Abstract
Iron deficiency and iron-deficiency anemia are associated with increased morbidity and mortality in a wide range of conditions. In many patient populations, this can be treated effectively with oral iron supplementation; but in patients who are unable to take or who do not respond to oral iron therapy, intravenous iron administration is recommended. Furthermore, in certain conditions, such as end-stage kidney disease, chronic heart failure, and inflammatory bowel disease, intravenous iron administration has become first-line treatment. One of the first available intravenous iron preparations is iron sucrose (Venofer®), a nanomedicine that has been used clinically since 1949. Treatment with iron sucrose is particularly beneficial owing to its ability to rapidly increase hemoglobin, ferritin, and transferrin saturation levels, with an acceptable safety profile. Recently, important new data relating to the use of iron sucrose, including the findings from the landmark PIVOTAL trial in patients with end-stage kidney disease, have been reported. Several years ago, a number of iron sucrose similars became available, although there have been concerns about the clinical appropriateness of substituting the original iron sucrose with an iron sucrose similar because of differences in efficacy and safety. This is a result of the complex and unique physicochemical properties of nanomedicines such as iron sucrose, which make copying the molecule difficult and problematic. In this review, we summarize the evidence accumulated during 70 years of clinical experience with iron sucrose in terms of efficacy, safety, and cost-effectiveness.
Keywords: Anemia, Iron deficiency, Iron sucrose, Nanomedicine, Venofer
Key Summary Points
| Intravenously administered (IV) iron is important for individuals who are unable to tolerate oral iron therapy, who are non-compliant with oral treatment, or in whom oral preparations are not effective. |
| One of the first IV iron preparations to be manufactured is iron sucrose (Venofer®; Vifor Pharma), which became available for clinical use over 70 years ago in 1949. It is the most commonly used IV iron therapy worldwide, with clinical experience encompassing 25 million patient-years. |
| Many studies across a broad range of therapy areas consistently demonstrate that iron sucrose is able to correct iron deficiency, in addition to promoting erythropoiesis and subsequently reducing the required doses of erythropoiesis-stimulating agents (ESAs). Not only is iron sucrose effective, but it is also well tolerated and rapidly increases bioavailable iron supplies. |
| Since the last review focused on iron sucrose was published in 2014, reassuring clinical data have continued to become available on iron sucrose from a number of studies. Most notably, the recently published PIVOTAL trial in patients with end-stage kidney disease compared the efficacy and safety of high- versus low-dose iron sucrose. |
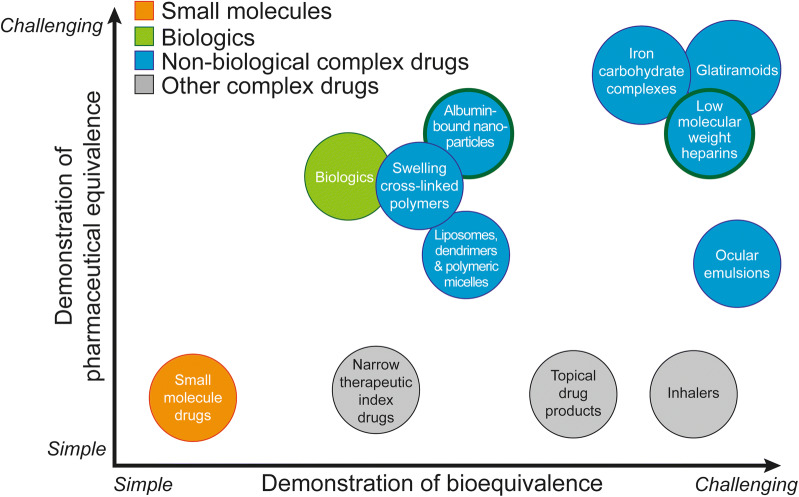
| Generic substitution of iron sucrose similar for iron sucrose should not be assumed to provide therapeutic equivalence, as the complex physicochemical properties of the original agent are extremely difficult to duplicate and studies have not been able to conclusively demonstrate that iron sucrose similars have safety and efficacy equivalent to that of iron sucrose. |
Introduction
Iron plays an important role in key cellular metabolic pathways in addition to its role in heme synthesis and subsequent oxygen transport [1]. Iron deficiency and iron-deficiency anemia typically occur as a consequence of a severe underlying condition, such as inflammatory bowel disease (IBD), gastrointestinal (GI) bleeding, chronic heart failure (CHF), chronic kidney disease (CKD), or cancer [2–9]. Heavy menstrual bleeding and pregnancy may also result in iron deficiency [10, 11]. Effective treatment of iron deficiency/iron-deficiency anemia is important to relieve symptoms, including extreme fatigue and tiredness, as well as to alleviate the adverse impact on quality of life [11–16]. Furthermore, anemia is a risk amplifier for mortality and morbidity in patients with heart disease [17] and those with CKD [18–20]. Iron deficiency, even in the absence of anemia, can be debilitating and can exacerbate any underlying chronic disease, leading to increased morbidity and mortality [21, 22]; for example, iron deficiency can be predictive of negative disease outcomes and has been associated with a worse prognosis in CHF [23, 24]. Additionally, in patients with iron deficiency undergoing cardiac surgery, mortality is elevated threefold, irrespective of the presence or absence of anemia [25]. Preoperative anemia, which is most commonly caused by iron deficiency, is also associated with an increased risk of poor outcomes after surgery [26, 27]. Iron deficiency and iron-deficiency anemia generate considerable financial burdens due to additional medical costs and loss of productivity [28].
Iron administration is recommended for the management of iron deficiency/iron-deficiency anemia associated with a variety of conditions [2–4, 7–10, 29, 30]. The Network for Advancement of Transfusion Alternatives recommends that iron deficiency is treated before using erythropoiesis-stimulating agents (ESAs) in patients with anemia [31, 32]. This is also advocated in guidelines for the treatment of anemia in CKD [33, 34]. Corrective strategies to normalize iron levels and hemoglobin (Hb) are recommended as part of perioperative care to optimize outcomes in patients undergoing surgery [35]. In patients lacking a response to, or unable to tolerate, oral iron therapy, treatment with intravenously administered (IV) iron should be considered [9]. There are also circumstances in which IV iron is recommended for use as first-line treatment, including cases of severe iron-deficiency anemia [2–4] and when rapid correction of Hb levels is warranted (e.g., when less than 6 weeks prior to surgery [35]), or in certain patient groups with iron deficiency/iron-deficiency anemia such as those with CHF [3, 4, 30], hemodialysis-dependent CKD [3, 4, 8], severe IBD, or cancer [7, 29]. Advantages of parenteral iron therapy include (1) similar or superior effectiveness, often with a more rapid response [36, 37]; (2) avoidance of poor or unreliable intestinal absorption, which is particularly problematic in patients with increased hepcidin levels associated with inflammatory conditions [37]; and (3) improved tolerability, as the GI side effects of oral iron therapy are avoided [38]. Several IV iron carbohydrate preparations are available (Table 1).
Table 1.
Overview of characteristics of approved IV iron formulations.
Adapted from Muñoz and Martín-Montañez. Reprinted by permission of the publisher (Taylor & Francis Ltd, https://www.tandfonline.com) [175]
| Iron gluconate | Iron sucrose | LMWID | Ferric carboxymaltose | Iron isomaltoside 1000 | Ferumoxytol | |
|---|---|---|---|---|---|---|
| Brand name | Ferrlecit® | Venofer® | Cosmofer® | Ferinject®, Injectafer® | Monofer® | FeraHeme® |
| Manufacturer | Sanofi-Aventis | Vifor Pharma | Pharmacosmos | Vifor Pharma, American Regent | Pharmacosmos | AMAG Pharmaceuticals |
| Carbohydrate shell | Gluconate (monosaccharide) | Sucrose (disaccharide) | Dextran (branched polysaccharide) | Carboxymaltose (branched polysaccharide) | Isomaltoside (linear oligosaccharide) | Polyglucose sorbitol (branched polysaccharide) |
| Molecular weight measured by manufacturer, kDa | 289–440 | 34–60 | 165 | 150 | 150 | 750 |
| Initial distribution volume, L | 6 | 3.4 | 3.5 | 3.5 | 3.4 | 3.16 |
| Terminal half-life (dose in mg Fe) [176] | 1.42 h (125) | 5.3 h (100) | 27–30 h (500–2000) | 7.4/9.4 h (100/1000) | 20.8/22.5 h (100/200) | 14.7 h (316) |
| Labile iron, % of dose | 3.3 | 3.4 | 1.9 | 0.6 | 1 | 0.9 |
| Direct iron donation to transferrin, % of dose | 5–6 | 4–5 | 1–2 | 1–2 | < 1 | < 1 |
| Iron content, mg/mL | 12.5 | 20 | 50 | 50 | 100 | 30 |
| Maximal single dose, mg (minimum administration time)a [176, 177] | 125 (10–60 min) | 200 (10–30 min) | 20 mg/kg BW (4–6 h) | 1000 (15 min) | 20 mg/kg BW (1 h) | 510 (15 min) |
BW body weight, IV intravenously administered, LMWID low molecular weight iron dextran
aMost common maximal dose and corresponding minimal administration time; the exact posology may vary between markets. Please refer to local prescribing information
One of the first IV iron preparations to be manufactured is iron sucrose (Venofer®; Vifor Pharma), which became available for clinical use over 70 years ago, in 1949. Indeed, like aspirin, it is one of the oldest therapeutic agents still being used widely today. The active ingredient of Venofer is an iron(III) hydroxide–sucrose complex, and the product is now registered in 91 countries worldwide. Indeed, it is the most commonly used IV iron formulation worldwide, with clinical experience encompassing 25 million patient-years [39].
The aim of this article is to provide a comprehensive overview of Venofer, focusing mainly on the characteristics, pharmacokinetics, efficacy, safety, and limitations associated with this iron preparation. While IV Venofer has a long history, there are a number of reasons why a review of its therapeutic use is timely. Firstly, important new data on the use of this iron sucrose preparation have recently become available. A large open-label, blinded-endpoint study in 2141 patients undergoing hemodialysis (PIVOTAL study) has recently demonstrated the clinical benefits of a proactive high-dose iron regimen of iron sucrose (Venofer) compared with a reactive low-dose iron regimen, including a lower incidence of death, heart attack, stroke, and hospitalization for heart failure, as well as reduced ESA dose requirements and use of blood transfusions [40]. Secondly, various iron sucrose similars have been developed and introduced as generic alternatives to Venofer. However, several recent studies have suggested that the therapeutic equivalence of Venofer and follow-on products cannot be assumed, given that these are complex nanomedicine entities that may have clinically relevant differences in their physicochemical properties.
In order to identify peer review publications of interest, we searched PubMed using the terms “iron sucrose” and filtered results by publication date (limited to the last 25 years), article type (clinical trials and reviews), human species, and English language. This review article is based on previously conducted studies and does not contain unpublished data from any studies with human participants or animals performed by any of the authors.
Pharmacokinetics and Pharmacodynamics
Venofer is rapidly cleared from the serum of healthy subjects, with a terminal half-life of 5.3 ± 1.6 h and total body clearance of 1.23 ± 0.22 L/h (20.5 ± 3.7 mL/min) [41]. Following IV administration of iron sucrose into patients with anemia, iron is rapidly taken up by the liver, spleen, and bone marrow [42]. The majority (97%) of injected iron is utilized for red blood cell (RBC) synthesis in these patients, and serum ferritin and transferrin saturation (TSAT) increase within 24 h and 1 week, respectively [42]. Furthermore, less than 5% of the overall elimination of Venofer in healthy individuals can be attributed to undesirable renal elimination, due to a relatively large molecular mass (greater than 18 kDa) [21].
Efficacy of Iron Sucrose in Various Conditions
The efficacy of iron sucrose has been demonstrated in a wide range of conditions that cause or are associated with iron deficiency and iron-deficiency anemia, as summarized below. Across these various conditions, iron sucrose treatment is associated with improved iron status (ferritin, TSAT); increased Hb levels, with or without ESA therapy; and improved health-related quality of life and clinical outcomes. When used in combination with ESA therapy, iron sucrose substantially reduces ESA dose requirements.
Chronic Kidney Disease
As summarized in Table 2, studies have consistently reported that iron sucrose is an effective treatment for iron deficiency/iron-deficiency anemia in patients with CKD, leading to increased Hb, serum ferritin, and TSAT in patients regardless of whether they are undergoing hemodialysis or receiving ESAs [40, 43–54].
Table 2.
Published clinical studies using iron sucrose in chronic kidney disease
| Study | Inclusion criteria | Patients, n | Patient dialysis status | Iron dose (mg)/dose, interval, treatment duration | Outcomes and safety information |
|---|---|---|---|---|---|
| Studies of iron sucrose | |||||
| Macdougall et al. (2019) [40] |
ESRD TSAT < 30% SF < 400 ng/mL |
High-dose IS + ESA: 1093 Low-dose IS + ESA: 1048 |
Hemodialysis ≤ 12 months prior to screening |
400 mg, monthly 0–400 mg, monthly 2.1 years (median follow-up) |
Significantly fewer events (non-fatal MI, non-fatal stroke, hospitalization for heart failure, or death) with high-dose IS versus low-dose IS (29.3% vs. 32.3%; p < 0.001 [non-inferiority]; p = 0.04 [superiority]) No differences between groups in SAEs, hospitalization, infection rate, or vascular access thrombosis |
| Haddad et al. (2009) [43] | Intolerance to iron dextran | IS + ESA: 15 | Hemodialysis | 100 mg q.w. |
Significant hematocrit increase No hypersensitivity reactions or effects on intradialytic blood pressure |
| Mircescu et al. (2006) [44] |
Hb < 11 g/dL SF < 200 ng/mL |
IS: 60 | No dialysis | 200 mg, monthly, 1 year |
Significant, continuous, and progressive Hb increase No worsening of renal function, blood pressure changes, or SAEs |
| Tagboto et al. (2008) [45] | Hb < 11.5 g/dL | IS: 82 | No dialysis | 4 × 200 mg, q.w. |
Hb increase in 74% of patients No specific safety results reported |
| Deng et al. (2017) [46] |
RLS TSAT < 20% SF < 200 ng/mL |
IS: 16 Placebo: 16 |
Hemodialysis | 100 mg, t.i.w. (1000 mg total) |
2 weeks after last injection, decrease in IRLS score was significantly greater for IS versus placebo, and increases in SF, TSAT, and Hb were significantly greater for IS versus placebo No AEs were observed |
| Wan and Zhang (2018) [47] |
Hb 10.0–13.0 g/dL SF 100–500 ng/mL iPTH < 800 pg/mL |
Continuous IS + ESA: 17 Intermittent IS + ESA: 17 |
Hemodialysis |
100 mg every session (1000 mg total; completed in 1 month) 100 mg q.w. (1000 mg total; completed in 3 months) |
SF levels increased significantly in both groups Hb levels were similar between groups, but intermittent IS significantly reduced Hb variability versus continuous IS No AEs were observed |
| Mitsopoulos et al. (2020) [54] |
Hb 9–11.5 g/dL TSAT < 45% SF < 500 ng/mL |
IS + ESA: 18 | Stable peritoneal dialysis | 200 mg loading dose, followed by 100 mg monthly for 5 months |
Hb and SF increased significantly from baseline ESA dose was reduced in five patients and discontinued in one No patients experienced any side effects related to IS |
| Comparative studies of iron sucrose versus oral iron formulations | |||||
| Li and Wang (2008) [48] |
Hb 6.0–9.0 g/dL TSAT < 30% SF < 500 ng/mL |
IS + ESA: 70 FeS + ESA: 66 |
Hemodialysis |
100 mg b.i.w. then q.w. 200 mg FeS t.i.d., 12 weeks |
Significant Hb increase versus baseline in both groups and with IS versus FeS No AEs with IS, 33.3% GI symptoms with FeS |
| Van Wyck et al. (2005) [49] |
Hb ≤ 11 g/dL TSAT ≤ 25% SF ≤ 300 ng/mL |
IS + ESA: 91 FeS + ESA: 91 |
No dialysis |
2 × 500 or 5 × 200 mg, 14 days 65 mg t.i.d., 56 days |
Significantly better Hb response (ΔHb ≥ 1.0 g/dL) and increase with IS versus FeS Dysgeusia most prominent IS-related GI complaint (6.6%) Fewer GI side effects with IS 200 mg (11.5%) and IS 500 mg (3.3%) versus FeS (17.6%) |
| Li and Wang (2008) [51] |
Hb 6.0–9.0 g/dL TSAT < 30% SF < 500 ng/mL |
IS + ESA: 26 FeS + ESA: 20 |
Peritoneal dialysis |
200 mg q.w. over 4 weeks then q.2.w. 200 mg FeS t.i.d., 8 weeks |
Significant Hb increase versus baseline in both groups and with IS versus FeS No AEs with IS, 40% GI symptoms with FeS |
| Agarwal et al. (2015) [52] |
Hb < 12 g/dL TSAT < 25% SF < 100 ng/mL |
IS ± ESA: 69 FeS ± ESA: 67 |
GFR > 20 and ≤ 60 mL/min/1.73 m2 (no hemodialysis) |
IS 200 mg, weeks 0, 2, 4, 6, 8 FeS 325 mg t.i.d., 8 weeks 24 months |
Increases in Hb similar between groups SF was significantly higher with IS versus FeS only from baseline to 6 months IS was associated with greater risk of infections and cardiovascular complications versus FeS GI AEs were more common with FeS, whereas gout was more frequent in the IS group |
| Comparative studies of iron sucrose versus other IV iron formulations | |||||
| Bhandari et al. (2015) [50] |
Hb 9.5–12.5 g/dL TSAT < 35% SF < 800 ng/mL |
IS + ESA: 117 IIso + ESA: 234 |
Hemodialysis |
IS according to local package insert/guidelines IIso 500 mg, single bolus IIso (split dose) 100 mg (baseline) + 200 mg (weeks 2 and 4) 6 weeks (follow-up) |
No significant difference in Hb control between groups Increases in SF from baseline to weeks 1, 2, and 4 were significantly greater for IIso versus IS Frequency, type, and severity of AEs were similar between groups |
| Macdougall et al. (2014) [58] |
Hb < 11.0 and ≥ 7.0 g/L TSAT < 30% |
IS: 82 FeruM: 80 |
On dialysis and not on dialysis |
200 mg × 5 within 14 days (non-dialysis) 100 mg for 10 consecutive sessions (dialysis 2 × 510 mg within 5 days) 5 weeks (follow-up) |
Increases in Hb similar between groups AE profiles similar between groups |
| Macdougall et al. (2019) [55] |
Hb < 11.5 g/dL TSAT < 30% SF ≤ 800 ng/mL |
IS: 97 FeruM: 196 |
Hemodialysis |
100 mg for 10 consecutive sessions 2 × 510 mg within 5 days 5 weeks (follow-up) |
Increases in Hb similar between groups AE profiles similar between groups |
| Onken et al. (2014) [53] |
Hb < 11.5 g/dL TSAT ≤ 30% SF ≤ 100 ng/mL (or ≤ 300 ng/mL if TSAT criterion met) |
IS ± ESA: 1294 FCM ± ESA: 1290 |
GFR < 60 mL/min/1.73 m2, non-dialysis-dependent |
IS 200 mg days 0, 7, and 14 + two additional doses (max. 1000 mg) FCM 15 mg/kg days 0 and 7 (max. 1500 mg), day 56 (end of treatment) |
Increase in Hb was statistically higher with FCM versus IS Increases in SF, TSAT, and serum iron were significantly greater in the FCM group versus IS Protocol-defined hypertensive events were significantly more common with FCM versus IS, whereas protocol-defined hypotensive events were more common with IS than FCM No significant difference in the primary composite safety endpoint (all-cause death, non-fatal MI, non-fatal stroke, unstable angina requiring hospitalization, congestive heart failure requiring hospitalization or medical intervention, cardiac arrhythmia, and hypertensive or hypotensive events) between treatment groups |
AE adverse event, b.i.w. twice weekly, ESA erythropoiesis-stimulating agent, ESRD end-stage renal disease, FCM ferric carboxymaltose, FeruM ferumoxytol, FeS ferrous succinate, GFR glomerular filtration rate, GI gastrointestinal, Hb hemoglobin, IIso iron isomaltoside 1000, iPTH intact parathyroid hormone, IRLS International Restless Legs Syndrome Study Group rating scale, IS iron sucrose, IV intravenously administered, MI myocardial infarction, q.2.w. every 2 weeks, q.w. weekly, RLS restless legs syndrome, SAE serious adverse event, SF serum ferritin, t.i.d. three times daily, t.i.w. three times weekly, TSAT transferrin saturation
In adults undergoing maintenance hemodialysis, differing regimens, including continuous and intermittent administration of iron sucrose, have been examined [40, 43, 46–48, 50, 55]. While each of these studies has demonstrated benefits of iron sucrose in maintenance hemodialysis, the most conclusive results are reported in the recent PIVOTAL study, a landmark trial that is already changing clinical practice and will almost certainly impact on future clinical guidelines. PIVOTAL was a multicenter, open-label trial with blinded-endpoint evaluation in 2141 hemodialysis patients; it is the largest prospective, controlled clinical trial of IV iron in patients with CKD [40]. In the PIVOTAL trial, patients were randomized into two groups: one receiving high-dose iron sucrose proactively (400 mg monthly; with temporary discontinuation of treatment if safety cutoffs of ferritin 700 µg/L or TSAT of 40% were exceeded) and the other group receiving low-dose iron sucrose administered reactively (0–400 mg monthly, adjusted to achieve minimum targets for ferritin and TSAT of 200 µg/L and 20%, respectively) [40]. Importantly, within the context of a rigorous study design, this study showed that the risk of cardiovascular adverse events (AEs), infections, hospitalization, and death was lower or similar with high-dose iron sucrose compared with low-dose iron sucrose.
High-dose iron sucrose was superior to low-dose iron sucrose with respect to the primary composite endpoint of non-fatal myocardial infarction, non-fatal stroke, hospitalization for heart failure, or death (p < 0.001 for non-inferiority; p = 0.04 for superiority) [40]. The effect of high-dose iron sucrose on the primary endpoint was consistent across all of the prespecified subgroups (duration of dialysis treatment, diabetes status, and vascular access). In addition, proactive administration of high-dose iron appeared to protect against recurrent cardiovascular events. An additional benefit of high-dose iron sucrose was the subsequent reduction in ESA dose required by patients in this group and the reduced likelihood of requiring blood transfusions [40].
Relative to the low-dose strategy, the high-dose approach to iron sucrose administration was not associated with any safety signals. There was no difference in vascular access thrombosis, or in hospitalizations between the dosing groups [40]. Additionally, infection rates were virtually identical between the high-dose and low-dose iron sucrose groups, suggesting no association between iron dose, ferritin/TSAT, and the risk of infection [40, 56]. This is reassuring because it has been previously suggested that IV iron administration may increase the risk of infection [57].
Studies comparing iron sucrose with oral iron administration consistently show iron sucrose to be more effective in patients with CKD, with significantly better outcomes in Hb, hematocrit, serum ferritin, and TSAT, as well as reduced recombinant human erythropoietin (rhEPO) dose requirements [48, 51].
Randomized trials have indicated that iron sucrose has comparable efficacy to other IV iron formulations in CKD; for example, ferumoxytol and iron sucrose have similar efficacy in patients with CKD, including in patients undergoing hemodialysis [55, 58]. An additional trial suggested superior efficacy of iron isomaltose versus iron sucrose in patients with non-dialysis CKD, although different dosing regimens make a direct comparison of these products problematic [59].
Limited data are available on the use of IV iron in peritoneal dialysis patients. A recent study has assessed the safety and efficacy of iron sucrose in this patient population and has shown that monthly maintenance with iron sucrose may improve iron parameters and erythropoietin response [54].
Chronic Heart Failure
Iron deficiency and anemia are commonly observed in patients with CHF. Anemia was previously thought to be a major contributor to the progression of CHF [60, 61]. In patients with CHF, iron deficiency is associated with increased mortality [24], increased risk of hospitalization [62], and reduced quality of life [14, 63]. A number of studies have evaluated the treatment effects of iron sucrose in patients with anemia and patients without anemia, both alone [64–68] and in combination with rhEPO [60, 69, 70]. A summary of the studies on iron sucrose use in CHF is provided in Table 3.
Table 3.
Published clinical studies using iron sucrose in patients with chronic heart failure
| Study | Inclusion criteria | Patients, n | Iron dose (mg)/dose, interval, treatment duration | Outcomes and safety information |
|---|---|---|---|---|
| Bolger et al. (2006) [65] | Stable systolic heart failure and Hb ≤ 12 g/dL | IS: 16 | 200 mg (10 mL) IV bolus over 10 min on days 1, 3, and 5 of study | IS improved hematological parameters (Hb, serum iron, SF, TSAT), symptoms, and exercise capacity (NYHA functional class, MLHFQ score, 6MWT). ISC was well tolerated with no local or systemic AEs |
| Silverberg et al. (2003) [60] | Octogenarians with anemia and severe, resistant CHF | IS: 40 | Combination of SC EPO (4–5 K IU/week, increasing to 10 K IU/week to a target Hb of 12.5 g/dL) and IS 200 mg in 150 mL saline IV infusion over 60 min every 1–2 weeks until SF reached 500 µg/L or iron saturation reached 40% or Hb reached 12.5 g/dL | Mean ± SD duration of follow-up was 17.4 ± 10 months. IS in combination with EPO significantly increased Hb, serum iron, SF, and % iron saturation and also improved NYHA, LVEF, and VAS index. Significantly fewer hospitalizations were reported compared with a comparable period prior to the study |
| Silverberg et al. (2003) [69] | Individuals with and without diabetes with moderate to severe resistant CHF (and CRF); NYHA functional classes I–IV and Hb range of 9.5–11.5 g/dL | IS: 179 (84 individuals with type 2 diabetes; 95 without diabetes) | Combination of SC EPO (4–5 K IU/week, increasing to 10 K IU/week to a target Hb of 12.5 g/dL) and IS 200 mg in 150 mL saline IV infusion over 60 min every 1–2 weeks until SF reached 500 µg/L or iron saturation reached 40% or Hb reached 12.5 g/dL | In individuals with/without diabetes with severe CHF and mild to moderate CRF, correction of anemia by the combined use of EPO and ISC was associated with improvements in LVEF and cardiac functional status (NYHA and VAS) and slowing of the rate of deterioration of renal function |
| Comin-Colet et al. (2009) [70] | Stable advanced CHF (NYHA class III–IV) and anemia (men, Hb < 13.0 g/dL; women, Hb < 12.0 g/dL) and mild to moderate renal dysfunction | IS: 27 | EPO (4 K IU/week, adjusted as necessary to achieve and maintain a target Hb between 12.5 and 14.5 g/dL). IS 200 mg in 100–200 mL saline IV infusion over 60–90 min q.w. for 5–6 weeks until SF reached 400 µg/L or TSAT of 40% or Hb > 14.5 g/dL. IS then given every 4–6 weeks to maintain these levels | Mean ± SD follow-up was 15.3 ± 8.6 months. Long-term combined therapy with EPO and ISC increased Hb, reduced NT-proBNP, and improved functional capacity and cardiovascular hospitalization rates |
| Toblli et al. (2007, 2015) [64, 66] | LVEF ≤ 35%; NYHA functional class II–IV; anemia with Hb < 12.5 g/dL for men and < 11.5 g/dL for women; SF < 100 ng/mL and/or TSAT ≤ 20%. Renal insufficiency (creatinine clearance ≤ 90 mL/min) | IS: 30 | 200 mg/200 mL ISC 60 min IV infusion q.w. for 5 weeks | At 6 months post-treatment, patients receiving ISC infusion experienced significant increases in Hb level, SF, and TSAT. Heart rate and body mass index were significantly reduced in the IS group, while LVEF was significantly increased, as were NYHA scores. Inflammatory markers CRP and NT-proBNP were also significantly reduced. Echocardiographic evaluation showed significant improvements in LVSd and LVDd, suggesting a positive effect on cardiac muscle. A significant improvement in renal function was also observed. Side effects were minimal across both groups and no severe drug-related AEs were reported |
| Okonko et al. (2008) [67] | Aged ≥ 21 years with symptomatic CHF (NYHA functional class II–IV; exercise limitation pVO2 ≤ 18 mL/kg/min; Hb < 12.5 g/dL (group with anemia) or 12.5–14.5 g/dL (group without anemia) | IS: 24 | IS administered at 200 mg in 50 mL saline via IV infusion over 30 min q.w. for 16 weeks. Then at weeks 4, 8, 12, and 16 thereafter | IS resulted in a significant treatment effect for SF, TSAT, and Hb levels in the patients with anemia. An improvement in exercise tolerance (pVO2), NYHA functional class, PGA, and fatigue score was also observed with IS in the patients with anemia. AE profiles were similar between groups: 42% and 64% in the IS and control groups, respectively. All events were unrelated (76%) or unlikely to be related (24%) to the study drug |
| Beck-da-Silva et al. (2013) [178] | Aged ≥ 18 years; NYHA functional class II–IV and able to perform ergospirometry; LVEF < 40%; Hb ≥ 9 and ≤ 12 g/dL; TSAT < 20%; SF < 500 μg/L |
IS: 10 FeS: 7 Placebo: 6 |
IS 200 mg IV infusion over 30 min q.w. for 5 weeks then oral placebo t.i.d. for 8 weeks FeS 200 mg orally t.i.d. for 8 weeks then IV placebo q.w. for 5 weeks Oral placebo t.i.d. for 8 weeks, then IV placebo q.w. for 5 weeks 3-month follow-up |
Correction of anemia, defined as Hb > 12 g/dL for women and > 13 g/dL for men, was achieved by two patients with IS, three with FeS, and two with placebo. Hb increase > 1.5 g/dL occurred in three patients each in the IS and FeS groups. SF levels increased from baseline with both IS and FeS (but not placebo), but this was only statistically significant for FeS. TSAT > 20% was achieved by five patients in each of the IS and FeS groups pVO2 increased by 3.5 mL/kg/min with IS whereas there was no change in pVO2 with oral iron (no statistically significant difference between groups) |
| Usmanov et al. (2008) [68] | Hb < 11 g/dL on two occasions within 1 week; serum creatinine < 4 mg/dL and NYHA classification III/IV | IS: 19 NYHA III and 13 NYHA IV; 22 healthy controls | IS 100 mg IV q3w for 3 weeks, then q.w. for 23 weeks (total dose 3200 mg of elemental iron over 26 weeks) | Hb, serum iron, SF, and TSAT were significantly lower in patients with NYHA classification III/IV versus healthy controls at baseline. The mean values of these parameters were significantly increased after 6 months of treatment with IV IS versus baseline. There were no AEs noted in any patient |
6MWT 6-min walk test, AE adverse event, CHF chronic heart failure, CRF chronic renal failure, CRP C-reactive protein, EPO erythropoietin, FeS ferrous sulfate, Hb hemoglobin, IS iron sucrose, ISC iron sucrose complex, IV intravenous, LVDd left ventricular diastolic diameter, LVEF left ventricular ejection fraction, LVSd left ventricular systolic diameter, MLHFQ Minnesota Living with Heart Failure Questionnaire, NT-proBNP N-terminal pro-B-type natriuretic peptide, NYHA New York Heart Association, PGA Patient Global Assessment, pVO2 peak oxygen uptake, q3w every 3 weeks, q.w. weekly, SC subcutaneous, SD standard deviation, SF serum ferritin, t.i.d. three times daily, TSAT transferrin saturation, VAS Visual Analog Scale
Intravenous administration of iron sucrose alone to patients with anemia and CHF improves the hematological parameters of Hb, ferritin, and TSAT [64–68]. Reductions in inflammatory markers such as natriuretic peptides and C-reactive protein (CRP) have also been observed after iron sucrose treatment [64, 66, 70].
These biochemical changes appear to be associated with symptom improvement in patients with CHF, while in one study, echocardiographic evaluation demonstrated significant improvements in left ventricular systolic diameter and left ventricular diastolic diameter [66]. In line with these findings, an improvement in cardiac remodeling was also observed in another study in patients with CHF [68].
Inflammatory Bowel Disease and Other Gastrointestinal Disorders
A summary of the studies of iron sucrose use in adults with GI disorders is provided in Table 4.
Table 4.
Published clinical studies using iron sucrose in gastrointestinal disorders
| Study | Inclusion criteria | Patients, n | Iron dose (mg)/dose, interval, treatment duration | Outcomes and safety information |
|---|---|---|---|---|
| Comparative studies of iron sucrose versus oral iron formulations | ||||
| Lindgren et al. (2009) [72] |
Hb < 11.5 g/dL SF < 300 ng/mL |
IS: 45 FeS: 46 |
200 mg q.w. or q.2.w. up to cumulative dose of 1000 mg 100 mg b.i.d., 20 weeks |
66% versus 47% Hb response to IS versus FeS (p = 0.07) One possibly related SAE (thrombocytopenia) with IS, AEs with FeS dominated by GI events |
| Lee et al. (2017) [73] | TSAT < 16% ± SF < 30 ng/mL (if normal CRP) or < 100 ng/mL (if elevated CRP) |
IS: 36 FeS: 36 |
3 × 300 mg (iron deficiency only); 4 × 300 mg (with anemia) 300 mg b.i.d 12 weeks (follow-up) |
Hb and TSAT levels similar between groups SF significantly higher with IS versus FeS Gut microbiota and metabolome altered differently by FeS and IS |
| Gisbert et al. (2009) [75] |
Hb < 12 or 13 g/dLa TSAT < 12% SF < 30 ng/mL |
IS: 22 FeS: 78 |
200 mg b.i.w. if Hb < 10 g/dL until calculated dose 106 mg q.d. if Hb > 10 g/dL |
77% and 89% response rate in IS and FeS group, respectively No AEs with IS, 5.1% with oral iron therapy intolerance (nausea, abdominal pain, and constipation), which led to discontinuation of treatment |
| Comparative studies of iron sucrose versus other IV iron formulations | ||||
|
Lichtenstein and Onken (2018) [74] [Pooled analysis of four studies] |
Hb ≤ 12 g/dL (one study); ≤ 11 g/dL (three studies) SF ≤ 100 ng/mL or ≤ 300 ng/mL if TSAT ≤ 30% (all four studies) |
IS: 32 FCM: 101 Oral iron: 25 Other IV iron: 61 |
15 mg/kg or 750 mg (variable dosing schedules) |
Hb, SF, and TSAT values increased significantly from baseline for all groups, with the exception of SF values in the oral iron group FCM and IS resulted in greater increases in Hb than orally administered and other IV iron products, which may be due to lower baseline Hb levels Safety profile of FCM was comparable with the other agents Incidence of treatment-related SAEs was 0% with FCM versus 6.3% with IS |
| Evstatiev et al. (2011) [76] |
Hb 7–12 g/dL for men and 7–12 g/dL for women SF < 100 µg/mL |
IS: 235 FCM: 240 |
200 mg (up to 11 doses) Maximum of three infusions of 1000 or 500 mg |
More patients with FCM than IS achieved Hb response (p = 0.04) or Hb normalization (p = 0.015). Both treatments improved quality of life scores by week 12 Study drugs were well tolerated and drug-related AEs were in line with drug-specific clinical experience |
AE adverse event, b.i.d. twice daily, b.i.w. twice weekly, CRP C-reactive protein, FCM ferric carboxymaltose, FeS ferrous sulfate, GI gastrointestinal, Hb hemoglobin, IS iron sucrose, IV intravenous, q.2.w. every 2 weeks, q.d. daily, q.w. weekly, SAE serious adverse event, SF serum ferritin, TSAT transferrin saturation
aFemale Hb < 12 g/dL, male < 13 g/dL
IBD (including Crohn’s disease and ulcerative colitis) is often treated with anti-inflammatory drugs, including tumor necrosis factor-alpha (TNFα) inhibitors. However, the persistence of anemia as a complication despite anti-TNFα treatment highlights the need for iron therapy even when biologics are used [71]. Oral iron therapy, however, is problematic for patients with IBD as a result of chronic inflammation leading to poor absorption and tolerance. In this respect, and consistent with findings in patients with CKD, several studies in patients with iron deficiency and iron-deficiency anemia associated with IBD indicate that iron sucrose is more efficacious than oral iron therapy [72, 73].
A study in patients with iron-deficiency anemia and IBD demonstrated significantly better outcomes in the iron sucrose arm for two out of three primary endpoints compared with oral iron sulfate therapy: fewer iron sucrose-treated patients remained anemic and more patients achieved Hb reference levels [72].
In a pooled analysis of four trials evaluating a total of 191 patients with iron-deficiency anemia resulting from GI disorders, greater increases in Hb levels were apparent in patients treated with iron sucrose compared with those receiving oral iron therapy [74]. However, the interpretation of these findings is somewhat problematic because patients with Hb levels below 10 g/dL were given iron sucrose treatment and patients with higher Hb levels (at least 10 g/dL) were treated with oral ferrous sulfate therapy. Iron sucrose treatment in patients with lower Hb levels (below 10 g/dL) led to 77% of subjects achieving normal Hb levels after 3 months. Oral administration of ferrous sulfate in patients with higher baseline Hb levels (at least 10 g/dL) resulted in 89% achieving normalized Hb [75]. Although the authors of this study reported that all patients were in remission, more details on the overall disease severity of the two groups would be of interest. Patients with IBD and severe anemia (Hb below 10 g/dL) usually have more severe and relapsing disease associated with a higher need for iron supplementation compared with patients with mild anemia and inactive disease. Moreover, the recurrence of anemia after iron treatment may be higher in patients with severe anemia.
When comparing iron sucrose with ferric carboxymaltose (FCM), Hb response rates were similar to those seen in the studies described above and in Table 4; however, outcomes with FCM were significantly better [76]. The pooled analysis in patients with GI disorders described above found that FCM was associated with greater increases in ferritin and TSAT compared with iron sucrose, although increases in Hb levels were similar [74].
Pediatric studies in children with GI disorders are summarized in the relevant section below.
Women’s Health, Including Obstetrics and Gynecology
A summary of the studies investigating iron sucrose use in women’s health (including in the pregnancy and postpartum settings) is provided in Table 5.
Table 5.
Published clinical studies using iron sucrose in obstetrics, gynecology, and women’s health disorders
| Study | Inclusion criteria | Patients, n | Iron dose (mg)/dose, interval, treatment duration | Outcomes and safety information |
|---|---|---|---|---|
| Use of iron sucrose during pregnancy and postpartum | ||||
| Al-Momen et al. (1996) [150] |
Gest. age < 32 weeks Hb < 9.0 g/dL SF < 20 ng/mL |
IS: 52 FeS: 59 |
IS: 200 mg q.d. or t.i.w. FeS: 60 mg t.i.d. |
Significantly higher Hb levels with IS versus FeS Self-limiting fever and tightness in skin (one each) with IS, 30% GI events and 32% non-compliance with FeS, 6% could not tolerate FeS |
| Al et al. (2005) [79] |
Gest. age 26–34 weeks Hb 8.0–10.5 g/dL SF < 13 ng/mL |
IS: 45 IPC: 45 |
IS: 200 mg until calculated dose, 5 days IPC: 100 mg t.i.d., whole pregnancy |
Significantly better Hb increase with IS versus IPC Possibly related AEs to IS: metallic taste (n = 11), hot flush (n = 12), dizziness (n = 8), nausea (n = 5), arthralgia (n = 1), vomiting (n = 1); significantly fewer GI symptoms with IS versus FeS (13.3% vs. 28.9% upper GI events) |
| Bayoumeu et al. (2002) [80] |
Hb 8.0–10.0 g/dL SF < 50 ng/mL |
IS: 24 FeS: 23 |
IS: 6 × 200 mg until calculated dose, 21 days FeS: 80 mg t.i.d., 4 weeks |
Hb increase in both groups without significant difference “Not-unpleasant taste” only AE with IS, during injection (dysgeusia). One treatment interruption due to AE (diarrhea) with FeS |
| Bencaiova et al. (2009) [81] |
Gest. age 15–20 weeks Hb < 10.5 g/dL SF < 100 ng/mL |
IS: 130 FeS: 130 |
IS: 200 or 300 mg FeS: 80 mg q.d. |
Significant Hb increase versus baseline in both groups Mild anemia (16.2%), infections (6.9%), muscle pains (2.3%), pruritus (2.3%), cough (1.5%), breast disorders (1.5%) with IS; GI events only with FeS (17.7%), 14 SAEs in IS group (preterm contractions n = 3, premature rupture of the membranes n = 3, moderate anemia after delivery n = 2, threatened preterm delivery because of cervical insufficiency n = 2, intrauterine growth restriction n = 2, infection n = 1, injury n = 1), seven SAEs in FeS group (preterm contractions n = 2, vaginal bleeding n = 1, premature rupture of the membrane n = 1, infection n = 1, gestational diabetes mellitus n = 1, postpartum pulmonary embolism n = 1) |
| Tariq et al. (2015) [82] |
Gest. age > 12 weeks Hb < 10.5 g/dL SF < 12 µg/L |
IS: 93 Iron dextran: 105 |
≥ 1 antepartum 300 mg IS dose |
IS and iron dextran were equally effective in treatment of IDA during pregnancy No major side effects were observed in either group |
| Hamm et al. (2018) [83] | Third trimester Hb < 9.5 g/dL |
IS: 25 No IS: 364 |
≥ 1 antepartum 300 mg IS dose | The earlier IS was received before delivery, the greater the median Hb increase. Only those receiving IS > 2 weeks before delivery had a significant increase in Hb level from third trimester to delivery. Increasing administrations incrementally impacted Hb difference from third trimester to delivery, with only those receiving ≥ 3 doses demonstrating statistically significant Hb change compared with the no IS group |
| Hamm et al. (2019) [84] | Third trimester Hb < 9.5 g/dL |
IS: 65 No IS: 458 |
Exact doses not stated |
Third trimester Hb was lower in the IS group compared with the no IS group Despite lower starting Hb in the IS group, antepartum IS reduced transfusions in patients with a third trimester Hb < 9.5 g/dL |
| Breymann et al. (2001) [85] |
Hb < 10.0 g/dL SF ≤ 15 ng/mL |
IS: 20 IS + ESA: 20 |
200 mg, b.i.w. |
Both regimens were effective; increases in hematocrit were greater from day 11 (p < 0.01) and the median duration of therapy was shorter (18 vs. 25 days) with adjuvant ESA Well tolerated; metallic taste was reported in 8% and warm feeling in 5% |
| Krafft et al. (2009) [86] |
Hb < 10.0 g/dL SF ≤ 15 ng/mL |
IS: 27 IS + ESA: 57 |
200 mg, b.i.w. |
IS or IS + ESA was effective: the overall Hb level after therapy was 11.0 g/dL (note: 32 patients responded poorly initially to IS alone, thus receiving additional ESA) Well tolerated; most patients reported metallic taste |
| Bencaiova et al. (2006) [87] | SF ≤ 15 ng/mL | IS + ESA: 19 | 100 mg, b.i.w. |
At the end of therapy, Hb, HCT, and serum EPO were statistically significantly improved cf. at the start (p = 0.01, p = 0.004, and p = 0.006, respectively) Well tolerated and no detectable negative effects on newborn or fetus |
| Bhandal et al. (2006) [88] |
Hb < 9.0 g/dL SF < 15 ng/mL |
IS: 22 FeS: 21 |
IS: 200 mg e.o.d., 3 days FeS: 200 mg b.i.d., 6 weeks |
Significantly better Hb increase with IS versus FeS 23% metallic taste, 18% facial flushing with IS, 33% GI events with FeS No SAEs, no hemodynamic disturbances during or after infusion |
| Giannoulis et al. (2009) [89] |
Hb < 8.0 g/dL SF < 10 ng/mL |
IS: 78 FeProtSu: 26 |
IS: 100 mg q.d., 3 days FeProtSu: 800 mg q.d., 28 days |
Significantly better Hb increase with IS versus FeProtSu Two AEs with IS (headache, nausea), 11 AEs with FeProtSu (constipation n = 5, hiccup n = 4, heartburn n = 2) |
| Westad et al. (2008) [90] | Hb 6.5–8.5 g/dL |
IS: 58 FeS: 70 |
IS: 200 mg q.d., 3 days FeS: 100 mg b.i.d., 12 weeks |
Hb increase in both groups Few and transient AEs with IS (phlebitis, pain at injection site), 22.9% withdrew because of drug-related AEs with FeS (GI events most common reason) |
| Perello et al. (2014) [130] | Hb 6–8 g/dL |
IS + FeS: 36 Placebo + FeS: 36 |
IS: 200 mg q.d., 2 days FeS: 525 mg b.i.d., 30 days |
Hb values were comparable in women receiving IS or placebo in addition to oral iron therapy at any of the time points. No differences were found between clinical symptoms of anemia, psychological status, and AEs between groups |
| Krafft and Breymann (2011) [91] |
Hb < 8.5 g/dL 24–48 h after delivery |
IS: 20 IS + ESA: 20 |
200 mg q.d., 4 days |
Hb values were close to normal in both groups within 2 weeks Both treatments were well tolerated; minor side effects included metallic taste in 30% of patients and warm flush in 8% of patients |
| Wågström et al. (2007) [92] | Hb ≤ 80 g/dL within 72 h after delivery |
IS: 15 IS + rhEPO 1: 19 IS + rhEPO 2: 15 |
IS: 200 mg q.d., day 0, day 3 IS + rhEPO 1: IS 200 mg q.d., day 0, day 3 + rhEPO 10,000 U on day 0, day 3 IS + rhEPO 2: IS 200 mg q.d., day 0, day 3 + rhEPO 20,000 U on day 0, day 3 |
Hb increased significantly in all three groups over time (p < 0.001), and there were no differences between the treatment groups on any day of evaluation (p = 0.59). The total mean increment in Hb in all subjects was 18 g/dL after 1 week and 28 g/dL after 2 weeks |
| Breymann et al. (2000) [93] | Hb < 10.0 g/dL |
IS: 20 IS + ESA: 20 Oral iron: 20 |
200 mg q.d., 4 days |
All three regimens were effective; day 7 hematocrit increases were higher with adjuvant ESA than for IS or oral iron alone: 8% versus 5% and 4%, respectively (both comparisons p < 0.01) Well tolerated |
| Use of iron sucrose for general women’s health | ||||
| Krayenbuehl et al. (2011) [94] |
Hb ≥ 12.0 g/dL SF ≤ 50 ng/mL |
IS: 43 Placebo: 47 |
200 mg q.d., 4 days |
Trend for better improvement of fatigue score with IS versus placebo 21% drug-related AEs with IS (nausea, chills, headache, dizziness, chest pain, dysesthesia, dysgeusia), 7% AEs with placebo (nausea, headache, dizziness, diarrhea) |
| Lee et al. (2019) [96] |
Menorrhagia Hb < 10 g/dL SF < 30 ng/mL |
IS: 49 FCM: 52 |
IS: 200 mg q.d. (≤ 600 mg/week) FCM: < 50 kg, 500 mg/week; ≥ 50 kg, 1000 mg/week |
FCM was as effective as IS in achieving Hb ≥ 10 g/dL within 2 weeks after first administration (78.8% vs. 72.3%). The time to reach Hb ≥ 10 g/dL was significantly shorter in the FCM group versus the IS group (7.7 days vs. 10.5 days). Mean Hb levels were higher in the FCM-treated patients than in the IS-treated patients (borderline significance, p = 0.013). QoL scores did not differ between groups. No deaths, anaphylactic reactions, or transfusion requirements were reported in either group. All AEs were mild |
AE adverse event, b.i.d. twice daily, b.i.w. twice weekly, e.o.d. every other day; EPO erythropoietin, ESA erythropoiesis-stimulating agent, FCM ferrous carboxymaltose, FeProtSu ferrous protein succinylate, FeS ferrous sulfate, Gest. gestational, GI gastrointestinal, HCT hematocrit, Hb hemoglobin, IDA iron-deficiency anemia, IPC iron polymaltose complex, IS iron sucrose, q.d. daily, QoL quality of life, SAE serious adverse event, rhEPO recombinant human erythropoietin, SF serum ferritin, t.i.d. three times daily, t.i.w. three times weekly
Pregnancy and Postpartum
Maintenance of normal iron stores is important not only for the health of the prospective mother, but also for that of her child. A recent summary of meta-analyses of the effects of iron status and iron therapy concluded that maternal anemia was associated with adverse birth and neonatal outcomes and that iron treatment reduced the risk of this [77]. A recent Swedish cohort study of over 500,000 children born between 1987 and 2010 and followed up until the end of 2016 found that the risks of developing autism, attention-deficit hyperactivity disorder, and intellectual disability were all increased in children of mothers who had prenatal anemia during the first 30 weeks of pregnancy [78].
Reflecting results in CKD and IBD, studies in pregnant women with iron deficiency indicate that iron sucrose is more effective than oral iron administration and is at least as effective in pregnant women with iron-deficiency anemia. For women with severe iron deficiency during pregnancy, iron sucrose treatment has been shown to increase Hb levels more effectively than an oral iron polymaltose complex [79], whereas in pregnant women with less severe iron-deficiency anemia and in those using iron prophylactically, Hb levels were comparable following either iron sucrose or oral ferrous sulfate treatment [80, 81].
Administering iron sucrose from the third trimester to pre-delivery can significantly increase Hb levels and reduce blood transfusion rates in pregnant women with third trimester Hb levels below 9.5 g/dL, compared with patients who did not receive iron sucrose [83]. Treatment with a minimum of three iron sucrose doses at least 2 weeks prior to delivery appears optimal for increasing Hb levels and treating antepartum anemia [84].
Addition of rhEPO to iron sucrose therapy can enhance the effectiveness of treatment of iron-deficiency anemia in pregnancy. In a study of pregnant women with iron-deficiency anemia resistant to treatment with oral iron therapy alone, iron sucrose administered either with or without rhEPO effectively treated anemia. However, increases in reticulocytes and hematocrit were greater, and more patients achieved target Hb levels at 4 weeks with the combination of rhEPO and iron sucrose compared with iron sucrose alone. Safety was similar in the two treatment groups [85]. Selective addition of rhEPO to iron sucrose for women with severe anemia or an inadequate response to iron sucrose alone has also been shown to be an effective approach to treatment of iron-deficiency anemia in pregnancy [86].
Furthermore, iron sucrose has demonstrated equal if not superior efficacy compared with oral iron administration in women with iron-deficiency anemia in the postpartum setting. For these women, a study has shown that iron sucrose treatment can achieve higher Hb levels than oral ferrous sulfate treatment [88]. Iron sucrose followed by standard oral iron treatment after 4 weeks also replenished iron stores more rapidly and resulted in a greater improvement in fatigue score compared with oral iron treatment alone in a randomized study of women with postpartum iron-deficiency anemia [90].
The effectiveness of iron sucrose either with or without rhEPO was assessed in a randomized study in women with severe postpartum anemia. Hb returned to near-normal levels within 2 weeks in both treatment groups. The findings suggest that iron sucrose alone is sufficient for the treatment of postpartum anemia for most women, although additional rhEPO treatment may benefit a subgroup of patients with pronounced inflammatory responses [91]. A second study in women with postpartum anemia found that the addition of rhEPO did not further increase Hb concentrations above those achieved with IV iron sucrose treatment alone [92], while another study reported greatest hematocrit increases with rhEPO and iron sucrose compared with either iron sucrose or oral iron treatment alone (both p < 0.01) [93].
General Women’s Health
Besides its use in pregnant women with iron-deficiency anemia, iron treatment can also benefit women with low ferritin levels and without anemia. In fatigued, premenopausal women with low ferritin levels and without anemia, iron sucrose treatment (four infusions of 200 mg iron during the first two study weeks) showed a trend toward a greater improvement in fatigue compared with placebo. The difference between the groups was significant in those with initial serum ferritin levels of 15 ng/mL or below [94].
A large number of women are iron deficient and suffer from fatigue. It has therefore been suggested that parenteral iron administration could benefit many women and could become more accepted. However, those who will benefit most, and the doses of iron required for an effect, need to be further defined [95].
Two randomized clinical studies have demonstrated that iron sucrose is effective for the correction of iron-deficiency anemia due to heavy menstrual bleeding (menorrhagia) [96, 97]; in one study, 72% of women who received treatment with iron sucrose achieved Hb levels of at least 10 g/dL within 2 weeks after the first administration [96].
Patient Blood Management
A summary of the studies assessing iron sucrose use in patient blood management is provided in Table 6.
Table 6.
Published clinical studies using iron sucrose in patient blood management
| Study | Inclusion criteria | Patients, n | Iron dose (mg)/dose, interval, treatment duration | Outcomes and safety information |
|---|---|---|---|---|
| Use of iron sucrose in the preoperative setting | ||||
| Theusinger et al. (2011) [101] | Preoperative orthopedic surgery | IS: 20 | 900 mg over 10 days |
Hb and SF levels increased significantly. TSAT did not change significantly. Endogenous EPO decreased from 261 to 190 pg/mL 2 weeks after IV iron treatment (p = 0.050, not significant after Bonferroni correction) No AEs related to IS were observed |
| Rohling et al. (2000) [102] |
Preoperative elective surgery Hb < 14.0 g/dL |
IS + ESA: 6 FeS + ESA: 6 |
IS: 200 mg b.i.w., 3 weeks FeS: 160 mg/day, 3 weeks |
Hb levels increased in both groups; Hb level increased significantly over 3 weeks with IS + ESA but not with FeS + ESA Preoperative reticulocyte count and SF were significantly higher with IS + ESA than FeS + ESA No dose-limiting AEs or allergic reactions were observed Two patients receiving FeS reported mild GI effects (constipation, epigastric pain) |
| Olijhoek et al. (2001) [103] |
Preoperative elective orthopedic surgery Hb ≥ 10.0 to ≤ 13.0 g/dL SF ≥ 50 ng/mL |
IS + ESA: 29 Oral iron + ESA: 29 IS + placebo: 25 Oral iron + placebo: 27 |
IS: 200 mg day 1 and day 8 Oral iron: 200 mg/day, 2 weeks |
IS + ESA and oral iron + ESA significantly increased total RBC production, Hb, HCT, and reticulocytes versus respective placebo groups; no significant differences for IS + ESA versus oral iron + ESA IS + placebo, and oral iron + placebo was not associated with increases in hematological values Incidence of AEs similar between groups; no thrombotic and/or vascular events were reported |
| Braga et al. (1995) [179] |
Preoperative stomach or colorectal cancer HCT < 34% SF < 700 ng/mL |
IS: 11 IS + ESA: 11 No iron: 11 (neither anemic nor iron deficient) |
IS: 200 mg q.d., 12 days IS + ESA: 200 mg q.d., days 1, 4, 8, 12 |
In the IS group, no patients could donate autologous blood compared with all patients in the IS + ESA group 36% of patients in the IS group received perioperative transfusion of homologous blood compared with none in the IS + ESA group No major AEs with either regimen |
| Xu et al. (2019) [104] | Preoperative hip fracture repair |
IS: 32 ESA: 32 IS + ESA: 32 |
3 days before surgery Dose not stated |
Combined IS + ESA was more effective than either EPO or IS alone Hb increased significantly more after IS + ESA than after either EPO or IS alone No significant difference in the incidence of adverse drug reactions among the three groups |
| Kim et al. (2009) [105] |
Menorrhagia Hb < 9.0 g/dL |
IS: 39 FeProtSu: 37 |
200 mg, e.o.d. t.i.w. 80 mg q.d., 3 weeks |
Significantly better Hb increase and response rate with IS versus FeProtSu Two myalgia events and one injection pain event with IS; one event each of nausea and dyspepsia with FeProtSu; no severe AEs reported |
| Use of iron sucrose in the perioperative setting | ||||
| Karkouti et al. (2006) [106] |
Postoperative anemia Hb 7–9 g/dL |
IS: 13 IS + ESA: 12 No iron: 13 |
200 mg days 1, 2, 3 postoperatively | With no between-group differences, early postoperative treatment with IS alone or in combination with ESA did not appear to accelerate early recovery from postoperative anemia |
| Madi-Jebara et al. (2004) [107] |
Postoperative cardiac surgery Hb 7–10 g/dL |
IS: 40 IS + ESA: 40 No iron: 40 |
200 mg q.d. to reach total iron deficit |
No significant difference in transfusion rates No significant difference in Hb increase Postoperative IS, with or without ESA, is not effective at correcting postoperative anemia No AEs with IS |
| Serrano-Trenas et al. (2011) [108] | Perioperative hip fracture surgery |
IS: 99 No iron: 97 |
200 mg, 3 × e.o.d. |
No significant difference in RBC transfusions between groups 3.0% AE-related treatment suspension with IS (one skin rash, two general discomfort); overall, 14.8% infections (mainly superficial surgical wound infections 5.6%) |
| Garrido-Martín et al. (2012) [109] |
Perioperative cardiac surgery Hb < 8 g/dL coronary patients; < 7 g/dL valve surgery patients |
IS: 54 Oral iron: 53 Placebo: 52 |
IS: 100 mg × 3 during perioperative period Oral iron: 105 mg q.d. pre- and postoperatively, and 1 month after discharge |
No between-group differences in Hb, HCT, or transfusions Neither IS nor oral iron therapy were effective in correcting anemia after cardiac surgery No AEs with IS |
| Shin et al. (2019) [110] |
Perioperative orthopedic surgery Meta-analysis |
1869 patients from 12 clinical trials | Various IV iron | Perioperative IV iron during orthopedic surgery, especially postoperatively, appears to reduce the proportion of patients transfused and units transfused, with shorter length of hospital stay and decreased infection rate |
| Xu et al. (2019) [111] |
Postoperative cardiac valvular surgery Hb < 12.0 g/dL (women) or < 13.0 g/dL (men) SF 30–100 ng/mL or TSAT < 20% |
IS: 75 Placebo: 75 |
200 mg e.o.d., until total iron deficiency was achieved |
Hb concentration and proportion of patients with anemia corrected or achieving Hb increments > 2.0 g/dL were significantly greater for IS than placebo 14 days postoperatively, but not 7 days postoperatively SF were significantly higher for IS versus placebo 7 days and 14 days postoperatively IS was well tolerated: no AEs or infusion reactions were observed |
| Muñoz et al. (2014) [112] |
Perioperative orthopedic surgery Hb ≥ 10.0 g/dL |
IS: 1142 IS + EPO: 351 FCM: 45 No iron: 1009 |
100–200 mg up to 3 × (2–5 days preoperatively or 2–3 days postoperatively) |
Very short-term perioperative IV iron in major lower limb orthopedic procedures is associated with reduced allogeneic blood transfusion rates and length of hospital stay In patients with hip fracture, IV iron is also associated with a reduction in postoperative nosocomial infection No significant AEs with IV iron |
| Pareja Sierra et al. (2019) [113] |
Perioperative hip fracture Descriptive study |
IS + ESA: 40 Transfusion: 12 Transfusion + IS + ESA: 51 No treatment: 27 |
Hb < 8.5 g/dL: transfusion Hb 8.5–10 g/dL: 2 × 200 mg (48 h apart) Hb 10–11 g/dL: 2 × 400 mg (48 h apart) |
IS did not reduce the proportion of transfused patients (56% transfused vs. 44% not transfused receiving IS), but it did reduce the number of blood units required Patients who received IS had better functional recovery than those who did not No AEs with IS |
| Montano-Pedroso et al. (2018) [114] |
Postoperative bariatric abdominoplasty Hb < 11.5 g/dL SF < 11 ng/mL |
IS: 28 Oral iron: 28 |
IS: 200 mg immediately and 1 day postoperatively Oral iron: 100 mg b.i.d. 8 days |
Superiority of IS was not shown; the minimum clinically relevant difference in Hb concentrations was not reached No AEs in the IS group Constipation (18%), diarrhea (11%), and nausea (4%) were reported with oral iron |
AE adverse event; b.i.d. twice daily, b.i.w. twice weekly, e.o.d. every other day, EPO erythropoietin, ESA erythropoiesis-stimulating agent, FCM ferric carboxymaltose, FeProtSu ferric protein succinylate, FeS ferrous sulfate, GI gastrointestinal, Hb hemoglobin, HCT hematocrit, IV intravenously administered, IS iron sucrose, q.d. every day, RBC red blood cell, SF serum ferritin, t.i.w. three times weekly, TSAT transferrin saturation
Preoperative Iron Treatment
Preoperative anemia is present in 30–40% of patients scheduled for elective surgery and can complicate surgery, increasing the likelihood of blood transfusion or intensive care admission, increasing the risk of infections or thromboembolic events, and prolonging the length of hospital stay [35, 98–100]. In addition, and as mentioned previously, in patients undergoing elective cardiac surgery, iron deficiency with and without concomitant anemia is associated with a threefold increase in mortality, more postoperative serious adverse outcomes, more blood transfusions, and longer intensive care and hospital stay than patients without iron deficiency [25].
Iron sucrose is an effective pre-surgical treatment for iron-deficiency anemia and has been shown to increase Hb, ferritin, and soluble transferrin receptor levels when administered prior to orthopedic surgery [101]. Increases in Hb were greatest 2 weeks after initiating iron sucrose treatment, suggesting that the optimal time to initiate iron sucrose may be 2–3 weeks prior to elective surgery [101].
In patients without anemia receiving rhEPO who were due for elective surgery, iron sucrose was associated with significantly higher ferritin and reticulocyte counts than with oral ferrous sulfate therapy, and prevented iatrogenic iron depletion [102]. In a separate study, there was no difference between oral iron therapy and IV iron in supporting preoperative erythropoietin-driven stimulation of erythropoiesis (transfusions were not reported) [103].
A benefit of iron sucrose and an ESA was also demonstrated in patients undergoing surgery for hip fractures. Combined treatment resulted in increased Hb levels and a lower transfusion rate compared with the use of either iron sucrose or ESA alone [104].
In surgical patients with iron-deficiency anemia resulting from heavy menstrual bleeding, iron sucrose achieved significantly better preoperative Hb and ferritin levels than oral iron protein succinylate treatment [105]. However, the study is limited by the premature cessation of the oral iron arm in the study.
Perioperative Iron Treatment
Results from four randomized controlled trials did not find convincing benefits of perioperative iron in orthopedic or cardiac surgery [106–109]. In contrast, however, a recent meta-analysis of IV iron therapies, including iron sucrose, showed that perioperative IV iron therapy during orthopedic surgery was associated with several benefits, including reduced transfusion rates and shorter hospital stays, but without impacting the mortality rate [110]. Additionally, a separate randomized study showed that the use of iron sucrose can significantly increase Hb levels versus placebo control in patients undergoing cardiac surgery [111]. This is important as patients undergoing cardiac surgery are at risk of postoperative functional iron deficiency.
For patients undergoing surgery for fractures, several studies have suggested a benefit of utilizing iron sucrose, particularly for hip fractures. A number of improved outcomes have been associated with perioperative IV iron (including iron sucrose) in patients undergoing surgery for hip fracture and arthroplasty, as highlighted in a pooled analysis of observational data, with benefits including reduced transfusion rates, shorter hospital stays, reduced infection rates (hip fracture only), and lower 30-day mortality (hip fracture only) [112].
Blood Donors
Birgegård et al. investigated the frequency and severity of iron depletion in regular blood donors and the effects of iron sucrose and oral iron sulfate therapy on iron status [115]. Iron sucrose was found to substitute iron loss in blood donors more efficiently compared with oral iron sulfate treatment, especially in women, and also reduced the severity of restless leg syndrome, which can occur as a complication of iron deficiency.
Oncology
A summary of the studies on iron sucrose use in oncology is provided in Table 7.
Table 7.
Published clinical studies using iron sucrose in oncology
| Study | Inclusion criteria | Patients, n | Iron dose (mg)/dose, interval, treatment duration | Outcomes and safety information |
|---|---|---|---|---|
| Hedenus et al. (2007) [116] |
Clinically stable lymphoproliferaltive malignancy Hb 9.0–11.0 g/dL |
IS + ESA: 33 ESA: 34 |
100 mg q.w. (weeks 0–6); 100 mg q.2.w. (weeks 8–14) 16 weeks (follow-up) |
Significantly greater Hb increase from week 8 onward with IS versus no IS Proportion of patients with Hb increase ≥ 2 g/dL was significantly higher with IS (93%) than no IS (53%; p = 0.001) ESA dose lower with IS than no IS from week 5 onward AEs were distributed evenly between groups |
| Beguin et al. (2013) [118] |
Autologous SCT SF > 100 ng/mL |
IS + ESA: 23 ESA: 25 No ESA: 24 |
200 mg on days 28, 42, and 56 after SCT |
Complete Hb response within 18 weeks achieved by 100% with IS + ESA, 79% with ESA, 21% with no ESA Erythropoietic response significantly higher with IS + ESA than ESA, resulting in lower ESA use, reduced drug costs, and improved quality of life scores; effect on transfusions was not significant Safety findings were similar between groups |
|
Jaspers et al. (2015) [119] [Long-term follow-up of Beguin et al. (2013) [118]] |
Autologous SCT SF > 100 ng/mL |
IS + ESA: 50 ESA: 52 No ESA: 25 |
1.4 years (median follow-up) |
Overall survival (1-year and 5-year) and progression-free survival (1-year and 5-year) not significantly different between groups Incidence of infections remained comparable between groups Other serious complications were uncommon and hardly attributable to ESA or IS |
| Dangsuwan and Manchana (2010) [120] | Hb < 10.0 g/dL |
IS: 22 FeS: 22 |
IS: 200 mg FeS: 200 mg t.i.d. |
Significantly higher Hb and significantly fewer RBC transfusions with IS than FeS Most common AEs were mild nausea and vomiting; no significant difference in AEs between groups; no SAEs or hypersensitivity reactions |
| Kim et al. (2007) [121] | Hb < 12.0 g/dL |
IS: 30 No iron: 45 |
1 × 200 mg per CT cycle |
Significant reduction in RBC transfusions with IS versus no iron No treatment-related AEs with IS; transfusion-related allergic reactions with similar frequency in both groups |
AE adverse event, CT chemotherapy, ESA erythropoiesis-stimulating agent, FeS ferrous sulfate, Hb hemoglobin, IS iron sucrose, q.2.w. every 2 weeks, q.w. every week, RBC red blood cell, SAE serious adverse event, SCT stem cell transplantation, SF serum ferritin, t.i.d. three times daily
Anemia is a common side effect of cancer treatments and ESAs may be used to aid in RBC production. In patients with anemia and lymphoproliferative malignancies who were not receiving chemotherapy, the addition of iron sucrose to an ESA resulted in a significantly faster and greater Hb increase compared with ESA therapy alone [116]. Furthermore, using data from this study [116], when iron sucrose was given as an additional therapy, ESA dose requirements were reduced from week 5 onward, allowing cost savings over the study period [117].
In patients with multiple myeloma or lymphoma who had undergone autologous hematopoietic cell transplantation, supplementation of an ESA with iron sucrose increased the proportion of patients with Hb responses from 79% to 100%, reduced the median response time, and lowered ESA dose requirements compared with those receiving no iron treatment [118]. There was no impact of iron sucrose treatment on long-term clinical outcomes or survival [119].
Utilization of iron sucrose in the absence of ESAs can also benefit some oncology patients by improving Hb levels and reducing the need for RBC transfusions [120–122].
Pediatric Populations
Data on the use of iron sucrose within pediatric patients are limited. The data that are available, however, suggest that iron sucrose is an effective option (Table 8).
Table 8.
Published clinical studies using iron sucrose in pediatric patients
| Study | Inclusion criteria | Patients, n | Iron dose (mg)/dose, interval, treatment duration | Outcomes and safety information |
|---|---|---|---|---|
| Crary et al. (2011) [123] |
Aged ≤ 18 years ≥ 1 dose of IS Patients could not have CKD |
IS: 38 |
Median dose: 100 mg Median number of infusions: 3 |
Patients had a good response to IS, with a median Hb rise of 1.9–3.1 g/dL depending on the indication IS was well tolerated with only one serious reaction (temporary and reversible hypotension) in a patient who had received IS 500 mg, which was greater than the recommended dose of 300 mg |
| Akarsu et al. (2006) [124] |
SF < 12 ng/mL Low Hb (adjusted for age) |
IS: 62 | Variable depending on observed Hb and body weight |
All children showed improvements in iron-deficiency anemia between diagnosis and week 1 IS was well tolerated with mild AEs in 13% of children |
| Pinsk et al. (2008) [125] |
Hb > 2 × SD below 15.5% level corrected for age SF < 16 ng/mL Did not respond to oral iron |
IS: 45 | Variable depending on observed Hb and body weight |
IS was effective at raising Hb concentration in all patient groups IS was well tolerated; one patient experienced transient hypotension and vomiting, and two patients had drug extravasation |
| Danko and Weidkamp (2016) [126] | IBD and iron-deficiency anemia | IS: 24 | 3 mg/kg (maximum 200 mg) |
IS was effective for routine management of iron-deficiency anemia in children with IBD IS significantly increased mean SF, TSAT, and Hb levels There were no adverse reactions |
| Danko et al. (2019) [128] | IBD and iron-deficiency anemia | IS: 39 | 3 mg/kg (maximum 200 mg) |
Mean Hb levels rose to 12.68 mg/dL and 12.86 mg/dL by 3 and 6 months, respectively, then remained normal (> 13 mg/dL) Mean SF/TSAT had normalized by 3 months and remained normal Significant positive correlations were found between the increase in Hb and improvement in emotional/physical quality of life scores |
| Venturieri et al. (2019) [127] |
IBD Hb below normal levels according to age SF < 30 ng/mL TSAT < 16% |
IS: 16 | Variable depending on observed Hb and body weight |
All patients had increased Hb Almost 70% of patients achieved therapeutic success (minimum increase of 2 g/dL of Hb and/or normalized Hb levels) No AEs were reported |
| Sharma et al. (2016) [129] |
Postmenarchal females aged < 21 years SF < 20 ng/mL Fatigue |
IS: 20 | 4 × 200 mg over 14 days |
Clinically significant improvement in fatigue in 19/20 patients at 6 weeks, 3 months, and 6 months after treatment IS was well tolerated, with IS-related AEs in four (20%) patients: two reported headache and two reported nausea |
AE adverse event, CKD chronic kidney disease, Hb hemoglobin, IBD inflammatory bowel disease, IS iron sucrose, SD standard deviation, SF serum ferritin, TSAT transferrin saturation
In children with, or at risk of, iron deficiency/iron-deficiency anemia, iron sucrose appears effective in those who cannot tolerate or do not respond to oral iron therapy (recommended maximum single dose of 7 mg iron per kg to minimize the risk of AEs) [123]. Where iron sucrose has been used in children with iron deficiency and iron-deficiency anemia, significant improvements in Hb levels have been shown [124, 125].
Where children also suffer from IBD, the use of oral iron therapy is difficult. In this setting, iron sucrose is effective for the routine management of iron-deficiency anemia. Children with iron deficiency resulting from IBD (which was treated with the anti-inflammatory drug infliximab) displayed significantly increased mean ferritin, TSAT, and Hb levels after treatment with iron sucrose, and a higher proportion of these children also had normalized ferritin, TSAT, and Hb levels versus historical control data from the same patients [126]. Similarly, in a cohort of children with IBD (mean age 11.3 years) who were mildly to severely anemic, iron sucrose (median dose 638.4 mg) increased Hb levels in all 16 patients, and ferritin and TSAT levels were also statistically higher post-infusion [127]. Another study in children with IBD showed that correction of iron-deficiency anemia using IV iron sucrose therapy was significantly correlated with better health-related quality of life scores [128].
Whether with anemia or without, postmenarchal adolescent female inviduals with iron deficiency tolerate iron sucrose well and treatment is associated with a sustained increase in ferritin and improvements in fatigue symptoms [129]. Interestingly, Hb levels in female individuals without anemia remained unchanged, suggesting a non-hematological function of iron in reducing fatigue.
Safety and Tolerability of Iron Sucrose
Because of the poor absorption and tolerance of oral iron therapy in patients suffering from conditions with chronic inflammation, the use of IV iron treatment has been studied extensively and the safety of iron sucrose use is well established. Indeed, iron sucrose has been widely used over many decades, extending to over 25 million patient-years of clinical use [39]. The safety profile is therefore well established in many different patient groups, including CKD, GI disorders, women’s health disorders, oncology, cardiology, and for patient blood management (Tables 2, 3, 4, 5, 6, 7). To date, more than 50 published clinical studies, covering numerous patient populations, have reported safety outcomes with administration of iron sucrose; 18 of these studies have been reported in the last 5 years [40, 46, 47, 50, 52, 53, 58, 66, 73, 74, 111, 113, 114, 126, 127, 129–131].
The summary of product characteristics for Venofer describes distortion of taste (dysgeusia) as being the most commonly reported AE at 4.5% [132]; however, this is not considered serious and in recent studies has only been reported in 0–2.3% of participants [40, 53, 94]. Other most common AEs with iron sucrose (occurring in at least 1% and less than 10% of patients) include hypotension, hypertension, nausea, and injection site reactions [132]. When they do occur, these AEs are generally categorized as being mild.
Additional potential AEs of iron sucrose and other IV iron formulations relate to a positive iron balance, which can arise if the increase in total body iron content is not compensated by equivalent iron losses. Patients receiving long-term therapy with parenteral iron may remain in a chronic state of positive iron balance [133]. This may lead to iron overload. Organs that appear to be most susceptible to the damaging effects of iron overload are the liver, heart, endocrine glands, and joints [133]. There is currently uncertainty around the risks of iron overload associated with IV iron treatment, but available data suggest that current treatment practices, for example in patients with CKD, are not associated with overt clinical toxicity despite a theoretical risk of positive iron balance [134].
Paravenous leakage of medication from the vein into the surrounding tissue is another potential complication of intravenously administered medication. Reactions are usually minor and transient, characterized by skin irritation, localized pain and inflammation, although paravenous leakage of IV iron may also cause long-lasting or permanent skin discoloration [135].
Contradictory evidence exists regarding whether iron treatment is linked with increased bacterial infection [136–139]. The REVOKE study comparing oral iron therapy versus IV iron sucrose in patients with CKD was terminated early because of significantly more infection-related AEs occurring in the IV iron group compared with the oral iron group (28.4% vs. 15.9%) [52]. However, there has been much debate surrounding the validity of the safety analyses from this study [140]. Questions have been raised regarding the statistical analyses driving the significance of the study findings; results were only significant when the analyses were adjusted for prognostic baseline characteristics (e.g., age, cardiovascular disease, and hospitalized infections) [141]. Several researchers have queried whether such adjustments were appropriate within a randomized trial [141, 142]. Also, in a systematic review and meta-analysis of IV versus oral iron supplementation for the treatment of anemia in CKD, REVOKE was identified as the only study at high risk of bias for selective outcome reporting according to the Cochrane criteria [143]. In contrast, the randomized FIND-CKD study found similar infection rates (most commonly of the urinary tract) between IV FCM (targeting higher [400–600 μg/L] or lower [100–200 μg/L] ferritin) and oral iron therapy [36, 140]. There was also a comparable rate of hospitalization because of infection between the FCM groups and oral iron therapy [140]. Most data associating IV iron with increased infection risk are derived from observational studies, and the evidence examining an association between IV iron use and infection is inconclusive. During a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference, it was concluded that there was insufficient evidence on the potential dangers of long-term IV iron treatment [133]. At the time, the authors of that report welcomed the upcoming PIVOTAL study as a randomized trial that would provide concrete answers to these safety questions [40]. The PIVOTAL study has since been published and is the largest randomized trial that has been performed with any IV iron. This multicenter study reported the same overall infection rates, as well as hospitalization and death from infection, between a proactive high-dose iron sucrose strategy and a reactive low-dose iron sucrose strategy in incident patients undergoing maintenance hemodialysis [40]. Moreover, a recently published case-crossover study specifically assessed whether IV iron treatment increases the risk of infectious disease. They found that IV iron treatment did not increase short-term infection risk among hemodialysis patients [144]. Nevertheless, consistent with previous recommendations in patients with CKD [33], avoidance of IV iron should be considered in the setting of active systemic infection to prevent hypothetically exacerbating the infection.
As noted previously, various IV iron formulations exist. Bailie et al. compared AE profiles for iron sucrose, iron dextrans, and ferric gluconate using US Food and Drug Administration (FDA) and World Health Organization (WHO) pharmacovigilance databases between 1997 and 2009 [145, 146]. Data revealed that iron sucrose use was associated with a significantly lower rate of AEs compared with iron dextran (highest rate) and ferric gluconate (intermediate rate). While a retrospective cohort of patients with hemodialysis-dependent CKD displayed similar longer-term safety profiles when receiving iron sucrose or ferric gluconate, modest decreases in infection-related hospitalizations and deaths were observed in those receiving iron sucrose [131]. Moreover, iron sucrose was associated with fewer type 1 hypersensitivity AEs and a lower incidence of life-threatening allergic AEs compared with iron dextran and ferric gluconate [145, 146], and was rarely associated with non-anaphylactoid reactions (e.g., non-life-threatening hypotension, nausea, and exanthema) [147]. Iron sucrose can also be administered to patients with intolerance to iron dextran or ferric gluconate [147]. Hypersensitivity reactions with IV iron therapy are generally very rare, but findings have varied among different IV iron treatments. In a recent retrospective pharmacoepidemiological study comparing all available IV iron products, iron sucrose showed one of the lowest reporting rates for severe hypersensitivity, although the limitations of such analyses of pharmacovigilance data are well recognized [148]. Similarly, among patients in a study in the US Medicare non-dialysis population to compare the risk of anaphylaxis among marketed IV iron products, anaphylaxis risk was lowest for iron sucrose [149].
A number of studies in pregnant women have shown there to be no serious AEs when using iron sucrose (Table 5) [79–82, 150]. Although side effects were reported in 40/130 (30.8%) patients in a study comparing iron sucrose versus oral iron therapy, no serious AEs were associated with iron sucrose [51]. Iron sucrose is also well tolerated in pediatric patients (Table 8) [123, 126]. For example, in a study of 38 children receiving iron sucrose, only one serious AE (anaphylaxis) was reported, and that occurred in a patient who had received more than the recommended dose [86].
On the basis of safety data obtained over many years and the wealth of published information on iron sucrose, it is clear that IV iron treatment is highly beneficial to a wide range of patients. The European Medicines Agency (EMA) assessed the use of IV iron-containing medicinal products and concluded that the benefits of these medicines outweigh the risks where oral iron therapy is poorly tolerated or insufficient [151].
Experience with Other Iron Sucrose Similars/Regulatory Update
The European Union categorizes follow-on products as generics (synthetic molecules) or biosimilars (from organic sources) that demonstrate equal therapeutic equivalence despite having a different mode of action than their reference product [152, 153]. During the last few decades, several follow-on iron sucrose products (iron sucrose similars) were approved as generics in the European market [154]. A growing body of clinical [155–159] and non-clinical [156, 160] evidence has nevertheless challenged the perception that originator iron sucrose and iron sucrose similars are interchangeable [152, 161].
Venofer contains a colloidal solution of nanoparticles consisting of a polynuclear Fe(III) oxyhydroxide/oxide core stabilized by an iron sucrose shell. Unlike most pharmaceuticals, Venofer is not a small molecule but a non-biological complex drug (NBCD) and is part of the class of drugs called nanomedicines [162]. The stabilized iron(III) hydroxide–sucrose complex in Venofer is produced through a unique manufacturing process. Nanomedicines, being NBCDs, consist of a multitude of closely related structures for which the entire complex is the active pharmaceutical ingredient [163]. Their properties cannot be fully characterized by physicochemical analysis, and a well-controlled, robust manufacturing process is fundamental to reproducing the product; these properties make general similars particularly difficult to generate [164].
These complex nanomedicines have brought about a class of similars termed nanosimilars [164]. Given the complex nature of nanomedicines, regulations governing generics may be inadequate for nanosimilars. Nanosimilars present unique challenges in determining equivalence to originator products as a result of difficulties establishing the equivalence of active ingredients, physiochemical properties, and in vivo drug exposure [165]. As a consequence, without head-to-head clinical studies demonstrating therapeutic equivalence, substitution of nanomedicines, such as iron sucrose, is not recommended [161] as safety concerns outweigh potential cost benefits [155].
The current regulatory paradigm consists of initially demonstrating qualitative and quantitative formulation equivalence with the reference drug, followed by physiochemical equivalence (e.g., particle size/distribution) and finally equivalent systemic exposure [165, 166]. This becomes more challenging with increasing complexity of the molecule or agent (Fig. 1). Although both the US FDA and EMA use close/comparable approaches to approving generic small-molecule drugs, they differ in their approaches to approving nanosimilars and there are no consensus requirements [165]. The inadequacy of a “one size fits all” approach to approving nanosimilars is reflected in the observed clinical differences in original formulations versus similars when they have been approved via a generic approach [164]. Specific areas of concern include the stability of the colloidal suspension and direct interaction of nanoparticles with the innate immune system.
Fig. 1.
Challenges associated with complex drugs in terms of pharmaceutical equivalence and bioequivalence between originator products and follow-on similar products.
Figure adapted from Hussaarts et al. [180] (https://creativecommons.org/licenses/by-nc/4.0/)
In a group of 658 gynecological operative and postpartum women, there were numerically more AEs (p < 0.2) in patients receiving an iron sucrose similar compared with those receiving iron sucrose [155]. A sequential observational study assessed the impact of switching from iron sucrose to an iron sucrose similar, by comparing two periods of 27 weeks each in 75 stable hemodialysis patients also receiving an IV ESA. Patients received iron sucrose in the first period and an iron sucrose similar in the second. Mean Hb and mean TSAT values were decreased during the second period. The mean IV iron dose, as well as the mean ESA dose per patient per week, was lower in the first period, and the total mean anemia drug costs increased by 12% in the second period. This study showed that switching from original iron sucrose to an iron sucrose similar in a group of patients with CKD undergoing hemodialysis led to destabilization of a well-controlled population and counterintuitively resulted in increased total drug costs [157]. In cases where patients with hemodialysis-dependent CKD had their iron sucrose similar replaced with the original iron sucrose, the requirements for IV iron dropped by a third, ESA doses were reduced, and TSAT and ferritin levels rose [155, 157, 159]. Interchanging or substituting an original nanomedicine, therefore, is strongly discouraged until therapeutic and safety equivalence have been demonstrated [161]. This was further stressed by a recent approval, where the UK Medicines & Healthcare products Regulatory Agency (MHRA) granted marketing authorization to an iron sucrose similar, not as a generic but as a hybrid medicine, clearly stating that it is not the same, but only similar to the reference listed drug [167].
Cost-Effectiveness of Iron Sucrose
Considerable cost savings to healthcare providers can be made by using IV iron treatment through its ability to reduce ESA dose [40, 117, 168–171] as well as reducing the need for RBC transfusions [40, 113, 118, 121, 172].
Despite iron sucrose similars being designed to reduce costs [173], these formulations are not necessarily cost-effective. In a sequential observational study, switching from iron sucrose to an iron sucrose similar led to an increase in total anemia drug costs [157, 173]. Additionally, in a recent cost-minimization analysis in hemodialysis patients, iron sucrose and iron sucrose similars were found to have comparable efficacy; however, using an iron sucrose similar was more expensive in 67% of iterations [171]. Although lower costs were associated with iron sucrose similars, this was offset by the requirement for higher ESA doses to obtain equivalent ferritin and TSAT levels [171].
Conclusions
Iron therapy through the use of iron sucrose produces many benefits, as summarized here and elsewhere [174]. Iron sucrose is able to correct iron deficiency, in addition to promoting erythropoiesis and subsequently reducing the required doses of ESAs. Not only is iron sucrose effective, but it is also well tolerated and rapidly increases bioavailable iron supplies. This is important for individuals who are unable to tolerate oral iron therapy, who are non-compliant with oral treatment, or in whom oral preparations are not effective. The efficacy and tolerability of iron sucrose are beneficial across a broad range of conditions causing or associated with iron deficiency/iron-deficiency anemia. Generic substitution of iron sucrose similar for iron sucrose should not be assumed to provide therapeutic equivalence, as the complex physicochemical properties of the original agent are extremely difficult to duplicate and studies have not been able to conclusively demonstrate that iron sucrose similars have safety and efficacy equivalent to that of iron sucrose.
Expert Opinion
The administration of iron via IV iron sucrose is beneficial in comparison with oral therapy for numerous reasons. Iron sucrose has demonstrated its ability to increase Hb levels with or without concomitant ESA therapy and improves both ferritin levels and TSAT. Administering iron sucrose via the IV route overcomes low intestinal absorption and reduced iron release that can hinder the performance of oral treatment. Overall, a hematological response is achieved more rapidly and consistently with iron sucrose than with oral iron administration, which, when considered along with reductions in ESA doses and the reduction in additional drugs to manage anemia in patients, can help to ensure that the use of iron sucrose is cost-effective. In contrast to earlier days, the EMA does not require a test dose when administering iron sucrose; however, there is a requirement for staff to be trained in cardiopulmonary resuscitation in case of anaphylaxis.
IV iron use should be considered in patients with functional iron deficiency and impaired iron absorption due to chronic inflammatory conditions, as well as in patients with time-critical iron deficiency/iron-deficiency anemia. Iron stores should be replenished before the use of ESA therapy. IV iron is first-line treatment for iron-deficiency anemia in patients with CKD undergoing hemodialysis; it is an option for patients with non-dialysis CKD, who often have functional iron deficiency. IV iron is recommended as first-line treatment in patients with symptomatic heart failure with reduced ejection fraction and iron deficiency. In patients with IBD and iron-deficiency anemia, IV iron is considered as first-line treatment in patients with clinically active disease, in cases with previous intolerance to oral iron, and in the presence of severe anemia (Hb below 10 g/dL). IV iron and ESAs should be used accordingly in order to correct pre- and postoperative iron deficiency anemia. IV iron is an option for treating iron deficiency/iron-deficiency anemia during the second or third trimester of pregnancy, and in women with iron-deficiency anemia due to heavy menstrual bleeding. Patients receiving ongoing chemotherapy who present with anemia and absolute iron deficiency should be offered IV iron treatment.
Iron sucrose has been studied extensively in a wide range of patients over many decades and has favorable tolerability compared with alternative IV iron products, such as ferric gluconate and iron dextran. Indeed, reassuring clinical data continue to be gained on iron sucrose, notably from the recently published PIVOTAL study in CKD comparing the efficacy and safety of high- versus low-dose iron sucrose.
Moving forward, there is a need for improved standardization of iron sucrose nanosimilar regulation that necessitates evidence of bioequivalence before substituting with, or switching to, an iron sucrose similar can be recommended.
Acknowledgements
Funding
Funding for the medical writing support, open access fee and rapid service fee for this article was provided by Vifor Pharma. In accordance with Good Publication Practice guidelines (https://www.ismpp.org/gpp3), authors did not receive any payment or compensation for developing the manuscript.
Medical Writing, Editorial, and Other Assistance
Medical writing support (including development of a draft outline and subsequent drafts in consultation with the authors, collating author comments, copyediting, fact checking, and referencing) was provided by Ryan Woodrow at Aspire Scientific (Bollington, UK).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Iain C. Macdougall has received consultancy fees, speaker fees, and unrestricted research funding from Vifor Pharma. Josep Comin-Colet has received speaker fees, consultancy honoraria, and an unrestricted research grant from Vifor Pharma. Christian Breymann is a medical consultant for Vifor International in the field of iron therapy in obstetrics and gynecology, and has participated in scientific sessions and meetings organized by Vifor International. Donat R. Spahn’s academic department is receiving some grant support from Vifor SA. Dr. Spahn is co-chair of the ABC-Trauma Faculty, sponsored by unrestricted educational grants from Novo Nordisk Health Care, CSL Behring, LFB Biomédicaments, and Octapharma. Dr. Spahn has received honoraria/travel support for consulting or lecturing from Baxter, Bayer, B. Braun Melsungen, Boehringer Ingelheim, Bristol-Myers Squibb, CSL Behring, Celgene, Curacyte, Daiichi Sankyo, GlaxoSmithKline, Haemonetics, Instrumentation Laboratory, LFB Biomédicaments, Merck Sharp & Dohme, Octapharma, Organon, PAION Deutschland, Pharmacosmos, Photonics Healthcare, Pierre Fabre Pharma, Roche, Sarstedt, Schering-Plough, Tem International, Verum Diagnostica, Vifor, and Zuellig Pharma. Ioannis E. Koutroubakis has served as an advisory board member for AbbVie, Astellas, Genesis, Janssen, MSD, Pharmacosmos, Pfizer, Shire, and Takeda; as a speaker for AbbVie, Astellas, Genesis, Janssen, MSD, and Takeda; and has received research support from AbbVie and Ferring.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
All data generated or analyzed during this study are included in this published article.
Footnotes
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12030552.
References
- 1.Evstatiev R, Gasche C. Iron sensing and signalling. Gut. 2012;61:933–952. doi: 10.1136/gut.2010.214312. [DOI] [PubMed] [Google Scholar]
- 2.Akpinar H, Cetiner M, Keshav S, Ormeci N, Toruner M. Diagnosis and treatment of iron deficiency anemia in patients with inflammatory bowel disease and gastrointestinal bleeding: iron deficiency anemia working group consensus report. Turk J Gastroenterol. 2017;28:81–87. doi: 10.5152/tjg.2017.17593. [DOI] [PubMed] [Google Scholar]
- 3.Cappellini MD, Comin-Colet J, de Francisco A, et al. Iron deficiency across chronic inflammatory conditions: international expert opinion on definition, diagnosis, and management. Am J Hematol. 2017;92:1068–1078. doi: 10.1002/ajh.24820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Franceschi L, Iolascon A, Taher A, Cappellini MD. Clinical management of iron deficiency anemia in adults: systemic review on advances in diagnosis and treatment. Eur J Intern Med. 2017;42:16–23. doi: 10.1016/j.ejim.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 5.Kassebaum NJ, Collaborators GBDA. The global burden of anemia. Hematol Oncol Clin N Am. 2016;30:247–308. doi: 10.1016/j.hoc.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Lam CSP, Doehner W, Comin-Colet J, Group IC. Iron deficiency in chronic heart failure: case-based practical guidance. ESC Heart Fail. 2018;5:764–771. doi: 10.1002/ehf2.12333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madeddu C, Gramignano G, Astara G, et al. Pathogenesis and treatment options of cancer related anemia: perspective for a targeted mechanism-based approach. Front Physiol. 2018;9:1294. doi: 10.3389/fphys.2018.01294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mikhail A, Brown C, Williams JA, et al. Renal association clinical practice guideline on anaemia of chronic kidney disease. BMC Nephrol. 2017;18:345. doi: 10.1186/s12882-017-0688-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peyrin-Biroulet L, Williet N, Cacoub P. Guidelines on the diagnosis and treatment of iron deficiency across indications: a systematic review. Am J Clin Nutr. 2015;102:1585–1594. doi: 10.3945/ajcn.114.103366. [DOI] [PubMed] [Google Scholar]
- 10.Sun D, McLeod A, Gandhi S, Malinowski AK, Shehata N. Anemia in pregnancy: a pragmatic approach. Obstet Gynecol Surv. 2017;72:730–737. doi: 10.1097/OGX.0000000000000510. [DOI] [PubMed] [Google Scholar]
- 11.Peuranpaa P, Heliovaara-Peippo S, Fraser I, Paavonen J, Hurskainen R. Effects of anemia and iron deficiency on quality of life in women with heavy menstrual bleeding. Acta Obstet Gynecol Scand. 2014;93:654–660. doi: 10.1111/aogs.12394. [DOI] [PubMed] [Google Scholar]
- 12.Wasada I, Eguchi H, Kurita M, et al. Anemia affects the quality of life of Japanese cancer patients. Tokai J Exp Clin Med. 2013;38:7–11. [PubMed] [Google Scholar]
- 13.Cella D. The effects of anemia and anemia treatment on the quality of life of people with cancer. Oncology (Williston Park) 2002;16:125–132. [PubMed] [Google Scholar]
- 14.Enjuanes C, Klip IT, Bruguera J, et al. Iron deficiency and health-related quality of life in chronic heart failure: results from a multicenter European study. Int J Cardiol. 2014;174:268–275. doi: 10.1016/j.ijcard.2014.03.169. [DOI] [PubMed] [Google Scholar]
- 15.Kanuri G, Sawhney R, Varghese J, Britto M, Shet A. Iron deficiency anemia coexists with cancer related anemia and adversely impacts quality of life. PLoS One. 2016;11:e0163817. doi: 10.1371/journal.pone.0163817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leaf DE, Goldfarb DS. Interpretation and review of health-related quality of life data in CKD patients receiving treatment for anemia. Kidney Int. 2009;75:15–24. doi: 10.1038/ki.2008.414. [DOI] [PubMed] [Google Scholar]
- 17.Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol. 2002;39:1780–1786. doi: 10.1016/s0735-1097(02)01854-5. [DOI] [PubMed] [Google Scholar]
- 18.Jurkovitz CT, Abramson JL, Vaccarino LV, Weintraub WS, McClellan WM. Association of high serum creatinine and anemia increases the risk of coronary events: results from the prospective community-based atherosclerosis risk in communities (ARIC) study. J Am Soc Nephrol. 2003;14:2919–2925. doi: 10.1097/01.asn.0000092138.65211.71. [DOI] [PubMed] [Google Scholar]
- 19.Abramson JL, Jurkovitz CT, Vaccarino V, Weintraub WS, McClellan W. Chronic kidney disease, anemia, and incident stroke in a middle-aged, community-based population: the ARIC Study. Kidney Int. 2003;64:610–615. doi: 10.1046/j.1523-1755.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 20.Kovesdy CP, Trivedi BK, Kalantar-Zadeh K, Anderson JE. Association of anemia with outcomes in men with moderate and severe chronic kidney disease. Kidney Int. 2006;69:560–564. doi: 10.1038/sj.ki.5000105. [DOI] [PubMed] [Google Scholar]
- 21.Macdougall IC, Canaud B, de Francisco AL, et al. Beyond the cardiorenal anaemia syndrome: recognizing the role of iron deficiency. Eur J Heart Fail. 2012;14:882–886. doi: 10.1093/eurjhf/hfs056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jankowska EA, Rozentryt P, Witkowska A, et al. Iron deficiency: an ominous sign in patients with systolic chronic heart failure. Eur Heart J. 2010;31:1872–1880. doi: 10.1093/eurheartj/ehq158. [DOI] [PubMed] [Google Scholar]
- 23.Jankowska EA, Malyszko J, Ardehali H, et al. Iron status in patients with chronic heart failure. Eur Heart J. 2013;34:827–834. doi: 10.1093/eurheartj/ehs377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klip IT, Comin-Colet J, Voors AA, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J. 2013;165(575–82):e3. doi: 10.1016/j.ahj.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 25.Rossler J, Schoenrath F, Seifert B, et al. Iron deficiency is associated with higher mortality in patients undergoing cardiac surgery: a prospective study. Br J Anaesth. 2020;124:25–34. doi: 10.1016/j.bja.2019.09.016. [DOI] [PubMed] [Google Scholar]
- 26.Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, Pearse RM. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015;102:1314–1324. doi: 10.1002/bjs.9861. [DOI] [PubMed] [Google Scholar]
- 27.Munoz M, Laso-Morales MJ, Gomez-Ramirez S, Cadellas M, Nunez-Matas MJ, Garcia-Erce JA. Pre-operative haemoglobin levels and iron status in a large multicentre cohort of patients undergoing major elective surgery. Anaesthesia. 2017;72:826–834. doi: 10.1111/anae.13840. [DOI] [PubMed] [Google Scholar]
- 28.Smith RE., Jr The clinical and economic burden of anemia. Am J Manag Care. 2010;16:S59–66. [PubMed] [Google Scholar]
- 29.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Hematopoietic growth factors v 2.2019. March 27, 2019. https://www.nccn.org/professionals/physician_gls/pdf/growthfactors.pdf. Accessed 30 Aug 2019.
- 30.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 31.Goodnough LT, Maniatis A, Earnshaw P, et al. Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: NATA guidelines. Br J Anaesth. 2011;106:13–22. doi: 10.1093/bja/aeq361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shander A, Javidroozi M, Perelman S, Puzio T, Lobel G. From bloodless surgery to patient blood management. Mt Sinai J Med. 2012;79:56–65. doi: 10.1002/msj.21290. [DOI] [PubMed] [Google Scholar]
- 33.Kidney Disease: Improving Global Outcomes (KDIGO) Anemia Work Group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int Suppl. 2012;2:279–335.
- 34.National Institute for Health and Care Excellence. Chronic kidney disease: managing anaemia. 2015. https://www.nice.org.uk/guidance/ng8. Accessed 10 Sep 2019. [PubMed]
- 35.Munoz M, Acheson AG, Auerbach M, et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia. 2017;72:233–247. doi: 10.1111/anae.13773. [DOI] [PubMed] [Google Scholar]
- 36.Macdougall IC, Bock AH, Carrera F, et al. FIND-CKD: a randomized trial of intravenous ferric carboxymaltose versus oral iron in patients with chronic kidney disease and iron deficiency anaemia. Nephrol Dial Transplant. 2014;29:2075–2084. doi: 10.1093/ndt/gfu201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alleyne M, Horne MK, Miller JL. Individualized treatment for iron-deficiency anemia in adults. Am J Med. 2008;121:943–948. doi: 10.1016/j.amjmed.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geisser P, Burckhardt S. The pharmacokinetics and pharmacodynamics of iron preparations. Pharmaceutics. 2011;3:12–33. doi: 10.3390/pharmaceutics3010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vifor Pharma. Half-year report. 2019. https://www.viforpharma.com/~/media/Files/V/Vifor-Pharma/documents/half-year-report-2019/vifor-pharma-hy-report-full-version-eng.pdf. Accessed 15 Jan 2020.
- 40.Macdougall IC, White C, Anker SD, et al. Intravenous iron in patients undergoing maintenance hemodialysis. N Engl J Med. 2019;380:447–458. doi: 10.1056/NEJMoa1810742. [DOI] [PubMed] [Google Scholar]
- 41.Danielson BG, Salmonson T, Derendorf H, Geisser P. Pharmacokinetics of iron(III)-hydroxide sucrose complex after a single intravenous dose in healthy volunteers. Arzneimittelforschung. 1996;46:615–621. [PubMed] [Google Scholar]
- 42.Beshara S, Lundqvist H, Sundin J, et al. Pharmacokinetics and red cell utilization of iron(III) hydroxide-sucrose complex in anaemic patients: a study using positron emission tomography. Br J Haematol. 1999;104:296–302. doi: 10.1046/j.1365-2141.1999.01179.x. [DOI] [PubMed] [Google Scholar]
- 43.Haddad A, Abbadi R, Marji A. Use of iron sucrose in dialysis patients sensitive to iron dextran. Saudi J Kidney Dis Transplant. 2009;20:208–211. [PubMed] [Google Scholar]
- 44.Mircescu G, Gârneaţǎ L, Cǎpuşǎ C, Ursea N. Intravenous iron supplementation for the treatment of anaemia in pre-dialyzed chronic renal failure patients. Nephrol Dial Transplant. 2006;21:120–124. doi: 10.1093/ndt/gfi087. [DOI] [PubMed] [Google Scholar]
- 45.Tagboto S, Cropper L, Mostafa S, Turner J, Bailey G, Pugh-Clarke K. Intravenous iron in chronic kidney disease: haemoglobin change shortly after treatment of patients neither on dialysis nor on erythropoietin. J Ren Care. 2008;34:112–115. doi: 10.1111/j.1755-6686.2008.00026.x. [DOI] [PubMed] [Google Scholar]
- 46.Deng Y, Wu J, Jia Q. Efficacy of intravenous iron sucrose in hemodialysis patients with restless legs syndrome (RLS): a randomized, placebo-controlled study. Med Sci Monit. 2017;23:1254–1260. doi: 10.12659/MSM.900520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wan L, Zhang D. Effect of frequency of intravenous iron administration on hemoglobin variability in maintenance hemodialysis patients. Int Urol Nephrol. 2018;50:1511–1518. doi: 10.1007/s11255-018-1916-8. [DOI] [PubMed] [Google Scholar]
- 48.Li H, Wang SX. Intravenous iron sucrose in Chinese hemodialysis patients with renal anemia. Blood Purif. 2008;26:151–156. doi: 10.1159/000113529. [DOI] [PubMed] [Google Scholar]
- 49.Van Wyck DB, Roppolo M, Martinez CO, Mazey RM, McMurray S. A randomized, controlled trial comparing IV iron sucrose to oral iron in anemic patients with nondialysis-dependent CKD. Kidney Int. 2005;68:2846–2856. doi: 10.1111/j.1523-1755.2005.00758.x. [DOI] [PubMed] [Google Scholar]
- 50.Bhandari S, Kalra PA, Kothari J, et al. A randomized, open-label trial of iron isomaltoside 1000 (Monofer®) compared with iron sucrose (Venofer®) as maintenance therapy in haemodialysis patients. Nephrol Dial Transplant. 2015;30:1577–1589. doi: 10.1093/ndt/gfv096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li H, Wang SX. Intravenous iron sucrose in peritoneal dialysis patients with renal anemia. Perit Dial Int. 2008;28:149–154. [PubMed] [Google Scholar]
- 52.Agarwal R, Kusek JW, Pappas MK. A randomized trial of intravenous and oral iron in chronic kidney disease. Kidney Int. 2015;88:905–914. doi: 10.1038/ki.2015.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Onken JE, Bregman DB, Harrington RA, et al. Ferric carboxymaltose in patients with iron-deficiency anemia and impaired renal function: the REPAIR-IDA trial. Nephrol Dial Transplant. 2014;29:833–842. doi: 10.1093/ndt/gft251. [DOI] [PubMed] [Google Scholar]
- 54.Mitsopoulos E, Lysitska A, Pateinakis P, et al. Efficacy and safety of a low monthly dose of intravenous iron sucrose in peritoneal dialysis patients. Int Urol Nephrol. 2020;52:387–92. [DOI] [PubMed]
- 55.Macdougall IC, Strauss WE, Dahl NV, Bernard K, Li Z. Ferumoxytol for iron deficiency anemia in patients undergoing hemodialysis. The FACT randomized controlled trial. Clin Nephrol. 2019;91:237–245. doi: 10.5414/CN109512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Macdougall IC, Bhandari S, White C, et al. Intravenous iron dosing and infection risk in patients on hemodialysis: a prespecified secondary analysis of the PIVOTAL trial. J Am Soc Nephrol. 2020 doi: 10.1681/ASN.2019090972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dwyer JP. We give too much intravenous iron. Semin Dial. 2016;29:309–311. doi: 10.1111/sdi.12509. [DOI] [PubMed] [Google Scholar]
- 58.Macdougall IC, Strauss WE, McLaughlin J, Li Z, Dellanna F, Hertel J. A randomized comparison of ferumoxytol and iron sucrose for treating iron deficiency anemia in patients with CKD. Clin J Am Soc Nephrol. 2014;9:705–712. doi: 10.2215/CJN.05320513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bhandari S, Thomsen LL. Single 1000 mg infusion of iron isomaltoside 1000 demonstrates a more rapid hemoglobin response and reduced risk of cardiovascular adverse events compared to multiple dose iron sucrose in patients with iron deficiency anemia and non-dialysis-dependent CKD. Nephrol Dial Transplant. 2019;34(Suppl_1):Abstract SaO035. [Google Scholar]
- 60.Silverberg DS, Wexler D, Blum M, et al. Effect of correction of anemia with erythropoietin and intravenous iron in resistant heart failure in octogenarians. Isr Med Assoc J. 2003;5:337–339. [PubMed] [Google Scholar]
- 61.Silverberg DS, Wexler D, Blum M, et al. The correction of anemia in severe resistant heart failure with erythropoietin and intravenous iron prevents the progression of both the heart and the renal failure and markedly reduces hospitalization. Clin Nephrol. 2002;58(Suppl 1):S37–45. [PubMed] [Google Scholar]
- 62.Martens P, Nijst P, Verbrugge FH, Smeets K, Dupont M, Mullens W. Impact of iron deficiency on exercise capacity and outcome in heart failure with reduced, mid-range and preserved ejection fraction. Acta Cardiol. 2018;73:115–123. doi: 10.1080/00015385.2017.1351239. [DOI] [PubMed] [Google Scholar]
- 63.Comin-Colet J, Enjuanes C, Gonzalez G, et al. Iron deficiency is a key determinant of health-related quality of life in patients with chronic heart failure regardless of anaemia status. Eur J Heart Fail. 2013;15:1164–1172. doi: 10.1093/eurjhf/hft083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Toblli JE, Lombrana A, Duarte P, Di Gennaro F. Intravenous iron reduces NT-pro-brain natriuretic peptide in anemic patients with chronic heart failure and renal insufficiency. J Am Coll Cardiol. 2007;50:1657–1665. doi: 10.1016/j.jacc.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 65.Bolger AP, Bartlett FR, Penston HS, et al. Intravenous iron alone for the treatment of anemia in patients with chronic heart failure. J Am Coll Cardiol. 2006;48:1225–1227. doi: 10.1016/j.jacc.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 66.Toblli JE, Di Gennaro F, Rivas C. Changes in echocardiographic parameters in iron deficiency patients with heart failure and chronic kidney disease treated with intravenous iron. Heart Lung Circ. 2015;24:686–695. doi: 10.1016/j.hlc.2014.12.161. [DOI] [PubMed] [Google Scholar]
- 67.Okonko DO, Grzeslo A, Witkowski T, et al. Effect of intravenous iron sucrose on exercise tolerance in anemic and nonanemic patients with symptomatic chronic heart failure and iron deficiency. FERRIC-HF: a randomized, controlled, observer-blinded trial. J Am Coll Cardiol. 2008;51:103–112. doi: 10.1016/j.jacc.2007.09.036. [DOI] [PubMed] [Google Scholar]
- 68.Usmanov RI, Zueva EB, Silverberg DS, Shaked M. Intravenous iron without erythropoietin for the treatment of iron deficiency anemia in patients with moderate to severe congestive heart failure and chronic kidney insufficiency. J Nephrol. 2008;21:236–242. [PubMed] [Google Scholar]
- 69.Silverberg DS, Wexler D, Blum M, et al. The effect of correction of anaemia in diabetics and non-diabetics with severe resistant congestive heart failure and chronic renal failure by subcutaneous erythropoietin and intravenous iron. Nephrol Dial Transplant. 2003;18:141–146. doi: 10.1093/ndt/18.1.141. [DOI] [PubMed] [Google Scholar]
- 70.Comin-Colet J, Ruiz S, Cladellas M, Rizzo M, Torres A, Bruguera J. A pilot evaluation of the long-term effect of combined therapy with intravenous iron sucrose and erythropoietin in elderly patients with advanced chronic heart failure and cardio-renal anemia syndrome: influence on neurohormonal activation and clinical outcomes. J Card Fail. 2009;15:727–735. doi: 10.1016/j.cardfail.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 71.Koutroubakis IE, Ramos-Rivers C, Regueiro M, et al. The influence of anti-tumor necrosis factor agents on hemoglobin levels of patients with inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1587–1593. doi: 10.1097/MIB.0000000000000417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lindgren S, Wikman O, Befrits R, et al. Intravenous iron sucrose is superior to oral iron sulphate for correcting anaemia and restoring iron stores in IBD patients: a randomized, controlled, evaluator-blind, multicentre study. Scand J Gastroenterol. 2009;44:838–845. doi: 10.1080/00365520902839667. [DOI] [PubMed] [Google Scholar]
- 73.Lee T, Clavel T, Smirnov K, et al. Oral versus intravenous iron replacement therapy distinctly alters the gut microbiota and metabolome in patients with IBD. Gut. 2017;66:863–871. doi: 10.1136/gutjnl-2015-309940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lichtenstein GR, Onken JE. Improved hemoglobin response with ferric carboxymaltose in patients with gastrointestinal-related iron-deficiency anemia versus oral iron. Dig Dis Sci. 2018;63:3009–3019. doi: 10.1007/s10620-018-5204-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gisbert JP, Bermejo F, Pajares R, et al. Oral and intravenous iron treatment in inflammatory bowel disease: hematological response and quality of life improvement. Inflamm Bowel Dis. 2009;15:1485–1491. doi: 10.1002/ibd.20925. [DOI] [PubMed] [Google Scholar]
- 76.Evstatiev R, Marteau P, Iqbal T, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease. Gastroenterology. 2011;141:846–853. doi: 10.1053/j.gastro.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 77.Iqbal S, Ekmekcioglu C. Maternal and neonatal outcomes related to iron supplementation or iron status: a summary of meta-analyses. J Matern Fetal Neonatal Med. 2019;32:1528–1540. doi: 10.1080/14767058.2017.1406915. [DOI] [PubMed] [Google Scholar]
- 78.Wiegersma AM, Dalman C, Lee BK, Karlsson H, Gardner RM. Association of prenatal maternal anemia with neurodevelopmental disorders. JAMA Psychiatry. 2019;76(12):1294–1304. doi: 10.1001/jamapsychiatry.2019.2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Al RA, Unlubilgin E, Kandemir O, Yalvac S, Cakir L, Haberal A. Intravenous versus oral iron for treatment of anemia in pregnancy: a randomized trial. Obstet Gynecol. 2005;106:1335–1340. doi: 10.1097/01.AOG.0000185260.82466.b4. [DOI] [PubMed] [Google Scholar]
- 80.Bayoumeu F, Subiran-Buisset C, Baka NE, Legagneur H, Monnier-Barbarino P, Laxenaire MC. Iron therapy in iron deficiency anemia in pregnancy: intravenous route versus oral route. Am J Obstet Gynecol. 2002;186:518–522. doi: 10.1067/mob.2002.121894. [DOI] [PubMed] [Google Scholar]
- 81.Bencaiova G, von Mandach U, Zimmermann R. Iron prophylaxis in pregnancy: intravenous route versus oral route. Eur J Obstet Gynecol Reprod Biol. 2009;144:135–139. doi: 10.1016/j.ejogrb.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 82.Tariq N, Ayub R, Khan WU, Ijaz S, Alam AY. Parenteral iron therapy in the treatment of iron deficiency anemia during pregnancy: a randomized controlled trial. J Coll Phys Surg Pak. 2015;25:193–197. [PubMed] [Google Scholar]
- 83.Hamm RF, Blauvelt C, Wang E, Srinivas S. Antepartum intravenous iron reduces peripartum blood transfusions [27B] Obstet Gynecol. 2018;131:S26–S27. [Google Scholar]
- 84.Hamm RF, Blauvelt C, Wang EY, Srinivas SK. Effectiveness of antepartum intravenous iron sucrose: dose timing and impact on outcomes. J Matern Fetal Neonatal Med. 2019;1–8. 10.1080/14767058.2019.1656189 . [DOI] [PubMed]
- 85.Breymann C, Visca E, Huch R, Huch A. Efficacy and safety of intravenously administered iron sucrose with and without adjuvant recombinant human erythropoietin for the treatment of resistant iron-deficiency anemia during pregnancy. Am J Obstet Gynecol. 2001;184:662–667. doi: 10.1067/mob.2001.111717. [DOI] [PubMed] [Google Scholar]
- 86.Krafft A, Bencaiova G, Breymann C. Selective use of recombinant human erythropoietin in pregnant patients with severe anemia or nonresponsive to iron sucrose alone. Fetal Diagn Ther. 2009;25:239–245. doi: 10.1159/000223441. [DOI] [PubMed] [Google Scholar]
- 87.Bencaiova G, Krafft A, Burkhardt T, Breymann C. Variable efficacy of recombinant human erythropoietin in anemic pregnant women with different forms of heterozygous hemoglobinopathy. Acta Haematol. 2006;116:259–265. doi: 10.1159/000095877. [DOI] [PubMed] [Google Scholar]
- 88.Bhandal N, Russell R. Intravenous versus oral iron therapy for postpartum anaemia. BJOG Int J Obstet Gynaecol. 2006;113:1248–1252. doi: 10.1111/j.1471-0528.2006.01062.x. [DOI] [PubMed] [Google Scholar]
- 89.Giannoulis C, Daniilidis A, Tantanasis T, Dinas K, Tzafettas J. Intravenous administration of iron sucrose for treating anemia in postpartum women. Hippokratia. 2009;13:38–40. [PMC free article] [PubMed] [Google Scholar]
- 90.Westad S, Backe B, Salvesen KÅ, et al. A 12-week randomised study comparing intravenous iron sucrose versus oral ferrous sulphate for treatment of postpartum anemia. Acta Obstet Gynecol Scand. 2008;87:916–923. doi: 10.1080/00016340802317802. [DOI] [PubMed] [Google Scholar]
- 91.Krafft A, Breymann C. Iron sucrose with and without recombinant erythropoietin for the treatment of severe postpartum anemia: a prospective, randomized, open-label study. J Obstet Gynaecol Res. 2011;37:119–124. doi: 10.1111/j.1447-0756.2010.01328.x. [DOI] [PubMed] [Google Scholar]
- 92.Wagstrom E, Akesson A, Van Rooijen M, Larson B, Bremme K. Erythropoietin and intravenous iron therapy in postpartum anaemia. Acta Obstet Gynecol Scand. 2007;86:957–962. doi: 10.1080/00016340701446157. [DOI] [PubMed] [Google Scholar]
- 93.Breymann C, Richter C, Huttner C, Huch R, Huch A. Effectiveness of recombinant erythropoietin and iron sucrose vs. iron therapy only, in patients with postpartum anaemia and blunted erythropoiesis. Eur J Clin Investig. 2000;30:154–161. doi: 10.1046/j.1365-2362.2000.00605.x. [DOI] [PubMed] [Google Scholar]
- 94.Krayenbuehl PA, Battegay E, Breymann C, Furrer J, Schulthess G. Intravenous iron for the treatment of fatigue in nonanemic, premenopausal women with low serum ferritin concentration. Blood. 2011;118:3222–3227. doi: 10.1182/blood-2011-04-346304. [DOI] [PubMed] [Google Scholar]
- 95.von Drygalski A, Adamson JW. Ironing out fatigue. Blood. 2011;118:3191–3192. doi: 10.1182/blood-2011-07-366120. [DOI] [PubMed] [Google Scholar]
- 96.Lee S, Ryu KJ, Lee ES, Lee KH, Lee JJ, Kim T. Comparative efficacy and safety of intravenous ferric carboxymaltose and iron sucrose for the treatment of preoperative anemia in patients with menorrhagia: an open-label, multicenter, randomized study. J Obstet Gynaecol Res. 2019;45:858–864. doi: 10.1111/jog.13893. [DOI] [PubMed] [Google Scholar]
- 97.Ikuta K, Hanashi H, Hirai K, et al. Comparison of efficacy and safety between intravenous ferric carboxymaltose and saccharated ferric oxide in Japanese patients with iron-deficiency anemia due to hypermenorrhea: a multi-center, randomized, open-label noninferiority study. Int J Hematol. 2019;109:41–49. doi: 10.1007/s12185-018-2501-8. [DOI] [PubMed] [Google Scholar]
- 98.Musallam KM, Tamim HM, Richards T, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet. 2011;378:1396–1407. doi: 10.1016/S0140-6736(11)61381-0. [DOI] [PubMed] [Google Scholar]
- 99.Klein AA, Collier TJ, Brar MS, et al. The incidence and importance of anaemia in patients undergoing cardiac surgery in the UK—the first Association of Cardiothoracic Anaesthetists national audit. Anaesthesia. 2016;71:627–635. doi: 10.1111/anae.13423. [DOI] [PubMed] [Google Scholar]
- 100.Baron DM, Hochrieser H, Posch M, et al. Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. Br J Anaesth. 2014;113:416–423. doi: 10.1093/bja/aeu098. [DOI] [PubMed] [Google Scholar]
- 101.Theusinger OM, Leyvraz PF, Schanz U, Seifert B, Spahn DR. Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology. 2007;107:923–927. doi: 10.1097/01.anes.0000291441.10704.82. [DOI] [PubMed] [Google Scholar]
- 102.Rohling RG, Zimmermann AP, Breymann C. Intravenous versus oral iron supplementation for preoperative stimulation of hemoglobin synthesis using recombinant human erythropoietin. J Hematother Stem Cell Res. 2000;9:497–500. doi: 10.1089/152581600419161. [DOI] [PubMed] [Google Scholar]
- 103.Olijhoek G, Megens JGN, Musto P, et al. Role of oral versus IV iron supplementation in the erythropoietic response to rHuEPO: a randomized, placebo-controlled trial. Transfusion. 2001;41:957–963. doi: 10.1046/j.1537-2995.2001.41070957.x. [DOI] [PubMed] [Google Scholar]
- 104.Xu HY, Dai ZH, Huang H. Clinical observation of iron sucrose combined with recombinant human erythropoietin in the treatment of anemia of hip fracture in elderly patients. Zhongguo Gu Shang. 2019;32:444–447. doi: 10.3969/j.issn.1003-0034.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 105.Kim YH, Chung HH, Kang SB, Kim SC, Kim YT. Safety and usefulness of intravenous iron sucrose in the management of preoperative anemia in patients with menorrhagia: a phase iv, open-label, prospective, randomized study. Acta Haematol. 2009;121:37–41. doi: 10.1159/000210062. [DOI] [PubMed] [Google Scholar]
- 106.Karkouti K, McCluskey SA, Ghannam M, Salpeter MJ, Quirt I, Yau TM. Intravenous iron and recombinant erythropoietin for the treatment of postoperative anemia. Can J Anesth. 2006;53:11–19. doi: 10.1007/BF03021522. [DOI] [PubMed] [Google Scholar]
- 107.Madi-Jebara SN, Sleilaty GS, Achouh PE, et al. Postoperative intravenous iron used alone or in combination with low-dose erythropoietin is not effective for correction of anemia after cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18:59–63. doi: 10.1053/j.jvca.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 108.Serrano-Trenas JA, Ugalde PF, Cabello LM, Chofles LC, Lázaro PS, Benítez PC. Role of perioperative intravenous iron therapy in elderly hip fracture patients: a single-center randomized controlled trial. Transfusion. 2011;51:97–104. doi: 10.1111/j.1537-2995.2010.02769.x. [DOI] [PubMed] [Google Scholar]
- 109.Garrido-Martín P, Nassar-Mansur MI, De La Llana-Ducrós R, et al. The effect of intravenous and oral iron administration on perioperative anaemia and transfusion requirements in patients undergoing elective cardiac surgery: a randomized clinical trial. Interact Cardiovasc Thorac Surg. 2012;15:1013–1018. doi: 10.1093/icvts/ivs344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shin HW, Park JJ, Kim HJ, You HS, Choi SU, Lee MJ. Efficacy of perioperative intravenous iron therapy for transfusion in orthopedic surgery: a systematic review and meta-analysis. PLoS One. 2019;14:e0215427. doi: 10.1371/journal.pone.0215427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xu H, Duan Y, Yuan X, Wu H, Sun H, Ji H. Intravenous iron versus placebo in the management of postoperative functional iron deficiency anemia in patients undergoing cardiac valvular surgery: a prospective, single-blinded, randomized controlled trial. J Cardiothorac Vasc Anesth. 2019;33:2941–2948. doi: 10.1053/j.jvca.2019.01.063. [DOI] [PubMed] [Google Scholar]
- 112.Muñoz M, Gõmez-Ramírez S, Cuenca J, et al. Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery: a pooled analysis of observational data from 2547 patients. Transfusion. 2014;54:289–299. doi: 10.1111/trf.12195. [DOI] [PubMed] [Google Scholar]
- 113.Pareja Sierra T, Bartolome Martin I, Rodriguez Solis J, et al. Results of an anaemia treatment protocol complementary to blood transfusion in elderly patients with hip fracture. Rev Esp Geriatr Gerontol. 2019;54:272–279. doi: 10.1016/j.regg.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 114.Montano-Pedroso JC, Bueno Garcia E, de Moraes M, Francescato Veiga D, Masako FL. Intravenous iron sucrose versus oral iron administration for the postoperative treatment of post-bariatric abdominoplasty anaemia: an open-label, randomised, superiority trial in Brazil. Lancet Haematol. 2018;5:e310–e320. doi: 10.1016/S2352-3026(18)30071-1. [DOI] [PubMed] [Google Scholar]
- 115.Birgegard G, Schneider K, Ulfberg J. High incidence of iron depletion and restless leg syndrome (RLS) in regular blood donors: intravenous iron sucrose substitution more effective than oral iron. Vox Sang. 2010;99:354–361. doi: 10.1111/j.1423-0410.2010.01368.x. [DOI] [PubMed] [Google Scholar]
- 116.Hedenus M, Birgegård G, Näsman P, et al. Addition of intravenous iron to epoetin beta increases hemoglobin response and decreases epoetin dose requirement in anemic patients with lymphoproliferative malignancies: a randomized multicenter study. Leukemia. 2007;21:627–632. doi: 10.1038/sj.leu.2404562. [DOI] [PubMed] [Google Scholar]
- 117.Hedenus M, Näsman P, Liwing J. Economic evaluation in Sweden of epoetin beta with intravenous iron supplementation in anaemic patients with lymphoproliferative malignancies not receiving chemotherapy. J Clin Pharm Ther. 2008;33:365–374. doi: 10.1111/j.1365-2710.2008.00924.x. [DOI] [PubMed] [Google Scholar]
- 118.Beguin Y, Maertens J, De Prijck B, et al. Darbepoetin-alfa and intravenous iron administration after autologous hematopoietic stem cell transplantation: a prospective multicenter randomized trial. Am J Hematol. 2013;88:990–996. doi: 10.1002/ajh.23552. [DOI] [PubMed] [Google Scholar]
- 119.Jaspers A, Baron F, Maertens J, et al. Long-term safety follow-up of a randomized trial of darbepoetin alpha and intravenous iron following autologous hematopoietic cell transplantation. Am J Hematol. 2015;90:E133–E134. doi: 10.1002/ajh.24013. [DOI] [PubMed] [Google Scholar]
- 120.Dangsuwan P, Manchana T. Blood transfusion reduction with intravenous iron in gynecologic cancer patients receiving chemotherapy. Gynecol Oncol. 2010;116:522–525. doi: 10.1016/j.ygyno.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 121.Kim YT, Kim SW, Yoon BS, et al. Effect of intravenously administered iron sucrose on the prevention of anemia in the cervical cancer patients treated with concurrent chemoradiotherapy. Gynecol Oncol. 2007;105:199–204. doi: 10.1016/j.ygyno.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 122.Steinmetz T, Tschechne B, Harlin O, et al. Clinical experience with ferric carboxymaltose in the treatment of cancer- and chemotherapy-associated anaemia. Ann Oncol. 2013;24:475–482. doi: 10.1093/annonc/mds338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Crary SE, Hall K, Buchanan GR. Intravenous iron sucrose for children with iron deficiency failing to respond to oral iron therapy. Pediatr Blood Cancer. 2011;56:615–619. doi: 10.1002/pbc.22930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Akarsu S, Taskin E, Yilmaz E, Yilmaz H, Kilic M, Aygun AD. Treatment of iron deficiency anemia with intravenous iron preparations. Acta Haematol. 2006;116:51–57. doi: 10.1159/000092348. [DOI] [PubMed] [Google Scholar]
- 125.Pinsk V, Levy J, Moser A, Yerushalmi B, Kapelushnik J. Efficacy and safety of intravenous iron sucrose therapy in a group of children with iron deficiency anemia. Israel Med Assoc J. 2008;10:335–338. [PubMed] [Google Scholar]
- 126.Danko I, Weidkamp M. Correction of iron deficiency anemia with intravenous iron sucrose in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2016;63:e107–e111. doi: 10.1097/MPG.0000000000001383. [DOI] [PubMed] [Google Scholar]
- 127.Venturieri MO, Komati JTS, Lopes LHC, Sdepanian VL. Treatment with Noripurum EV(®) is effective and safe in pediatric patients with inflammatory bowel disease and iron deficiency anemia. Scand J Gastroenterol. 2019;54:198–204. doi: 10.1080/00365521.2019.1570326. [DOI] [PubMed] [Google Scholar]
- 128.Danko I, Weidkamp M, Eickhoff JC. Improvement of health-related quality of life in children with inflammatory bowel disease receiving routine intravenous iron supplementation. J Pediatr Pharmacol Ther. 2019;24:517–527. doi: 10.5863/1551-6776-24.6.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sharma R, Stanek JR, Koch TL, Grooms L, O'Brien SH. Intravenous iron therapy in non-anemic iron-deficient menstruating adolescent females with fatigue. Am J Hematol. 2016;91:973–977. doi: 10.1002/ajh.24461. [DOI] [PubMed] [Google Scholar]
- 130.Perello MF, Coloma JL, Masoller N, Esteve J, Palacio M. Intravenous ferrous sucrose versus placebo in addition to oral iron therapy for the treatment of severe postpartum anaemia: a randomised controlled trial. BJOG. 2014;121:706–713. doi: 10.1111/1471-0528.12480. [DOI] [PubMed] [Google Scholar]
- 131.Winkelmayer WC, Goldstein BA, Mitani AA, et al. Safety of intravenous iron in hemodialysis: longer-term comparisons of iron sucrose versus sodium ferric gluconate complex. Am J Kidney Dis. 2017;69:771–779. doi: 10.1053/j.ajkd.2016.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Vifor Pharma UK Ltd. Venofer (iron sucrose) 20 mg iron/mL, solution for injection or concentrate for solution for infusion summary of product characteristics. 2019. https://www.medicines.org.uk/emc/product/5911/smpc. Accessed 30 Aug 2019.
- 133.Macdougall IC, Bircher AJ, Eckardt KU, et al. Iron management in chronic kidney disease: conclusions from a "Kidney Disease: Improving Global Outcomes" (KDIGO) Controversies Conference. Kidney Int. 2016;89:28–39. doi: 10.1016/j.kint.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 134.Wish JB, Aronoff GR, Bacon BR, et al. Positive iron balance in chronic kidney disease: how much is too much and how to tell? Am J Nephrol. 2018;47:72–83. doi: 10.1159/000486968. [DOI] [PubMed] [Google Scholar]
- 135.King Edward Memorial Hospital. Clinical practice guideline. Iron therapy: intravenous. 2019. https://www.kemh.health.wa.gov.au/~/media/Files/Hospitals/WNHS/For%20health%20professionals/Clinical%20guidelines/OG/WNHS.OG.IronTherapyIV.pdf. Accessed 8 Mar 2020.
- 136.Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005;352:1011–1023. doi: 10.1056/NEJMra041809. [DOI] [PubMed] [Google Scholar]
- 137.Aronoff GR, Bennett WM, Blumenthal S, et al. Iron sucrose in hemodialysis patients: safety of replacement and maintenance regimens. Kidney Int. 2004;66:1193–1198. doi: 10.1111/j.1523-1755.2004.00872.x. [DOI] [PubMed] [Google Scholar]
- 138.Litton E, Xiao J, Ho KM. Safety and efficacy of intravenous iron therapy in reducing requirement for allogeneic blood transfusion: systematic review and meta-analysis of randomised clinical trials. BMJ. 2013;347:f4822. doi: 10.1136/bmj.f4822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bansal A, Sandhu G, Gupta I, et al. Effect of aggressively driven intravenous iron therapy on infectious complications in end-stage renal disease patients on maintenance hemodialysis. Am J Ther. 2014;21:250–253. doi: 10.1097/MJT.0b013e31825425bd. [DOI] [PubMed] [Google Scholar]
- 140.Roger SD, Gaillard CA, Bock AH, et al. Safety of intravenous ferric carboxymaltose versus oral iron in patients with nondialysis-dependent CKD: an analysis of the 1-year FIND-CKD trial. Nephrol Dial Transplant. 2017;32:1530–1539. doi: 10.1093/ndt/gfw264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Macdougall IC, Roger SD. New data on the safety of IV iron-but why the discrepancy with FIND-CKD? Kidney Int. 2015;88:1445–1446. doi: 10.1038/ki.2015.302. [DOI] [PubMed] [Google Scholar]
- 142.Bhandari S, Kalra PA, Coyne DW. Data confusion. Kidney Int. 2015;88:1445. doi: 10.1038/ki.2015.303. [DOI] [PubMed] [Google Scholar]
- 143.Shepshelovich D, Rozen-Zvi B, Avni T, Gafter U, Gafter-Gvili A. Intravenous versus oral iron supplementation for the treatment of anemia in CKD: an updated systematic review and meta-analysis. Am J Kidney Dis. 2016;68:677–690. doi: 10.1053/j.ajkd.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 144.Yen CL, Lin YS, Lu YA, et al. Intravenous iron supplementation does not increase infectious disease risk in hemodialysis patients: a nationwide cohort-based case-crossover study. BMC Nephrol. 2019;20:327. doi: 10.1186/s12882-019-1495-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bailie GR, Clark JA, Lane CE, Lane PL. Hypersensitivity reactions and deaths associated with intravenous iron preparations. Nephrol Dial Transplant. 2005;20:1443–1449. doi: 10.1093/ndt/gfh820. [DOI] [PubMed] [Google Scholar]
- 146.Bailie GR, Verhoef JJ. Differences in the reporting rates of serious allergic adverse events from intravenous iron by country and population. Clin Adv Hematol Oncol. 2012;10:101–108. [PubMed] [Google Scholar]
- 147.Yee J, Besarab A. Iron sucrose: the oldest iron therapy becomes new. Am J Kidney Dis. 2002;40:1111–1121. doi: 10.1053/ajkd.2002.36853. [DOI] [PubMed] [Google Scholar]
- 148.Nathell L, Gohlke A, Wohlfeil S. Reported severe hypersensitivity reactions after intravenous iron administration in the European Economic Area (EEA) before and after implementation of risk minimization measures. Drug Saf. 2020;43:35–43. doi: 10.1007/s40264-019-00868-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang C, Graham DJ, Kane RC, et al. Comparative risk of anaphylactic reactions associated with intravenous iron products. JAMA. 2015;314:2062–2068. doi: 10.1001/jama.2015.15572. [DOI] [PubMed] [Google Scholar]
- 150.Al-Momen AK, Al-Meshari A, Al-Nuaim L, et al. Intravenous iron sucrose complex in the treatment of iron deficiency anemia during pregnancy. Eur J Obstet Gynecol Reprod Biol. 1996;69:121–124. doi: 10.1016/0301-2115(95)02538-3. [DOI] [PubMed] [Google Scholar]
- 151.European Medicines Agency. Assessment report for: Iron containing intravenous (IV) medicinal products (EMA/549569/2013). 2013. https://www.ema.europa.eu/en/documents/referral/intravenous-iron-containing-medicinal-products-article-31-referral-assessment-report_en.pdf. Accessed 30 Aug 2019.
- 152.Borchard G, Flühmann B, Mühlebach S. Nanoparticle iron medicinal products—requirements for approval of intended copies of non-biological complex drugs (NBCD) and the importance of clinical comparative studies. Regul Toxicol Pharmacol. 2012;64:324–328. doi: 10.1016/j.yrtph.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 153.Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use. Off J Eur Communities. 2001;L311:67–128.
- 154.Klein K, Stolk P, De Bruin ML, Leufkens HGM, Crommelin DJA, De Vlieger JSB. The EU regulatory landscape of non-biological complex drugs (NBCDs) follow-on products: observations and recommendations. Eur J Pharm Sci. 2019;133:228–235. doi: 10.1016/j.ejps.2019.03.029. [DOI] [PubMed] [Google Scholar]
- 155.Lee ES, Park BR, Kim JS, Choi GY, Lee JJ, Lee IS. Comparison of adverse event profile of intravenous iron sucrose and iron sucrose similar in postpartum and gynecologic operative patients. Curr Med Res Opin. 2013;29:141–147. doi: 10.1185/03007995.2012.760444. [DOI] [PubMed] [Google Scholar]
- 156.Martin-Malo A, Merino A, Carracedo J, et al. Effects of intravenous iron on mononuclear cells during the haemodialysis session. Nephrol Dial Transplant. 2012;27:2465–2471. doi: 10.1093/ndt/gfr711. [DOI] [PubMed] [Google Scholar]
- 157.Rottembourg J, Kadri A, Leonard E, Dansaert A, Lafuma A. Do two intravenous iron sucrose preparations have the same efficacy? Nephrol Dial Transplant. 2011;26:3262–3267. doi: 10.1093/ndt/gfr024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Stein J, Dignass A, Chow KU. Clinical case reports raise doubts about the therapeutic equivalence of an iron sucrose similar preparation compared with iron sucrose originator. Curr Med Res Opin. 2012;28:241–243. doi: 10.1185/03007995.2011.651527. [DOI] [PubMed] [Google Scholar]
- 159.Aguera ML, Martin-Malo A, Alvarez-Lara MA, et al. Efficiency of original versus generic intravenous iron formulations in patients on haemodialysis. PLoS One. 2015;10:e0135967. doi: 10.1371/journal.pone.0135967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Toblli JE, Cao G, Oliveri L, Angerosa M. Comparison of oxidative stress and inflammation induced by different intravenous iron sucrose similar preparations in a rat model. Inflamm Allergy Drug Targets. 2012;11:66–78. doi: 10.2174/187152812798889358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Schellekens H, Stegemann S, Weinstein V, et al. How to regulate nonbiological complex drugs (NBCD) and their follow-on versions: points to consider. AAPS J. 2014;16:15–21. doi: 10.1208/s12248-013-9533-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ehmann F, Sakai-Kato K, Duncan R, et al. Next-generation nanomedicines and nanosimilars: EU regulators' initiatives relating to the development and evaluation of nanomedicines. Nanomedicine. 2013;8:849–856. doi: 10.2217/nnm.13.68. [DOI] [PubMed] [Google Scholar]
- 163.Martin-Malo A, Borchard G, Fluhmann B, Mori C, Silverberg D, Jankowska EA. Differences between intravenous iron products: focus on treatment of iron deficiency in chronic heart failure patients. ESC Heart Fail. 2019;6:241–253. doi: 10.1002/ehf2.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Astier A, Barton Pai A, Bissig M, et al. How to select a nanosimilar. Ann N Y Acad Sci. 2017;1407:50–62. doi: 10.1111/nyas.13382. [DOI] [PubMed] [Google Scholar]
- 165.Zheng N, Sun DD, Zou P, Jiang W. Scientific and regulatory considerations for generic complex drug products containing nanomaterials. AAPS J. 2017;19:619–631. doi: 10.1208/s12248-017-0044-1. [DOI] [PubMed] [Google Scholar]
- 166.European Medicines Agency. Reflection paper on the data requirements for intravenous iron-based nano-colloidal products developed with reference to an innovator medicinal product (EMA/CHMP/SWP/620008/2012). 2015. https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-data-requirements-intravenous-iron-based-nano-colloidal-products-developed_en.pdf. Accessed 14 Nov 2019.
- 167.Medicines & Healthcare products Regulatory Agency. Public Assessment Report Decentralised Procedure: Sucrofer 20 mg iron/ml, Solution of injection/infusion (iron sucrose) (Procedure No: UK/H/6369/001/DC; UK Licence No: PL 20568/0083). 2018. https://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con917038.pdf. Accessed 14 Nov 2019.
- 168.Macdougall IC, Chandler G, Elston O, Harchowal J. Beneficial effects of adopting an aggressive intravenous iron policy in a hemodialysis unit. Am J Kidney Dis. 1999;34:S40–S46. doi: 10.1053/AJKD034s00040. [DOI] [PubMed] [Google Scholar]
- 169.Szucs TD, Blank PR, Schwenkglenks M, Aapro M. Potential health economic impact of intravenous iron supplementation to erythropoiesis-stimulating agent treatment in patients with cancer- or chemotherapy-induced anemia. Oncology. 2011;81:45–49. doi: 10.1159/000330738. [DOI] [PubMed] [Google Scholar]
- 170.Lacueva-Moya J, Antolín-Carinena A, Santamaría C, Vicent-Bayarri C. Effect on anaemia of haemodialysis patients after the change from iron gluconate to iron sucrose. Dial Tras. 2005;26:19–26. [Google Scholar]
- 171.Pages A, Porteils C, Labadens I, et al. Cost-minimization analysis between intravenous iron sucrose and iron sucrose similar in hemodialysis patients. Expert Rev Pharmacoecon Outcomes Res. 2019;1–7. 10.1080/14737167.2019.1632193. [DOI] [PubMed]
- 172.Bastit L, Vandebroek A, Altintas S, et al. Randomized, multicenter, controlled trial comparing the efficacy and safety of darbepoetin alfa administered every 3 weeks with or without intravenous iron in patients with chemotherapy-induced anemia. J Clin Oncol. 2008;26:1611–1618. doi: 10.1200/JCO.2006.10.4620. [DOI] [PubMed] [Google Scholar]
- 173.Fluhmann B, Ntai I, Borchard G, Simoens S, Muhlebach S. Nanomedicines: the magic bullets reaching their target? Eur J Pharm Sci. 2019;128:73–80. doi: 10.1016/j.ejps.2018.11.019. [DOI] [PubMed] [Google Scholar]
- 174.Beguin Y, Jaspers A. Iron sucrose—characteristics, efficacy and regulatory aspects of an established treatment of iron deficiency and iron-deficiency anemia in a broad range of therapeutic areas. Expert Opin Pharmacother. 2014;15:2087–2103. doi: 10.1517/14656566.2014.953928. [DOI] [PubMed] [Google Scholar]
- 175.Muñoz M, Martín-Montañez E. Ferric carboxymaltose for the treatment of iron-deficiency anemia [corrected] Expert Opin Pharmacother. 2012;13:907–921. doi: 10.1517/14656566.2012.669373. [DOI] [PubMed] [Google Scholar]
- 176.Neiser S, Rentsch D, Dippon U, et al. Physico-chemical properties of the new generation IV iron preparations ferumoxytol, iron isomaltoside 1000 and ferric carboxymaltose. Biometals. 2015;28:615–635. doi: 10.1007/s10534-015-9845-9. [DOI] [PubMed] [Google Scholar]
- 177.AMAG Pharmaceuticals Inc. Ferahem (ferumoxytol) injection. US Prescribing Information. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022180s011s013lbl.pdf. Accessed 29 Jan 2020.
- 178.Beck-da-Silva L, Piardi D, Soder S, et al. IRON-HF study: a randomized trial to assess the effects of iron in heart failure patients with anemia. Int J Cardiol. 2013;168:3439–3442. doi: 10.1016/j.ijcard.2013.04.181. [DOI] [PubMed] [Google Scholar]
- 179.Braga M, Gianotti L, Vignali A, et al. Evaluation of recombinant human erythropoietin to facilitate autologous blood donation before surgery in anaemic patients with cancer of the gastrointestinal tract. Br J Surg. 1995;82:1637–1640. doi: 10.1002/bjs.1800821216. [DOI] [PubMed] [Google Scholar]
- 180.Hussaarts L, Muhlebach S, Shah VP, et al. Equivalence of complex drug products: advances in and challenges for current regulatory frameworks. Ann N Y Acad Sci. 2017;1407:39–49. doi: 10.1111/nyas.13347. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.