Abstract
We have witnessed successive stages since the Seventies in the advancements towards digital pathology. We agree with Dr Pallua et al on the tremendous changes that are taking place in pathology, all leading toward greater role of digitalization in the field of pathology, both in terms of consultation and teaching. In particular, distance teaching using digital pathology will grow into a mainstream mode of pathology teaching, something that has been reinforced by COVID-19.
Keywords: Digital pathology, Projection screen, Glass, Slide scanner, Virtual slide, Smart working, Confocal microscopy
1. Introduction
We have read with great interest the review paper by Dr Pallua et al. entitled “The future of pathology is digital” published in the September issue of Pathology, Research and Practice. According to them, “digital pathology allows a change from classical histopathological diagnosis with microscopes and glass slides to virtual microscopy on the computer, with multiple tools using artificial intelligence and machine learning to support pathologists in their future work” [1].
Their contribution has led us, a transnational group of closely collaborating (uro)pathologists, all from teaching hospitals, to some considerations on what we call “pathology without microscope eyepieces”. Some of us have practiced and taught pathology for several years, and have witnessed four successive stages, since the Seventies, in the development of digital pathology.
2. Stage No 1: Microscope image from a glass slide shown on projection screen
The first stage was the advancement in the traditional optical microscopy, compared to what was like previously, i.e., lonely view of a glass slide by an individual pathologist, looking through the microscope eyepieces, who recounted in words what he/she was seeing.
In the Seventies the microscope became more sophisticated and enriched with single or multiple “non-digital” cameras, first for black and white, and later on for color film photography. Film photography (also known as analog photography), with the exception of the Polaroid instant camera and film, took some time and even days to get the printed material ready for discussion and teaching, or for publication. For this reason, some microscopes were equipped with a directionally adjustable projection screen, often of a diameter of 250 mm. While the pathologist examined the slide under the microscope through the eyepieces, part of the field of view was projected in real time on the surface of the screen. This allowed him/her to discuss the features of the lesion with a colleague and/or a student who were able to see the lesion as if they were looking through the eyepieces simultaneously with him/her (Fig. 1A and B). To us this was the real beginning of joint examination of a slide.
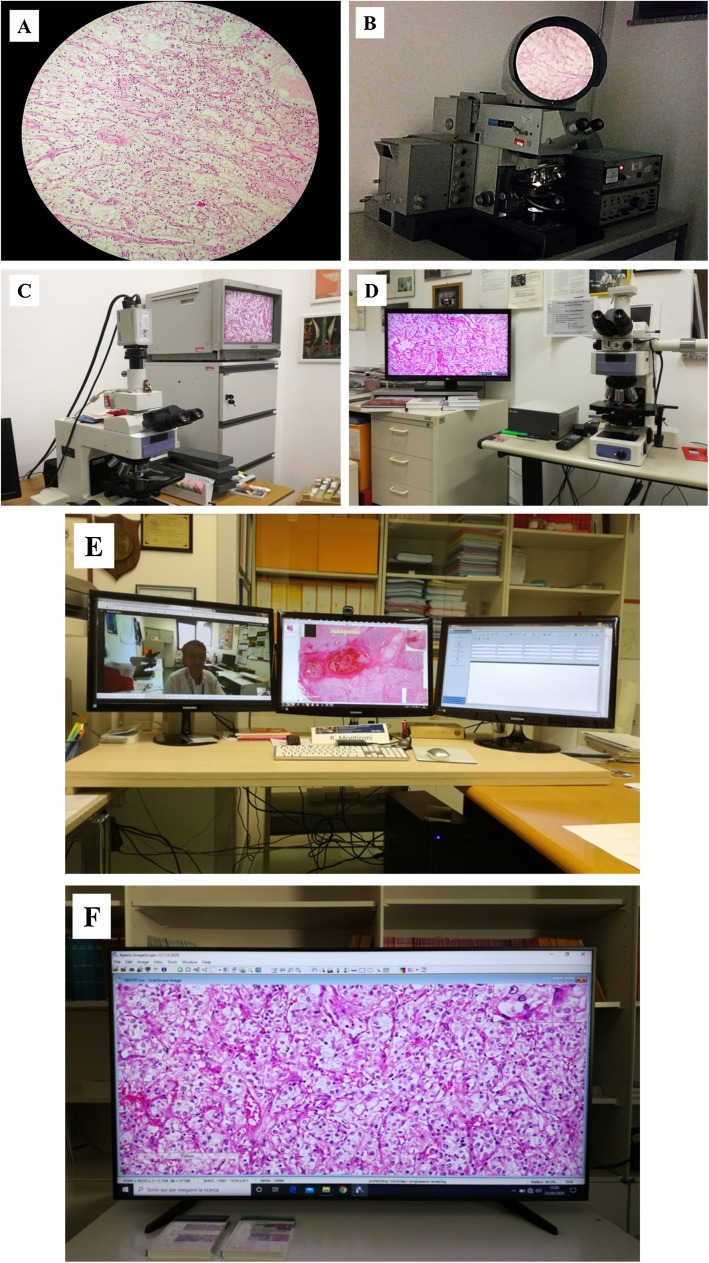
Fig. 1.
A. Microscope image of a clear cell renal cell carcinoma from a glass slide taken with a cell phone camera through the eyepieces of the same microscope as in Fig. 1B (The images of all the Figures are from the same case).
B. Microscope image from a glass slide shown on projection screen.
C. Microscope image from a glass slide shown on cathode-ray tube-based television via an CCD camera with analog output.
D. Microscope image of a clear cell renal cell carcinoma from a glass slide shown on a computer monitor, obtained with a digital camera attached to a microscope.
E. Digital image obtained with a slide scanner, examined in multi-monitor setting in the office (See text).
F. Digital image obtained with a slide scanner, examined on a TV home (consumer) screen.
3. Stage No 2: Microscope image from a glass slide shown on an old style television via an analog camera
The second stage took place in the early Eighties and was based on analog signal processing. The system included an analog camera, or video-camera, connected to an optical microscope. This is a device that converts an optically magnified image into an electric signal and displays its image on a terminal display, at that time on an analog receiver or old style (cathode-ray tube-based) television (TV).
In this second stage of simultaneous view of the microscopic image by the examining pathologist with others, the basic advantages were that the size of the image displayed on the TV was greater than that on projection screen and that the person viewing and discussing the image could have done it away from the microscope room (Fig. 1C). One of the limitations was the quality of the image shown, this being linked not only to the video-camera but also to the TV itself.
4. Stage No 3: Digital imaging and computer monitor
The third stage started approximately in the Nineties with the development of CCD (charge-coupled device) or CMOS (complementary metal oxide semiconductor) camera, a major technology used in digital imaging. The digital output was for LCD computer monitor, whose resolution increased over time from 320 × 200 to top and consumer monitors with resolution in the range of 3840 × 2160 (Fig. 1D). For those of us who had previous experience with histopathological image viewing without microscope eyepieces (See Stages No 1 and No 2), this represented a quantum leap forward, for the high quality of the dynamic image on the monitor, offering a vision somewhat similar to that in a cinema movie. In addition to that, a mouse attached to the camera was used to point out specific features, to take a picture of it or to make some basic annotations, such as size of an object. This is what we have nowadays in most of our office linked to a microscope.
One of our group (RM) has adopted the device of this third stage for a quite long period of time. It has been used in such a way that first the image is examined under the microscope through the eyepieces and then the same image or field of view on the computer monitor. The reason has been to get used to examining an image on the screen with the same level of confidence as when using the microscope. This is an important point, because we are used to the image under the microscope and we need to build confidence with the lesion on the monitor before we move to the fourth stage (See below).
5. Stage No 4: Virtual slide and TV home (consumer) screen
The fourth stage is basically related to the appearance on the market in the last few years of glass slide scanners and of virtual slides. This has freed the pathologist from the use of the microscope. In this stage, virtual slide examination has been done in two different ways.
One way is in a multi-monitor setting such as that shown in Fig. 1E. This is mainly used for reporting. The virtual slide is shown in one of the monitors. The user can navigate and change magnification in order to define the lesion and its nature. Another monitor is used to type the pathology report, such as the one on the right of Fig. 1E, while another is used for interacting via one of the video conferencing platforms with others. This system is such that a screen can be shared and the remote colleague or student can see the lesion being shown on the user’s monitor. The advantage with this approach is that there is full integration with reporting as well as full interaction with colleague or student.
The other way is the so-called smart working from home [2]. Virtual slides are sent and received via a home internet connection and shown in real time on a TV consumer (home) screen, linked to a mini PC. A wireless mouse can be used to scan the slide, zoom in, and make annotations (Fig. 1F). The viewing pathologist does not feel isolated because he/she, while analyzing the slide, can simultaneously communicate with others via one of the platforms easily available. Such communication includes voice and image of a colleague and/or student, shown in a window in a corner of the TV home screen, at the same time as the virtual slide.
Currently available scanners are not primarily intended for use with non-formalin-fixed paraffin embedded tissue specimens. Confocal microscopy acquires digital images from fresh tissue that are either displayed on a computer monitor or shared with a remote viewer for real time evaluation. Our group has acquired some experience on this with prostate tissue specimens for the evaluation of the surgical margins at the time of a radical prostatectomy procedure (4). In particular, one of us (AC) has been able to evaluate virtual slides of surgical margins displayed on a high definition TV screen at home and at the night in the USA, while a radical prostatectomy was performed in the morning in Europe [3].
6. Conclusions
We have witnessed successive stages since the Seventies in the advancements towards digital pathology. We agree with Dr Pallua et al. on the tremendous changes that are taking place in pathology, all leading toward greater role of digitalization in the field of pathology, both in terms of consultation and teaching [1]. In particular, distance teaching using digital pathology will grow into a mainstream mode of pathology teaching, something that has been reinforced by COVID-19 [4].
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Pallua J.D., Brunner A., Zelger B. The future of pathology is digital. Pathol. Res. Pract. 2020;216 doi: 10.1016/j.prp.2020.153040. [DOI] [PubMed] [Google Scholar]
- 2.Cimadamore A., Lopez-Beltran A., Scarpelli M. Digital pathology and COVID-19 and future crises: pathologists can safely diagnose cases from home using a consumer monitor and a mini PC. J. Clin. Pathol. 2020 doi: 10.1136/jclinpath-2020-206943. jclinpath-2020-206943. [DOI] [PubMed] [Google Scholar]
- 3.Rocco B., Sighinolfi M.C., Cimadamore A. Digital frozen section of the prostate surface during radical prostatectomy: a novel approach to evaluate surgical margins. BJU Int. 2020 doi: 10.1111/bju.15108. [DOI] [PubMed] [Google Scholar]
- 4.Evans A.J., Depeiza N., Allen S.G. Use of whole slide imaging (WSI) for distance teaching. J. Clin. Pathol. 2020:1–4. doi: 10.1136/jclinpath-2020-206763. [DOI] [PubMed] [Google Scholar]