Abstract
Today, health is a human right in India, and the government is working hard for universalization of health services provision till the grassroots. Health without accountability is a challenging task in hand, and recently, state governments drafted a bill toward public health system to move in the strengthened direction of accountability mechanism. Accountability is the quality or state of being accountable, and it is an important component of the health-care reforms in India. This article provides more nuanced understanding of accountability which includes the specification of accountability, conceptual framework of accountability, and its potential approaches for how accountability is viewed today in India with reference to the Central, State, District, and other stakeholders. It examines the role of accountability in making accountable health plans, and its relationship governance/ownership structures as a key component of health-care reforms as improved accountability is a major element in improving the health system performance. The article elaborates on the definition of accountability in terms of answerability and sanctions and distinguishes the three types of accountability, namely financial, performance, and political/democratic. The article describes three accountability-enhancing strategies, namely reducing the pilferage, assuring acquiescence with procedures and standards, and improved learning from the past experience. The recent events in Indian health care put forward a serious issue on how accountability can be fixed if health mishaps happened and how we can make our health plans accountable to the needs and aspiration for the people of India. Overall, the accountability is discouraging and more needs to be done to enhance the accountability compliance in India.
Keywords: Accountability, health care, health plan, health policymakers, health system performance
INTRODUCTION
Today, the major debate in the Indian health sector lies in accessibility, availability, affordability, and accountability of the health and health-care services. The major concerns of all are to improve the quality and safety of care, the control of costs of the health care, and the optimum health care to the population. To attain the highest optimal utilization of health care, the researchers rely on correctness, effectiveness, and efficacy of care[1] to quantification of accountability. The perspective of accountability is one in which a governing body (e.g., Union Government, State Government, District Health Administration, Professional Association, and Private Entities) are mandated providers or organizations to meet certain goals or objectives of the programs (e.g., National Health Mission [NHM] and Revised National Tuberculosis Control Program). The Implementing agency or the governing body who owns the authority or legitimacy of program planning, implementation, monitoring and evaluation and accountability must account for the final output of the programs in terms of achievements or goals of the plan. Need for accountability to the health sector is even more relevant in the view of the launch of highly ambitious schemes such as Ayushman Bharat (Pradhan Mantri Jan Arogya Yojana [PMJAY]) and Health and Wellness Centre 2017.
State versus center
The association among these two sides of the accountability equation (provider and client) in India is not necessarily hierarchical at least in the principle.[2] An accountability relationship can be based on a dialogue where providers and organizations argue with governing bodies or beneficiaries about their relative achievement of predefined goals. In the Indian context, we can say that the accountability is only reduced to the application of formal controls of activities only, but in true sense, the accountability will result from the public reporting for better future of multiple indicators in practice.
Current system of accountability
The recent health tragedies in Gorakhpur Hospital, Chhattisgarh Sterilization camps, Bhubaneswar hospital fire, Kolkata hospital tragedy, Erwadi mental asylum tragedy, and many others put the serious question of accountability, if any mishap occurs. In all the cases, the medical doctors are either suspended or terminated without going into the root cause of problems. The present article looks deeper into the current system of accountability in health care in India.
DEFINING ACCOUNTABILITY
Accountability entails the procedures and progressions by which one stakeholder justifies and takes responsibility for its action. The concept of accountability contains three critical components as follows: (1) the loci of accountability, (2) the domains of accountability, and (3) the procedures of accountability.[3]
Overall, an attitude of accountability lies at the core of any effort to improve quality, build team, and get results.[4] An accountable stakeholder acknowledges the reality of a situation (perceives it, sees it, and relate to it) and accepts responsibility for the situation (owns it), finds and implements creative solutions to problems (solves it), and exhibits the commitment and courage needed to follow through (does it). Make sense, doesn't it? Common sense?[5] Human factors, lapses, and errors by individuals in a system, including communication failures, had been at the core of errors in health care.
ACCOUNTABILITY IN HEALTH CARE
Equitable health care is an integral part of the health system, and the accountability in health care is directly related to the level of safety and quality of care a patient receives and that same quality of care is directly related to the success of a health-care.[6] In health care, improving the quality of life for a patient is the ultimate goal: no patients to treat means, no health business to run. Knowing the delicately balanced relationship between the patient and the health-care organization is vital to recognizing the needs of the patient versus the wants of the organization.[7] An accountable health-care programme and policy will constantly investigate and restructure the processes to meet the needs of the patient to improve on the quality of care.
In National Health Policy 2017, “accountability” is a keyword, and all the programs and policy must have the accountability aspect, so that the equitable and just programs are created. Grievance redressal and feedback in India started the “Mera Aspatal” initiative in ten central and later expanded to other hospitals and health facilities. In the United States also, few instances were accountability that was the central theme of the project. The projects are as follows: (1) in President Clinton Health Security Act, accountability was made a critical part of the Programme;[8] (2) the advocates of the health maintenance organizations renamed health management organizations as “Accountable health plans”;[9] and (3) the notion about accountability are normative guides to determine the institutional structures for health-care organizations and type of health-care delivery system we should have.[10]
ACCOUNTABILITY IN HEALTH IN INDIA
The National Rural Health Mission document recognized the lack of community ownership of public health programs and impacts the levels of efficiency, accountability, and effectiveness. It also calls for the strengthening of the rural hospital for effective curative care measurable and accountable to the community through the Indian Public Health Standards and the establishment of Public Accountability Systems. Making public health a shared value across the various sectors is a politically challenging but such collective action is crucial.[11] In order to ensure that the benefits of social security measures reach the intended sections of the society, enumeration of below poverty line families and other eligible sections is vital.[12]
POLICY AND GOVERNANCE ISSUES AMONG DIFFERENT STAKEHOLDERS
Ministry of Health and Family Welfare – Government of India
The ministry is charged with health policy and it's implementation. The government programs relating to health and family planning in India. Apart from planning for health care, the ministries also prepare and disseminate guidelines, financial allocation, social deliverables, private regulation, and prevention of disease outbreak like Zika/Ebola. In this direction, the mission of the ministry encompasses establishing the comprehensive primary health-care delivery system and well-functioning linkages with the secondary and tertiary care health delivery system and regulating health service delivery through the Clinical Establishments (Registration and Regulation) Act 2010 and promoting rational use of pharmaceuticals in the country.[13]
The key features to achieve the goals of the mission include making the public health delivery system fully functional and accountable to all stakeholders for improving the health indicators. With the recent replacement of India's Planning Commission with NITI Aayog, the new government has sought to involve state leaders in policymaking as well as financial planning but decentralization needs to extend beyond financial devolution and be accompanied by a clear chain of accountability for policy implementation. The main problem with centrally-sponsored schemes in general (NHM or otherwise) is that federal (center-to-state) transfers have done little to respond to state need.
State health ministry (Chief Minister/Health Minister)
At the state level, the mission would function under the overall guidance of the State Health Mission headed by the Health Minister of the State. The functions under the mission would be carried out through the State Health and Family Welfare Society. Health being a state subject, the overall coordination and implementation of the program are totally based on state government interventions. While individual responsibility is important in appropriate cases, accountability also includes the assessment at the performance of district-level planning and decision-making and identifying systemic flaws that need to be set right. The State Government always looks for constructive changes that should be made to break the cycle of health system shortcomings by monitoring implementation, replicating successful health interventions, and identifying and rectifying those interventions that do not work.[14]
Another thread of accountability at the state level is grievance redressal but how it is done in the program planning and implementation is not clearly defined. The grievance mechanisms should be capable of identifying through a fair and transparent process whether there is culpable behavior on the part of particular individuals, but the mechanisms should also contribute to identifying the full extent of the state's liability for any harm sustained by anyone when they seek to access health care.
District health department
In India, instrument to guarantee external accountability of policymakers are exceptionally inadequate. It emanated as the part or consequence of colonial legacy, which by design imposed a need for an opaque administration that was detached people from any administrative or civil service accountability in India, and majorly, the accountability is only limited to auditing and has always been internal. Moreover, there are no methods to determine the outcomes of policy decisions, as there is no information on principles and purpose that policies seek to achieve. As a result, accountability breaks down at all levels.
At the district level, on the lines of the State Health Mission, every district will have a District Health Society (DHS) chaired by the Chairperson, Zila Parishad. The DHS will be responsible for planning and managing all health and family welfare programs in the district, and there are two important implications of this requirement. First, DHSs planning will have to take note of both treasury and nontreasury sources of funds, even though it may not be handling all sources directly. Second, its geographical jurisdiction will be greater than those of the Zila Parishad and/or Urban Local Bodies in the district.[15]
Health workers and specialists
The health situation in India is under great stress, and accidents happen in health care are due to the repositioning of health stress. The central feature of the existing public health-care system is a system of primary health-care centers (PHCs) and subcenters where salaried, government-appointed doctors and nurses are expected to treat patients, but at the PHCs estimated average vacancies to be 18% among doctors, 15% among nurses and 30% among paramedics stated in a recent countrywide study. The hiring of the Human resource for health is very skewed and eventually it leads to the poor quality and substandard performance of the health services, Moreover, the salaries and the incentives of the Healthcare professionals and Medical doctors are not linked to performance; a PHC doctor performance has no linkages to remuneration he receives. If Public doctor miss the Healthcare centres opening hours or do not provide standard quality of care, the medical doctors still gets the salary so what's the incentive to perform?
Politicians/bureaucrats
Accountability of politicians and bureaucrats is extremely essential for the projects and program implementation. Politicians make the plans and bureaucrats implement them at the field level. The creation and implementation of the programs follow the set protocols and procedures, but the problems lie at the outcome indicators. Moreover, there are no mechanisms for measuring outcomes of policy decisions as there is no information on standards and goals that policies seek to achieve. As a result, accountability breaks down and for that, no one from the policy side or implementation sides takes the blame.
Beneficiary and consumers
Consumers of health care are the common citizens of India. For them, all the policies and programs are made, but his participation in conceptualization and monitoring of the programs involvement is zero so what is the role of consumers and beneficiaries in accountability mapping is still not defined. To make the programs and policies, the government came with the idea of social audit, the idea of social audits – cross-verification of government account and information with information on the ground and the sharing of audit findings with government through public hearings – has gained much ground in recent years as an important tool through which accountability can be comprehended.
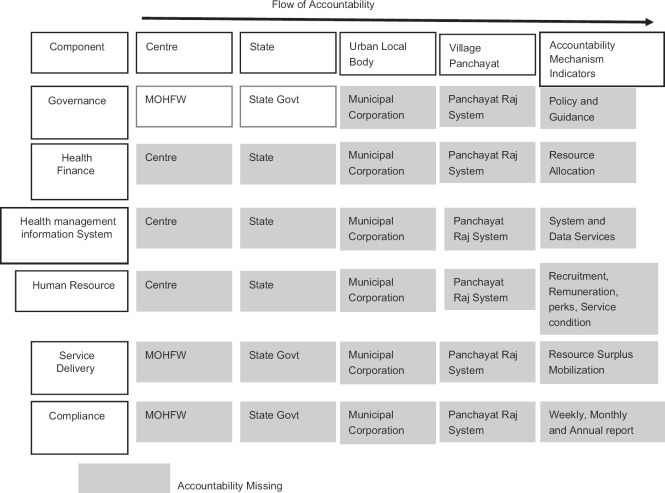
A similar accountability framework needs to be prepared for service delivery of every health program and clinical services provided by the public health system [Figure 1].
Figure 1.
Schematic analysis plan of accountability for indian immunization programme accountability framework in immunization programme. Ref: Conceived and Designed by Dr Manish Priyadarshi and Dr Sanjiv Kumar (IIHMR, Delhi)
Accountability under Pradhan Mantri Jan Arogya Yojana
At present, accessibility of the health services contrasts considerably across the Indian states. At the national average for India is only 0.62 doctors for 1000 populations, which lags significantly from the World Health Organization standard of 1 doctor per 1000 populations. In terms of accountability of Pradhan Mantri Jan Arogya Yojana is concerned, limited accountability is prescribed under it, although Ayushman Bharat-PMJAY offers India a chance to tackle long-term and embedded shortcomings in governance, quality control, and stewardship with active promotion of promotive and preventive care by the Swachh Bharat Abhiyan.
Evaluation of accountability in different health systems
Members of Parliament play a pivotal role in apportioning resources, enacting regulations, supervising the implementation, and reflecting the opinions of citizens about their health services, outline policies, appropriate budgets, and hold the decision-making division of government to interpretation – all dynamic mechanisms of the intensive desired to improve ex RMNCH.
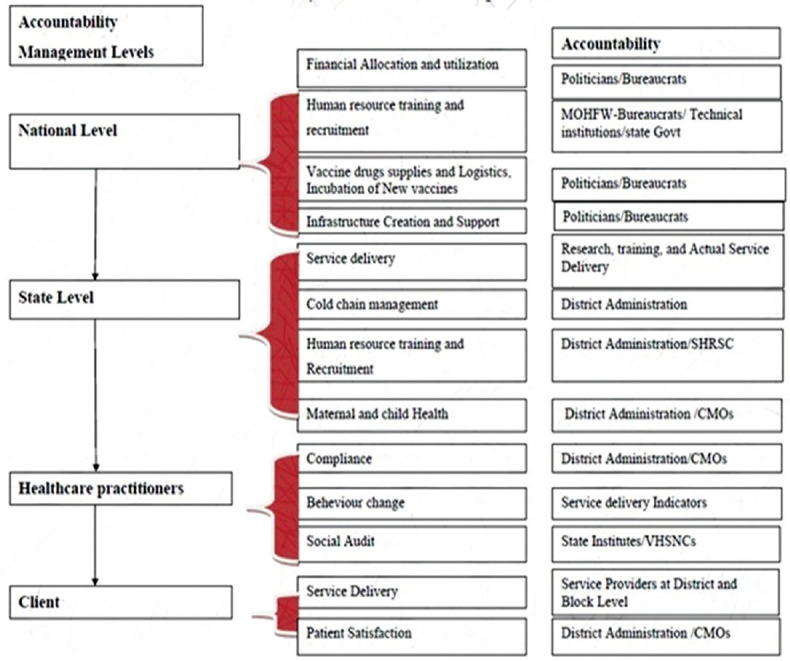
Figure 2 shows the accountability and evaluation of the accountability mechanism among different indicators adapted from the Monitoring and Accountability Platform for national governments and global partners (Global health workforce Alliance), Oct 2013. In developing, implementing, and managing community-based health worker programs, the analysis found out that accountability mechanism is missing from health finance, health management information system, human resource, service delivery, and compliance part, only place where limited accountability mechanism is working are the areas governance at center and state level. At the Municipal and Panchayat level, the accountability mechanism is totally missing.
Figure 2.
Health system and accountability analysis. Ref: Conceived and Designed by Dr Manish Priyadarshi and Dr Sanjiv Kumar (IIHMR, Delhi)
Engendering accountability
Global health vision reports talk about the additional accountability is the need of the hour to make maternal and other allied services equitable and accessible to the government and civil society for planning review and implementation of the health services. Today, due to the global attention, the international donors are looking for accountability from all the stakeholders, so that holistic development of maternal and child health services is delivered to the beneficiaries belonging to the last bench.
CONCLUSION
Accountability for the project and to the people is both desirable and essential. Ensuring this accountability is arguably one of the greatest challenges that face up to the Indian health-care sector. To reach every nook and corner of the system, the accountability needs to take root and procedures need to be built into the system. However, the question arises that how accountability can be achieved in the days to come and who would be held responsible if desired and essential results are not achieved. To achieve the results, we need greater transparency and resultant public scrutiny in every aspect of the project and its management. Still, we are not being in the position to achieve then what we should think of achieve accountability, and then we have the last recourse of putting accountability for informal appraisal system for promotion of health-care professionals and health policy-makers.
Overall, we can say that India follows the model of accountability in a very limited sense and more innovations and socioeconomic experimentations of the accountability needs to be imparted in future policies and programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Maynard A. Health care rationing: Doing it better in public and private health care systems. J Health Polit Policy Law. 2013;38:1103–27. doi: 10.1215/03616878-2373157. [DOI] [PubMed] [Google Scholar]
- 2.Saltman RB, Ferroussier-Davis O. The concept of stewardship in health policy. Bull World Health Organ. 2000;78:732–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Emanuel EJ, Emanuel LL. What is accountability in health care? Ann Intern Med. 1996;124:229–39. doi: 10.7326/0003-4819-124-2-199601150-00007. [DOI] [PubMed] [Google Scholar]
- 4.Conners R, Smith T, Hickmen C. The Oz Principle: Getting Results through Individual and Organizational Accountability. London, UK: Penguin; 2004. p. 16. [Google Scholar]
- 5.Conners R, Smith T, Hickmen C. The Oz Principle: Getting Results through Individual and Organizational Accountability. London, UK: Penguin; 2004. p. 11. [Google Scholar]
- 6.O'Hagan J, Persaud D. Creating a culture of accountability in health care. Health Care Manag (Frederick) 2009;28:124–33. doi: 10.1097/HCM.0b013e3181a2eb2b. [DOI] [PubMed] [Google Scholar]
- 7.Porter-O'Grady T, Malloch K. Managing for Success in Health Care. St. Louis, MO: Mosby; 2007. [Google Scholar]
- 8.Clinton B. The President's Health Security Plan; the Complete Draft and Final Reports of the White House Domestic Policy Council. New York: Times Books; 1993. [Google Scholar]
- 9.Iglehart JK. Managed competition. N Engl J Med. 1993;328:1208–12. doi: 10.1056/nejm199304223281627. [DOI] [PubMed] [Google Scholar]
- 10.Day P, Klein R. Accountabilities. London: Tavistock; 1987. pp. 4–104. [Google Scholar]
- 11.Lakshminarayanan S. Role of government in public health: Current scenario in India and future scope. J Family Community Med. 2011;18:26–30. doi: 10.4103/1319-1683.78635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Planning Commission. Eleventh Five-year plan (2007-2012) Planning Commission: GOI New Delhi. 2007 [Google Scholar]
- 13. [Last accessed on 2019 Jun 11]. Available from: http://mohfw.nic.in/sites/default/files/5_CH_I_Introduction.pdf .
- 14.Freedman LP. Human rights, constructive accountability and maternal mortality in the Dominican Republic: A commentary. Int J Gynaecol Obstet. 2003;82:111–4. doi: 10.1016/s0020-7292(03)00147-4. [DOI] [PubMed] [Google Scholar]
- 15. [Last accessed on 2019 May 27]. Available from: http://mohua.gov.in/uploadfiles/files/74th CAA13.pdf/the 74th amendment .