Abstract
Background
Patients with coronavirus disease 2019 (COVID-19) who have underlying malignancy have a higher mortality rate compared with those without cancer, although the magnitude of such excess risk is not clearly defined. We performed a systematic review and pooled analysis to provide precise estimates of the mortality rate among patients with both cancer and COVID-19.
Methods
A systematic literature search involving peer-reviewed publications, preprints and conference proceedings up to July 16, 2020, was performed. The primary end-point was the case fatality rate (CFR), defined as the rate of death among patients with cancer and COVID-19. The CFR was assessed with a random effects model, which was used to derive a pooled CFR and its 95% confidence interval (CI).
Results
Fifty-two studies, involving a total of 18,650 patients with both COVID-19 and cancer, were selected for the pooled analysis. A total of 4243 deaths were recorded in this population. The probability of death was 25.6% (95% CI: 22.0%–29.5%; I2 = 48.9%) in this patient population.
Conclusions
Patients with cancer who develop COVID-19 have high probability of mortality. Appropriate and aggressive preventive measures must be taken to reduce the risk of COVID-19 in patients with cancer and to optimally manage those who do contract the infection.
Keywords: Cancer, COVID-19, Mortality, Malignancy, Pandemic, SARS-CoV-2, CFR, Death rate
Abbreviations: AACR, American Association of Cancer Research; ASCO, American Society of Clinical Oncology; COVID-19, coronavirus disease 2019; CCC-19, COVID-19 and Cancer Consortium; ESMO, European Society for Medical Oncology; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TERAVOLT, Thoracic cancERs international coVid 19 cOLlaboraTion
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by the beta-coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread globally and resulted in more than 635,000 deaths as of July 24, 2020 [1]. Among patients with COVID-19, those with cancer have worse outcomes compared with those without underlying malignancy, but mortality rates differ significantly among studies, ranging from 3.7% to 61.5% [2,3].
Even larger studies have significantly different mortality rates – for example, a prospective observational cohort study from the UK reported a mortality rate of 35.4% (617 deaths among 1743 patients with COVID-19 and cancer) [4], while the most recent update from the COVID-19 and Cancer Consortium (CCC-19) showed a death rate of 15.8% (433 deaths in a cohort of 2749 patients with both diseases) [5].
Many of the studies reporting outcomes of patients with both cancer and COVID-19 to date have included relatively small numbers of such patients. Data related to this subpopulation are rapidly increasing but are mostly fragmented. The aim of this systematic review and pooled analysis is to provide a more robust estimate of the mortality rate among SARS-CoV-2–infected patients with underlying cancer.
2. Methods
2.1. Literature search
A systematic literature review of PubMed, Google Scholar, MedRxiv and conference proceedings from the American Association of Cancer Research (AACR), American Society of Clinical Oncology, European Society for Medical Oncology 2020 up to July 16, 2020, was performed by two coauthors (KSS and MT), and disagreement was resolved by consensus with all authors. Multiple combinations of search terms were used: (COVID OR coronavirus OR SARS-CoV-2) AND (cancer OR tumour OR tumour OR malignancy OR malignancies OR neoplasia) AND (mortality OR death). The included study references were cross searched for additional studies. The duplicated reports were removed. The CCC-19 data were updated to reflect the keynote address at the AACR Virtual Meeting: COVID-19 and Cancer by Dr Solange Peters on July 21, 2020.
2.2. Study selection
Inclusion criteria were as follows: (i) studies reporting mortality rate in patients with cancer and COVID-19; (ii) any type of study (including retrospective studies, randomised controlled trials, prospective cohort studies and case series); (iii) studies involving adults; (iv) studies published in English, Spanish or French language.
Exclusion criteria were as follows: (i) studies with less than 10 patients with both cancer and COVID-19; (ii) studies reported in languages other than the aforementioned ones.
2.3. Data extraction
Data were independently extracted by two authors (KSS and MT). Extracted data consisted of first author's name, type of publication (i.e. peer reviewed, preprint or conference proceeding), reported number of patients with cancer and COVID-19, the number of deaths among the study population, study time period, institution or country involved and type of cancer.
2.4. Statistical analysis
Primary end-point was the case fatality rate (CFR), defined as the rate of death among patients with cancer and COVID-19. The CFR was assessed with a random effects model, which was used to derive a pooled CFR and its 95% confidence interval (CI). Heterogeneity was assessed with the I2 test (substantial heterogeneity whenever I2 ≥ 50%). A sensitivity analysis was performed excluding reports including less than 100 patients.
3. Results
After the systematic literature search, 682 references (including 216 preprints) were retrieved, of which 598 were excluded on the basis of their titles and 32 on the basis of their abstract or full text due to various reasons (inclusion of paediatric patients, duplicated results, cohorts with less than 10 patients, studies not reporting number of deaths, studies not involving patients). In total, 52 studies were included in this pooled analysis with a total of 18,650 patients with cancer and reporting 4243 deaths (Table 1 ).
Table 1.
Mortality data from 52 studies on patients with cancer and COVID-19.
| S No. | First author | Type of study | Total patients with cancer and COVID-19 | Deaths in patients with cancer and COVID-19 | Time period | Institution or country | Type of cancer |
|---|---|---|---|---|---|---|---|
| 1 | Burn et al. [11] | Preprint | 6656 | 1317 | 1 Mar to 6 May 2020 | Catalonia, Spain | Any |
| 2 | Peters [5] | Conference proceedings | 2749 | 433 | 17 Mar to 26 June 2020 | COVID-19 and Cancer Consortium (CCC-19), USA, Canada, Spain | Any |
| 3 | Docherty et al. [4] | Peer reviewed | 1743 | 617 | 6 Feb to 19 Apr 2020 | UK | Any |
| 4 | Fratino et al. [12] | Peer reviewed | 909 | 150 | Upto 30 Mar 2020 | Italy | Any |
| 5 | Lee et al. [13] | Peer reviewed | 800 | 226 | 18 Mar to 26 Apr 2020 | UK Coronavirus Cancer Monitoring Project (UKCCMP) | Any |
| 6 | Montopoli et al. [14] | Peer reviewed | 430 | 75 | Upto 1 Apr 2020 | 68 hospitals, Veneto, Italy | Any (but population restricted to men only) |
| 7 | Robilotti et al. [15] | Peer reviewed | 423 | 51 | 10 Mar to 7 Apr 2020 | New York, USA | Any |
| 8 | Horn et al. [16] | Conference proceedings | 400 | 141 | 26 Mar to 12 Apr 2020 | TERAVOLT Registry (8 countries) | Thoracic cancers only |
| 9 | Miyashita et al. [17] | Peer reviewed | 334 | 37 | 1 Mar to 6 Apr 2020 | Mt Sinai Health System, New York, USA | Any |
| 10 | Graselli et al. [18] | Peer reviewed | 331 | 202 | Upto 22 Apr 2020 | Lombardy, Italy | Any |
| 11 | Wang et al. [19] | Preprint | 283 | 50 | 17 Dec 2019 to 18 Mar 2020 | Hubei, China | Any |
| 12 | COVIDSurg Collaborative [20] | Peer reviewed | 239 | 66 | 1 Jan to 31 Mar 2020 | 24 countries | Any (COVID-19 was diagnosed based on lab, clinical or radiological features) |
| 13 | Tian et al. [21] | Peer reviewed | 232 | 46 | 13 Jan to 18 Mar 2020 | 9 hospitals in Wuhan, China | Any |
| 14 | Mehta et al. [22] | Peer reviewed | 218 | 61 | 18 Mar to 8 Apr 2020 | New York, USA | Any |
| 15 | Yang et al. [23] | Peer reviewed | 205 | 30 | 13 Jan to 18 Mar 2020 | 9 hospitals from Hubei, China | Any |
| 16 | Pinato et al. [24] | Peer reviewed | 204 | 59 | Upto 6 Mar 2020 | 8 hospitals in the UK, Italy and Spain | Any |
| 17 | Scarfò et al. [25] | Peer reviewed | 190 | 55 | 28 Mar to 22 May 2020 | Europe | Chronic lymphocytic leukaemia only |
| 18 | de Melo et al. [26] | Preprint | 181 | 60 | 30 Apr to 26 May 2020 | Brazilian National Cancer Institute | Any |
| 19 | Martinez-Lopez et al. [27] | Preprint | 167 | 56 | 1 Mar to 30 Apr 2020 | 73 hospitals in Spain | Multiple myeloma only |
| 20 | Russel et al. [28] | Preprint | 156 | 34 | 29 Feb to 12 May 2020 | Guys Hospital, London, UK | Any |
| 21 | Basse et al. [29] | Preprint | 141 | 26 | 13 Mar to 25 Apr 2020 | Institute Curie Hospital, Paris, France | Any |
| 22 | Barlesi et al. [30] | Conference proceedings | 137 | 20 | 14 Mar to 15 Apr 2020 | Gustave Roussy Cancer Campus, Villejuif, France | Any |
| 23 | Angelis et al. [31] | Peer reviewed | 113 | 29 | 1 Mar to 30 Apr 2020 | Royal Marsden, London, UK | Any |
| 24 | Gupta et al. [32] | Peer reviewed | 112 | 60 | 4 Mar to 4 Apr 2020 | 65 hospitals, USA | Any |
| 25 | Zhang et al. [33] | Peer reviewed | 107 | 23 | 5 Jan to 18 Mar 2020 | 5 hospitals from Wuhan, China | Any |
| 26 | Deng et al. [34] | Peer reviewed | 107 | 6 | Upto 11 Feb 2020 | China | Any |
| 27 | Dai et al. [35] | Peer reviewed | 105 | 12 | 1 Jan to 24 Feb 2020 | 14 hospitals from Hubei, China | Any |
| 28 | Luo et al. [36] | Peer reviewed | 102 | 25 | 12 Mar to 6 May 2020 | New York, USA | Lung cancer only |
| 29 | Hultcrantz et al. [37] | Preprint | 100 | 18 | 10 Mar to 30 Apr 2020 | New York, USA | Multiple myeloma only |
| 30 | Cook et al. [38] | Peer reviewed | 75 | 41 | Upto 18 May 2020 | UK | Multiple myeloma only |
| 31 | Booth et al. [39] | Peer reviewed | 66 | 34 | 1 Mar to 6 May 2020 | England, UK | Haematological malignancies only |
| 32 | Yarza et al. [40] | Peer reviewed | 63 | 16 | 9 Mar to 19 Apr 2020 | Hospital Universitario 12 de Octubre, Madrid, Spain | Any |
| 33 | Assaad et al. [41] | Peer reviewed | 55 | 8 | 1 Mar to 25 Apr 2020 | Centre Léon Bérard, Paris, France | Any |
| 34 | Wang et al. [42] | Peer reviewed | 58 | 14 | 1 Mar to 30 Apr 2020 | New York, USA | Multiple myeloma only |
| 35 | Gonzalez-Cao et al. [43] | Preprint | 50 | 13 | 1 Apr to 17 May 2020 | Spain | Melanoma only |
| 36 | Suleyman et al. [44] | Peer reviewed | 49 | 19 | 9 Mar to 27 Mar 2020 | Henry Ford Health System, Detroit, Michigan, USA | Any |
| 37 | Rogado et al. [45] | Peer reviewed | 45 | 19 | 1 Feb to 7 Apr 2020 | Hospital Universitario Infanta Leonor of Madrid, Spain | Any |
| 38 | Aries et al. [46] | Peer reviewed | 35 | 14 | 11 Mar to 11 May 2020 | Barts Cancer Centre, UK | Haematological malignancies only |
| 39 | Martín-Moro et al. [47] | Peer reviewed | 34 | 11 | 9 Mar to 17 Apr 2020 | Ramón y Cajal University Hospital, Madrid Spain | Haematological malignancies only |
| 40 | Zhang et al. [48] | Peer reviewed | 28 | 8 | 13 Jan to 26 Feb 2020 | 3 hospitals in Wuhan, China | Any |
| 41 | Kalinsky et al. [2] | Peer reviewed | 27 | 1 | 10 Mar to 29 Apr 2020 | Columbia University Irving Medical Center, USA | Breast cancer only |
| 42 | Joharatnam-Hogan et al. [49] | Preprint | 26 | 6 | 12 Mar to 7 Apr 2020 | London, UK | Any |
| 43 | Stroppa et al. [50] | Peer reviewed | 25 | 9 | 21 Feb to 18 Mar 2020 | Piacenza's general hospital, Italy | Any |
| 44 | Ciceri et al. [51] | Peer reviewed | 22 | 11 | 25 Feb to 24 Mar 2020 | San Raffaele Hospital, Lombardy, Italy | Any |
| 45 | Bogani et al. [52] | Peer reviewed | 19 | 3 | Feb and Mar 2020 | Lombardy, Italy | Any |
| 46 | Guan et al. [53] | Peer reviewed | 18 | 3 | 11 Dec 2019 to 31 Jan 2020 | Wuhan, China | Any |
| 47 | Tagliamento et al. [54] | Peer reviewed | 17 | 4 | 10 Mar to 6 Apr 2020 | Italy | Solid cancers |
| 48 | Wang L et al. [55] | Peer reviewed | 15 | 3 | 1 Jan to 6 Feb 2020 | Wuhan, China | Any |
| 49 | He et al. [3] | Peer reviewed | 13 | 8 | 23 Jan to 14 Feb 2020 | Union Hospital and Wuhan Central Hospital, China | Haematological malignancies only |
| 50 | Lattenist et al. [56] | Peer reviewed | 13 | 6 | 13 Mar to 15 May 2020 | Universite´ catholique de Louvain, Brussels, Belgium | Haematological malignancies only |
| 51 | Yu et al. [57] | Peer reviewed | 12 | 3 | 30 Dec 2019 to 17 Feb 2020 | Wuhan, China | Any |
| 52 | Wu et al. [58] | Peer reviewed | 11 | 4 | 9 Jan to 20 Mar 2020 | Hubei, China | Any, with prior exposure to immune checkpoint inhibitors |
COVID-19, coronavirus disease 2019; TERAVOLT, Thoracic cancERs international coVid 19 cOLlaboraTion.
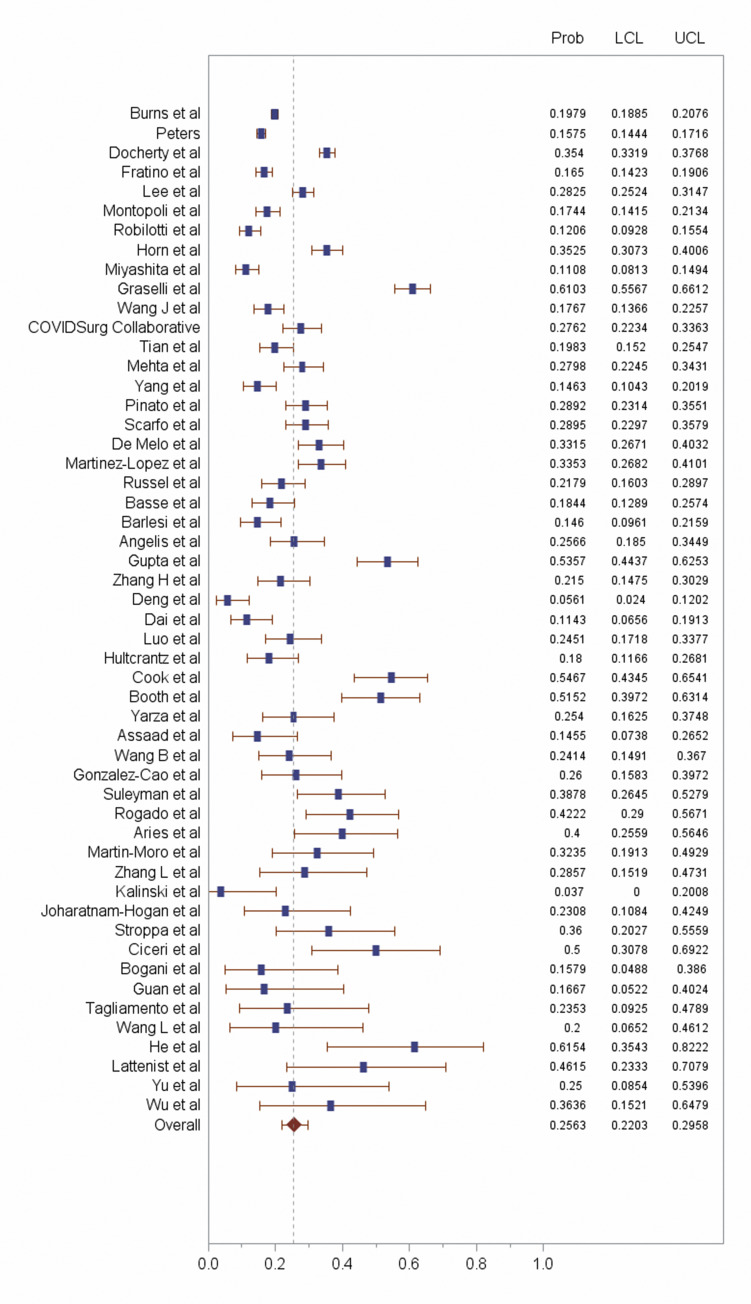
Pooled case mortality rate among patients with cancer and COVID-19 was 25.6% (95% CI: 22.0%–29.5%; I2 = 48.9%) (Fig. 1 ). A sensitivity analysis excluding reports with less than 100 patients showed an I2 = 49.7% for studies with ≥100 patients.
Fig. 1.
Forest plot of 52 studies reporting outcomes in patients with both cancer and COVID-19. COVID-19, coronavirus disease 2019.
4. Discussion
The COVID-19 pandemic has had a major impact on patients with cancer [6], including a sharp reduction in cancer screening and the postponement of ongoing or planned therapy during the initial months of the pandemic, which could result in excess deaths from cancer in the future [7,8].
To restart standard cancer treatment protocols, it is important to quantify the risk of mortality among patients with both cancer and COVID-19, and data generated by large registries such as CCC-19 and Thoracic cancERs international coVid 19 cOLlaboraTion could be valuable in this regard [9,10]. Meta-analyses are also a useful tool to aggregate smaller data sets and estimate mortality risks in this vulnerable population.
The results of our pooled analysis clearly show that the mortality is high among patients with cancer and COVID-19 and should be considered as an independent risk factor, in addition to older age, male sex, black race, current smoker, other comorbidities and so on. As more data become available, it is becoming increasingly clear that within the population of patients with both cancer and COVID-19, there are subsets with greater risk, such as patients with haematological malignancies or lung cancer, which need deeper analysis.
5. Conclusions
Patients with cancer who develop COVID-19 have high probability of mortality. Appropriate and aggressive preventive measures must be taken to reduce the risk of infection with SARS-CoV-2 in patients with cancer and to optimally manage those who do contract the infection.
Author statements
Conflict of interest statement
K.S.S. reports receiving consulting fees from the European Commission outside the submitted work. M.T. reports receiving travel grants from Roche, Bristol-Myers Squibb, AstraZeneca and Takeda and receiving honoraria as a medical writer from Novartis and Amgen outside the submitted work. M.L. reports acting as a consultant for Roche and Novartis and receiving speaker honoraria from Roche, Takeda, Lilly, Novartis, Pfizer and Theramex outside the submitted work. G.C. reports receiving personal fees for consulting, advisory role and speakers’ bureau from Roche/Genentech, Novartis, Pfizer, Lilly, Foundation Medicine, Samsung and Daichii-Sankyo; receiving honoraria from Ellipses Pharma; fees for travel and accommodation from Roche/Genentech and Pfizer outside the submitted work. E.d.A. reports receiving honoraria and advisory board fees from Roche/GNE, Novartis and Seattle Genetics; receiving travel grants from Roche/GNE, GSK and Novartis and receiving research grant to institution from Roche/GNE, AstraZeneca, GSK, Novartis and Servier outside the submitted work. The other authors do not report any conflicts of interest.
Role of funding source
None.
Ethical approval and consent to participate
Not applicable.
Authors' contributions
K.S.S. and E.d.A. conceptualised the manuscript; all authors provided significant inputs; K.S.S. and M.T. collected the data, and R.M.N. performed the analysis. All authors wrote, reviewed, edited and approved this final manuscript.
References
- 1.COVID-19 dashboard. https://coronavirus.jhu.edu/map.html. [Accessed 24 July 2020].
- 2.Kalinsky K., Accordino M.K., Hosi K., et al. Characteristics and outcomes of patients with breast cancer diagnosed with SARS-Cov-2 infection at an academic center in New York City. Breast Cancer Res Treat. 2020;182(1):239–242. doi: 10.1007/s10549-020-05667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He W., Chen L., Chen L., et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34(6):1637–1645. doi: 10.1038/s41375-020-0836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Docherty A.B., Harrison E.M., Green C.A., et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. Published 2020 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peters, S. Keynote address. Flexibility to sustain solidity: addressing new vulnerabilities in cancer at the time of COVID-19. AACR virtual meeting: COVID-19 and cancer. https://www.aacr.org/meeting/aacr-virtual-meeting-covid-19-and-cancer/program/. [Accessed 23 July 2020].
- 6.Saini K.S., de Las Heras B., de Castro J., et al. Effect of the COVID-19 pandemic on cancer treatment and research. Lancet Haematol. 2020;7(6):e432–e435. doi: 10.1016/S2352-3026(20)30123-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai A.G., Pasea L., Banerjee A., et al. Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency. medRxiv. 2020 doi: 10.1101/2020.05.27.20083287. (Preprint) [DOI] [Google Scholar]
- 8.Sharpless N.E. COVID-19 and cancer. Science. 2020;368(6497):1290. doi: 10.1126/science.abd3377. [DOI] [PubMed] [Google Scholar]
- 9.Kuderer N.M., Choueiri T.K., Shah D.P., et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907–1918. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garassino M.C., Whisenant J.G., Huang L.C., et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): first results of an international, registry-based, cohort study. Lancet Oncol. 2020;21(7):914–922. doi: 10.1016/S1470-2045(20)30314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burn E., Tebe C., Fernandez-Bertolin S., et al. The natural history of symptomatic COVID-19 in Catalonia, Spain: a multi-state model including 109,367 outpatient diagnoses, 18,019 hospitalisations, and 5,585 COVID-19 deaths among 5,627,520 people. medRxiv. 2020 doi: 10.1101/2020.07.13.20152454. preprint. [DOI] [Google Scholar]
- 12.Fratino L., Procopio G., Di Maio M., Cinieri S., Leo S., Beretta G. Coronavirus: older persons with cancer in Italy in the COVID-19 pandemic. Front Oncol. 2020;10:648. doi: 10.3389/fonc.2020.00648. Published 2020 Apr 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee L.Y.W., Cazier J.B., Starkey T., et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395(10241):1919–1926. doi: 10.1016/S0140-6736(20)31173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montopoli M., Zumerle S., Vettor R., et al. Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532) Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.04.479. [published online ahead of print, 2020 May 6] S0923-7534(20)39797-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robilotti E.V., Babady N.E., Mead P.A., et al. Determinants of COVID-19 disease severity in patients with cancer. Nat Med. 2020 doi: 10.1038/s41591-020-0979-0. [published online ahead of print, 2020 Jun 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horn L., Whisenant J.G., Torri V., et al. Thoracic Cancers International COVID-19 Collaboration (TERAVOLT): impact of type of cancer therapy and COVID therapy on survival. J Clin Oncol. 2020;38(18_suppl) LBA111-LBA111. [Google Scholar]
- 17.Miyashita H., Mikami T., Chopra N., et al. Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.04.006. [published online ahead of print, 2020 Apr 21] S0923-7534(20)39303-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grasselli G., Greco M., Zanella A., et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.3539. [published online ahead of print, 2020 Jul 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang J., Song Q., Chen Y., et al. Systematic investigations of COVID-19 in 283 cancer patients. medRxiv. 2020 doi: 10.1101/2020.04.28.20083246. [DOI] [Google Scholar]
- 20.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [published correction appears in Lancet. 2020 Jun 9] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tian J., Yuan X., Xiao J., et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):893–903. doi: 10.1016/S1470-2045(20)30309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehta V., Goel S., Kabarriti R., et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov. 2020 doi: 10.1158/2159-8290.CD-20-0516. [published online ahead of print, 2020 May 1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang K., Sheng Y., Huang C., et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020 doi: 10.1016/S1470-2045(20)30310-7. [published online ahead of print, 2020 May 29] S1470-2045(20)30310-30317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinato D.J., Lee A.J.X., Biello F., et al. Presenting features and early mortality from SARS-CoV-2 infection in cancer patients during the initial stage of the COVID-19 pandemic in Europe. Cancers (Basel) 2020;12(7):E1841. doi: 10.3390/cancers12071841. Published 2020 Jul 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scarfò L., Chatzikonstantinou T., Rigolin G.M., et al. COVID-19 severity and mortality in patients with chronic lymphocytic leukemia: a joint study by ERIC, the European Research Initiative on CLL, and CLL Campus. Leukemia. 2020 doi: 10.1038/s41375-020-0959-x. [published online ahead of print, 2020 Jul 9] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Melo AC, Thuler LCS, da Silva JL, et al. Cancer inpatient with COVID-19: a report from the Brazilian National Cancer Institute. https://www.medrxiv.org/content/10.1101/2020.06.27.20141499v2. [Accessed 23 July, 2020]. [DOI] [PMC free article] [PubMed]
- 27.Martinez-Lopez J., Mateos M.V., Encinas C., et al. Multiple myeloma and SARS-CoV-2 infection: clinical characteristics and prognostic factors of inpatient mortality. medRxiv. 2020 doi: 10.1101/2020.06.29.20142455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Russell B., Moss C., Papa S., et al. Factors affecting COVID-19 outcomes in cancer patients − a first report from Guys Cancer Centre in London. medRxiv. 2020 doi: 10.1101/2020.05.12.20094219. (Preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basse C., Diakite S., Servois V., et al. Characteristics and outcome of SARS-CoV-2 infection in cancer patients. medRxiv. 2020 doi: 10.1101/2020.05.14.20101576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barlesi F., Foulon S., Bayle A., et al. AACR virtual meeting. 2020. Abstract CT403 - outcome of cancer patients infected with COVID-19, including toxicity of cancer treatments.https://www.abstractsonline.com/pp8/#!/9045/presentation/10935 [Google Scholar]
- 31.Angelis V., Tippu Z., Joshi K., et al. Defining the true impact of coronavirus disease 2019 in the at-risk population of patients with cancer. Eur J Cancer. 2020;136:99–106. doi: 10.1016/j.ejca.2020.06.027. [published online ahead of print, 2020 Jul 7] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gupta S., Hayek S.S., Wang W., et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.3596. [published online ahead of print, 2020 Jul 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang H., Wang L., Chen Y., et al. Outcomes of novel coronavirus disease 2019 (COVID-19) infection in 107 patients with cancer from Wuhan, China. Cancer. 2020 doi: 10.1002/cncr.33042. [published online ahead of print, 2020 Jun 23] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deng G., Yin M., Chen X., Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit Care. 2020;24(1):179. doi: 10.1186/s13054-020-02902-w. Published 2020 Apr 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dai M., Liu D., Liu M., et al. Patients with cancer Appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov. 2020;10(6):783–791. doi: 10.1158/2159-8290.CD-20-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo J., Rizvi H., Preeshagul I.R., et al. COVID-19 in patients with lung cancer. Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.06.007. [published online ahead of print, 2020 Jun 16] S0923-7534(20)39894-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hultcrantze M., Richter J., Rosenbaum C.A., et al. COVID-19 infections and outcomes in patients with multiple myeloma in New York City: a cohort study from five academic centers. Blood Cancer Discov. July 30 2020 doi: 10.1158/2643-3230.BCD-20-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cook G., John Ashcroft A., Pratt G., et al. Real-world assessment of the clinical impact of symptomatic infection with severe acute respiratory syndrome coronavirus (COVID-19 disease) in patients with multiple myeloma receiving systemic anti-cancer therapy. Br J Haematol. 2020 doi: 10.1111/bjh.16874. [published online ahead of print, 2020 May 21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Booth S., Willan J., Wong H., et al. Regional outcomes of severe acute respiratory syndrome coronavirus 2 infection in hospitalised patients with haematological malignancy. Eur J Haematol. 2020 doi: 10.1111/ejh.13469. [published online ahead of print, 2020 Jun 16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yarza R., Bover M., Paredes D., et al. SARS-CoV-2 infection in cancer patients undergoing active treatment: analysis of clinical features and predictive factors for severe respiratory failure and death. Eur J Cancer. 2020 doi: 10.1016/j.ejca.2020.06.001. [published online ahead of print, 2020 Jun 6] S0959-8049(20)30313-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Assaad S., Avrillon V., Fournier M.L., et al. High mortality rate in cancer patients with symptoms of COVID-19 with or without detectable SARS-COV-2 on RT-PCR. Eur J Cancer. 2020 doi: 10.1016/j.ejca.2020.05.028. [published online ahead of print, 2020 Jun 7] S0959-8049(20)30314-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang B., Van Oekelen O., Mouhieddine T.H., et al. A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward. J Hematol Oncol. 2020;13(1):94. doi: 10.1186/s13045-020-00934-x. Published 2020 Jul 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gonzalez-Cao M., Antonazas-Basa M., Puertolas T., et al. Cancer immunotherapy does not increase the risk of death by COVID-19 in melanoma patients. medRxiv. 2020 doi: 10.1101/2020.05.19.20106971. [DOI] [Google Scholar]
- 44.Suleyman G., Fadel R.A., Malette K.M., et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan detroit. JAMA Netw Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.12270. Published 2020 Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rogado J., Obispo B., Pangua C., et al. Covid-19 transmission, outcome and associated risk factors in cancer patients at the first month of the pandemic in a Spanish hospital in Madrid. Clin Transl Oncol. 2020:1–5. doi: 10.1007/s12094-020-02381-z. [published online ahead of print, 2020 May 25] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aries J.A., Davies J.K., Auer R.L., et al. Clinical outcome of coronavirus disease 2019 in haemato-oncology patients. Br J Haematol. 2020 doi: 10.1111/bjh.16852. [published online ahead of print, 2020 May 18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martín-Moro F., Marquet J., Piris M., et al. Survival study of hospitalised patients with concurrent COVID-19 and haematological malignancies. Br J Haematol. 2020;190(1):e16–e20. doi: 10.1111/bjh.16801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang L., Zhu F., Xie L., et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31(7):894–901. doi: 10.1016/j.annonc.2020.03.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Joharatnam-Hogan N., Hochhauser D., Shiu K.K., et al. Outcomes of the 2019 Novel Coronavirus in patients with or without a history of cancer - a multi-centre North London experience. medRxiv. 2020 doi: 10.1101/2020.04.16.20061127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stroppa E.M., Toscani I., Citterio C., et al. Coronavirus disease-2019 in cancer patients. A report of the first 25 cancer patients in a western country (Italy) Future Oncol. 2020;16(20):1425–1432. doi: 10.2217/fon-2020-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ciceri F., Castagna A., Rovere-Querini P., et al. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin Immunol. 2020;217:108509. doi: 10.1016/j.clim.2020.108509. [published online ahead of print, 2020 Jun 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bogani G., Ditto A., Bosio S., Brusadelli C., Raspagliesi F. Cancer patients affected by COVID-19: experience from Milan, Lombardy. Gynecol Oncol. 2020 doi: 10.1016/j.ygyno.2020.06.161. [published online ahead of print, 2020 Jun 10] S0090-8258(20)31976-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guan W.J., Liang W.H., Zhao Y., et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi: 10.1183/13993003.00547-2020. Published 2020 May 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tagliamento M., Lambertini M., Genova C., et al. Call for ensuring cancer care continuity during COVID-19 pandemic. ESMO Open. 2020;5(3) doi: 10.1136/esmoopen-2020-000783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang L., He W., Yu X., et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639–645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lattenist R., Yildiz H., De Greef J., Bailly S., Yombi J.C. COVID-19 in adult patients with hematological disease: analysis of clinical characteristics and outcomes. Indian J Hematol Blood Transfus. 2020:1–5. doi: 10.1007/s12288-020-01318-4. [published online ahead of print, 2020 Jul 7] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6(7):1108–1110. doi: 10.1001/jamaoncol.2020.0980. [published online ahead of print, 2020 Mar 25] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Q., Chu Q., Zhang H., et al. Clinical outcomes of coronavirus disease 2019 (COVID-19) in cancer patients with prior exposure to immune checkpoint inhibitors. Cancer Commun (Lond) 2020 doi: 10.1002/cac2.12077. [published online ahead of print, 2020 Jul 15] [DOI] [PMC free article] [PubMed] [Google Scholar]