Abstract
Background:
Oral feeding is one of the most complex maturational skills of infancy. Difficulties with feeding require specialized attention, and if not well managed, may prolong the newborn's hospital length of stay. This is particularly true for prenatally opioid exposed (POE) infants. A paucity of literature exists characterizing feeding behaviors of POE infants, yet feeding problems are common.
Purpose:
The purpose of this integrative review was to synthesize and critically analyze the evidence that characterizes feeding behaviors in full-term, POE infants.
Methods/Search Strategy:
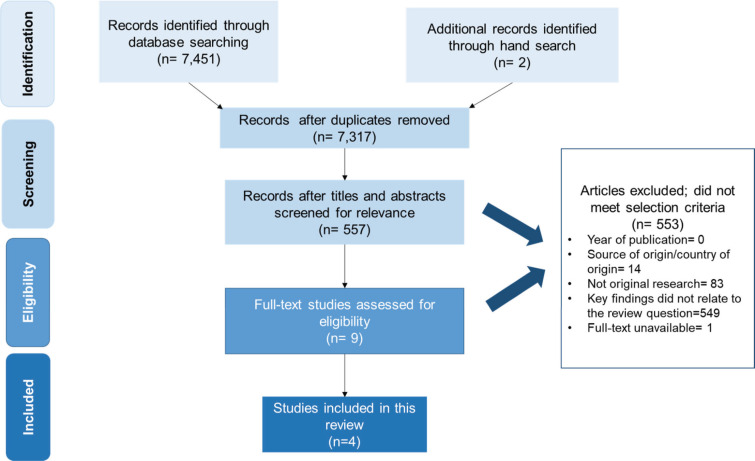
The electronic databases of CINAHL, PubMed, Scopus, and PsycINFO were used. Inclusion criteria were studies in English, conducted from 1970 to 2019, with participant samples consisting of infants with prenatal opioid exposure, born full-term, and between 38 and 40 weeks of gestation. Based on the inclusion criteria, our search yielded 557 articles. After further screening, only 4 studies met our full inclusion/exclusion criteria. These studies were analyzed for evidence of infant feeding behaviors, including characterization of problematic feeding behavior for POE infants.
Findings/Results:
Our findings revealed inconsistencies in characterization of feeding behaviors among POE infants. A synthesis of the most common evidence-based behaviors was constructed. Infant feeding behaviors were identified and grouped into 2 major behavior domains: (1) typical feeding behavior and (2) problematic feeding behavior.
Implications for Practice and Research:
Feeding behaviors related to sucking and behavioral states may be different in POE infants. Further examination of effective assessment methods and the categorization of infant feeding behaviors are warranted for use in the development of evidence-based, targeted intervention.
Keywords: bottle feeding, breastfeeding, feeding behavior, neonatal abstinence syndrome, prenatal exposure delayed effects, sucking behavior
Perinatal opioid use disorders are a rapidly growing public health concern that has significantly increased healthcare costs.1 Paralleling the increased rates of opioid use disorders in pregnancy is the increase in infants born prenatally exposed to opioids.2 The national incidence of prenatal opioid exposure increased from 1.5 to 8.0 per 1000 hospital births from 2004 to 2014.3 Following in utero exposure, opioid withdrawal may cause infants to experience both symptoms of central nervous system and gastrointestinal irritability of varying severity.4 Management of these complex symptoms typically requires a costly and lengthy hospital stay, with care often occurring in the neonatal intensive care unit (NICU).2,5
Admissions to the NICU for prenatally opioid exposed (POE) infants increased 5-fold between 2000 and 2012.2,5 Furthermore, neonatal hospital costs occurring because of prenatal opioid exposure increased from 1.6% in 2004 to 6.7% in 2014 for births covered by Medicaid.3 The high cost of hospital care is primarily due to the considerable treatment needs associated with prenatal opioid exposure and the potential subsequent diagnosis of neonatal abstinence syndrome (NAS).1
Traditionally, “neonatal abstinence syndrome” is the term used to describe a group of withdrawal symptoms that result from in utero substance exposure.6 However, more recently, the term “neonatal opioid withdrawal syndrome” (NOWS) has been used to describe a distinct form of NAS, with clinical characteristics and management techniques specific to withdrawal from opioids.1 Infants with NOWS often require extensive pharmacological and/or nonpharmacological nursing care to support necessary behavioral and biological processes such as feeding.2,4
Feeding is one of the most complex tasks required of young infants, including full-term POE infants.7 Nonetheless, little empirical evidence exists to characterize the feeding behaviors of POE infants. Difficulty with feeding is extremely common in POE infants, regardless of whether their symptoms are characterized as NOWS.8 Of particular interest is the fact that these infants appear to have different patterns of feeding behavior than non–opioid-exposed infants.8–11
Research has demonstrated that neonatal clinicians may benefit from monitoring an infant's cues or behaviors in combination with suck-swallow-breathe coordination and volume intake measurements.12 In comparison with other term infants, compromised infants, such as those born with prenatal opioid exposure, may face significant challenges in exhibiting feeding readiness behaviors.13 Early feeding difficulties are often persistent and extend beyond hospital discharge.
Early assessment and implementation of strategies to support feeding and nutrition are essential for optimization of nutritional intake, oral feeding skill development, and prevention of long-term feeding problems in high-risk populations.14 Because feeding is an essential activity for infants, further complicated by prenatal opioid exposure and NOWS, there is a need for further study of feeding behaviors specific to full-term, POE infants. Nonetheless, a dearth of understanding regarding the phenomena of feeding and feeding behaviors exists for POE infants. Therefore, the purpose of this review is to synthesize and analyze the existing literature on feeding behaviors of full-term, POE infants and/or those diagnosed with NOWS. Finally, we offer implications for nursing clinical practice and research.
METHODS
Objective
A modified version of the Meta-analyses of Observational Studies in Epidemiology (MOOSE) guidelines was used to guide interpretation of our results.15 The objective of this review was to identify the current science that characterizes feeding behaviors in POE infants. Our goal was to answer 2 key questions:
What types of feeding behaviors are observed in POE infants?
What are the gaps in existing knowledge related to infant feeding behavior in POE infants?
Data Sources and Extraction
A medical librarian-assisted literature search was conducted using the Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed, Scopus, PsycINFO, and a hand-searched reference list of articles obtained. Infant feeding is considered a nursing function; thus, we included the database CINAHL. PubMed was chosen as the largest searchable biomedical database. Scopus was chosen as the largest abstract and citation database of peer-reviewed literature: scientific journals, books, and conference proceedings. Finally, PsycINFO was chosen as a focused resource of interdisciplinary, behavioral, and social science research and literature. Common key words used for searches included breastfeeding, bottle feeding, feeding behavior, sucking behavior, in utero exposure, and NAS (refer to Table 1 for exhaustive list of used search terms). Searches were completed using Boolean operators “AND” and “OR” with each search term (Table 1).
TABLE 1. Database Search Strategies.
| Database | Infant Feeding Search Strategy | Prenatal Opioid Exposure Search Strategy |
|---|---|---|
| CINHAL | ( TITLE-ABS-KEY ( breastfeeding OR “breast feeding” OR “bottle feeding” OR bottlefeeding OR “feeding behavior” OR “Infant Nutritional Physiological Phenomena” OR “sucking behavior” ) ) | ( ( TITLE-ABS-KEY ( ( ( substance OR drug ) W/3 ( exposure OR exposed ) ) AND ( “in utero” OR uterus OR pregnan* OR prenatal OR fetal OR fetus ) ) ) OR ( TITLE-ABS-KEY ( ( neonatal OR neonate ) W/2 ( withdraw OR withdrawal ) ) ) OR ( TITLE-ABS-KEY ( prenatal AND exposure AND delayed AND effects ) ) OR ( TITLE-ABS-KEY ( “neonatal abstinence syndrome” OR nas ) ) ) |
| PubMed | ( TITLE-ABS-KEY ( breastfeeding OR “breast feeding” OR “bottle feeding” OR bottlefeeding OR “feeding behavior” OR “Infant Nutritional Physiological Phenomena” OR “sucking behavior” ) ) | ( ( TITLE-ABS-KEY ( ( ( substance OR drug ) W/3 ( exposure OR exposed ) ) AND ( “in utero” OR uterus OR pregnan* OR prenatal OR fetal OR fetus ) ) ) OR ( TITLE-ABS-KEY ( ( neonatal OR neonate ) W/2 ( withdraw OR withdrawal ) ) ) OR ( TITLE-ABS-KEY ( prenatal AND exposure AND delayed AND effects ) ) OR ( TITLE-ABS-KEY ( “neonatal abstinence syndrome” OR nas ) ) ) |
| Scopus | ( TITLE-ABS-KEY ( breastfeeding OR “breast feeding” OR “bottle feeding” OR bottlefeeding OR “feeding behavior” OR “Infant Nutritional Physiological Phenomena” OR “sucking behavior” ) ) | ( ( TITLE-ABS KEY ( ( ( substance OR drug ) W/3 ( exposure OR exposed ) ) AND ( “inutero” OR uterus OR pregnan* OR prenatal OR fetal OR fetus ) ) ) OR ( TITLE-ABS-KEY ( ( neonatal OR neonate ) W/2 ( withdraw OR withdrawal ) ) ) OR ( TITLE-ABS-KEY ( prenatal AND exposure AND delayed AND effects ) ) OR ( TITLE-ABS-KEY ( “neonatal abstinence syndrome” OR nas ) ) ) |
| PsycINFO | ( TITLE-ABS-KEY ( breastfeeding OR “breast feeding” OR “bottle feeding” OR bottlefeeding OR “feeding behavior” OR “Infant Nutritional Physiological Phenomena” OR “sucking behavior” ) ) | ( ( TITLE-ABS-KEY ( ( ( substance OR drug ) W/3 ( exposure OR exposed ) ) AND ( “in utero” OR uterus OR pregnan* OR prenatal OR fetal OR fetus ) ) ) OR ( TITLE-ABS-KEY ( ( neonatal OR neonate ) W/2 ( withdraw OR withdrawal ) ) ) OR ( TITLE-ABS-KEY ( prenatal AND exposure AND delayed AND effects ) ) OR ( TITLE-ABS-KEY ( “neonatal abstinence syndrome” OR nas ) ) ) |
Study Selection
Prospective studies were identified through electronic and manual searches. References were retrieved and screened. Then relevant articles were kept for further review and synthesis. The inclusion criteria were peer-reviewed research studies in journals from various discipline journals from 1970 to 2019. The dates for article selection were chosen on the basis of historical evidence of the introduction of the Comprehensive Drug Abuse Prevention and Control Act of 1971. The purpose of this law was to improve the manufacturing, distribution, and provision of controlled substances. In addition, it led to an increase in the conduction of research of drug abuse,16 including studies related to POE infants.
Opioid use disorders in pregnancy are associated with an increased incidence of preterm birth.6,17 However, a paucity of literature exists examining NAS/NOWS manifestations in preterm infants, and little is understood regarding how NAS/NOWS is characterized in preterm populations.17 Therefore, the population of interest selected for this integrative review included samples of full-term infants born between 38 and 40 weeks.
Because of global differences in guidelines for managing NOWS, only those studies conducted in the United States and printed in English were considered eligible for inclusion. Studies were not included if they were not original research or if the full publication was not available. Systematic reviews were also excluded. This group of criteria resulted in 7 key items for extraction (Table 2).
TABLE 2. Inclusion and Exclusion Criteria for Literature Review.
| Criteria | Include | Exclude |
|---|---|---|
| Date | Studies conducted after 1970 | Studies conducted before 1970 |
| Source of origin/country of origin | United States | Studies conducted outside of the United States |
| Language | English language | Studies not in English language |
| Purpose | Publications with a purpose related to infant feeding behaviors in infants with prenatal opioid exposure | Publications with a purpose not related |
| Study population | Sample includes infants with prenatal opioid exposures | Sample does not include infants with prenatal opioid exposure |
| Context | Key findings that relate to the review question | Key findings that do not relate to review question |
| Publication | Full text of article available Primary empirical study Peer-reviewed journal article |
Grey literature, reports, conference proceedings |
The CINHAL, PubMed, Scopus, and PsycINFO searches resulted in 7453 articles with no relevant systematic reviews. All of the articles were retrieved and screened, with 136 duplicates deleted. Titles and abstracts of the remaining articles were reviewed for relevance. Of those, 557 remained (6760 were excluded) for further analysis. Of the remaining articles, 546 were excluded, as they did not meet inclusion criteria. The remaining articles were reviewed in their entirety for relevance. Studies were excluded if they were not original research articles, if they were not conducted in the United States, or if they were related to infant feeding but did not include feeding behaviors (see Figure 1 for details about exclusions). Four studies were included in the full review process (Figure 1).
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram for the scoping review process.
RESULTS
Description of the Studies
While there were several clinical articles describing the most common gastrointestinal symptoms observed with NAS/NOWS, research on the specific feeding behaviors of infants with NOWS was limited. Table 3 provides further details of the studies in this review, including purpose, population/setting, research design, tools used to gather data, infant feeding behaviors reported, and main findings when that information was supplied for each included study. Three studies included mother–infant dyads,8,10,11 while only 1 study included POE infants.18 Of the 3 studies that included dyads, 1 study included a comparison group with prenatal exposure to cocaine11 while another study included dyads with opioid exposure to include either heroin or methadone.10 The third study did not have a comparison group and included only dyads with opioid exposure.8 All studies in this review evaluated infant feeding with infants and/or mothers prenatally exposed to opioids.
TABLE 3. Studies of Infant Feeding Behaviors in Infants With Prenatal Opioid Exposure.
| Author and Year, Journal | Purpose | MethodsDesign/SettingAssessment Tool | Sample of Interest | Characteristics/Behavior Reported | Main Findings |
|---|---|---|---|---|---|
| Kron et al10 (1976), Journal of Pediatrics | Apply objective measures of nutritive sucking to (1) evaluate the relative severity of neonatal abstinence in relation to maternal enrollment in the methadone clinic and (2) study currently recommended pharmacotherapy for neonatal narcotic abstinence |
|
|
|
In infants born to mothers actively using heroin, sucking measures were significantly reduced relative to normal control subjects. The sucking behavior of infants born to mothers on methadone was significantly depressed compared with that of infants of active heroin users. |
| LaGasse et al11 (2003), Archives of Disease in Childhood Fetal Neonatal Education | To evaluate feeding difficulties and maternal behavior during a feeding session with 1-mo-old infants prenatally to cocaine and/or opiates |
|
|
|
Opiate-exposed infants and their mothers both contributed to increased arousal and heightened feeding behavior |
| Gewolb et al18 (2004), Developmental Medicine & Child Neurology | To delineate quantitatively differences in suck-swallow-respiration coordination during feeding in term infants exposed to drugs in utero. |
|
|
|
Integration of respiratory efforts into the suck-swallow rhythms of infant feeding is a key factor in achieving successful nutrition with the least expended energy. |
| Maguire et al8 (2015), Advances in Neonatal Care | Describe the infant behaviors that disrupt feeding in infants with neonatal abstinence syndrome |
|
N = 11: mother–infant dyads with opioids exposure |
|
Feeding behavior occurred only 24% of the time, while fussing and crying occurred 51% of the time. Fussing was the primary transitional behavior from one category to another. Infants who did not complete their feeding had nearly twice the mean number of fussing episodes as those who completed their feeding. |
Within the studies included in our review, different assessment tools were used to evaluate feeding behaviors. Video recordings including their coding schemas were used in 2 studies.8,11 The coding schema used were predominately developed for use with healthy term or preterm infants. In the other 2 studies, an apparatus was used to measure the physical characteristics of sucking.10,18 Investigators for all studies confirmed maternal drug use through self-report, positive toxicology screens of mothers, and/or meconium toxicology with presumptive positive screens confirmed with gas chromatography-mass spectrometry.8,10,11,18
Summary of Evidence
Three of the studies in this review compared feeding behavior differences between POE and non-POE infants.10,11,18 Only 1 study included a homogeneous sample of POE infants.8 Infant feeding observations were included in all studies. However, definitions used to characterize the feeding behaviors varied. LaGasse et al11 defined behaviors observed during feeding as competence to include appropriateness of state, infant responsiveness, and ease of feeding.
In 3 of the 4 studies, researchers discovered greater feeding problems (nipple rejection/refusal, dribbling, spitting up, and coughing) in POE infants than in non–opioid-exposed infants.10,11,18 Maguire et al8 found that similar problematic behaviors were displayed by POE infants. However, these behaviors were referred to as “fussing” behaviors.
Based on our synthesis, we identified 2 infant feeding behavior domains that we used to organize the studies by behavioral measures. Studies that examined typical feeding behaviors such as sucking, breathing, and feeding were grouped under Infant Feeding Behavior in domain I. Studies that examined ineffective feeding behaviors such as sleeping/sedated, resting (drowsy), and fussing/crying were grouped under Problematic Feeding Behavior in domain II. Table 4 summarizes the studies first in chronological order and then in relationship to their behavior domains.
TABLE 4. Literature Review of Key Outcome Domainsa.
| Study Authors | Behaviors | |||||||
|---|---|---|---|---|---|---|---|---|
| Sucking | Breathing | Feeding | Competence/Problems | Arousal | Sleeping/Sedated | Resting (Drowsy) | Fussing/Crying | |
| Kron et al10 (1976) | X | X | ||||||
| LaGasse et al11 (2003) | X | X | X | |||||
| Gewolb et al18 (2004) | X | X | X | |||||
| Maguire et al8 (2015) | X | X | X | X | X | |||
aDescription of study domains: (1) sucking characteristics included (a) sucking rate (sucks per minute), (b) average suck duration (seconds per suck), (c) percentage time during the experiment that the infant is actively sucking (suck time/total time x 100), and (d) sucking burst (interburst interval, proportion sucking, and burst per minute); (2) breathing characteristics included swallow-breath and breath-breath intervals; (3) feeding characteristics included feeding, nutrient consumption, and swallowing; (4) competence characteristics included the appropriateness of state for feeding; and (5) arousal characteristics include the predominant behavioral state.
Domain I: Typical Infant Feeding Behaviors
In the following section, findings of the review studies are discussed in terms of typical infant feeding behaviors.
Sucking
Across studies, the most frequently cited infant feeding behavior reported during assessment was sucking.10,11,18 Sucking characteristics included (1) sucking rate (sucks per minute), (2) average suck duration (seconds per suck), (3) percentage time actively sucking (suck time/total time × 100), and (4) sucking burst (interburst interval, proportion sucking, and burst per minute). Overall, opioid-exposed infants demonstrated differences in sucking patterns; however, results were inconsistent across studies.10,11,18
For example, Kron et al10 found that the average peak pressure per suck was significantly (P < .05) different between POE and non-POE infants. However, differences in the average suck duration did not vary significantly between the 2 groups.10,18 Gewolb et al18 did not observe significant differences in suck rate, sucks per run, or in suck rhythm between POE and non-POE infants at 1 month of age. In contrast, LaGasse et al11 observed that POE infants displayed longer sucking bursts (unadjusted, P = .044; adjusted, P = .004) but fewer bursts per minute (unadjusted, P = .001; adjusted, P = .001). Overall, the research suggests that POE infants may demonstrate some differences in sucking characteristics; however, the findings are inconsistent.
Breathing
During feeding observations, Gewolb et al18 examined swallow-breath and breath-breath intervals. Swallow-breath intervals and coefficients of variation were calculated on the basis of swallows in runs (or succession). Breath-breath intervals and coefficients of variation were calculated for breaths occurring during swallow runs of at least 3 consecutive swallows. Apneic runs were also calculated by observing runs of at least 3 swallows not associated with breathing movements, divided by total run-swallows. The researchers observed significantly more apneic swallows in POE infants (mean: 5.3%, SEM: 1.7% vs mean: 0.9%, SEM: 0.4%; P < .02). Findings from the study suggest that abnormalities associated with sucking may be different in POE infants when compared with non–opioids-exposed infants.
Feeding
Three of the 4 studies included the feeding behavior domain, which included the subcategories of feeding, nutrient consumption, and swallowing. Maguire et al8 focused on 3 behaviors including latched on the nipple; sucking and swallowing in a rhythmical pattern, and an occasional, brief (up to 5 seconds) pause. Feeding was measured over a period of 30 minutes or less. The duration of feeding episodes was characterized by continuous sucking and swallowing in a rhythmic patter, with occasional, brief pauses lasting for 5 seconds or less. In this study, feeding behavior accounted for 24% of the duration of the videotape, with the number of feeding episodes ranging from 2 to 34 (M = 16.1; SD = 9.6). On average, infants spent 8.5 minutes feeding.
Gewolb et al18 measured feeding efficiency as volume per suck or volume per swallow in milliliters. At 0 to 3 days of life, non-POE infants had significantly greater (P < .005) swallowing efficiency than POE infants. However, by 1 month of age, POE infants ingested comparable amounts of formula per swallow as non-POE infants. Likewise, Kron et al10 observed nutrient consumption (milliliter per minute) between POE and non-POE infants. They found that POE infants had significantly less nutrient consumption per feeding than non-POE infants (P < .01). Overall, differences in feeding efficiency were noted among POE infants and non-POE infants across studies.
Domain II: Problematic Feeding Behavior
For the purposes of this review, all behaviors listed in this domain are characterized as problematic feeding behavior.
Competence/Problems
LaGasse et al11 examined the specific concept of competence. Although only 1 study identified this concept as a feeding behavior, it was included in the analysis as it characterized the infant state or behavior in relation to feeding. These researchers described competence as the appropriateness of state for feeding, ease of feeding, and infant's responsiveness.11 Higher scores in this category indicated greater competence. The main effects for opiate exposure on competence failed to reach significance (unadjusted, P = .979; adjusted, P = .801). Overall, there were no significant differences between opioid-exposed and non–opioid-exposed infants in the measure of competence.11
Although the term “competence” was not used to describe the behaviors noted, LaGasse et al11 studied the associated behaviors in a sample of 1028 infants. The researchers found that POE infants displayed several behaviors consistent with feeding problems. These behaviors included rejection of the nipple, hiccoughing, spitting up, and coughing.11 Prenatally opioid exposed infants showed more feeding problems (unadjusted, P = .031; adjusted P = .028) than non-POE infants.
Arousal
While typical feeding behaviors were identified across the studies, 2 studies examined states of arousal and the impact this had on feeding effectiveness.8,11 The researchers also examined states of arousal by grouping several states under the category of “arousal.”11 LaGasse et al11 defined arousal as the predominant state or level of arousal of the infant. The researchers also examined states of arousal by grouping several states under the category of “arousal.”11 Behaviors were rated on a 4-point scale including sleeping, drowsy, alert, and fussy/crying (state definitions of the Brazelton Scale).11 In this study, POE infants showed higher arousal (unadjusted, P = .002; adjusted, P = .021) than non-POE infants.
Similarly, Maguire et al8 examined infant behavioral states that disrupt feeding in infants with NAS. However, rather than explicitly defining infant states during feeding as arousal, the researcher characterized the states as separate categories for problematic feeding.8 Behaviors observed during feeding included feeding, sleeping/sedated, resting, and crying.8 Later, these behaviors are described in detail.
Sleeping/Sedated
In the investigation conducted by Maguire et al,8 behaviors of sleeping and sedated were grouped into one behavioral category due to difficulties in differentiating between the behaviors during the observation period. Maguire et al8 categorized sleeping/sedated behavior as a state in which the infant's eyes were closed or open with a glassy appearance, or if the infant's limbs or facial expressions were limp. The category sleeping/sedated was also coded if the mother verbalized that the infant was asleep. Five of the POE infants (n = 11) displayed sleeping/sedated behavior during the feeding observation (45%) and accounted for 12.1% of the entire feeding period.8
Resting (Drowsy)
Resting was categorized as a state in which the infant was not feeding for greater than 5 seconds but appeared to remain awake. Infants in this category displayed relaxed facial features.8 Resting behavior occurred during 12% of the total feeding time for 9 of the infants (82%).8
Fussing/Crying
Maguire et al defined fussing behaviors as, “the infant averting their face, pulling or turning away, or otherwise resisting; grimacing or frowning; hyperextending arms or legs; flailing arms; splaying fingers; pushing or spitting out the nipple; and vocal objections like whimpering, but not a robust cry.”8(pp432) Fussing behavior accounted for 40.2% of the feeding episodes and was found to be the behavior most likely to disrupt the feeding. Fussing largely characterized the transition from feeding to not feeding. Disrupted feeding occurred in every observation with every infant at least once and occurred almost 3 times more often (n = 117) as the next most frequent behavior (sleeping/sedated, n = 42).
Maguire et al8 characterized crying behaviors as a loud outburst of crying. Crying was classified both independently and in association with other fussing behaviors. Crying behaviors were observed in 6 infants (55%). When combined with the behavior of fussing, crying and fussing accounted for 51% of the feeding episode.8 Overall, when compared with all other feeding behaviors, a predominance of fussing behaviors occurred among participants in this study.
DISCUSSION
Our findings reveal a significant gap in the science related to full-term, POE infants. We discovered that research on infant feeding behaviors among POE infants is lacking and the research that does exist is riddled with inconsistencies in the way infant feeding behaviors are characterized. Nonetheless, we attempted to compile this evidence to provide a general understanding of the most common behaviors. This was necessary since prenatal opioid exposure is a growing public health concern; therefore, evidence-based practices are needed to better support the care and nutrition of POE infants.
Problematic feeding among full-term, POE infants is often the driver behind their associated lengthy and costly hospital stay. Since infant feeding lies directly within the domain of nursing care, the lack of evidence we discovered is concerning and has great significance for our practice.8,10,18 More specifically, our review uncovered that POE infants are more likely to experience uncoordinated suck-swallow-breath reflex, which may present a significant safety concern.
Furthermore, our integrative review identified that in addition to problems of suck-swallow-breath coordination, POE infants struggle with feeding efficiency.10,11,18 For example, Gewolb et al18 reported that POE infants displayed less feeding efficiency than non-POE infants. These researchers also discovered that POE infants had more apneic swallow episodes than their non-POE counterparts during the first 3 days of life.18 Furthermore, when examining differences among the type of opioid exposure, Kron and colleagues10 reported poor sucking patterns in infants exposed to methadone, when compared with infants exposed to heroin, and non-POE infants.
The findings of our integrative review show that feeding may be a major challenge for POE infants. As such, POE infants deserve greater nursing support through the development of more targeted and individualized nursing intervention and care. Nursing research that results in the better categorization of common problematic feedings behaviors is critical for nursing practice to involve into more supportive therapeutic interventions that will help POE infants thrive. Findings should support the standardization of measures to assess infant feeding behaviors and cues specific to POE infants. These tools should be applicable to the assessment of early feeding skills and effectively address the issue of problematic feeding behaviors common to POE infants.
Limitations
While this integrative review has the strength of being the first of its kind to examine the evidence regarding feeding behaviors in infants with prenatal opioid exposure, there are several limitations. First, there was exclusive access to North American databases and sources in the English language. An expanded review with international, multilanguage sources would be of use to continue to map the current state of our knowledge and understanding of practice in the care of these infants. Likewise, studies included in this review were limited by geographical area. Only studies from the United States were included in this analysis; thus, it may be beneficial to extend the literature search beyond the US border to gain a broader perspective on the phenomena of interest.
In general, the studies included small sample sizes and samples that do not fully represent the diversity of racial and ethnic groups, making it difficult to generalize the findings. In addition, this article specifically looked at term infants. Infants younger than 37 weeks have an array of feeding behaviors that differ from those of the term infants. Efforts to obtain larger sample sizes and an examination of covariates such as maternal parity and age, infant gestational age, type of opioid exposure, severity of infant withdrawal, symptom management strategies, and contextual conditions are warranted as they may all influence infant behavior and feeding patterns.
Our emphasis in this integrative review on the characterization of feeding behaviors in infants with prenatal opioid exposure necessarily resulted in the exclusion of other subsets of the literature. Systematic reviews and gray literature (those produced outside of the traditional academic publishing channels) were excluded. Consequently, there may be excluded studies that shed light on the characterization of feeding behaviors in infants with prenatal opioid exposure. Finally, the reliance on observational data limits the interpretations and conclusions drawn. The number and inconsistency of diagnostic tools support the need to identify more formalized infant feeding assessments in this population. Despite the limitations, these results have implications for practice and research.
Implications for Nursing Practice and Research
The feeding behaviors displayed by POE infants may present significant challenges for caregivers attempting to successfully feed these infants.18 Findings from most of the studies included in this review suggest that infants in this population may have increased rates for uncoordinated feeding patterns.8,11 In addition, POE infants have been reported to display hyperarousal during feedings and increased fussiness, further complicating feeding episodes. For this reason, it is important to identify feeding strategies that nurses may employ to support feeding success in full-term POE infants. Findings from one study revealed that a sample of NICU nurses developed a characteristic skill set to promote successful feedings for POE infants.4 These strategies included adequately managing withdrawal signs, positioning of the infant, and comfort techniques such as vertical rocking, patting, swaddling, and making loud, rhythmic shushing noises.4
The literature also supports the importance of including the mother in the caregiving process of her infant, as well as supporting the maternal–infant dyad as a whole.19,20 Often, women with substance use disorder feel stigmatized by nurses and other healthcare providers. This stigma and judgment impede the mother's involvement in the care of her infant.21 Cleveland and Gill20 suggested that efforts should be made to include the mother in the care of her infant. Nurses in this study reported encouraging mothers to attend as many feeding sessions as possible and used this time to teach mothers about their infant's cues and feeding behaviors.20
In addition, a need exists in the identification and description of specific maternal behaviors that may influence the feeding patterns of infants with prenatal opioid exposure.8 LaGasse et al11 found that mothers with opioid exposure showed increased rates of maternal stimulation during the feeding session when compared with their healthy counterparts. Behaviors associated with maternal stimulation included vocalizations, stroking, and kissing the infants. Mothers in this group also had heightened feeding activity. For example, participants in this group had higher usage rates of nipple stimulation, burping of the infant, and moving of the infant. Mothers of infants with prenatal opioid exposure also displayed less flexible behaviors including behaviors associated with confidence and appropriateness of behavior.
These behaviors can be associated with problematic feeding patterns if they are not responsive to the infant's cues. Thus, future research should examine interactions between the maternal–infant dyad during feedings. Continued efforts should be made to describe maternal behaviors that influence infant feeding experiences. Targeted interventions should be developed in response to these findings. Inclusion of mothers in the development of such interventions can help make them feel supported through the infant's opioid withdrawal process, as well as improve growth–fostering interactions with the goal of improving infant health outcomes.
To date, little is known about the role of the father in the feeding experience of POE infants. However, consideration should also be given to the influence of fathers on the feeding environment and infant's behaviors. Moreover, nurses may use feedings as a time to encourage parents and nurture the parent–infant relationship.4,19
CONCLUSION
Feeding is an important task in the spectrum of infant's health and development, especially when the newborn period is complicated by a medical condition such as prenatal opioid exposure. Furthermore, the regulatory process of feeding may be difficult to characterize in prenatally opioid-exposed infants. Moreover, adequate assessment and categorization of infant feeding problems are important in the development of targeted interventions to aid in managing the care of compromised infants. A paucity of literature exists to guide recommendations for practice in this population. Therefore, a review of current literature on infant feeding behaviors of POE infants is timely and has significant potential for implementation and dissemination in several respects.
Infant feeding assessments require little time or effort from nursing staff and consequently can be easy to implement in the real-world setting of a busy NICU. Building scientific evidence to support the identification of infant feeding problems is essential. Future prospective studies on feeding behaviors, growth, and developmental outcomes for POE infants are urgently needed. These developments may result in significant cost savings through shorter and less costly hospital admissions. The development of targeted feeding interventions among infants with NOWS will improve health outcomes throughout infancy and across the life span.
Summary of Recommendations for Practice and Research.
| What we know: |
|
| What needs to be studied: |
|
| What can we do today: |
|
Acknowledgement
The authors would like to acknowledge Emme Lopez, MLS, the UT Health San Antonio Librarian Liaison to the School of Nursing, for her assistance in identifying the reviewed sample of manuscripts.
Footnotes
For more than 137 additional continuing education articles related to neonatal topics, go to NursingCenter.com.
This work was funded by the NIDA T32 Postdoctoral Training Program (T32DA031115) at the University of Texas Health Science Center, San Antonio, Texas.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Klaman S, Issacs K, Leopold A, et al. Treating women who are pregnant and parenting for opioid use disorder and the concurrent care of their infants and children: literature review to support national guidance. J Addict Med. 2017;11(3):178–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patrick S, Schumacher R, Bennyworth B, Krans E, McAllister J, Davis M. Neonatal abstinence syndrome and associated health care expenditures. JAMA. 2012;307(18):1934–1940. [DOI] [PubMed] [Google Scholar]
- 3.Winkelman T, Villapianp N, Kozhimannil K, Davis M, Patrick S. Incidence and costs of neonatal abstinence syndrome among infants with Medicaid: 2004-2014. Pediatrics. 2018;141(4):e20173520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maguire D, Shaffer-Hudkins E, Armstrong K, Clark L. Feeding infants with neonatal abstinence syndrome: finding the sweet spot. Neonatal Netw. 2018;37(1):11–18. [DOI] [PubMed] [Google Scholar]
- 5.Patrick S, Davis M, Lehman C, Cooper W. Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. J Perinat. 2015;35(8):650–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American College of Obstetricians and Gynecologists. Committee Opinion No. 711 summary. Obstet Gynecol. 2017;130(2):488–489. [DOI] [PubMed] [Google Scholar]
- 7.Briere CE, McGrath J, Cong X, Cusson R. State of the science: a contemporary review of feeding readiness in the preterm infant. J Perinat Neonatal Nurs. 2014;28(1):51–58. [DOI] [PubMed] [Google Scholar]
- 8.Maguire DJ, Rowe MA, Spring H, Elliott AF. Patterns of disruptive feeding behaviors in infants with neonatal abstinence syndrome. Adv Neonatal Care. 2015;15(6):429–439; quiz E421-E422. [DOI] [PubMed] [Google Scholar]
- 9.Kron RE, Litt M, Finnegan LP. Effect of maternal narcotic addiction on sucking behavior of neonates. Pediatr Res. 1974;8(4):364. [Google Scholar]
- 10.Kron RE, Litt M, Eng D, Phoenix MD, Finnegan LP. Neonatal narcotic abstinence: effects of pharmacotherapeutic agents and maternal drug usage on nutritive sucking behavior. J Pediatr. 1976;88(4, pt 1):637–641. [DOI] [PubMed] [Google Scholar]
- 11.LaGasse LL, Messinger D, Lester BM, et al. Prenatal drug exposure and maternal and infant feeding behaviour. Arch Dis Child Fetal Neonatal Ed. 2003;88(5):F391–F399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaker CS. Cue-based co-regulated feeding in the neonatal intensive care unit: supporting parents in learning to feed their preterm infant. Newborn Infant Nurs Rev. 2013;13(1):51–55. [Google Scholar]
- 13.Thoyre SM, Shaker CS, Pridham KF. The early feeding skills assessment for preterm infants. Neonatal Netw. 2005;24(3):7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pados BF, Estrem HH, Thoyre SM, Park J, McComish C. The neonatal eating assessment tool: development and content validation. Neonatal Netw. 2017;36(6):359–367. [DOI] [PubMed] [Google Scholar]
- 15.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA. 2000;283(15):2008–2012. [DOI] [PubMed] [Google Scholar]
- 16.Andreae MH, Rhodes E, Bourgoise T, et al. An ethical exploration of barriers to research on controlled drugs. Am J Bioeth. 2016;16(4):36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allocco E, Melker M, Rojas-Miguez F, Bradley C, Hahn K, Wachman E. Comparison of neonatal abstinence syndrome manifestations in preterm versus term opioid-exposed infants. Adv Neonatal Care. 2016;16(5):329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gewolb IH, Fishman D, Qureshi MA, Vice FL. Coordination of suck-swallow-respiration in infants born to mothers with drug-abuse problems. Dev Med Child Neurol. 2004;46(10):700–705. [PubMed] [Google Scholar]
- 19.Maguire DJ, Taylor S, Armstrong K, et al. Characteristics of maternal-infant interaction during treatment for opioid withdrawal. Neonatal Netw. 2016;35(5):297–304. [DOI] [PubMed] [Google Scholar]
- 20.Cleveland LM, Gill SL. “Try not to judge”: mothers of substance exposed infants. MCN Am J Matern Child Nurs. 2013;38(4):200–205. [DOI] [PubMed] [Google Scholar]
- 21.Cleveland LM, Bonugli R, McGlothen K. The mothering experiences of women with substance use disorders. Adv Neonatal Care. 2016;39(2):119–129. [DOI] [PubMed] [Google Scholar]