Abstract
Adherence to antiretroviral therapy (ART) during pregnancy and the postpartum period is necessary to prevent vertical HIV transmission and to secure the long-term health of an HIV-infected woman. Health behavior theory suggests that patients’ attitudes towards medication can predict their medication-taking behaviour. This study sought to understand how women’s attitudes towards ART changes between the pregnancy and postpartum periods, and the factors associated with these attitudes. The study enrolled 200 pregnant women living with HIV. Structured surveys were administered during pregnancy and at three and six months postpartum. Overall, attitudes towards ART were stable over time. More positive attitudes towards ART were associated with HIV acceptance, lower levels of depression, and lower levels of shame. Counselling interventions are needed to help HIV-infected women accept their status and reduce shameful emotions. Depression screening and treatment should be integrated into PMTCT services. This study emphasizes the importance of early attention to attitudes towards ART, in order to establish a trajectory of sustained care engagement.
Keywords: Tanzania, HIV/AIDS, Prevention of Mother-to-Child Transmission (PMTCT), Option B+, adherence
Background
Under the Option B+ protocol for the prevention of mother-to-child transmission of HIV (PMTCT), all pregnant women identified as living with HIV during antenatal care initiate antiretroviral therapy (ART) for lifetime use (1). When taken consistently, ART can effectively suppress HIV RNA and greatly reduce the risk of vertical transmission from mother-to-child. To achieve these benefits, it is critical to initiate treatment as early as possible and maintain adherence to medication (2,3). Poor ART adherence can lead to drug resistance (4), viral rebound, opportunistic infections, and premature mortality for both the mother and child (5). The rise of resistant strains of HIV represents a vital public health issue, as second- and third-line treatment options are limited, expensive, and often difficult to access in low-and middle-income countries. The literature suggests that care engagement and ART adherence are poorer among pregnant and postpartum women living with HIV as compared to the general population (6–8), likely due to the added stressors associated with this stage of life (9).
Poor adherence to medications is a well-known challenge in chronic illnesses that require lifelong treatment, including HIV (2). Studies have linked poor adherence with factors such as age, substance use, depression, stigma, and poor communication with health care providers (10), as well as the patient’s own perception of the importance of adherence to treatment (11). These findings suggest that although some barriers to optimal adherence are beyond patients’ control, other factors are patient-driven and related to how they perceive and value treatment.
There is a substantial body of literature, grounded in health behaviour theory, that demonstrates that patients’ beliefs about medication can predict their adherence to medication (12–14), with patients who perceive ART as necessary to their long-term health being more likely to have better adherence (15–17). In order to design and tailor interventions to improve adherence to medication, it is important to understand patient-level factors associated with motivation and commitment to lifelong ART treatment.
This study sought to understand attitudes toward ART among a population of pregnant women living with HIV in Tanzania and to explore how those attitudes evolved through the perinatal period. The study was designed with the following objectives: 1) to assess changes in patients’ attitudes about long-term use of ART from pregnancy to six-months postpartum, and 2) to identify factors that are associated with patients’ beliefs about long-term use of ART over time.
Methods
A prospective cohort of 200 pregnant women living with HIV were enrolled and followed until six months after the birth of their child. The full characteristics and HIV care engagement of this cohort has been described elsewhere (18). Participants were recruited from nine antenatal clinics (six urban and three rural) in the Kilimanjaro region. All clinics were providing care following the Tanzanian national PMTCT guidelines, which were adapted from WHO Option B+ guidelines (19). Under Option B+, all pregnant and breastfeeding women living with HIV initiate or maintain lifelong ART starting at the first perinatal appointment, regardless of WHO staging or CD4 cell count (1). PMTCT patients attend monthly appointments in the reproductive and child health clinic, combining pregnancy or new-born care with HIV management and ART medication refills.
Procedures
The study was introduced to HIV-infected pregnant women by a clinic nurse during antenatal care visits. If a woman was interested in participation, she was referred to a research nurse who screened for eligibility, provided additional details about the study, and obtained informed consent. Women were eligible for the study if they were at least 16 weeks pregnant, 18 years or older, and had been on ART for at least one month. Women who were interested in participating but referred within 30 days of initiating ART were asked to return when eligible. Both newly diagnosed women and women with established HIV diagnoses were included in the study.
Participants completed assessments during pregnancy, at three months postpartum, and at six months postpartum. Surveys were interviewer-administered in Swahili and took approximately 60 minutes to complete. Using contact information provided at enrolment, participants were reminded about the follow-up assessment through phone calls or text messages; if they were unreachable, home visits were made for those who had given prior permission. Participants were compensated 5,000 Tanzanian shillings (approximately $2.50) for each assessment to assist with transport costs. The study received ethical approval from the ethical review boards of Duke University, the Kilimanjaro Christian Medical Centre, and the Tanzanian National Institute for Medical Research.
Measures
All survey measures were translated from English to Swahili and back-translated to English to ensure cultural equivalence and quality.
Outcome measure
The primary outcome in this study was attitudes toward long-term use of ART. To examine this, women responded to the “necessity” and “concerns” subscales of the Beliefs About Medicines Questionnaire (BMQ) (20). The specific necessity subscale included five questions (e.g., “Without my ARVs I would become very ill”) and the specific concerns subscale included five questions (e.g., “Having to take ARVs for the rest of my life worries me”). Participants responded on a five-point scale, ranging from “strongly disagree” to “strongly agree”. Items from the “concerns” subscale were reversed scored, and all 10 items were summed to create an aggregate score ranging from 10 to 50 (Cronbach’s α = 0.68), with higher scores indicating more positive attitudes toward ART.
Covariates
Demographics and HIV information.
Demographics included age, level of education, and marital status. HIV diagnosis was categorized as either a new diagnosis (i.e., the woman learned her HIV status during the index pregnancy) or an established diagnosis (i.e., the woman had known her HIV status prior to the index pregnancy). Additionally, participants reported whether they had ever disclosed their HIV status to another person.
HIV acceptance.
HIV acceptance was measured using the “acceptance” subscale of the Illness Cognition Questionnaire (ICQ) (21). The subscale has six questions that measure HIV acceptance (e.g., “I can handle the problems related to my HIV status”). Participants responded on a four-point scale (1 to 4). Items were summed for a total possible score of 6 to 24 (Cronbach’s α = 0.83), with higher score indicating higher disease acceptance.
Social support.
Social support was assessed using the Perceived Availability of Social Support scale (PASS) (22). The measure contains eight questions (e.g., “Would someone be available to talk to you if you were upset, nervous, or depressed?”) that were answered in a five-point scale (1 to 5). Items were summed to get a possible total score of 8 to 40 (Cronbach’s α = 0.83), with higher scores indicating more perceived social support.
Depression.
Depressive symptoms were measured with the Edinburgh Postnatal Depression Scale (EPDS) (23). The measure contains 10 items rated from 0 to 3. Items in the measure included statements like “I have been so unhappy that I have had difficulty sleeping”. Items were summed to get a possible total score of 0 to 30 (Cronbach’s α = 0.89), with higher scores indicating higher likelihood of having depression and scores of 10 or greater indicating “possible depression” (23).
HIV related shame.
Feelings of HIV-related shame, a concept closely related to internalized stigma, were measured using Scale A of the HIV and Abuse Shame Related Inventory (HARSI) (24). The HARSI contained 13 items (e.g., “I have an overpowering dread that my HIV status will be revealed to others”). Participants responded in a five-point scale (0 to 4). Items were summed for a total possible score of 0 to 52 (Cronbach’s α = 0.86), with higher score indicating higher levels of shame related to HIV.
Analysis
Statistical analysis was performed using STATA 14.0 (25). Categorical variables were summarized with frequencies and percentages, while continuous variables were presented as medians with interquartile ranges. For scaled measures, mean imputation was performed to replace missing data and obtain total scores for the participants who answered at least 80% of items. Regression coefficients and their corresponding 95% confidence intervals for the factors associated with the BMQ were estimated using a generalized estimating equation model (linear regression case) with a robust variance estimator to account for repeated observations from the same individual. Covariates that had p < .10 in a univariate analysis were included in the final multivariate model. Selected covariates (age, education, marital status) were identified a priori to be included in the multivariate model, regardless of univariate significance.
Results
Sample description
At the time of study enrolment, the median (Q1, Q3) age of participants was 30 (25, 35) years (Table 1). Most participants (58.0%) had a primary school education or less. About half (49.0%) were married. Most women (79.5%) reported that they had disclosed their HIV status to at least one other person, most often the father of the child or a family member. Slightly more than half (53.0%) knew their HIV status prior to the index pregnancy. During pregnancy, 25.0% of participants met EPDS criteria for possible depression.
Table 1.
Characteristics of study participants at baseline (n = 200)
| n | % | |
|---|---|---|
| Education | ||
| None | 4 | 2.0 |
| Primary | 113 | 56.0 |
| Secondary | 70 | 35.0 |
| College/University | 13 | 6.5 |
| Marital status | ||
| Single | 19 | 9.5 |
| Married | 98 | 49.0 |
| In relationship; not married | 74 | 37.0 |
| Separated or divorced | 6 | 3.0 |
| Widowed | 3 | 1.5 |
| HIV diagnosis | ||
| New diagnosis during current pregnancy | 94 | 47.0 |
| Previously established diagnosis | 106 | 53.0 |
| HIV status disclosure | ||
| Yes | 159 | 79.5 |
| No | 41 | 20.5 |
| Median (Q1, Q3) | ||
| Age (years) | 30 (25, 35) | |
| Depression – EPDS | ||
| [range 0 –30; high score = more depression] | 5 (2, 9.5) | |
| HIV related shame – HARSI | ||
| [range 0 – 52; high score = more shame] | 16 (12, 25) | |
| Social support – PAS | ||
| [range 8 – 40; high score = more support] | 29 (24, 34) | |
| HIV acceptance | ||
| [range 6 – 24; high score = more acceptance] | 18 (15, 20) | |
Of the 200 enrolled participants, 168 (84.0%) completed a follow-up survey at 3 months postpartum, and 179 (89.5%) completed a follow-up survey at 6 months postpartum. Figure 1 shows how attitudes towards ART changed over time; attitudes toward ART tended to be stable over time, with non-significant improvement in the composite BMQ score.
Figure 1.
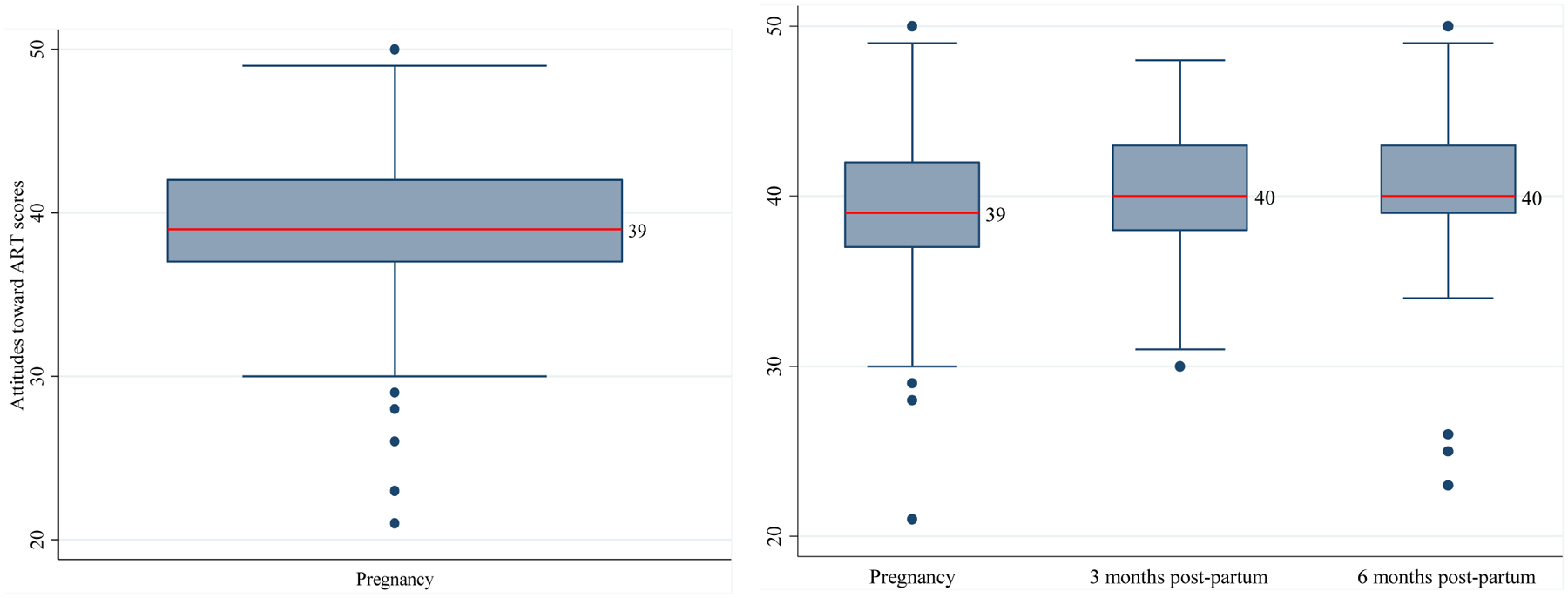
Cohort variation of attitudes towards ART across study time points, during pregnancy (n=200) and across study period (n = 159) for those with data at all timepoints
Factors associated with attitudes toward long-term use of ART
Among our covariates, some variables were stable (i.e., did not change significantly across time points), while others differed across time points. The univariate and multivariate regression models are shown in Table 2. In the final multivariate model, attitudes toward long-term ART use was significantly associated with level of education, acceptance of HIV status, shame, and depression. Having a primary education or lower (ß = 0.92; 95%CI: 0.13, 1.70) and having more acceptance of one’s HIV status (ß= 0.46; 95%CI: 0.35, 0.57) were associated with more positive attitudes toward long-term use of ART. The ß coefficients show an average change in attitudes towards ART for a unit increase in a co-variate, provided other co-variates remain constant. For example, study participants with a primary education or lower had an average of 0.92-point increase on the attitudes towards ART scale compared to those with secondary education or higher, controlling for all other co-variates. Higher levels of HIV-related shame (ß = −0.07; 95%CI: −0.12, −0.03) and higher depression scores (ß = −0.12; 95%CI: −0.21, −0.03) were negatively associated with attitudes toward long-term use of ART. There was a slight improvement in attitudes toward ART from baseline to 3 months (ß = 0.24; 95%CI: −0.45, 0.94), but this was not significant when controlling for other variables. Similarly, there was no difference in attitudes toward ART between women who were diagnosed with HIV during the index pregnancy and those with an established HIV diagnosis (ß = −0.14; 95%CI: −0.62, 0.90).
Table 2.
Factors associated with attitudes towards long term use of ART (n=200)
| Regression coefficient (95%CI) | Adjusted regression coefficient (95%CI) | |
|---|---|---|
| Age (5 years increments) | 0.34 (− 0.03, 0.72) | 0.08 (− 0.21, 0.37) |
| Education | ||
| Primary or lower | 0.78 (− 0.16, 1.73) | 0.92 (0.13, 1.70) * |
| [ref: Secondary or higher] | ||
| HIV diagnosis | ||
| New diagnosis | − 0.70 (− 1.61, 0.20) | − 0.14 (− 0.62, 0.90) |
| [ref: Established diagnosis] | ||
| Marital status | ||
| Single/Divorced/Widowed | − 0.42 (− 1.63, 0.79) | 0.37 (− 0.57, 1.32) |
| [ref: Married/Cohabiting] | ||
| HIV status disclosure | ||
| Never disclosed | − 0.87 (− 1.95, 0.21) | |
| [ref: Has disclosed] | ||
| Depression – EPDS scale | ||
| [range 0 –30; high score ~ more depression] | − 0.24 (− 0.32, − 0.17) *** | − 0.12 (− 0.21, − 0.03) ** |
| HIV related shame – HARSI | ||
| [range 0 – 52; high score ~ more shame] | − 0.14 (− 0.19, − 0.10) *** | − 0.07 (− 0.12, − 0.03) ** |
| Social support - PAS | ||
| [range 8 – 40; high score ~ more support] | 0.14 (0.06, 0.22) *** | 0.06 (− 0.003, 0.12) |
| HIV acceptance | ||
| [range 6 – 24; high score ~ more acceptance] | 0.50 (0.39, 0.61) *** | 0.46 (0.35, 0.57) *** |
| Timepoints | ||
| Baseline – 3 months post-partum | 1.41 (0.73, 2.09) *** | 0.24 (− 0.45, 0.94) |
| 3 months post-partum – 6 months post-partum | 0.24 (− 0.92, 0.87) | 0.006 (− 0.63, 0.64) |
p<0.05
p<0.01
p<0.001
Discussion
In this cohort study of women receiving PMTCT services during the Option B+ era, we prospectively followed 200 women during pregnancy and the early postpartum period. We identified important factors that were associated with attitudes toward ART, namely acceptance of one’s HIV status, depression and shame. Notably, attitudes toward ART were stable over time and did not improve or decline from the pregnancy to the postpartum period.
Acceptance of one’s HIV status was a strong predictor of positive attitudes towards ART. Previous studies have shown that HIV status acceptance is an important factor in initiating and remaining in HIV care (26), while denial of one’s HIV status has an opposite effect (27,28). Accepting one’s HIV status can help an individual to accommodate the types of changes that occur with a new HIV diagnosis, such as making regular clinic visits and integrating pill-taking into a daily routine. Evidence has shown that patients who accepted their HIV status were more committed to remaining adherent to ART and worked to find solutions to obstacles they faced (29).
In this cohort of women, we observed that participants who had greater levels of depression or HIV related shame had more negative attitudes towards ART. Both depression (30–32) and shame (33) have been closely connected to the experience of HIV stigma and have been identified as barriers to engagement in HIV care and treatment. Depression can contribute to cognitive distortions about one’s self and the future, resulting in negative attitudes towards activities that can improve one’s life, such as use of ART (34). Feeling ashamed as someone living with HIV, or feeling fearful of the consequences of having one’s status revealed, are core components of HIV internalized stigma and can weaken commitment to lifelong treatment (35,36). These connections may be particularly poignant among pregnant women, who may experience additional shame and fear surrounding the potential to transmit HIV to their child (37,38).
Our findings support past studies of health behaviour theory in this population by reinforcing the need for more ongoing, personalized services to support pregnant women’s long-term HIV care engagement. When implemented effectively, antenatal counselling serves to educate women about the role of ART in preventing mother-to-child transmission of HIV, which may temporarily motivate patients to adhere to ART (12,14–15). However, without ongoing support to address underlying emotional challenges and doubts about treatment, this motivation is likely to wane. Thus, these findings reveal the need for comprehensive counselling that addresses HIV acceptance, depressive symptoms, disclosure, and stigma – factors that are closely linked and mutually reinforcing (39). Past studies in sub-Saharan Africa have largely focused on incorporating brief counselling into voluntary testing services (40), but few have assessed the acceptability, feasibility, or effectiveness of more intensive counselling approaches that seek to address the many complex personal factors that influence ART adherence (14,41). One pilot study of a cognitive-behavioural intervention to address HIV stigma in South Africa led to positive changes in coping skills, stigma, self-esteem, and depressive symptoms (42). Future studies should seek to advance similar research in more diverse settings.
In our cohort, attitudes toward ART remained stable in our cohort over time, from pregnancy to the postpartum period. Furthermore, attitude scores were not significantly different in comparing women who were diagnosed during the current pregnancy with women who entered pregnancy with a known HIV diagnosis. This finding suggests that interventions addressing patients’ attitudes toward ART may be reasonably implemented at any stage of the perinatal period. At the same time, intervening at the time of entry into antenatal care can be an opportunity to address attitudes about ART and improve care engagement prior to giving birth, which may prevent vertical transmission to the child.
The expansion of ART access under Option B+ presents an important opportunity for improved outcomes of HIV-infected mothers and their children if ART is used as prescribed. In Tanzania, Option B+ guidelines have been integrated in the national PMTCT protocol and a “test and treat” approach has been extended to all individuals with a new HIV diagnosis. The success of these initiatives requires comprehensive programs, including counselling, that facilitate care engagement and enhance adherence to medication. Addressing patients’ attitudes to long-term antiretroviral therapy is a precursor for long-term retention in care, and deserves our upmost attention.
The major strength of this prospective cohort study is that it enabled repeated assessment of attitudes toward ART and factors associated with these attitudes. However, there are several important limitations to note. First, this study only enrolled women who had been using ART for at least one month; women who didn’t return after the first PMTCT visit were not enrolled. This group of women were likely to have more negative attitudes toward ART, and hence, attitudes towards ART scores presented in this paper may have overestimated positive attitudes toward ART. Second, although this study was designed to be an observational study with no deviations from the standard of care at PMTCT, regular contact with the study nurses over an extended period of time may have impacted how patients perceived care and ART. Lastly, not all measures used in this study had been previously validated in a Tanzanian setting, which may contribute to measurement bias.
Conclusions
This study found evidence that attitudes toward lifelong use of ART remain stable over time, stressing the importance of providing targeted and intensive support at the time of HIV diagnosis and entry into care. Interventions are needed to support newly diagnosed women to accept their status, to mitigate the formation of internalized stigma, and to reduce mental health symptoms. Investments in comprehensive counselling and support programs may have the potential to improve commitment and motivation to care, and to lead to better care engagement and adherence.
Funding:
This study was funded by a grant from the NIH National Institute of Allergies and Infectious Diseases (NIAID), Grant R21 AI124344. We also acknowledge support received from the Duke Center for AIDS Research, Grant P30 AI064518.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was reviewed and approved by the ethical review boards at Duke University, the Kilimanjaro Christian Medical Centre, and the Tanzanian National Institute for Medical Research.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.World Health Organization, Department of HIV/AIDS. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. 2015. http://www.ncbi.nlm.nih.gov/books/NBK327115/. [PubMed]
- 2.Sabaté E, World Health Organization, editors. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. https://www.who.int/chp/knowledge/publications/adherence_report/en/ [Google Scholar]
- 3.Nachega JB, Marconi VC, van Zyl GU, Gardner EM, Preiser WY Hong S, et al. HIV Treatment Adherence, Drug Resistance, Virologic Failure: Evolving Concepts. Infect Disord Drug Targets. 2011;11(2):167–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sethi AK, Celentano DD, Gange SJ, Moore RD, Gallant JE. Association between Adherence to Antiretroviral Therapy and Human Immunodeficiency Virus Drug Resistance. Clin Infect Dis. 2003;37(8):1112–8. [DOI] [PubMed] [Google Scholar]
- 5.Bangsberg DR, Perry S, Charlebois ED. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–3. [DOI] [PubMed] [Google Scholar]
- 6.Nachega JB, Uthman OA, Anderson J, Peltzer K, Wampold S, Cotton MF, et al. Adherence to Antiretroviral Therapy During and After Pregnancy in Low-, Middle and High Income Countries: A Systematic Review and Meta-Analysis. AIDS. 2012;26(16):2039–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tenthani L, Haas AD, Tweya H, Jahn A, van Oosterhout JJ, Chimbwandira F, et al. Retention in care under universal antiretroviral therapy for HIV-infected pregnant and breastfeeding women (‘Option B+’) in Malawi: AIDS. 2014;28(4):589–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cichowitz C, Mazuguni F, Minja L, Njau P, Antelman G, Ngocho J, et al. Vulnerable at Each Step in the PMTCT Care Cascade: High Loss to Follow Up During Pregnancy and the Postpartum Period in Tanzania. AIDS Behav. 2018; doi: 10.1007/s10461-018-2298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knettel BA, Cichowitz C, Ngocho JS, Knippler ET, Chumba LN, Mmbaga BT, et al. Retention in HIV Care During Pregnancy and the Postpartum Period in the Option B+ Era: Systematic Review and Meta-Analysis of Studies in Africa. J Acquir Immune Defic Syndr. 2018;77(5):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adeniyi OV, Ajayi AI, Ter Goon D, Owolabi EO, Eboh A, Lambert J. Factors affecting adherence to antiretroviral therapy among pregnant women in the Eastern Cape, South Africa. BMC Infect Dis. 2018;18(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mbirimtengerenji ND, Jere G, Lengu S, Maluwa A. Factors That Influence Anti-Retroviral Therapy Adherence among Women in Lilongwe Urban Health Centres, Malawi. World J AIDS. 2013;03(01):16–25. [Google Scholar]
- 12.Lemay J, Waheedi M, Al-Sharqawi S, Bayoud T. Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer Adherence. 2018;12:1687–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rajpura JR, Nayak R. Role of Illness Perceptions and Medication Beliefs on Medication Compliance of Elderly Hypertensive Cohorts. J Pharm Pract. 2014;27(1):19–24. [DOI] [PubMed] [Google Scholar]
- 14.Kalichman S, Kalichman MO, Cherry C. Medication beliefs and structural barriers to treatment adherence among people living with HIV infection. Psychol Health. 2016;31(4):383–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horne R, Buick D, Fisher M. Doubts about necessity and concerns about adverse effects Identifying the types of beliefs that are associated with non-adherence to HAART. Int J STD AIDS. 2004;15(1):38–44. [DOI] [PubMed] [Google Scholar]
- 16.Horne R, Cooper V, Gellaitry G, Date HL, Fisher M. Patients’ Perceptions of Highly Active Antiretroviral Therapy in Relation to Treatment Uptake and Adherence: The Utility of the Necessity-Concerns Framework. J Acquir Immune Defic Syndr. 2007;45(3):334–41. [DOI] [PubMed] [Google Scholar]
- 17.Horne R, Chapman SCE, Parham R, Freemantle N, Forbes A, Cooper V. Understanding Patients’ Adherence-Related Beliefs about Medicines Prescribed for Long-Term Conditions: A Meta-Analytic Review of the Necessity-Concerns Framework Xia Y, editor. PLoS ONE. 2013;8(12):e80633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Watt MH, Cichowitz C, Kisigo G, Minja L, Knettel BA, Knippler ET, et al. Predictors of postpartum HIV care engagement for women enrolled in prevention of mother-to-child transmission (PMTCT) programs in Tanzania. AIDS Care. 2018;1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National AIDS Control Programme. NATIONAL GUIDELINES FOR THE MANAGEMENT OF HIV AND AIDS. Ministry of Health, Community Development, Gender, Elderly and Children; 2017. https://aidsfree.usaid.gov/sites/default/files/04_11_2016.tanzania_national_guideline_for_management_hiv_and_aids_may_2015._tagged.pdf [Google Scholar]
- 20.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. [Google Scholar]
- 21.Evers AW, Kraaimaat FW, van Lankveld W, Jongen PJ, Jacobs JW, Bijlsma JW. Beyond unfavorable thinking: the illness cognition questionnaire for chronic diseases. J Consult Clin Psychol. 2001;69(6):1026–36. [PubMed] [Google Scholar]
- 22.O’Brien K, Wortman CB, Kessler RC, Joseph JG. Social relationships of men at risk for AIDS. Soc Sci Med. 1993;36(9):1161–7. [DOI] [PubMed] [Google Scholar]
- 23.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. [DOI] [PubMed] [Google Scholar]
- 24.Neufeld SAS, Sikkema KJ, Lee RS, Kochman A, Hansen NB. The development and psychometric properties of the HIV and Abuse Related Shame Inventory (HARSI). AIDS Behav. 2012;16(4):1063–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp, LLC; 2015. [Google Scholar]
- 26.Horter S, Thabede Z, Dlamini V, Bernays S, Stringer B, Mazibuko S, et al. “Life is so easy on ART, once you accept it”: Acceptance, denial and linkage to HIV care in Shiselweni, Swaziland. Soc Sci Med. 2017;176:52–9. [DOI] [PubMed] [Google Scholar]
- 27.Nam SL, Fielding K, Avalos A, Dickinson D, Gaolathe T, Geissler PW. The relationship of acceptance or denial of HIV-status to antiretroviral adherence among adult HIV patients in urban Botswana. Soc Sci Med. 2008;67(2):301–10. [DOI] [PubMed] [Google Scholar]
- 28.Nakigozi G, Atuyambe L, Kamya M, Makumbi FE, Chang LW, Nakyanjo N, et al. A Qualitative Study of Barriers to Enrollment into Free HIV Care: Perspectives of Never-in-Care HIV-Positive Patients and Providers in Rakai, Uganda. BioMed Res Int. 2013;2013:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vervoort SCJM, Grypdonck MHF, de Grauwe A, Hoepelman AIM, Borleffs JCC. Adherence to HAART: processes explaining adherence behavior in acceptors and non-acceptors. AIDS Care. 2009;21(4):431–8. [DOI] [PubMed] [Google Scholar]
- 30.Starace F, Ammassari A, Trotta MP, Murri R, De Longis P, Izzo C, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31 Suppl 3:S136–139. [DOI] [PubMed] [Google Scholar]
- 31.Spire B, Duran S, Souville M, Leport C, Raffi F, Moatti J-P. Adherence to highly active antiretroviral therapies (HAART) in HIV-infected patients: from a predictive to a dynamic approach. Soc Sci Med. 2002;54(10):1481–96. [DOI] [PubMed] [Google Scholar]
- 32.MACH14 Investigators, Wagner GJ, Goggin K, Remien RH, Rosen MI, Simoni J, et al. A Closer Look at Depression and Its Relationship to HIV Antiretroviral Adherence. Ann Behav Med. 2011;42(3):352–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Konkle-Parker DJ, Erlen JA, Dubbert PM. Barriers and Facilitators to Medication Adherence in a Southern Minority Population With HIV Disease. J Assoc Nurses AIDS Care. 2008;19(2):98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DiMatteo MR, Lepper HS, Croghan TW. Depression Is a Risk Factor for Noncompliance With Medical Treatment: Meta-analysis of the Effects of Anxiety and Depression on Patient Adherence. Arch Intern Med. 2000;160(14):2101. [DOI] [PubMed] [Google Scholar]
- 35.Florom‐Smith AL, Santis JPD. Exploring the Concept of HIV-Related Stigma. Nurs Forum. 2012;47(3):153–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV Stigma Mechanisms and Well-Being Among PLWH: A Test of the HIV Stigma Framework. AIDS Behav. 2013;17(5):1785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buregyeya E, Naigino R, Mukose A, Makumbi F, Esiru G, Arinaitwe J, et al. Facilitators and barriers to uptake and adherence to lifelong antiretroviral therapy among HIV infected pregnant women in Uganda: a qualitative study. BMC Pregnancy Childbirth. 2017;17(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Onono M You Know You Are Sick, Why Do You Carry A Pregnancy Again? Applying the Socio-Ecological Model to Understand Barriers to PMTCT Service Utilization in Western Kenya. J AIDS Clin Res. 2015;6(6):437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hutchinson P, Dhairyawan R. Shame and HIV: Strategies for addressing the negative impact shame has on public health and diagnosis and treatment of HIV. Bioethics. 2018;32(1):68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fonner VA, Denison J, Kennedy CE, O’Reilly K, Sweat M. Voluntary counseling and testing (VCT) for changing HIV-related risk behavior in developing countries. Cochrane HIV/AIDS Group, editor. Cochrane Database Syst Rev. 2012; http://doi.wiley.com/10.1002/14651858.CD001224.pub4 (accessed March 11, 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brittain K, Remien RH, Mellins CA, Phillips TK, Zerbe A, Abrams EJ, et al. Determinants of suboptimal adherence and elevated HIV viral load in pregnant women already on antiretroviral therapy when entering antenatal care in Cape Town, South Africa. AIDS Care. 2018;30(12):1517–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tshabalala J, Visser M. Developing a Cognitive Behavioural Therapy Model to Assist Women to Deal with HIV and Stigma. South Afr J Psychol. 2011;41(1):17–28. [Google Scholar]


