required but could be virtual. Teams of administrators, schedulers, and ophthalmic technicians used defined scripts and standardized emails to communicate results of categorization to patients. Flowcharts were devised to schedule and implement telemedicine visits. Informational videos were made accessible on social media to prepare patients for the telemedicine experience. Simultaneously our children's hospital launched a pediatric on-demand e-consult service, the data analytics of which could be used to determine how many visits were eye related.
Results
A total of 237 virtual ophthalmology consult visits were offered during the study period: 212 were scheduled, and 206 were completed, of which 43 were with new patients and 163 with returning patients. Following the initial virtual visit, another was required on average in 4 weeks by 21 patients; in-person follow-up was required for 170 patients on average 4.6 months after the initial virtual visit. None needed review within 72 hours. The pediatric on-demand service completed 290 visits, of which 25 had eye complaints.
Conclusions
With proper materials, technology, and staffing, a telemedicine strategy based on three patient categories can be rapidly implemented to provide continued patient care during pandemic conditions. In our study cohort, the scheduled clinic e-visits had a low no-show rate (3%), and 8% of the on-demand virtual access for pediatric care was eye related.
COVID-19 is a novel coronavirus with efficient transmission and a high mortality.1 The World Health Organization (WHO) designated it an ongoing pandemic on March 11, 2020.2 The only effective control strategy to date is to decrease transmission. National lockdowns have been enforced globally, and physical distancing is being universally recommended. The pandemic has profoundly affected the practice of medicine.
On February 29, 2020, the Centers for Disease Control and Prevention (CDC) recommended rescheduling elective surgeries as necessary and exploring alternatives to in-person hospital visits.3 The American Academy of Ophthalmology (AAO) issued a statement strongly recommending that all ophthalmologists provide only urgent or emergent care, which was endorsed by the American Association for Pediatric Ophthalmology and Strabismus (AAPOS). The statement includes both office-based care and surgical care. The AAO recognized that “urgency” is determined by physician judgment and must always take into account individual patient medical and social circumstances.4
Epidemiological models have predicted that the pandemic will continue for 6-18 months, with longer predictions associated with decreased mortality. This seemingly counterintuitive modeling takes into account limitations in critical care resources5 and attempts to “flatten the curve” until the much-anticipated vaccine is available to the general population. The stopgap strategies that pediatric ophthalmologists use to continue to care for patients through this period are evolving by the day. Considering the likely duration of the social distancing measures, it is important to develop alternative methods of practicing medicine in general and ophthalmology in particular.
Telemedicine is the clearest path forward during this time, reducing the risk of exposure for both patient and provider. Telemedicine has been in existence for several years in the field of ophthalmology but has largely been used as a supplemental practice tool for outreach purposes. Previously mired in uncertain regulations and reimbursement policies, pediatric telemedicine has seen a slow uptake in the past few years.6 Current events, however, have thrust it to the forefront of clinical ophthalmology. The purpose of this study is to describe the experience of a hospital-based, university-affiliated pediatric ophthalmology program in implementing the above-mentioned guidelines in light of current information about COVID-19.
Ophthalmology relies heavily on objective assessments through examination techniques and investigations. Some techniques lend themselves to widely available smartphone and web-based technology. These include visual acuity examinations, contrast testing, color vision testing, and gaze photography. Numerous applications are available for these tests online; unfortunately, most lack standardization. Sophisticated examinations, such as retinal examination must rely on specialized equipment and currently, trained personnel to obtain images in a standardized manner. A multitude of smartphone extensions have been developed to obtain retinal imaging and are being systematically evaluated.7 These are crucial for increasing access. Some of these devices have already demonstrated promising early results, specifically for diabetic retinopathy.8
With rapid technological advances, software-based ophthalmic applications have burgeoned in recent years. These applications will enhance the practice of ophthalmology, but they must be rigorously tested before being adopted for widespread use.9 A recent workshop explored issues of safety, efficacy, cybersecurity, privacy, and interoperability that must be incorporated into the approval process for ophthalmic software.10
Telemedicine can be delivered in an asynchronous or synchronous manner.11 Asynchronous telemedicine is defined as a “term describing store-and-forward transmission of medical images and/or data because the data transfer takes place over a period of time, and typically in separate time frames” and has been previously used for intervisit care.11 In pediatric ophthalmology it has been the mainstay for retinopathy of prematurity screening.11, 12, 13, 14, 15 Synchronous telemedicine is delivered in real-time with the intention of replacing or safely delaying in-person visit(s). Synchronous telemedicine can be further divided into encounters scheduled for the provider by a scheduler, with the patient being given specific instructions as to how to join a virtual clinic room at a given time or can be triggered by a patient wanting advice or an examination as the need arises, with a provider team available 24/7.
Subjects and Methods
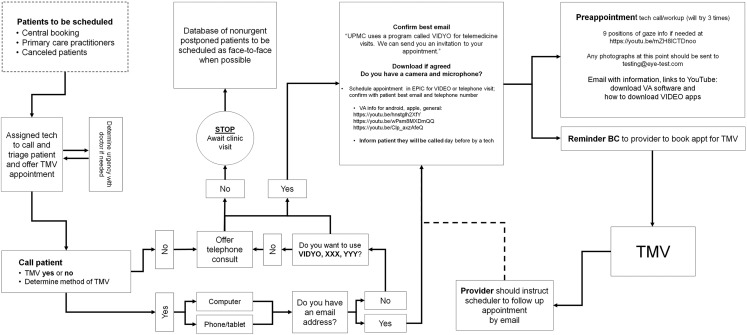
We retrospectively investigated the outcomes of already-scheduled face-to-face encounters between March 21, 2020, and April 10, 2020, and the actions taken during the week leading up to March 21, when we devised our workflow for a routine telemedicine protocol (Figure 1 ). The medical records of patients to be seen at the Ophthalmology Department of UPMC Children's Hospital of Pittsburgh between March 21 and April 10 were reviewed by a provider (MP, KKN, PP, EM, CL EK), and all visits in the study period were categorized as follows: (1) requiring an in-person visit, (2) face-to-face visit that could be postponed, and (3) consultation required but could be virtual. In the case of children who needed an in-person visit, it would be advised that they be accompanied by the healthiest family member (ie, <65 years or any age with no comorbidities as defined by the CDC). If these patients refused or canceled, a virtual visit was offered.
Fig 1.
Ophthalmology telemedicine workflow. TMV, telemedicine visit; BC, blind copy.
Teams of administrators, schedulers, and ophthalmic technicians used defined scripts and standardized emails to communicate results of categorization to patients. Flowcharts were devised to schedule and implement telemedicine visits.
We instituted the protocol on March 19, 2020, and monitored results of virtual visits from March 21 to April 10. To set up a virtual visit, the following procedure was followed. All eligible patients were offered the option for video visit first. If they did not have the means or declined the video visit, they were then offered a scheduled telephone visit with their provider. If the patient declined both, they were then offered a delayed scheduled in-person visit, but only after the ophthalmologist confirmed that it was safe to do so. To ensure that patients were consistently informed that their physician deemed the visit to be necessary and that it could be completed via telemedicine, a standardized script was used by schedulers.
Three teams were established to facilitate the telemedicine visit—administrators, schedulers, and ophthalmic technicians. Administrators provided patient information to the physician and assisted with cohorting patients. Schedulers spoke to parents or caregivers about the telemedicine visit using a standardized script and sent an email with details and instructions; they also scheduled a phone call with the technician within a set time frame (eg, 9 a.m.-11 a.m., 11 a.m.-1 p.m., etc) a day prior to their telemedicine visit. The ophthalmic technicians called the parents within the set time frame to obtain medical information and histories and to ensure that vision testing was performed. They would also provide troubleshooting advice on using the applications.
A standardized email was constructed to send to all patients after the conclusion of their scheduling phone call, should they accept the telemedicine visit. The email provided details regarding their scheduled appointment and provider. It also included links to available visual acuity testing applications and instructions on how to use them. Our group identified a free mobile application (https://apps.apple.com/us/app/visual-acuity-charts/id1442509969), with accurate calibrations, conventional optotypes, and standard notations for results, but made it clear that parents were free to choose any application they wished as long as they informed us which testing method they used. Videos explaining how to use these applications correctly were uploaded to YouTube by our team (https://youtu.be/hnstglh2XfY, https://youtu.be/wPsm8MXDmQQ, https://youtu.be/Clp_axzAfeQ).
We used two platforms for most of our visits: VIDYO and Doxy.me. We also informed our patients that Skype and FaceTime could be used if necessary but also ensured an up-to-date telephone number was available in case all web-based systems failed. Once the background work was completed by our administrative staff, the providers carried out the virtual visit. A standardized phrase for notes was created to ensure that documentation conveyed that the encounter took place virtually.
For urgent care visits, our children's hospital implemented a 24/7 patient-driven virtual care service on March 27, 2020. This was attended by emergency room providers. Ophthalmic emergencies were also evaluated by these providers and referred to ophthalmology if needed. Subsequently the above algorithm was followed for these visits.
Results
Using these guidelines, virtual visits were offered to 237 patients. Of these, 25 patients declined, and 212 visits were scheduled. Of the scheduled visits, our service was able to complete 206 (97%) between March 21 and April 10, 2020 with 7 providers. Of these, 43 were new patient visits and 163 were follow-up visits. Following the initial virtual visit, 21 needed a virtual visit follow-up an average of 4 weeks later, and 170 needed an in-person visit an average of 4.6 months later; none needed to be seen within 72 hours. The date of the scheduled repeat virtual visit and scheduled in person visit was determined at the time of the initial virtual visit.
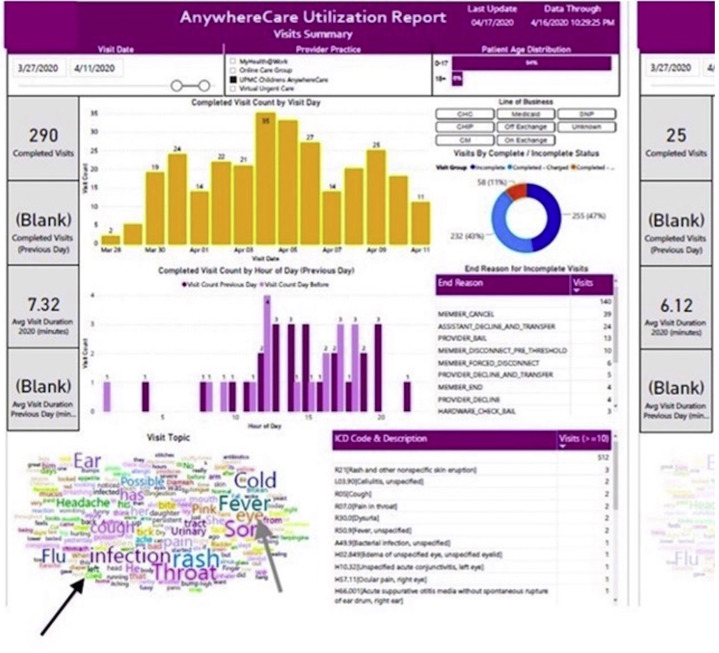
In the urgent care virtual platform, until April 11, there were 290 encounters for children between 0-17 years, of which 25 were for eye-related problems (eye pain, conjunctivitis, edema of lid[s]). None of these cases subsequently attended the ophthalmology clinic at our institution but may have followed up elsewhere. See eFigure 1.
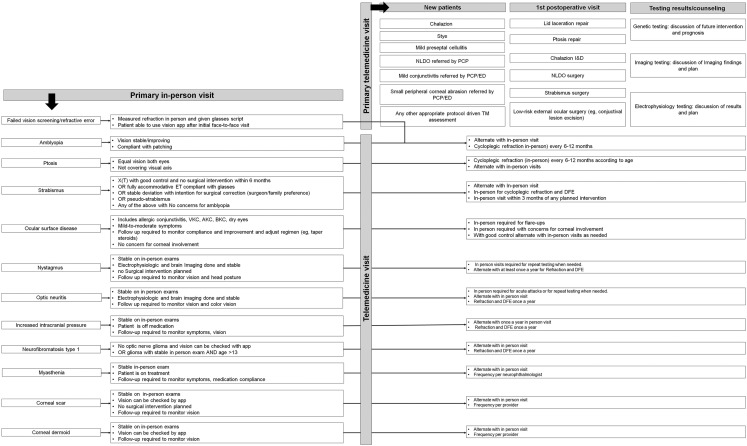
We encountered several challenges during deployment of telemedicine. The telemedicine protocol was continually being refined even as it was being used by providers. To ensure that all providers and administrators were updated on current workflows, a “live” document was made accessible via a link. Consistent communication with patients emphasized the importance of their visits through standardized scripts. We also had to find free and reliable applications for testing visual acuity and subsequently create instructional videos for patients to demonstrate their correct use. Efforts were also made to identify appropriate video platforms that would meet requirements of the US Health Insurance Portability and Accountability Act of 1996 (HIPAA) and security issues, ease of use for both providers and patients, quality of video, and costs. Based on our experience we created a flow chart with proposed management strategies for common diseases (eFigure 2). We hope this would help institutions build their own decision trees.
Discussion
In the wake of COVID-19, the face of medicine has changed overnight. The strategies we develop now will shape the delivery of care for years to come. For health care providers, adapting to a telemedicine platform requires a change in mindset. The shift from a physical examination to a virtual visit can be challenging, and the first challenge is to decide which patients can be seen with minimal clinical risk virtually versus in person. This decision should be made by the physician on the basis of careful consideration of patient history and complaints.
A virtual visit can accomplish the same amount of history taking as an in-person evaluation. This becomes all the more important with limitations being placed on examination and investigations. Subtle details might need to be elicited by nuanced questioning. A virtual visit does not mean a complete absence of examination. An external eye examination can be performed by instructing parents to position the child closer to the camera. Extraocular movements can also be tested during the encounter using a handy fixation target. One can simulate a cover test, at least at near fixation, by asking the parents to alternately cover either eye while the child looks at the camera. Following evaluation, the ophthalmologist needs to perform a risk/benefit analysis and triage patients into management over video encounter or requesting an in-person encounter.
The conditions that can be managed over a video encounter usually have a subacute to chronic natural history. Examples include follow-up visit for amblyopia or strabismus, assuming parents are able to perform visual acuity assessments and accomplish distance and near fixation during the visit. Medical/behavioral interventions can be recommended or reinforced over telemedicine. Parents need to be educated on warning signs, and a follow-up must be planned. Follow-up visits could be another telemedicine encounter or an in-person visit, at the discretion of the treating physician.
In undertaking ophthalmology telemedicine, providers must recognize that it is impossible to eliminate all risk of error. Patients with suspicion for immediately sight-threatening conditions merit an in-person examination, and in this case the healthiest family member should be instructed to accompany the child to the clinic. Decision making on the basis of video encounters is as complex, if not more so, than evaluations based on in-person encounters and should be valued and compensated accordingly.
The limitations of telemedicine ophthalmology deserve mention. Visual acuity testing is a critical component of any clinical examination, and although there are many applications that claim to check visual acuity reliably at home, standardization is lacking, with no ability to calibrate the device and ensure proper testing distance, use of nonstandard optotypes, and results given in nonconventional notations. Despite our finding an application that overcame these drawbacks, there is uncertainty about the examination. Other general limitations include an inability to examine patients that lack the device to complete a video visit, the need to be conservative with investigations and concerns for HIPAA violations.
In the wake of the crisis, the Office of Civil Rights responsible for enforcing HIPAA announced that providers may use any non-public-facing communication product to communicate with patients. The US Department of Health and Human Services website provides a list of services that will enter into HIPAA Business Associate Agreement Video if providers desire additional privacy protections. This declaration expands the scope of telemedicine and removes the barrier of patients, who may not be technologically adept, having to install specific software.
Telemedicine also brings its share of advantages too. It removes the burden of travel and increases access to subspecialty care. We envision integrating an ophthalmologist with the virtual urgent care service at our institution to provide seamless transition of care. Our particular approach to telemedicine for pediatric ophthalmology is one of many successful approaches currently being implemented. Regardless of the model, it is clear that a more comprehensive remote visual acuity testing method is needed. Intuitive standardized software for smartphones, with interoperability and privacy protections, are crucial.10 Our telemedicine paradigm might also encompass remote visual assessment facilities that house sophisticated testing equipment, such as widefield fundus photography, optical coherence tomography, and electroretinogram. Trained personnel would still be required to acquire high quality data, but the reduction in exposure and increase in accessibility might justify this model.
We expect that our protocol will continue to develop as we learn from our experiences and patient feedback. We are in the process of conducting patient surveys in order to be able to report on patient-related experience measures from this initial cohort. We are also in the process of assessing the visual acuity methods used by our patients.
Footnotes
This work was supported by NIH CORE Grant P30 EY08098 to the Department of Ophthalmology, the Eye and Ear Foundation of Pittsburgh, and from an unrestricted grant from Research to Prevent Blindness, New York, NY.
Supplementary Data
eFig 1.
The dashboard for the on-demand urgent care service attended by emergency room providers. The diagnosis cloud (black arrow) shows different diagnoses of the patients calling in; the diagnoses pertaining to eye problems (gray arrow) is delineated on the righthand side.
eFig 2.
Telemedicine guidelines common diseases, outlining the common patient presentations that would require an initial face-to-face assessment (for new patients) and how/when they would be transferred to telemedicine visits and other common scenarios that would be fit for telemedicine either as new patients or for follow-up. AKC, atopic kerato-conjunctivitis; BKC, blepharo-kerato-conjunctivitis; DFE, dilated fundus examination; ED, emergency department; ET, esotropia; I&D, incision and drainage; NLDO, nasolacrimal duct obstruction; PCP, primary care physician; VKC, vernal kerato-conjunctivitis; X(T), intermittent exotropia.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
- 3.Centers for Disease Control Interim guidance for healthcare facilities: preparing for community transmission of COVID-19 in the United States 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html Available at:
- 4.American Academy of Ophthalmology Recommendations for urgent and nonurgent patient care. 2020. https://www.aao.org/headline/new-recommendations-urgent-nonurgent-patient-care Available at:
- 5.Waldman A., Shaw A., Ngu A., Campbell S. Are hospitals near me ready for coronavirus? Here are nine different scenarios. https://projects.propublica.org/graphics/covid-hospitals ProPublica.2020. Available at:
- 6.Olson C.A., McSwain S.D., Curfman A.L., Chuo J. The current pediatric telehealth landscape. Pediatrics. 2018;141:e20172334. doi: 10.1542/peds.2017-2334. [DOI] [PubMed] [Google Scholar]
- 7.Martel J., Anders U., Kravchuk V. Comparative study of teleophthalmology devices: smartphone adapted ophthalmoscope, robotic ophthalmoscope, and traditional fundus camera—the recent advancements in telemedicine. New Front Ophthalmol. 2015 doi: 10.15761/NFO.1000102. [DOI] [Google Scholar]
- 8.Micheletti J.M., Hendrick A.M., Khan F.N., Ziemer D.C., Pasquel F.J. Current and next generation portable screening devices for diabetic retinopathy. J Diabetes Sci Technol. 2016;10:295–300. doi: 10.1177/1932296816629158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ting D.S.J., Ang M., Mehta J.S., Ting D.S.W. Artificial intelligence-assisted telemedicine platform for cataract screening and management: a potential model of care for global eye health. Br J Ophthalmol. 2019;103:1537–1538. doi: 10.1136/bjophthalmol-2019-315025. [DOI] [PubMed] [Google Scholar]
- 10.Bodnar Z.M., Schuchard R., Myung D. Evaluating new ophthalmic digital devices for safety and effectiveness in the context of rapid technological development. JAMA Ophthalmol. 2019. doi: 10.1001/jamaophthalmol.2019.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Telemedicine Association Telehealth basics. https://www.americantelemed.org/resource/why-telemedicine/ Available at:
- 12.Patel S.N., Singh R., Jonas K.E., Imaging and Informatics for Retinopathy of Prematurity Research Consortium Telemedical diagnosis of stage 4 and stage 5 retinopathy of prematurity. Ophthalmol Retina. 2018;2:59–64. doi: 10.1016/j.oret.2017.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Patel S.N., Martinez-Castellanos M.A., Berrones-Medina D., GEN-ROP. i-ROP Research Consortium Assessment of a tele-education system to enhance retinopathy of prematurity training by international ophthalmologists-in-training in Mexico. Ophthalmology. 2017;124:953–961. doi: 10.1016/j.ophtha.2017.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Redd T.K., Campbell J.P., Brown J.M., Imaging and Informatics in Retinopathy of Prematurity (i-ROP) Research Consortium Evaluation of a deep learning image assessment system for detecting severe retinopathy of prematurity. Br J Ophthalmol. 2018 doi: 10.1136/bjophthalmol-2018-313156. bjophthalmol-2018-313156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown J.M., Campbell J.P., Beers A., Imaging and Informatics in Retinopathy of Prematurity (i-ROP) Research Consortium Automated diagnosis of plus disease in retinopathy of prematurity using deep convolutional neural networks. JAMA Ophthalmol. 2018;136:803–810. doi: 10.1001/jamaophthalmol.2018.1934. [DOI] [PMC free article] [PubMed] [Google Scholar]