Abstract
Background
Syphilis is a sexually transmitted infection with an incidence of 14.9 cases per 100 000 persons in the USA in 2011. Untreated syphilis may remain quiescent for years but can also result in clinical sequelae, including neurosyphilis. End-stage renal disease (ESRD) patients may be at risk for syphilis due to a higher incidence of risk factors for the disease, including human immunodeficiency virus (HIV). Despite the presence of these risk factors, the incidence of syphilis in the ESRD population has not been reported. To address this issue, we investigated the incidence and risk factors for syphilis in the ESRD population using the United States Renal Data System (USRDS).
Methods
This study analyzed incident ESRD patients from 2004 to 2010. Based on International Classification of Diseases, Ninth Revision codes for syphilis, we determined the incidence and risk factors for syphilis following an inpatient diagnosis. Generalized linear modeling was used to examine the relative risk (RR) for the disease when controlling for demographic and other clinical risk factors.
Results
A total of 383 diagnoses of syphilis were identified after screening 759 066 patients. The 8-year incidence of any type of syphilis was 50.45 cases per 100 000 person-years. Other unspecified syphilis (29.77 cases per 100 000 person-years) and neurosyphilis (10.93 cases per 100 000 person-years) were the most common diagnoses. The greatest incidence was found on the East and West Coasts. Patients with the disease were younger and more likely to be black and non-Hispanic. In the final model, the adjusted RR for syphilis was significantly increased with HIV (7.61), hepatitis C (3.57), herpes simplex (2.06) and hepatitis B (1.75).
Conclusions
The incidence of syphilis is >3-fold greater in ESRD patients when compared with the general population and is associated with sexually transmitted viral infections. Neurosyphilis is a common occurrence and is treatable, suggesting that all assessments of confusion in dialysis patients should include screening for the disease.
Keywords: dialysis, neurosyphilis, risk factors, syphilis
INTRODUCTION
Syphilis is a sexually transmitted infection caused by Treponema pallidum. The incidence of new cases is increasing in the general US population, with 14.9 cases per 100 000 individuals in 2011 [1, 2]. Clinically the disease progresses from a painless chancre at the site of exposure to secondary syphilis characterized by mucocutaneous lesions and lymphadenopathy, followed by a latent phase. Untreated syphilis may remain quiescent for years but may also result in significant late clinical sequelae. Neurosyphilis can occur at any stage of infection and can cause serious clinical complications, including cranial nerve dysfunction, ophthalmic disturbances and meningitis [1].
Patients with end-stage renal disease (ESRD) may be at particular risk for syphilis due to the more frequent occurrence of known risk factors for the disease, including human immunodeficiency virus (HIV). Despite the presence of these comorbidities, the incidence of syphilis in the ESRD population has not been reported. It is important to appreciate the prevalence of syphilis in this group, because if detected, the disease is easily treatable. On this basis, this project investigated the incidence of syphilis and the occurrence of potential risk factors in the ESRD population using the United States Renal Data System (USRDS). From this data set, we assessed for a diagnosis of syphilis, calculated the incidence of infection, queried for the occurrence of comorbidities and mapped the geographic distribution of the disease.
MATERIALS AND METHODS
Study cohort
The USRDS is a deidentified database that includes physician/supplier Medicare claims and vital statistics on all ESRD patients in the USA [3]. Subjects included in the present analysis had incident dialysis start dates from 2004 to 2010 and were of 11–100 years of age. Those without hospital claims, missing or unknown age, sex, race or ethnicity were excluded.
Demographic information, access type and treatment modality at the initiation of dialysis were obtained from the USRDS patient information data set and/or the latest version of the form CMS-2728. For patients with the disease, the yearly incidence from 2004 to 2011 was calculated based on those who were diagnosed with syphilis in a specific year divided by the number of individuals at risk for developing syphilis in that year expressed per 100 000 patients. Due to the large number of individuals without syphilis, a 5% random sample of those without the diagnosis was used for analysis of risk factors. Exclusions included individuals who had a prevalent diagnosis of syphilis before starting dialysis.
Outcome variables
The primary outcome of interest was the first diagnosis of syphilis following the incident date of dialysis. Hospital claims data were screened for seven syphilis-associated conditions, including early symptomatic, early latent, cardiovascular, neurosyphilis, other late forms with symptoms, late latent and other unspecified syphilis diagnoses using International Classification of Diseases, Ninth Revision (ICD-9) diagnosis or Current Procedural Terminology (CPT) codes from hospital claims data. Neurosyphilis cases were defined by the presence of two parameters: the ICD-9 code for neurosyphilis (094.0–094.9) and the CPT code for lumbar puncture dated 90 days before or 30 days after the diagnosis. The geographic distribution of syphilis in this group was determined by mapping the states from the claims data of the syphilis cases.
Covariates
Clinical covariates were selected based on known risk factors for syphilis and included hepatitis B virus (HBV), hepatitis C virus (HCV), herpes simplex virus (HSV), HIV, gonococcal infection, chancroid, lymphogranuloma venereum, granuloma inguinale, Chlamydia, cervical cancer, pelvic inflammatory disease, epididymitis and urethritis. To be consistent with regard to time for accrual of risk factors for control patients, the end date for querying risk factors for control patients was set to the median time to a syphilis diagnosis from the start of dialysis among those with syphilis (604 days). The incidence of neurosyphilis among HIV-infected dialysis patients was queried, but there were insufficient numbers for analysis due to low case numbers.
Statistical analysis
The statistical analysis was performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and statistical significance was assessed at a level of 0.05. Descriptive statistics (frequencies and percentages or means and standard deviations) by syphilis status were determined. Chi-square tests (or Fisher’s exact tests if assumptions were violated) and t-tests were used to examine preliminary differences between those with syphilis and those without. To examine the relative risk (RR) of demographic and clinical risk factors for syphilis, a generalized linear model, assuming a Poisson distribution with log link, was used, controlling for the person-years each individual contributed as an offset parameter. Person-years were defined as the number of years from the start of dialysis to syphilis diagnosis or the last known date of follow-up. Each potential independent risk factor was first examined in simple bivariate models and the RR and corresponding 95% confidence interval (CI) were estimated. All variables were then entered into a comprehensive full model and a backward model-building strategy used to arrive at the final model. Variables that had the least significant P-value in the full model were eliminated one by one until the final model consisted of those variables that were statistically significant at the 0.05 significance level or were needed in the model using quasi-information criterion (QICu) model fit criteria. The QICu was examined after each nonsignificant variable was removed from the model. The final model consisted of all risk factors that were statistically significant or were needed in the model to improve model fit to the data. The adjusted RR (aRR) and corresponding 95% CI were estimated for each variable in the final model. Note that the aRR is interpreted as the RR for a given variable, adjusting for all other variables in the final model.
RESULTS
Incidence of syphilis
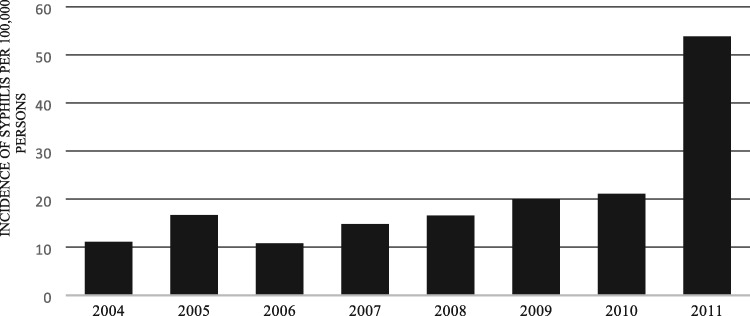
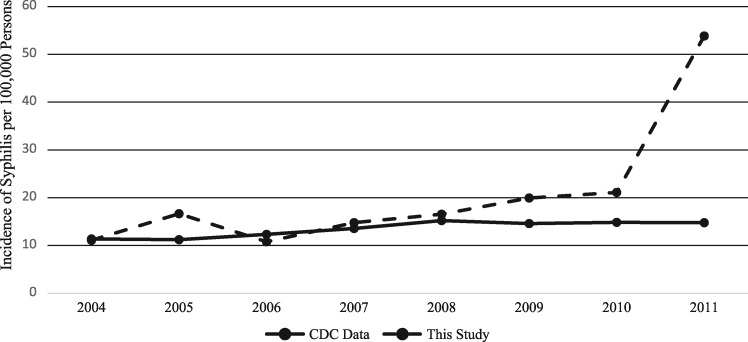
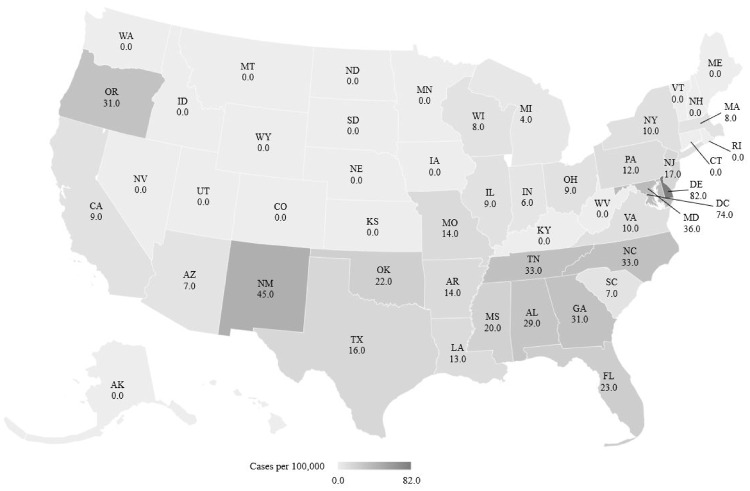
A total of 759 066 ESRD patients were eligible to be included in the analysis, from which 383 diagnoses of syphilis were identified (Table 1). In this analysis, the 8-year incidence of any type of syphilis was 50.45 cases per 100 000 person-years. The most common forms diagnosed (per 100 000 person-years) were other unspecified syphilis (29.77 cases) and neurosyphilis (10.93 cases). The incident rate of any syphilis diagnosis (per 100 000 patients) has increased every year from 2004 to 2011, with the biggest jump from 2010 to 2011 (Figure 1). The increasing incidence of syphilis in our population compared with the national incidence is steadily higher from 2007 to 2011 (Figure 2). Nationally, the incidence of ESRD patients with syphilis was highest in the northeast, southeast and West Coast (Figure 3). By area, the highest incidence per 100 000 patients was in Delaware (82), Washington, DC (74) and New Mexico (45).
Table 1.
Eight-year incidence of syphilis (2004–2011) by type in ESRD patients
| Variable | Counta | Incidence per 100 000 person-years |
|---|---|---|
| Any syphilis | 383 | 50.45 |
| Type of syphilis | ||
| Other unspecified syphilis | 226 | 29.77 |
| Neurosyphilis | 83 | 10.93 |
| Late syphilis, latent | 31 | 4.08 |
| Early syphilis, symptomatic | 16 | 2.11 |
| Cardiovascular syphilis | 12 | 1.58 |
| Other forms late syphilis with symptoms | <10 | 1.05 |
| Early syphilis, latent | <10 | 0.92 |
Number per 759 066 at-risk patients.
FIGURE 1.
Yearly incidence of syphilis from 2004 to 2011 per 100 000 persons.
FIGURE 2.
Yearly incidence of syphilis from 2004 to 2011 comparing national data from the Centers for Disease Control (CDC) with the data from this study.
FIGURE 3.
The geographic incidence of syphilis per 100 000 ESRD patients in 2011 for each state in the USA. States with a 0.0 incidence rate indicate insufficient data to calculate incidence.
Descriptive statistics
Those with syphilis were younger and more likely to be black and non-Hispanic than those without the diagnosis (Table 2). The disease was more common in patients initiating renal replacement therapy with hemodialysis, but there was no difference in access type at the initiation of dialysis.
Table 2.
Descriptive statistics by syphilis status
| Variable | Level | Syphilis | No syphilis | P-value |
|---|---|---|---|---|
| [N = 383 (1.3%)] | [N = 28 397 (98.7%)] | |||
| Age, mean (SD) | 58.7 (15.5) | 64.8 (15.1) | <0.0001 | |
| Sex, n (%) | Female | 166 (43.3) | 12 773 (45.0) | 0.5221 |
| Male | 217 (56.7) | 15 624 (550) | ||
| Race, n (%) | Black | 272 (71.0) | 7915 (27.9) | <0.0001 |
| Other | 14 (3.7) | 1311 (4.6) | ||
| White | 97 (25.3) | 19 171 (67.5) | ||
| Ethnicity, n (%) | Hispanic | 31 (8.1) | 3374 (11.9) | 0.0226 |
| Non-Hispanic | 352 (91.9) | 25 023 (88.1) | ||
| Dialysis modality, n (%) | HD | 364 (95.0) | 26 024 (91.6) | 0.0253 |
| PD | 17 (4.4) | 1721 (6.1) | ||
| Missing/unknown | <10 | 652 (2.3) | ||
| Access type, n (%) | AVF | 38 (9.9) | 2847 (10.0) | 0.5225 |
| Catheter | 233 (60.8) | 17 450 (61.5) | ||
| Graft | 15 (3.9) | 828 (2.9) | ||
| Other | <10 | 267 (0.9) | ||
| Missing/unknown | 96 (25.1) | 7005 (24.7) |
AVF: arteriovenous fistula; HD: hemodialysis; PD: peritoneal dialysis; SD: standard deviation.
For the control population (patients without the disease), the sample group was not statistically different from the remaining population with regard to sex, race, access type, dialysis modality or age.
Risk factors for syphilis diagnosis
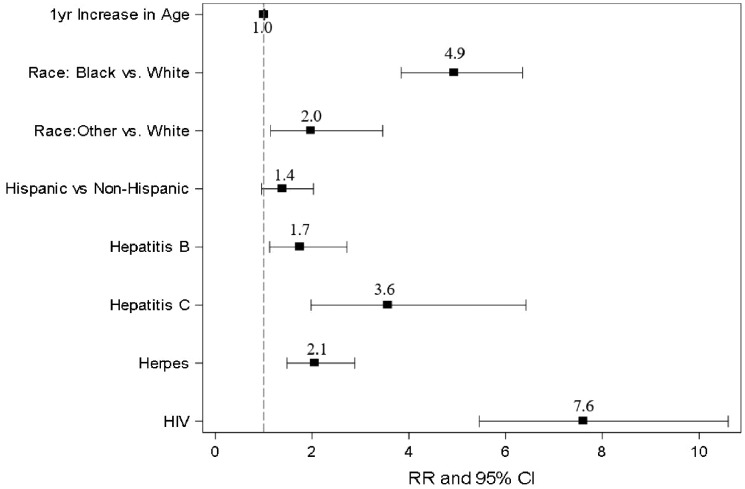
Table 3 indicates the results of the final model for the determination of risk factors for a diagnosis of syphilis. Significant risk factors associated with a syphilis diagnosis were increased age at the time of first dialysis, black and other races versus white and Hispanic versus non-Hispanic ethnicity. Clinical diagnoses with a significant increase in aRR included HIV, HCV, HSV and HBV and ranged from a high of 7.61 for HIV to a low of 1.75 for HBV (Figure 4). Among HIV-infected dialysis patients, 1.4% had neurosyphilis, whereas among non-HIV-infected dialysis patients, 0.3% had neurosyphilis. Unfortunately, due to the small case numbers, no further analysis was possible.
Table 3.
Final model for demographic and clinical risk factors for any diagnosis of syphilis
| Variable | aRR | 95% CI |
P-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age at first dialysis | 1.01 | 1.00 | 1.02 | 0.0129 |
| Black versus white | 4.94 | 3.84 | 6.35 | <0.0001 |
| Other versus white | 1.98 | 1.14 | 3.46 | |
| Hispanic versus non-Hispanic | 1.39 | 0.96 | 2.03 | 0.0819 |
| HIV | 7.61 | 5.46 | 10.60 | <0.0001 |
| HCV | 3.57 | 1.98 | 6.42 | <0.0001 |
| HSV | 2.06 | 1.48 | 2.88 | <0.0001 |
| HBV | 1.75 | 1.12 | 2.72 | 0.0135 |
FIGURE 4.
Forest plot of the aRRs and 95% CIs for risk factors for diagnosis of syphilis in ESRD patients.
DISCUSSION
This is the first study to investigate the incidence of syphilis and the occurrence of potential risk factors from a large ESRD population from the USA. This work showed an incidence of syphilis of 53.84 per 100 000 people in 2011 in dialysis patients, with neurosyphilis being the second most common diagnosis. Significant risk factors for a syphilis diagnosis in our ESRD cohort included younger patients, black race and non-Hispanic ethnicity and the presence of HIV, HCV, HSV or HBV. Taken together, our study demonstrates that ESRD patients coinfected with sexually transmitted viruses may be at high risk for contracting syphilis. Moreover, neurosyphilis is the second most common diagnosis in this group.
In the present study, the incidence of syphilis per 100 000 ESRD patients in 2011 was 53.84 compared with 14.9 for the general population [2]. It is not clear from our study why the incidence of the disease is so much higher in our patients; coding errors or flaws in our query could not be identified. It is possible that this change reflects an increasing trend in the general population as well; however, we do not have access to data beyond 2011. Others have shown that latent syphilis is prevalent in dialysis units in Taiwan [4], France [5] and Saudi Arabia [6], but these studies did not report incidence. To our knowledge, our work is the first to examine the incidence and risk factors for syphilis in a large ESRD cohort.
Our study showed that the incidence of syphilis diagnoses increased from 2004 to 2011 in ESRD patients, a pattern similar to the general population [2]. In addition, we show that the peak incidence of the disease in dialysis patients was found on the East and West Coasts, likely related to larger urban populations.
In the present study, younger age, nonwhite race and the presence of other sexually transmitted diseases were risk factors for syphilis, similar to the epidemiology of the general population. However, unlike the general population, our study indicates a very high incidence of neurosyphilis in ESRD patients.
The diagnosis of neurosyphilis should include a lumbar puncture with cerebral spinal fluid pleocytosis, elevated protein, lowered glucose, Venereal Disease Research Laboratory test or other indications of the disease in the central nervous system [2]. The USRDS does not contain specific laboratory results, thus the accuracy of the diagnosis of neurosyphilis from this data set must be inferred by the use of a combination of diagnostic and procedural codes. In this regard, we required the presence of the ICD-9 code for neurosyphilis (0.94) and the presence of a lumbar puncture 90 days before or 30 days after the neurosyphilis diagnosis date.
Mental status changes in dialysis patients are common [7] and the evaluation of mental status changes necessitates screening for syphilis. Alterations in mental status may be due to chronic pathologies, such as stroke and dementia, as well as more acute pathologies, such as metabolic and infectious causes [8]. Our data suggest that in confused dialysis patients, neurosyphilis should be considered, especially if there is serologic evidence of HIV, HCV, HBV or HSV. Making a diagnosis of neurosyphilis is important because, with proper antibiotic therapy, it is treatable [9].
The present study is based on a query of the USRDS data set and therefore has several limitations. All diagnoses are inferred from diagnostic and procedural billing codes submitted to Medicare or from form CMS-2728 and are not from actual medical documentation. Moreover, information about sexual or risk-taking behaviors for syphilis is not available in the USRDS data set. The patients reported in our study were from inpatient encounters in which syphilis diagnoses were coded. We could not account for patients in whom the diagnosis was made as an outpatient, those not identified in the inpatient setting or for whom there were coding errors. In this work, a diagnosis of syphilis could not be validated through confirmatory testing or direct measures, raising the possibility of bias in our results. However, the large size of the data set and our attempt at stringency for a neurosyphilis diagnosis may offset, at least in part, some of these limitations.
In summary, this is the first large-scale study of the incidence of syphilis in an ESRD population from the USA. The work showed that the incidence of the disease is >3-fold greater in dialysis patients when compared with the general population, is associated with sexually transmitted viral infections and that neurosyphilis is a common occurrence. We would suggest that neurosyphilis should be considered in the differential diagnosis of confusion in dialysis patients with appropriate risk factors and that screening for syphilis in this cohort is indicated.
ACKNOWLEDGEMENTS
Ethical approval was not required for this study. The data reported here were supplied by the USRDS. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US government. The contents do not represent the views of the Department of Veterans Affairs or the US government.
FUNDING
This work was supported by the Augusta University Medical Scholars Program (E.W.), a grant from Dialysis Clinic, Inc. (M.F.K. and N.S.N.) and the Translational Research Program of the Department of Medicine, Augusta University.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2014. Atlanta, GA: U.S. Department of Health and Human Services, 2015 [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2011. Atlanta, GA: US Department of Health and Human Services, 2012, 63–67 [Google Scholar]
- 3.United States Renal Data System. USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases, MD, 2013
- 4. Lee CT, Lam KK, Liao SC. et al. The significance of syphilis serology tests on long-term hemodialysis patients. Changgeng yi xue za zhi 1998; 21: 447–452 [PubMed] [Google Scholar]
- 5. Dahmani O, Belkhalfa S, Servonnat J. et al. Late latent syphilis in two hemodialysis units. Saudi J Kidney Dis Transpl 2013; 24: 124–127 [DOI] [PubMed] [Google Scholar]
- 6. Saxena AK, Panhotra BR, Naguib M. et al. Nosocomial transmission of syphilis during haemodialysis in a developing country. Scand J Infect Dis 2002; 34: 88–92 [DOI] [PubMed] [Google Scholar]
- 7. Sehgal AR, Grey SF, DeOreo PB. et al. Prevalence, recognition, and implications of mental impairment among hemodialysis patients. Am J Kidney Dis 1997; 30: 41–49 [DOI] [PubMed] [Google Scholar]
- 8. Arnold R, Issar T, Krishnan AV. et al. Neurological complications in chronic kidney disease. JRSM Cardiovasc Dis 2016; 5: 2048004016677687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Workowski KA. Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines. Clin Infect Dis 2015; 61(Suppl 8): S759–S762 [DOI] [PubMed] [Google Scholar]