Abstract
Background:
The organizational environment can foster or impede full deployment of advance practice registered nurses (APRNs), affecting the quality of care and patient outcomes. Given the critical role APRNs play in healthcare, it is important to understand organizational factors that promote or hinder APRN practice to maximize the potential of this workforce in healthcare systems.
Purpose:
Synthesize evidence about APRN practice environments, identify organizational facilitators and barriers, and make recommendations for better APRN utilization.
Methods:
A literature search was conducted in CINAHL, PubMed, and PsychInfo, yielding 366 studies. No time or geographic limitations were applied. Study quality was appraised using the National Institutes of Health National Heart, Lung and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies and The Joanna Briggs Institute Critical Appraisal Checklist for Qualitative Studies.
Results:
Thirty studies, conducted in the United States, Canada, and the Netherlands met inclusion criteria. The majority of the studies involved nurse practitioners. Facilitators to optimal practice environment were autonomy/independent practice and positive physician/APRN relations. Barriers included policy restrictions on practice, poor physician relations, poor administrator relations, and others’ lack of understanding of APRN role. Barriers correlate with job dissatisfaction and increased intent to leave job.
Practice Implications:
The review highlights the importance of physician and administration relations, organizational-level policies, and colleagues’ understanding of APRN role in promoting effective practice environments. Organizations should align policy reform efforts with factors that foster positive APRN practice environments to efficiently and effectively utilize this increasingly vital workforce. Future research is warranted.
Keywords: advanced practice registered nurse, practice environment, integrative review, organizational culture, organizational climate, nurse practitioner, nurse midwife, nurse anesthetist, clinical nurse specialist
Introduction
The United States (U.S.) healthcare system currently faces an economic and quality crisis due to an aging population and more patients living with chronic diseases needing timely access to high quality care (Association of American Medical Colleges [AAMC], 2017; Institute of Medicine [IOM], 2011). Further, provider shortages threaten the ability of the system to meet care demands. The use of Advance Practice Registered Nurses (APRN) has been singled out by policy makers and organizations as critical to meeting these increasing demands (IOM, 2011; National Council of State Boards of Nursing [NCSBN], 2015). However, state-based regulations and inhibitive practice environments within APRN employment settings often impede the effective utilization of APRNs to the full extent of their education and training (IOM, 2011).
APRNs are registered nurses (RNs) with advanced education and training, typically a master’s or doctoral degree, who can assess, diagnose, and treat patients, and whose scope of practice is defined by variable state-based practice regulations (NCSBN, 2015). In the U.S., recognized APRN roles include certified registered nurse anesthetists (CRNA), nurse practitioners (NP), certified nurse midwives (CNM), and clinical nurse specialists (CNS).
Many overlapping terms exist in the literature to discuss the environment nurses work in, including organizational climate, organizational culture, work environment, and work context. One of the more common nursing research terms used is practice environment (Sleutal, 2000). There is evidence that positive nurse practice environments correlate to improved outcomes, including increased job satisfaction, lower burnout, and reduced patient mortality (Kutney-Lee, et al., 2015; Laschinger & Leiter, 2006). While over forty years of research reinforces the importance of RN practice environments for patients, nurses, and health care organizations (IOM, 2011; Lake, 2002; Lake, 2007; Laschinger, Almost, & Tuer-Hodes, 2003; Laschinger & Leiter, 2006; McGibbon, Peter, & Gallop, 2010; Sleutel, 2000), research surrounding APRN practice environments remains less mature. Although the foundation of APRN practice is nursing, the APRN role is different from those of RNs and includes other responsibilities such as diagnosing and prescribing treatments. Thus, RN practice environment research may not directly translate to APRN practice. The identification of organizational attributes important to APRN practice environment may lead to improvements in patient and APRN outcomes, and help reach the overall goal of healthcare system fiscal and quality progression. The purpose of this review is to synthesize existing evidence on organizational factors that act as facilitators or barriers to optimal APRN practice environment. Understanding the current state of APRN practice environments and identifying relevant gaps in the literature can promote the full deployment of APRNs and inform policy, practice, and future research.
Theory
Institutional Theory guided this review (Scott, 2014). An institution is a social construct in which practices universally accepted by employees become part of the culture of an organization. Institutions form when structures and processes become embedded in organizations and acquire legitimacy in their own right, rather than through demonstrated benefit to the organization (Scott, 2014). Once these established practices develop into institution form, they are very resistant to change. Institutions form through several methods, including coercive forces, which exert pressure through manipulation of resources on which the organization depends (Scott, Ruef, Mendel, & Caronna, 2000). Institutions can also form through mimetic forces, where organizations copy successful competitors’ practices. Additionally, institutions can form through normative forces where structures and processes develop by following established professional standards and norms (Scott, 2014). According to Institutional Theory, three systems maintain institutions: 1) regulative systems, where behavior is constrained through formal and informal rules, 2) normative systems, where values and norms govern behavior, and 3) cultural-cognitive systems, which govern behavior through shared conceptions of social reality (Scott, 2014). The term institution used in this paper refers to these aforementioned constructs; organizations is used to indicate entities where APRNs work.
Organizational change can occur when outside functional, political, or social forces act to destabilize these systems leading to a breakdown of established institutions in a process called deinstitutionalization. As established institutions are challenged, new practices emerge and gain more widespread acceptance (legitimization) (Reay, Colden-Biddle, & Germann, 2006). If new practices gain enough traction, they eventually become institutionalized in their own right. Many institutions exist that impede the APRN role in healthcare delivery, including licensing laws, hospital privileging, insurance reimbursement, and medications prescribing (Starr, 1982). In addition, gender and power dynamics may play a role in maintaining institutions that impede APRN practice (Rudner, 2016). This review analyzes APRN practice environment literature through the lens of Institution Theory to guide understanding of how organizational attributes that affect APRN practice may be the result of such previously established institutions.
Methods
Literature search
The Whittemore and Knafl (2005) integrative review approach guided the literature search. An electronic search was conducted across three databases (Cumulative Index to Nursing and Allied Health [CINAHL], PubMed, and PsychInfo) in November, 2017. The following key words were searched: “advanced practice nurs*, nurse practitioner, nurse anesthetist, nurse midwi*, clinical nurse specialist AND practice environment, work environment, organizational climate, and organizational culture.” Studies were eligible if they met each of the following inclusion criteria: 1) peer reviewed research; 2) available in English; and 3) investigated the practice environment of APRNs. All publication years were considered. Further, although APRN practice environments and regulations may differ in countries outside the U.S., studies conducted in all countries were eligible for inclusion because they may provide insights into common workplace factors influencing APRN practice. Exclusion criteria included: 1) studies not relevant to APRNs (e.g., RNs only); and 2) studies that did not investigate organizational factors affecting APRN practice environment.
Quality appraisal
Quality appraisals of quantitative studies were conducted using the National Institutes of Health [NIH] National Heart, Lung and Blood Institute, Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (US Department of Health and Human Services [HHS], 2017). Qualitative studies were appraised using the Johanna Briggs Institute Critical Appraisal Checklist for Qualitative Research (Johanna Briggs Institute [JBI], 2016). Three researchers independently appraised the included studies, and consensus was reached for all quality appraisals. Study quality was scored good, fair, or poor based upon criteria identified in quality assessment tools (HHS, 2017; JBI, 2016).
Synthesis
From each study, we extracted data about study characteristics, facilitators, and barriers to optimal APRN practice environments. Next, using Eileen Lake’s (2002) “practice environment” definition, — “… the organizational characteristics of a work setting that facilitate or constrain professional nurse practice”— as a guide, we assessed for the presence of critical domains for a practice environment in each study. Critical domains of a nurse practice environment include autonomy, a quality-based philosophy of care, status of nursing (including organizational participation), recognition of expertise, professional development, and supportive/collaborative relationships with managers, physicians, and peers (Lake, 2007).
Results
The initial literature search yielded 366 studies. A search of study reference lists identified twenty additional studies. After removing 42 duplicates, two researchers screened the titles and abstracts of each study, applying the inclusion/exclusion criteria. A total of 313 records were removed for the following reasons: 1) the study did not focus on organizational factors that impact APRN practice environment (n=129); 2) the study focused on practice environment of RNs, and not APRNs (n=45); and 3) the article did not describe a research study (n=129). Forty-one articles remained for full text review. Next, ten articles were excluded as they did not investigate APRN practice environment (e.g., focused on RN practice environment only), leaving thirty-one articles eligible for inclusion.
Study characteristics
Studies were conducted in the U.S. (n=25), Canada (n=3), and the Netherlands (n=2). (Table 1). The majority of studies focused on the practice environment of NPs (n=14) or NPs in combination with other clinicians (n=5). Two studies identified its population generally as APRNs; one focused on family planning clinics (typically staffed by NPs and CNMs but the study did not specify provider type), and another included all APRN types as well as physician assistants (PA). Two studies focused on CRNA population, and five examined practice environments of CNS and NPs.
Table 1.
Study Characteristics
| Study | n | Study Focus | Quality |
|---|---|---|---|
| Poghosyan et al. (2017) | 314 | PCNP work environments effect on role | Good |
| Athey, et al. (2016) | 8311 | NP work setting, autonomy, job satisfaction | Good |
| Bae (2016) | 9010 | NP satisfaction, work conditions | Good |
| Brom, et al. (2016) | 181 | NP role perception, stress, satisfaction and intent to stay | Fair |
| Motley, et al. (2016) | 39 | APCs’ perceptions of an ideal work environment | Fair |
| Poghosyan et al. (2016a) | 314 | PCNP autonomy, leadership and NP-physician teamwork | Fair |
| Poghosyan et al. (2016b) | 314 | PCNP practice environments, NP retention | Fair |
| Lelli, et al. (2015) | 310 | PCNP autonomy, satisfaction in retail clinics and primary care | Good |
| Poghosyan, et al. (2015b) | 569 | PCNP organization, regulatory, and practice environments | Fair |
| Poghosyan et al. (2015a) | 592 | PCNP roles and organizational characteristics in 2 states | Fair |
| Cheng, et al. (2014) | 406 | Factors affecting APRNs intention to stay | Fair |
| Doran, et al. (2014)* | 359 | RN, CNS, APRN demographics, work patterns, exit rates | Fair |
| Pasaron (2013) | 39 | NP, physician satisfaction, retention, recruitment | Fair |
| Poghosyan, et al. (2013b) | 23 | PCNP roles, responsibilities, barriers and facilitators | Good |
| Poghosyan, et al. (2013a) | 16 | Organizational climate, PCNP professional practice | Good |
| Pron (2013) | 99 | NMHC characteristics, PCNP job satisfaction, autonomy | Fair |
| Meeusen,et al. (2011a)** | 923 | CRNA work environment, satisfaction and intent to stay | Fair |
| Meeusen,et al. (2011b)** | 923 | CRNA work climate, work characteristics, job satisfaction | Fair |
| Faris et al. (2010) | 1983 | NP, CNS job satisfaction and practice barriers in the VA | Good |
| Chevalier et al. (2006) | 834 | Practice barriers for mental health CNSs and NPs | Fair |
| Plager & Conger (2006) | 30 | Role differentiation among graduate CNS, NPs | Fair |
| Lindeke, et al. (2005) | 191 | NP perceptions of barriers to rural practice | Fair |
| Laschinger et al. (2003)* | 55 | RN, ACNP autonomy, magnet status, and satisfaction | Good |
| Almost et al. (2002)* | 117 | PCNP workplace empowerment, collaboration with physicians and managers, job strain | Good |
| Freeborn et al. (2002) | 747 | PCNP, PA, physician practice environment, job satisfaction in a large HMO | Fair |
| Chumbler et al. (2000) | 373 | PCNP demographics, practice attributes, clinical decision making, productivity | Good |
| Byers, et al. (1999) | 58 | PCNP, PA, physician job satisfaction in Army clinics | Good |
| Domine, et al. (1998) | 1816 | A profile of NPs and CNSs and their practices in the VA | Fair |
| Howard et al. (1997) | 341 | Constraints, barriers to CNS and NP psychiatric practice | Fair |
| Hupcey (1993) | 91 | NP work settings in one state | Fair |
Note: APC-advanced practice clinician not specified. ACNP-acute care nurse practitioner. APRN-advanced practice registered nurse. CNS-clinical nurse specialist. CRNA-Certified Registered Nurse Anesthetist. HMO-health maintenance organization. NMHC- nurse managed health center. NP-nurse practitioner. PA- physician assistant. PCNP- primary care nurse practitioner. RN- registered nurse. VA-Veteran’s Administration. Studies are U.S.-based except those marked
Canada
Netherlands
Twenty-six studies were quantitative, with 25 cross-sectional descriptive studies and one trend-study design. Of the 26 quantitative studies, nine studies were appraised as good quality (Almost & Laschinger, 2002; Athey et al., 2016; Bae, 2016; Byers, Mays, & Mark, 1999; Chumbler, Geller & Weier, 2000; Faris, Douglas, Maples, Berg, & Thrailkill, 2010; Laschinger, Almost &Tuer-Hodes, 2003; Lelli, Hickman, Savrin & Peterson, 2015; Poghosyan, Liu, & Norful, 2017). Sixteen studies received a fair quality rating due to low or undetermined response rates, use of a non-validated measure, and/or decreased generalizability (Brom, Melnyk, Szalacha, & Graham, 2016; Cheng, Kelly, Carlson, & Witt, 2014; Chevalier, Steinberg, & Lindeke, 2006; Domine, Siegal, Zicafoose, Antai-Otong, & Stone, 1998; Doran, Duffield, Rizk, Nahm, & Chu, 2014; Freeborn, Hooker, & Pope, 2002; Hupcey, 1993; Lindeke, Jukkala, & Tanner, 2005; Meeusen, Van Dam, Brown-Mahoney, Van Zundert, & Knape, 2011a; Meeusen, Van Dam, Brown-Mahoney, Van Zundert, & Knape, 2011b; Pasaron, 2013; Poghosyan, Shang, Liu, Poghosyan, Liu, & Berkowitz, 2015; Poghosyan & Aiken, 2015; Poghosyan & Liu, 2016; Poghosyan, Liu, Shang, & D’Aunno, 2016; Pron, 2013). One study received a poor rating for high risk of bias in the methodology and was subsequently removed from the synthesis (Hayden, Davies, & Clore, 1982). Of the five qualitative studies, two were rated as good quality (Poghosyan et al., 2013a; Poghosyan, Nannini, Stone, & Smaldone, 2013b), and three were rated as fair due to methodologic issues including the research question not matching the research method, lack of disclosure of researcher influence, or no documentation of IRB approval or informed consent (Howard & Grenier, 1997; Motley, et al., 2016; Plager & Conger, 2006).
Major findings
Organizational factors that affect APRN practice environment were categorized as facilitators of, or barriers to APRN practice. Major organizational characteristics found to facilitate APRN practice environment were high levels of autonomy/independent practice, and positive APRN-physician relations. Barriers to APRN practice environment reported in the literature were policy restrictions on APRN practice, poor APRN-administration relations, physician opposition to independent APRN practice free from physician oversight or supervision, lack of understanding of the APRN role, and lack of professional recognition. One study investigated practice environment through the lens of job design, and the findings could not be categorized into a facilitator/barrier schema (Cheng, et al., 2014).
Facilitators to APRN practice
Autonomy/Independent Practice
Across studies, APRNs reported moderately high (Lelli, et al., 2015) to high levels of autonomy (Hupcey, 1993; Pron, 2013; Poghosyan & Liu, 2016; Poghosyan, et a., 2017; Poghosyan, Liu, Shang, …et al., 2016) in their current positions. These studies were predominantly conducted in primary care ambulatory settings (Lelli, et al., 2015; Pron, 2012; Poghosyan & Liu, 2016; Poghosyan, et al., 2017; Poghosyan, Liu, Shang, … et al., 2016). Two studies found autonomy higher in primary care settings than in hospital-based surgical or acute care settings, and lowest in hospital-based surgical specialty settings (Almost & Laschinger, 2002; Athey, …et al., 2016). APRNs reported being satisfied with the level of autonomy in their settings in six studies (Brom, et al., 2016; Faris, et al., 2010; Freeborn et al., 2002; Motley, et al., 2016; Poghosyan et al., 2017; Pron, 2013). Factors that increased autonomy included rural settings (Bae, 2016), increased tenure as an APRN (Chumbler, et al., 2000; Faris, et al., 2010), age (Faris, et al., 2010), fewer on-site physicians, and family- or multi-specialty setting (Chumbler et al., 2000). Use of clinical guidelines increased APRN autonomy in an ambulatory study (Chumbler et al., 2000). One NP study reported a significantly higher level of autonomy/independent practice if participants had their own designated panel of patients (Poghosyan et al., 2017).
Increased autonomy/independent practice was associated with lower job strain (Almost & Laschinger, 2002), increased job satisfaction (Athey, et al., 2016; Bae, 2016; Byers, et al., 1999; Laschinger, Almost, …et a., 2003; Meeusen, et al., 2011a; Pasaron, 2013), increased clinical productivity (Chumbler et al., 2000), decreased intent to leave current position (Poghosyan, Liu, & Shang, …et al., 2016), and increased teamwork (Poghosyan & Liu, 2016). However, one study found freedom to make decisions about work, a form of autonomy, was not a significant factor in satisfaction (Cheng, et al., 2014). In one study, APRNs in a state with less restrictive APRN practice laws reported improved workplace autonomy over those in a state with more restrictive laws (Poghosyan, et al., 2015). APRNs in another study reported high workplace autonomy despite state practice regulations (Poghosyan et al., 2013).
Positive APRN-Physician Relations
Several studies reported positive relations with physician colleagues (Doran, et al., 2014; Freeborn, et al., 2002; Motley, et al., 2016; Pasaron, 2013; Poghosyan et al., 2013a; Poghosyan, et al., 2015; Poghosyan et al., 2017; Poghosyan, Liu, Shang, … et al., 2016; Poghosyan & Liu, 2016). Positive physician relations were linked to improved job satisfaction (Almost & Laschinger, 2002; Athey, et al., 2016; Poghosyan et al., 2016) and lower intent to leave (Poghosyan et al., 2016). Positive physician relationships were more common in a state with less restrictive APRN practice laws (Poghosyan et al., 2015). Studies reporting positive relations with physicians were all published after 2013, involved mostly NP participants, and occurred chiefly in primary care settings (Poghosyan et al., 2013a; Poghosyan, et al., 2015; Poghosyan et al., 2017; Poghosyan et al., 2016; Poghosyan & Liu, 2016). Other settings reporting positive physician relations included a hospital setting (Pasaron, 2013), and a healthcare network (Motley, et al., 2016). APRN and physicians alike reported favorable relationships (Pasaron, 2013; Poghosyan et al., 2013a).
Barriers to APRN Practice
Policy Restrictions on APRN Practice
Whereas high autonomy/independent practice was reported to facilitate APRN practice in some studies, organizational policies than limit autonomy/independent practice have been reported as a barrier in others (Almost & Laschinger, 2002; Athey, et al., 2016; Chevalier et al., 2006; Domine, et al., 1998; Faris et al., 2010; Howard & Grenier, 1997; Hupcey, 1993; Pasaron, 2013; Plager & Conger, 2006; Poghosyan et al., 2013a; Poghosyan, et al., 2015; Poghosyan et al., 2016; Poghosyan & Liu, 2016; Poghosyan et al., 2017). In particular, the inability to prescribe medications (Domine, et al., 1998; Howard & Grenier, 1997; Hupcey, 1993), admit patients to facilities (Domine, et al., 1998; Howard & Grenier, 1997; Plager & Conger, 2006), and the need for physician co-signatures (Domine, et al., 1998; Plager & Conger, 2006; Poghosyan et al., 2013a) constituted barriers to APRN practice. Restrictions on autonomy were reportedly higher in acute care settings (Almost & Laschinger, 2002; Athey, et al., 2016; Chumbler et al., 2000). Third-party reimbursement practices such as reimbursement restrictions on APRN care or reimbursing APRN care at a lower rate than physician colleagues performing similar activities (Howard & Grenier, 1997; Plager & Conger, 2006; Poghosyan et al., 2013a) affected autonomy/independent practice.
Lack of resources or support also restricted APRN practice, (Howard & Greiner, 1997; Motley, et al., 2016; Poghosyan, et al., 2015) including lower funding (Hupcey, 1993), space (Lindeke et al., 2005), or resources preferentially supplied to physician colleagues (Poghosyan et al., 2013b; Poghosyan, et al., 2015). Lack of a voice in governing structures (Athey, et al., 2016; Motley, et al., 2016; Poghosyan et al., 2013a) and insufficient time for patient care were also barriers to APRN practice (Hupcey, 1993; Plager & Conger, 2006; Poghosyan et al., 2013b).
Poor APRN-Administration Relations
Poor APRN-administration relationships were reported as a barrier to practice in several studies (Brom, et al., 2016; Domine, et al., 1998; Faris, et al., 2010; Howard & Greiner, 1997; Hupcey, 1993; Meeusen, et al., 2011a; Meeusen, et al., 2011b; Motley, et al., 2016; Pasaron, 2013; Poghosyan et al., 2013a; Poghosyan & Aiken, 2015; Poghosyan et al., 2016; Poghosyan & Liu, 2016). Lack of support from administration (Chevalier, et al., 2006; Domine, et al., 1998; Faris, et al., 2010; Hupcey, 1993; Pasaron, 2013) and treating APRNs differently than physician colleagues despite similar functions (Poghosyan et al., 2015; Poghosyan et al., 2013b; Poghosyan & Aiken, 2015; Poghosyan & Liu, 2016) were commonly reported. Suboptimal relations with administrators led to decreased job satisfaction (Brom, et al., 2016; Faris, et al., 2010; Poghosyan et al., 2016). In one study, the inability to identify immediate supervisor was found to be disempowering (Motley, et al., 2016).
Poor APRN-physician relations
The relationship with physicians was found to act as both facilitator and barrier to APRN practice (Chevalier, et al., 2006; Hupcey, 1993; Poghosyan, et al., 2013a; Poghosyan, et al., 2013b; Poghosyan, et al., 2015; Poghosyan & Liu, 2016; Poghosyan, et al., 2016). Language such as lack of physician support (Brom, et al., 2016; Faris, et al., 2010; Howard & Greiner, 1997; Poghosyan, et al., 2013b) and physician resistance to APRN role (Chevalier, et al., 2006; Hupcey, 1993) characterized physician relations that constituted a barrier to APRN practice. In addition, a lack of physicians willing to serve as an APRN’s state-mandated collaborator was also identified as a barrier to APRN practice (Howard & Griener, 1997; Hupcey, 1993). Poor physician relations were correlated with diminished scope of practice in one study of primary care NPs (Poghosyan et al., 2013a).
APRN Role Not Well Understood and Lack of Professional Recognition
Lack of understanding of the APRN role was a consistent barrier to APRN practice across studies (Athey, et al., 2016; Brom, et al., 2016; Chevalier, et al., 2006; Domine, et al., 1998; Faris, et al., 2010; Howard & Greiner, 1997; Hupcey, 1993; Lindeke, et al., 2005; Pasaron, 2013; Plager & Conger, 2007; Poghosyan, et al., 2016; Poghosyan, et al., 2013a; Poghosyan et al., 2013b; Poghosyan, et al., 2015; Poghosyan & Aiken, 2015). Coworkers and other healthcare professionals (Chevalier, et al., 2006; Domine, et al., 1998; Lindeke, et al., 2005; Poghosyan et al., 2013a), physicians (Hupcey, 1993; Poghosyan, et al., 2013a; Poghosyan, et al., 2013b), administrators (Hupcey, 1993; Pasaron, 2013; Poghosyan & Aiken, 2015), and patients or the public (Chevalier, et al., 2006; Plager & Conger, 2006; Poghosyan, et al., 2013a; Poghosyan, et al., 2013b) lacked understanding of NP role. Primary care APRNs in a state with restricted SOP regulations were more likely to report lack of understanding of APRN role compared to a state with less restrictive laws (Poghosyan, et al., 2015). APRNs working in organizations with 10 or fewer APRNs reported less understanding of the role than those working in settings with greater than 10 APRNs (Poghosyan & Aiken, 2015).
The absence of professional recognition has been identified as an APRN practice barrier (Domine, et al., 1998; Howard & Grenier, 1997; Motley, et al., 2016; Poghosyan, et al., 2013a; Poghosyan & Liu, 2016; Poghosyan & Aiken, 2015). Notably, the lack of promotion of the APRN role within the organization, and externally (e.g. promoting on website) (Poghosyan, et al., 2013a), the inability of APRNs to be listed as provider of record or carry their own patient panel (Athey, et al., 2016; Poghosyan, et al., 2017; Poghosyan, et al., 2013a; Poghosyan & Liu, 2016), and electronic health records that do not capture APRN care (Motley, et al., 2016; Poghosyan, et al., 2013a). Such practices not only render APRN care invisible (Poghosyan, et al., 2013a; Poghosyan, et al., 2013b) but also interfere with patient communication and ability to provide proper follow up, and also limits patient choice of providers (Poghosyan, et al., 2013a).
Discussion
This review synthesizes available literature about APRN practice environments and examines organizational level facilitators and barriers to APRN practice through the lens of Institutional Theory. Increased APRN education, training, and enhanced professional standards are transforming normative systems and facilitating full deployment of APRNs in previously unrecognized advanced roles in healthcare delivery. The high autonomy/independent practice in ambulatory settings, the improvement of APRN-physician relations, and the movement of APRNs into acute care settings identified in this review are seen as harbingers of an improving APRN practice environment.
Despite advances in APRN roles, it is important to recognize that several organizational barriers, including historical institutions that maintain restrictive policies, still hinder APRN practice. Legislation regarding APRN practice varies from state to state, yet organizations often restrict APRNs beyond what is legally permitted by state law (Anen, & McElroy, 2015). Common restrictions involve the dependence on physicians for prescriptive and hospital admission capabilities, need for physician co-signatures, and inability to care for a panel of patients. These restrictions represent healthcare institutions that have not yielded to functional, political, and societal forces for change. Outside of regulatory institutions such as state laws mandating physician oversight or prohibiting certain APRN activities (Faris, et al., 2010; Howard & Greiner, 1997; Poghosyan, et al., 2014; Poghosyan & Aiken, 2015), third-party payer reluctance to reimburse organizations for APRN services (Howard & Greiner, 1997; Plager & Conger, 2006; Poghosyan, et al., 2013a) continue to exert coercive influence to maintain status quo. As the U.S. moves toward value-based payment, functional, political, and societal forces will continue to exert pressure on these institutions that limit non-physician care.
Per Lake’s domains of professional nursing practice environments, several domains of APRN and RN practice environments overlap, including relationships with administrators, organizational participation, and recognition of expertise. However, there were additional domains of a practice environment found to be unique to APRNs including organizational policies directed by outside forces including state legislation and third party payers, and lack of understanding regarding the APRN role. Considering the projected deficit of healthcare providers, this review raises concerns that organizational factors leading to poor practice environments may yield higher APRN turnover and result in difficulty with recruitment. Barriers to practice identified in this review contributed to lower job satisfaction (Brom, et al., 2016; Meeusen, et al., 2011a; Poghosyan, Liu, Shang, … et al., 2016), and increased intent to leave the current position (Cheng, et al., 2014; Lelli, et al., 2015; Meeusen, et al., 2011a; Poghosyan, Liu, Shang, … et al., 2016), lending support to the concern that barriers to APRN practice environments may negatively impact APRN satisfaction and retention. The National Academy of Medicine identified decreased job satisfaction and turnover in healthcare workers as major concerns for decreased quality of care and increased costs in the future (Dyrbye, Shanafelt, Sinsky, …et al., 2017). Based on these considerations and the findings in our review, administrators should evaluate existing organizational policies that lead to poor APRN practice environments.
This recommendation is aligned with several studies that have encouraged organizations to increase APRN involvement in decision-making as a way to improve these work environments (Almost & Laschinger, 2002; Freeborn, et al., 2002; Laschinger, et al., 2003; Pasaron, 2013; Poghosyan et al., 2013a). Hospitals with bureaucratic, hierarchical power structures are prone to centralized decision-making with diminished nurse participation at executive levels (McGibbon, et al., 2010). Evidence suggests that federal, state, professional, and market forces are exerting coercive pressure on hospitals, in particular, to decrease these outdated institutions (Scott, 2014). However, it is apparent from the findings of this review that institutions restricting APRN practice in healthcare remain. Deinstitutionalization of historical barriers to APRN practice has been linked to improved APRN job satisfaction and retention (Bae, 2016; Byers et al., 1999; Laschinger, et al., 2003; Pasaron, 2013; Poghosyan, et al., 2016), and increased clinical productivity (Chumbler, et al., 2000), that will optimistically exert mimetic pressure across the industry in the future.
Practice Implications
This review can serve as a guide for organizations interested in achieving the maximum benefit of a fully-utilized, stable APRN workforce. The retention of APRNs through supporting positive APRN practice environments will help healthcare administrators effectively use all health care workforce resources to meet the demands of an aging and complex patient population, while managing the shift to value-based reimbursement (NCSBN, 2015). It has been suggested that market pressures are responsible for the shift from historically medical, physician-oriented healthcare institutions to systems that embrace APRN care delivery (Scott, 2014). Optimistically, the steadily increasing volume of APRNs will help meet anticipated increased healthcare demand (AAMC, 2017). However, attention to organizational attributes that promote APRN practice environment is required to adequately support and sustain this vital labor force. Resolving organizational and inter-professional ambivalence and confusion regarding APRNs could contribute to more efficient use of APRNs.
Future studies are recommended to identify supportive internal policies that reduce APRN practice barriers in their organizations, specifically in the areas of prescriptive authority, admitting privileges, requirement for physician co-signature on orders, and policies regarding APRN patient panels. Great variation in APRN policies exist within and between organizations, even within the same state (Anen & McElroy, 2015). These policy variations are often the result of organizational policies (institutions) that inhibit the efficient use of APRNs.
Further, results of this review suggest that APRN-physician and APRN-administration relations can profoundly affect APRN practice environment. Structures and processes that promote positive physician-APRN co-management of patients, including provider communication, mutual respect and trust, and clinical alignment have been encouraged in previous studies (Norful, deJarq, Carlino, & Poghosyan, 2018; Norful, Swords, Marichal, Cho, & Poghosyan, 2017). We recommend administrators make efforts to expand their knowledge of APRN capabilities, improve communication lines between APRNs and physicians, and include APRN participation at decision making levels in the organization. APRNs are increasingly being called upon to improve efficiency and effectiveness of U.S. healthcare (Anen & McElroy, 2015). It is incumbent upon organizational administrators to stay abreast of evolving APRN practice abilities to derive maximal benefits from their use. This review also reveals the underrepresentation of CRNAs, CNSs and CNMs in studies investigating APRN practice environments. Future research should focus on these types of APRNs to understand how to optimize their practice environment and best use them across settings.
Limitations
There are limitations to this review. The sheer number of terms applicable to practice environment makes literature detection difficult. To mitigate this limitation, multiple search terms were employed along with several literature search strategies. A second limitation was the inclusion of only articles published in English. Additionally, the APRN search strategy utilized terminology consistent with NCSBN consensus model language which could bias the review to U.S. studies. An additional limitation concerns the fair data quality of the majority of studies in this review due to descriptive cross-sectional designs. Critics have raised concerns over this problem in nursing practice environment research at large, with calls for more rigorous study designs investigating causal mechanisms (Norman, 2013). Future studies should investigate what relationship APRN practice environment has on patient outcomes, and whether intervening factors play a role in this relationship.
Conclusion
This integrative review revealed several facilitators of, and barriers to positive APRN practice environments. Evidence surrounding APRN practice environments has steadily increased and this review acknowledges the influence of relations with physicians and administration, the importance of knowledge of the APRN role, and organizational level policies that may hinder or restrict APRN practice. Efforts to promote a positive APRN practice environment, especially through organizational policy reform are recommended to efficiently and effectively utilize this increasingly vital workforce.
Figure 1.
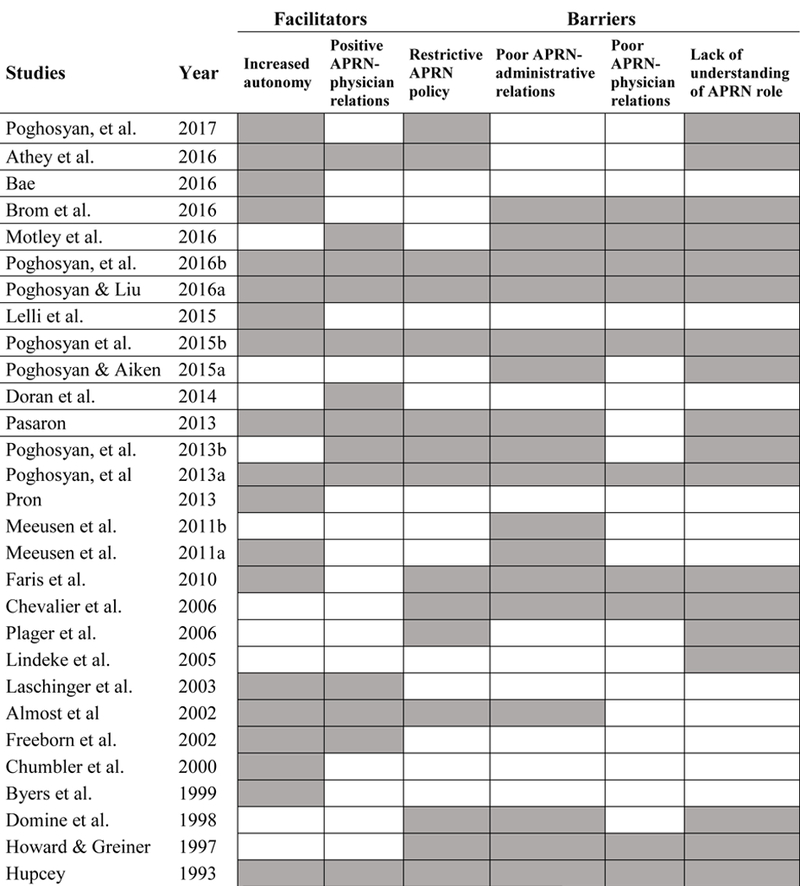
Organizational Facilitators and Barriers to Optimal APRN Practice Environments
Note: CheNote: Cheng et al. not included---study did not identify barriers and facilitators
Acknowledgments
Funding: Dr. Norful was supported by the National Center for Advancing Translational Sciences, National Institutes of Health through Grant Number TL1TR001875. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contributor Information
Lori Schirle, Vanderbilt University School of Nursing, 461 21st Avenue South, 408 Godchaux Hall, Nashville, Tennessee 37240, Tel. (615)343-5992, Fax (615)343-7788, Lori.schirle@vanderbilt.edu.
Allison A. Norful, Columbia University School of Nursing, Columbia University Medical Center Irving Institute for Clinical and Translational Research.
Nancy Rudner, George Washington University.
Lusine Poghosyan, Columbia University School of Nursing.
References
- Almost J, & Laschinger HK (2002). Workplace empowerment, collaborative work relationships, and job strain in nurse practitioners. Journal of the American Academy of Nurse Practitioners, 14(9), 40–420. doi: 10.1111/j.1745-7599.2002.tb00142.x [DOI] [PubMed] [Google Scholar]
- Anen T, & McElroy D (2015). Infrastructure to optimize APRN practice. Nurse Leader, 13(2), 50–56. doi: 10.1016/j.mnl.2015.01.004 [DOI] [Google Scholar]
- Association of American Medical Colleges [AAMC]. (2017). The Complexities of Physician Supply and Demand: Projections from 2015 to 2030. Washington DC: Association of American Medical Colleges; Retrieved from https://aamc-black.global.ssl.fastly.net/production/media/filer_public/c9/db/c9dbe9de-aabf-457f-aee7-1d3d554ff281/aamc_projections_update_2017_final_-_june_12.pdf [Google Scholar]
- Athey EK, Leslie MS, Briggs LA, Park J, Falk NL, Pericak A, El-Banna MM, Greene J (2016). How important are autonomy and work setting to nurse practitioners’ job satisfaction? Journal of the American Association of Nurse Practitioners, 28(6), 320–326. doi: 10.1002/2327-6924.12292 [DOI] [PubMed] [Google Scholar]
- Bae SH (2016). Nurse practitioners’ job satisfaction in rural versus non-rural areas. Journal of the American Association of Nurse Practitioners, 28(9), 471–478. doi: 10.1002/2327-6924.12362 [DOI] [PubMed] [Google Scholar]
- Brom HM, Melnyk BM, Szalacha LA, & Graham M (2015). Nurse practitioners’ role perception, stress, satisfaction, and intent to stay at a Midwestern academic medical center. Journal of the American Association of Nurse Practitioners, 28(5). doi: 10.1002/2327-6924.12278 [DOI] [PubMed] [Google Scholar]
- Byers VL, Mays MZ, & Mark DD (1999). Provider satisfaction in Army primary care clinics. Military Medicine, 164(2), 132–135. [PubMed] [Google Scholar]
- Cheng A, Kelly PJ, Carlson K, & Witt J (2014). The intention of advanced practice registered nurses to remain in positions at family planning clinics serving low-income women. Journal of Professional Nursing, 30(1), 72–79. doi: 10.1016/j.profnurs.2012.12.013 [DOI] [PubMed] [Google Scholar]
- Chevalier C, Steinberg S, & Lindeke L (2006). Perceptions of barriers to psychiatric-mental health CNS practice. Issues in Mental Health Nursing. 27(7), 753–763. doi: 10.1080/01612840600781147 [DOI] [PubMed] [Google Scholar]
- Chumbler NR, Geller JM, & Weier AW (2000). The effects of clinical decision making on nurse practitioners’ clinical productivity. Evaluation & the Health Professions, 23, 285–304. doi: 10.1177/01632780022034615 [DOI] [PubMed] [Google Scholar]
- Domine LM, Siegal M, Zicafoose B, Antal-Otong D, & Stone JT (1998). Survey of APNs employed by the Veterans Health Administration. The Nursing Practitioner, 22(7), 16–23. [PubMed] [Google Scholar]
- Doran D, Duffield C, Rizk, Pl, Nahm, S., & Chu, C.H. (2014). A descriptive study of employment patterns and work environment outcomes of specialist nurses in Canada. Clinical Nurse Specialist, 28(2), 105–114. doi: 10.1097/nur.0000000000000031 [DOI] [PubMed] [Google Scholar]
- Dyrbye LN, Shanafelt TD, Sinsky CA, Cipriano PF, Bhatt J, Ommaya A, West CP, & Meyers D (2017). Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. doi: 10.31478/201707b Retrieved 8/22/18 from https://nam.edu/burnout-among-health-care-professionals-a-call-to-explore-and-address-this-underrecognized-threat-to-safe-high-quality-care/ [DOI] [Google Scholar]
- Faris JA, Douglas MK, Maples DC, Berg LR, & Thrailkill A (2010). Job satisfaction of advanced practice nurses in the Veterans Health Administration. Journal of the American Academy of Nurse Practitioners, 22(1), 35–44. [DOI] [PubMed] [Google Scholar]
- Freeborn DK, Hooker RS, & Pope CR (2002). Satisfaction and well-being of primary care providers in managed care. Evaluation & the Health Professions, 25(2), 239–254. doi: 10.1177/01678702025002008 [DOI] [PubMed] [Google Scholar]
- Hayden ML, Davies LR, & Clore ER (1982). Facilitators and inhibitors of the emergency nurse practitioner role. Nursing Research, 31(5): 294–299. [PubMed] [Google Scholar]
- Howard PB, & Greiner D (1997). Constraints to advanced psychiatric-mental health nursing practice. Archives of Psychiatric Nursing, 11(4), 198–209. doi: 10.1016/s0883-9417(97)80027-1 [DOI] [PubMed] [Google Scholar]
- Hupcey JE (1993). Factors and work settings that may influence nurse practitioner practice. Nursing Outlook, 41(4), 181–185. [PubMed] [Google Scholar]
- Institute of Medicine, [IOM]. (2011). The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Joanna Briggs Institute [JBI]. (2016). The Joanna Briggs Institute Critical Appraisal Tools for use in JBI Systematic Reviews: Checklist for Qualitative Research. Retrieved from http://joannabriggs.org/research/critical-appraisal-tools.html [Google Scholar]
- Kutney-Lee A, Stimpfel AW, Sloane DM, Cimiotti JP, Quinn LW, Aiken LH (2015). Changes in patient and nurse outcomes associated with magnet hospital recognition. Medical Care, 53(6), 550–557. doi: 10.1097/mlr.0000000000000355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET (2002). Development of the practice environment scale of the nursing work index. Research in Nursing & Health, 25(3), 176–188. doi: 10.1002/nur.10032 [DOI] [PubMed] [Google Scholar]
- Lake ET (2007). The nurse practice environment: Measurement and evidence. Medical Care Research and Review, 64(2), 104S–122S. Doi: 10.1177/1077558707299253 [DOI] [PubMed] [Google Scholar]
- Laschinger HK, Almost J, & Tuer-Hodes D (2003). Workplace empowerment and magnet hospital characteristics: Making the link. Journal of Nursing Administration, 33(7/8), 410–422. doi: 10.1097/00005110-200307000-00011 [DOI] [PubMed] [Google Scholar]
- Laschinger HK, & Leiter MP (2006). The impact of nursing work environments on patient safety outcomes. The Journal of Nursing Administration, 36(5), 259–267. doi: 10.1097/00005110-200605000-00019 [DOI] [PubMed] [Google Scholar]
- Lelli VR, Hickman RL, Savrin CL, Peterson RA (2015). Retail clinics versus traditional primary care: Employee satisfaction guaranteed? Journal of the American Association of Nurse Practitioners. 27(9), 514–520. doi: 10.1002/2327-6924.12220 [DOI] [PubMed] [Google Scholar]
- Lindeke L, Jukkala A, & Tanner M (2005). Perceived barriers to nurse practitioner practice in rural settings. The Journal of Rural Health, 21(2), 178–181. doi.org/10.1111/j.1748-0361.2005.tb00079.x [DOI] [PubMed] [Google Scholar]
- McGibbon E, Peter E, & Gallop R (2010). An institutional ethnography of nurses’ stress. Qualitative Health Research, 20(10), 1353–1378. doi: 10.1177/1049732310375435 [DOI] [PubMed] [Google Scholar]
- Meeusen VC, Van Dam K, Brown-Mahoney C, Van Zundert AA, & Knape HT (2011a). Understanding nurse anesthetists’ intention to leave their job: How burnout and job satisfaction mediate the impact of personality and workplace characteristics. Health Care Management Review, 36(2), 155–163. doi: 10.1097/HMR.0b013e3181fb0f41 [DOI] [PubMed] [Google Scholar]
- Meeusen VC, Van Dam K, Brown-Mahoney C, Van Zundert AA, & Knape HT (2011b). Work climate related to job satisfaction among Dutch nurse anesthetists. American Association of Nurse Anesthetists Journal, 79(1), 63–70. doi: 10.1097/00000446-193311000-00040 [DOI] [PubMed] [Google Scholar]
- Motley RJ, Mazzaccaro RJ, Burmeister DB, Land SD, Boulay RM, Chung H, Deitrick L, & Sumner AD (2016). Using focus groups to identify characteristics of an ideal work environment for advanced practice clinicians. Healthcare, 4(3), 151–154. doi: 10.1016/j.hjdsi.2015.10.007 [DOI] [PubMed] [Google Scholar]
- National Council of State Boards of Nursing [NCSBN]. (2015). The 2015 environmental scan. Journal of Nursing Regulation, 5(4), s1–s36. Retrieved from https://www.ncsbn.org/6212.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norful AA, de Jacq K, Carlino R, & Poghosyan L (2018). Nurse Practitioner–Physician Comanagement: A Theoretical Model to Alleviate Primary Care Strain. The Annals of Family Medicine, 16(3), 250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norful AA, Swords K, Marichal M, Cho H, & Poghosyan L (2017). Nurse practitioner-physician co-management of primary care patients: The promise of a new delivery care model to improve quality of care. Health Care Management Review [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman I (2013). The nursing practice environment. International Journal of Nursing Studies, 50(12): 1577–1579. doi: 10.1016/j.ijnurstu.2013.09.006 [DOI] [PubMed] [Google Scholar]
- Pasaron R (2013). Nurse practitioner job satisfaction: Looking for successful outcomes. Journal of Clinical Nursing, 22(17–18), 2593–2604. doi: 10.1111/j.1365-2702.2012.04331.x [DOI] [PubMed] [Google Scholar]
- Plager K & Conger M (2006). Advanced practice nursing: Constraints to role fulfillment. The Internet Journal of Advanced Practice Nursing, 9(1). doi: 10.5580/187 [DOI] [Google Scholar]
- Poghosyan L, & Aiken LH (2015a). Maximizing nurse practitioners’ contributions to primary care through organizational changes. Journal of Ambulatory Care Management, 38(2), 109–117. doi: 10.1097/JAC.0000000000000054 [DOI] [PubMed] [Google Scholar]
- Poghosyan L, & Liu J (2016a). Nurse practitioner autonomy and relationships with leadership affect teamwork in primary care practices: A cross-sectional survey. Journal of General Internal Medicine, 31(7), 771–777. doi: 10.1007/s11606-016-3652-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poghosyan L, Liu J, & Norful AA (2017). Nurse practitioners are primary care providers with their own patient panels and organizational structures: A cross-sectional study. International Journal of Nursing Studies. doi: 10.1016/j.ijnurstu.2017.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poghosyan L, Liu J, Shang J, & D’Aunno T (2016b). Practice environments and job satisfaction and turnover intentions of nurse practitioners: Implications for primary care workforce capacity. Health Care Manage Review doi: 10.1097/HMR.0000000000000094 [DOI] [PubMed] [Google Scholar]
- Poghosyan L, Nannini A, Smaldone A, Clarke S, O’Rourke NC, Rosato BG, & Berkowitz B (2013a). Revisiting scope of practice facilitators and barriers for primary care nurse practitioners: A qualitative investigation. Policy, Politics, & Nursing Practice, 14(6), 6–15. doi: 10.1177/1527154413480889 [DOI] [PubMed] [Google Scholar]
- Poghosyan L, Nannini A, Stone PW, & Smaldone A (2013b). Nurse practitioner organizational climate in primary care settings: implications for professional practice. Journal of Professional Nursing, 29(6), 338–349. doi: 10.1016/j.profnurs.2013.07.005 [DOI] [PubMed] [Google Scholar]
- Poghosyan L, Shang J, Liu J, Poghosyan H, Liu N, & Berkowitz B (2015b). Nurse practitioners as primary care providers: Creating favorable practice environments in New York State and Massachusetts. Health Care Management Review. 40(1), 46–55. doi: 10.1097/hmr.0000000000000010 [DOI] [PubMed] [Google Scholar]
- Pron AL (2013). Job satisfaction and perceived autonomy for nurse practitioners working in nurse-managed health centers. Journal of the American Association of Nurse Practitioners, 25(4), 213–221. doi: 10.1111/j.1745-7599.2012.00776.x [DOI] [PubMed] [Google Scholar]
- Reay T, Golden-Biddle K, & Germann K (2006). Legitimizing a new role: Small wins and microprocesses of change. The Academy of Management Journal, 49(5), 977–998. [Google Scholar]
- Rudner Lugo N (2016). Full practice authority for advanced practice registered nurses is a gender issue. Online Journal of Issues in Nursing, 21(2). [DOI] [PubMed] [Google Scholar]
- Scott WR (2014). Institutions and organizations: Ideas, Interests, and identities (4th ed.). Los Angeles, CA: Sage. [Google Scholar]
- Scott WR, Ruef M Mendel PJ, & Caronna CA (2000). Institutional Change and Healthcare Organizations. The University of Chicago Press: Chicago, IL. [Google Scholar]
- Sleutel MR (2000). Climate, culture, context or work environment: Organizational factors that influence nursing practice. The Journal of Nursing Administration, 30(2), 53–58. doi: 10.1097/00005110-200002000-00002 [DOI] [PubMed] [Google Scholar]
- Starr P (1982). The social transformation of American medicine: The rise of a sovereign profession and the making of a vast industry. New York: Basic Books. [Google Scholar]
- US Department of Health and Human Services [HHS]. (2017). National Institute of Heart, Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Retrieved from https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools [Google Scholar]
- Whittemore R, & Knafl K (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52(5), 546–553. doi: 10.1111/j.1365-2648.2005.03621.x [DOI] [PubMed] [Google Scholar]


