Abstract
A subset of patients with coronavirus disease 2019 (COVID-19) and lung involvement pose a disposition challenge, particularly when hospital resources are constrained. Those not in respiratory failure are sent home, often with phone monitoring and/or respiratory rate and oxygen saturation monitoring. Hypoxemia may be a late presentation and is often preceded by abnormal lung findings on ultrasound. Early identification of pulmonary progression may preempt emergency hospitalization for respiratory decompensation and facilitate more timely admission. With the goal of safely isolating infected patients while providing advanced monitoring, we present a first report of patient self-performed lung ultrasound in the home with a hand-held device under the guidance of a physician using a novel teleguidance platform.
Key Words: coronavirus disease 2019, lung ultrasound, telemedicine
Abbreviations: EMS, emergency medical service; LUS, lung ultrasound; POCUS, point-of-care ultrasound
In late March of 2020, the Piedmont region, Italy, reported more than 7,000 diagnosed cases of coronavirus disease 2019 (COVID-19), with 3,000 of these patients discharged to home quarantine.1 , 2 The rapid increase in infected patients created an unmanageable situation for hospitals and emergency medical service (EMS) providers.3
Lung ultrasound (LUS) imaging for pneumonia and ARDS has been documented for years,4, 5, 6 and recent evidence suggests a possible role for LUS in the treatment of patients with COVID-19.7 , 8 LUS has been demonstrated in the home setting,9 , 10 but never by the patient him/herself. This novel report details the integration of LUS into the home treatment plan of a patient with COVID-19, using a novel teleguidance approach.
Case Report
In March of 2020, a 26-year-old female nurse was occupationally exposed to COVID-19 while working at the ED. The patient went into home isolation with no symptoms and monitored her vitals twice daily after receiving confirmation of a positive RT-qPCR (quantitative reverse transcription polymerase chain reaction) result. The nurse reported first symptoms (myalgia and headache) 5 days after the likely contact with a SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2)-infected patient. After an additional week, she began to experience shortness of breath on mild-moderate exertion (associated with mild desaturation), diarrhea, and localized left chest pain. On days 1 to 8, she performed daily unsupervised LUS examinations, using a small handheld ultrasound probe (Butterfly iQ; Butterfly Network Inc.) and uploaded the results to the cloud for review by an expert operator (E. P., with 12 years of experience). The patient had prior point-of-care ultrasound (POCUS) training, including a single-day didactic course and 40 supervised bedside evaluations for peripheral IV access and bladder examinations; thus she is a home user with POCUS experience who does not fully represent the complexity of self-scanning by a lay user.
Beginning on day 9, a teleguidance feature became available on the device that allowed real-time remote support by the expert operator, who could use two-way audio and video to guide the novice to obtain optimized views. The expert operator could adjust the ultrasound settings (preset, depth, gain) and capture cines. The subject obtained images under teleguidance supervision from days 9 to 16.
Daily LUS examinations were saved and scored for image quality by a second expert (M. S.) blinded to the acquisition and interpretation. The scoring convention used was as follows: 0, no lung visualized; 1, image poorly informative, pleural line partially visualized; 2, image interpretable, pleural line partially visualized but sufficient for evaluation; 3, image easily interpreted, pleural line well visualized. Images scored 0 or 1 were considered nondiagnostic. Image quality was compared between the self-guided and remote expert-guided approach (using the Kruskal-Wallis test).
Table 1 describes the number of zones imaged, the diagnostic quality, the daily sonographic findings, and oxygen saturation. Over time, bilateral B lines and small subpleural consolidations developed. Initially the patient had a few B lines, mainly in the lateral and posterior areas. Beginning on day 6, a subpleural consolidation developed in the left inferior region and was visible for the next 7 days. Bilateral lung sliding was present and no pleural effusions were found for the entire period. Overall, 114 images were acquired. The median quality score for unsupervised scans (n = 35) was significantly lower than for supervised teleguidance scans (n = 79) (2 vs 3, respectively; P < .001), but only three images were reviewed as nondiagnostic (2.6%). For the initial, unsupervised scans, cines were recorded for three zones (anterior, lateral, and posterior) per hemithorax. During teleguidance sessions, a 12-zone protocol was followed (superior and inferior, anterior, lateral, and posterior). The patient’s flexibility and dexterity were sufficient to reach the posterior region, albeit slightly more laterally and inferior than if performed by a health-care professional or caregiver. An example teleguidance session is shown in Figure 1 .
Table 1.
Daily Lung Ultrasound Reports Including the Number of Images, Image Quality, and Ultrasound Findingsa
| Day | No. of Lung Zones Imaged | % Diagnostic Quality | POCUS Findings |
Lowest Spo2 (Mild Exertion) | |
|---|---|---|---|---|---|
| Left | Right | ||||
| 1 | 7 | 100 |
Anterior: A few vertical artifacts; thin pleural line Lateral: A few nonconfluent B lines Posterior: A few nonconfluent lines |
Anterior: Multiple nonconfluent B lines (inferior) Lateral: A few nonconfluent B lines; single B line and some small vertical artifacts (inferior) Posterior: Multiple nonconfluent B lines |
N/A |
| 2 | 6 | 100 |
Anterior: A few small vertical artifacts Lateral: A few nonconfluent vertical artifacts (inferior) Posterior: Multiple vertical artifacts; rare or no B lines |
Anterior: A few vertical artifacts Lateral: Some nonconfluent B lines (inferior) Posterior: A few B lines (inferior) |
N/A |
| 3 | 7 | 86 |
Anterior: Some nonconfluent B lines Lateral: Some nonconfluent B lines Posterior: Some isolated B lines (left > right) |
Anterior: Some B lines, not confluent (inferior) Lateral: Isolated B lines (superior); diffuse B lines, not confluent (inferior) Posterior: Some isolated B lines (left > right) |
91-93 |
| 4 | 6 | 100 |
Anterior: Some small vertical artifacts Lateral: Some nonconfluent B lines Posterior: Some small vertical artifacts |
Anterior: Some vertical artifacts Lateral: A few nonconfluent B lines Posterior: A few nonconfluent B lines |
91-93 |
| 5 | 9 | 100 |
Anterior: A few vertical artifacts and a single B line in the inferior area Lateral: A few vertical artifacts Posterior: Some small vertical artifacts |
Anterior: Some vertical artifacts; a single B line between superior and inferior zones Lateral: Some B lines in inferior area Posterior: Some B lines |
91-93 |
| 6 | 9 | 100 |
Anterior: Normal Lateral: Some small vertical artifacts and two or three in the basal area Posterior: Some B lines with a likely subpleural consolidation |
Anterior: A single B line between superior and inferior areas and a few small vertical artifacts Lateral: Two or three B lines Posterior: Two or three B lines |
91-93 |
| 7 | 11 | 100 |
Anterior: Normal Lateral: Some vertical artifacts and two or three B lines in the inferior, lateral area Posterior: Some B lines with a likely subpleural consolidation |
Anterior: A single B line between superior and inferior anterior areas; a few small vertical artifacts Lateral: Two or three basal B lines Posterior: Two or three basal B lines |
N/A |
| 8 | 8 | 100 |
Anterior: A few vertical artifacts with irregular pleural line Lateral: Irregular and thickened pleural line with some B lines Posterior: Some B lines with a subpleural consolidation |
Anterior: A few small vertical artifacts Lateral: Two or three B lines between superior and inferior areas with a small subpleural consolidation Posterior: Two or three basal B lines |
N/A |
| 9 | 10 | 100 |
Anterior: A few vertical artifacts with irregular pleural line Lateral: Irregular and thickened pleural line with some B lines Posterior: Some B lines with a subpleural consolidation |
Anterior: A few vertical artifacts Lateral: Some B lines in the inferior area Posterior: Two or three basal B lines |
N/A |
| 10 | 7 | 100 |
Anterior: A few vertical artifacts Lateral: Some vertical artifacts with some B lines Posterior: Some B lines with a subpleural consolidation |
Anterior: A few vertical artifacts Lateral: Some vertical artifacts in the inferior area with an irregular pleural line Posterior: Some basal B lines |
91-93 |
| 11 | 11 | 100 |
Anterior: A few vertical artifacts Lateral: A few vertical artifacts Posterior: Some B lines in the basal zone with a subpleural consolidation |
Anterior: Some small vertical artifacts Lateral: Some small vertical artifacts Posterior: Two or three basal B lines |
N/A |
| 12 | 11 | 91 |
Anterior: A few vertical artifacts Lateral: Two or three B lines in the basal area Posterior: Two or three B lines in the basal area with a small subpleural consolidation |
Anterior: Some small vertical artifacts Lateral: A single B line Posterior: An irregular pleural line with a small subpleural consolidation in the inferior area |
91 |
| 13 | 12 | 92 |
Anterior: Irregular pleural line Lateral: Two B lines in the basal area Posterior: Two B lines in the basal area |
Anterior: Irregular pleural line with a few vertical artifacts Lateral: A few B lines Posterior: Vertical artifacts with a small subpleural consolidation in the inferior area |
93-94 |
| 14 | 12 | 100 |
Anterior: Irregular pleural line Lateral: Irregular pleural line with some B lines in the basal area Posterior: Some B lines in the basal area |
Anterior: Irregular pleural line with one B line in the superior area Lateral: Two or three nonconfluent B lines in the basal lateral area Posterior: Two B lines in the basal area |
93-94 |
| 15 | 12 | 100 |
Anterior: Irregular pleural line Lateral: Some vertical artifacts between superior and inferior anterior areas with a single B line Posterior: A few B lines in the basal area |
Anterior: Irregular pleural line Lateral: Some diffuse small vertical artifacts and a single B line in the basal area Posterior: A few B lines in the basal area |
93-94 |
| 16 | 12 | 100 |
Anterior: Irregular pleural line Lateral: Some vertical artifacts with two or three basal B lines Posterior: A few B lines in the basal area |
Anterior: Minimally irregular pleural line Lateral: One or two B lines in the basal area Posterior: One or two B lines in the basal area |
95 |
N/A = data not available; POCUS = point-of-care ultrasound; Spo2 = arterial oxygen saturation as determined by pulse oximetry.
The last day reported (day 16) corresponds to the day the subject was assessed in hospital.
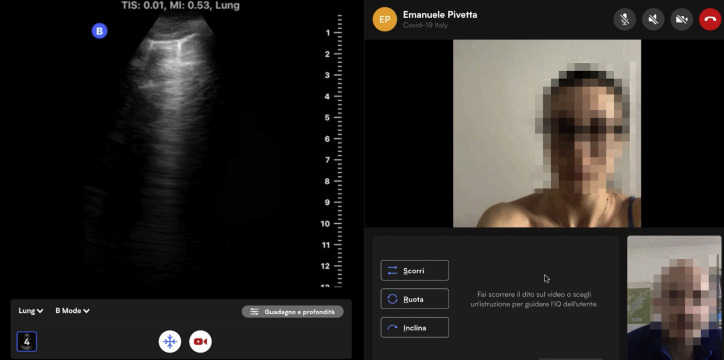
Figure 1.
The expert’s view of a teleguidance session with the lung image shown on the left and the two-way video features on the right. The expert can change modes, adjust depth and gain, and save clips. Directions can be given through augmented reality buttons and/or auditory feedback.
On the basis of the patient’s symptoms, a focused cardiac ultrasound was also performed because of the presence of bilateral chest pain, using parasternal short- and long-axis views. This examination excluded a pericardial effusion, dilatation of the right ventricle, and abnormal left ventricular contractility.
On day 16, during a telephone follow-up with the Hygiene and Public Health Service, the patient reported dyspnea on mild exertion. Per protocol, EMS brought her to the ED, where chest radiography, arterial blood gas analysis, and laboratory tests were performed. The laboratory test results were all normal and the chest radiograph was negative for pneumonia, which was different from the bilateral basal B lines found on POCUS the same day (Table 1). The patient was not admitted and was monitored at home until symptom resolution.
Discussion
We highlight three clinical observations within this case: first, daily LUS allowed the attending physician to correlate the reported symptoms of shortness of breath with ultrasonographic findings. Second, when the subject reported bilateral chest pain, an untrained patient was able to acquire adequate cardiac images to rule out severe changes. Third, despite a normal chest radiograph in the ED, lung involvement was still present as documented by the presence of B lines, suggesting that LUS could provide additional information that is not seen on chest radiography for patients with COVID-19. The most significant findings from this case are that teleguidance improved the image quality of the lung ultrasonography performed by a patient in her home by guiding the patient to follow a standard imaging protocol; decreased the already low nondiagnostic image rate even further; and increased the number of high-quality images for interpretation.
In conclusion, we present a new mechanism for monitoring patients with COVID-19 in the home, using a novel teleguidance system for LUS that can be used by the patient (or by EMS). Integrating LUS into home management could decrease the need for patients to be transported to a hospital or imaging center, avoiding unnecessary disease transmission through patient movement.11 Further work to investigate a larger implementation into common telehealth platforms and the ease of use by lay people and their caregivers is warranted.
Acknowledgments
Financial/nonfinancial disclosures: None declared.
Other contributions: CHEST worked with the authors to ensure that the Journal policies on patient consent to report information were met.
References
- 1.Lazzerini M., Putoto G. COVID-19 in Italy: momentous decisions and many uncertainties. Lancet Glob Health. 2020;8(5):e641–e642. doi: 10.1016/S2214-109X(20)30110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piedmont Regional Service for Epidemiology, Surveillance, Prevention and Infectious Diseases Control. Epidemia COVID-19. March 27, 2020. https://www.seremi.it/
- 3.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Volpicelli G., Elbarbary M., Blaivas M. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 5.Gargani L., Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014;12(1):25. doi: 10.1186/1476-7120-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soldati G., Smargiassi A., Inchingolo R. Lung ultrasonography may provide an indirect estimation of lung porosity and airspace geometry. Respiration. 2014;88(6):458–468. doi: 10.1159/000368086. [DOI] [PubMed] [Google Scholar]
- 7.Peng Q.Y., Wang X.T., Zhang L.N., Chinese Critical Care Ultrasound Study Group (CCUSG) Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020;46(5):849–850. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soldati G., Smargiassi A., Inchingolo Proposal for international standardization of the use of lung ultrasound for COVID-19 patients; a simple, quantitative, reproducible method. J Ultrasound Med. 2020;39(7):1413–1419. doi: 10.1002/jum.15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Namiki H., Kobayashi T. Lung ultrasound for initial diagnosis and subsequent monitoring of aspiration pneumonia in elderly in home medical care setting. Gerontol Geriatr Med. 2019;5 doi: 10.1177/2333721419858441. 2333721419858441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonnel A.R., Baston C.M., Wallace P., Panebianco N., Kinosian B. Using point-of-care ultrasound on home visits: the home-oriented ultrasound examination (HOUSE) J Am Geriatr Soc. 2019;67(12):2662–2663. doi: 10.1111/jgs.16188. [DOI] [PubMed] [Google Scholar]
- 11.Nacoti M., Ciocca A., Giupponi A. At the epicenter of the Covid-19 pandemic and humanitarian crises in Italy: changing perspectives on preparation and mitigation. NEJM Catal Innov Care Deliv. 2020;1(2) [Google Scholar]