Abstract
Background
This longitudinal study identified risk factors for frequency of hospitalization among patients with any medical condition who had previously visited one of six Quebec (Canada) emergency departments (ED) at least once for mental health (MH) conditions as the primary diagnosis.
Methods
Records of n = 11,367 patients were investigated using administrative databanks (2012–13/2014–15). Hospitalization rates in the 12 months after a first ED visit in 2014–15 were categorized as no hospitalizations (0 times), moderate hospitalizations (1–2 times), and frequent hospitalizations (3+ times). Based on the Andersen Behavioral Model, data on risk factors were gathered for the 2 years prior to the first visit in 2014–15, and were identified as predisposing, enabling or needs factors. They were tested using a hierarchical multinomial logistic regression according to the three groups of hospitalization rate.
Results
Enabling factors accounted for the largest percentage of total variance explained in the study model, followed by needs and predisposing factors. Co-occurring mental disorders (MD)/substance-related disorders (SRD), alcohol-related disorders, depressive disorders, frequency of consultations with outpatient psychiatrists, prior ED visits for any medical condition and number of physicians consulted in specialized care, were risk factors for both moderate and frequent hospitalizations. Schizophrenia spectrum and other psychotic disorders, bipolar disorders, and age (except 12–17 years) were risk factors for moderate hospitalizations, while higher numbers (4+) of overall interventions in local community health service centers were a risk factor for frequent hospitalizations only. Patients with personality disorders, drug-related disorders, suicidal behaviors, and those who visited a psychiatric ED integrated with a general ED in a separate site, or who visited a general ED without psychiatric services were also less likely to be hospitalized. Less urgent and non-urgent illness acuity prevented moderate hospitalizations only.
Conclusions
Patients with severe and complex health conditions, and higher numbers of both prior outpatient psychiatrist consultations and ED visits for medical conditions had more moderate and frequent hospitalizations as compared with non-hospitalized patients. Patients at risk for frequent hospitalizations were more vulnerable overall and had important biopsychosocial problems. Improved primary care and integrated outpatient services may prevent post-ED hospitalization.
Keywords: Hospitalization; mental disorders; substance related disorders; risk factors, Needs factors, Predisposing factors, Enabling factors, Medical conditions, Predictors, Service use
Introduction
Frequent use of inpatient treatment is a common occurrence among patients with mental disorders (MD) [1–3]. Most MD, including schizophrenia [4, 5] and mood disorders [6–8] as well as substance use disorders (SUD) [9, 10] involve a high risk of relapse which may explain frequent hospitalizations. Those with MD also experience high hospitalization rates for medical and surgical conditions [11] related to illnesses such as diabetes [12], heart problems and pneumonia [13, 14]. The frequent co-occurrence of MD with chronic physical illnesses [15–17] may affect access and challenge the capacity of primary care to provide adequate services [18], resulting in increased hospitalization rates [15–17].
Frequent hospitalizations account, in part, for the high costs of psychiatric treatment [19–21]. Understanding which risk factors predict frequency of patient hospitalizations among individuals with MD is important for improving care management and service organization. The Andersen Behavioral Model [22], one of the most widely used conceptual frameworks in studies of health service utilization, may serve to identify various risk factors for hospitalization. In this model, variables are categorized as needs, predisposing and enabling factors [22]. Needs factors include diagnoses and other clinical variables; predisposing factors refer to sociodemographic and economic status (e.g. age, sex), while enabling factors include variables with particular impact on healthcare use (e.g. access to care and continuous follow-up) [23].
Studies have examined risk factors for frequency of hospitalization in the general population [11, 24, 25]. The following needs factors were associated with high hospitalization rates: MD diagnoses [24], especially depressive symptoms [26] and personality disorders [27], co-occurring MD and physical illnesses [11], and co-occurring SUD and physical illnesses [25]. One study [24] found that older age (predisposing factors) and possession of health insurance (enabling factors) were linked to high hospitalization rates. However, other key factors which may influence hospitalization have been underexplored. These include enabling factors such as continuity of care, access to specialized ambulatory and primary care services and community treatment, and predisposing factors such as social deprivation. Moreover, no study to our knowledge has examined patient subgroups with MD or patients visiting ED for mental health (MH) conditions in terms of their frequency of hospitalization for medical conditions in a 12-month period. Examining risk factors of hospitalization for medical conditions in this patient cohort may capture the overall impact of this subpopulation on hospitalization rates, either for MH or physical health conditions. Reasons for inadequacy of care among these patients may be identified, allowing for further development of recommendations aimed at improving services.
Using the Andersen Model [22], this study assessed risk factors of hospitalization for any medical condition (no hospitalization (0 times), moderate hospitalizations (1–2 times), and frequent hospitalizations (3+ times)) in a 12 month-period after a first patient emergency department (ED) visit in 2014–15 for MH conditions as the primary diagnosis. Risk factors were gathered over a 2-year period prior to the first patient ED visit. Based on literature which identified key links between hospitalization rates and diagnoses, we hypothesized that frequent hospitalizations would be more strongly associated with needs factors, compared with enabling and predisposing factors.
Methods
Study population and design
This longitudinal study included 11,367 patients identified through clinical administrative databanks and followed over a three-year period (2012–13/2014–15). Participants were 12 years old or older and eligible for Quebec (Canada) healthcare insurance. They visited one of six Quebec ED at least once between April 1, 2014 and March 31, 2015 (index year) for MH conditions (including SUD and suicidal behaviors) as a primary diagnosis. The six selected ED operated in various local health networks, which represented three of the largest cities in Quebec. The Access to Information Commission of Quebec and the ethics committee of a MH university institute approved this study.
Data sources
Data for the study were collected from the Régie d’Assurance Maladie du Québec (RAMQ), the Quebec healthcare insurance databanks which contain medical administrative information including billing files for medical services provided by physicians. These files cover most outpatient medical activities as only 6% of physician billing occurs outside of the public system [28]. The RAMQ also integrates demographic and socioeconomic information, including material and social deprivation indices [29]. Other data included the hospitalization/discharge databank (Maintenance et exploitation de données pour l’étude de la clientèle hospitalière: MED-ECHO) and the Quebec emergency databank (Banque de données commune des urgences: BDCU), adding pertinent complementary information (e.g., having a family physician or not, illness acuity, patient reasons for visiting ED as evaluated by triage nurses). Finally, the local community health service center databank (Système d’information clinique et administrative des centres locaux de services communautaires) provided additional data on biopsychosocial services offered by the Quebec public primary care system, including medical interventions provided by salaried general practitioners (GP) and primary care MH services.
Variables
The dependent variable, frequency of patient hospitalization in 2014–15, included three categories: no hospitalization (0 times), moderate hospitalizations (1–2 times) and frequent hospitalizations (3+ times). While no consensus exists on the definition of frequent hospitalization, 3 hospitalizations per year has been the usual benchmark [3, 30–32]. Patients with 1–2 or moderate numbers of hospitalizations were considered at possible risk for frequent hospitalizations. The no-hospitalization group was used as a case control for the other group comparisons.
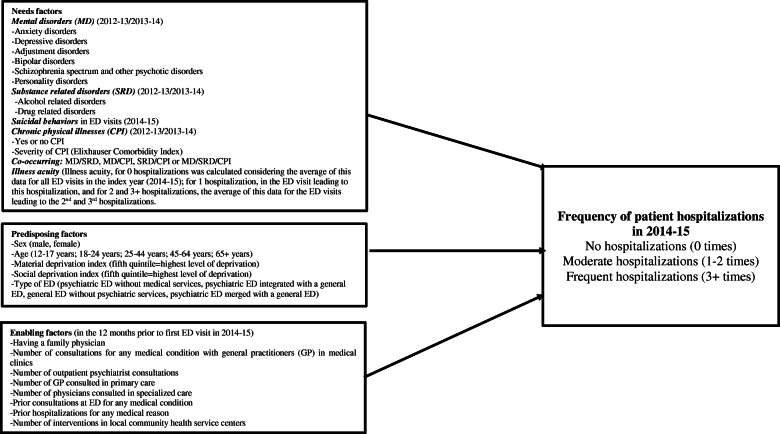
Based on the Andersen Behavioral Model (Fig. 1), needs factors consisted of various MD, including substance related disorders (SRD), based on the International Classification of Diseases Ninth Revision (ICD-9) from the RAMQ databank, or the Tenth Revision (ICD-10-CA) from the MED-ECHO and BDCU databanks. MD included: anxiety disorders, depressive disorders, adjustment disorders (common MD); and bipolar disorders, personality disorders, schizophrenia spectrum and other psychotic disorders (serious MD). SRD encompassed: alcohol related disorders (alcohol use disorders, alcohol induced disorders, alcohol intoxication) and drug related disorders (drug use disorders, drug induced disorders, drug intoxication). Suicidal behaviors, related to both suicidal ideation and attempt, as the reason for ED visit was extracted from the 2014–15 BDCU. Based on the Elixhauser Comorbidity Index [33], having chronic physical illnesses or not, and level of severity (0 to 3+), were recorded. Different combinations of co-occurring disorders involving MD, SRD and chronic physical illnesses were included. MD and SRD had to be recorded at least once in the two years (2012–13/2013–14) prior to the index year; and chronic physical illnesses twice yearly in the RAMQ databank, or once in the MED-ECHO, based on previous research [34]. As MD usually involve a course lasting more than one year, a two-year period was chosen as the standard for identifying patients diagnosed with MD prior to a first ED visit in 2014–15 [35–37]. Illness acuity at ED visit was also considered, based on the Canadian Triage Acuity Scale [38]. Illness acuity levels range from 1 (most urgent) to 5 (least urgent) and determine ED treatment order based on symptoms. For this study, they were grouped into levels 1–2 (immediate and very urgent), 3 (urgent) and 4–5 (less urgent and non-urgent). Ambulatory care is considered more appropriate than ED treatment for triage levels 4 and 5 [38]. For patients with no hospitalization following an ED visit, average illness acuity for all ED visits in 2014–15 was considered. Whereas for patients with 1–2 hospitalizations, or those with 3+ hospitalizations, illness acuity at the most recent ED visit prior to last hospitalization in each group was calculated.
Fig. 1.
Conceptual framework of factors tested for associations with no, moderate, and frequent hospitalizations for any medical condition in 2014–15 (for patients who visited Quebec emergency departments (ED) at least once in 2014–15 for mental health (MH) reasons)
Predisposing factors were sex (male, female), age (12–17 years, 18–24 years, 25–44 years, 45–64 years, and 65+ years) and material and social deprivation indices [29]. Deprivation indices combine six indicators from the 2011 Canadian census for the smallest geographical units from which census data are retrieved. The material deprivation index considers the employment-to-population ratio, the proportion of individuals without a high school diploma, and average income [29]. The social deprivation index includes proportions of individuals living alone, single-parent families, and individuals separated, divorced, or widowed [29]. Both indices are classified in quintiles, with the fifth quintile representing highest level of deprivation. The types of ED were classified in four groups: psychiatric ED without medical services within a MH university institute, psychiatric ED integrated with a general ED located in a separate site, general ED without psychiatric services, and psychiatric ED merged with a general ED.
Enabling factors included having a family physician (2014–15), and use of the following services in the 12 months preceding the first 2014–15 ED visit: number of consultations for any medical condition with a general practitioner (GP) in medical clinics (0, 1–3 and 4+ consultations); number of outpatient psychiatrist consultations (0, 1–3, 4–6, and 7+ consultations); number of GP consulted in primary care (0, 1–2, 3+); number of physicians consulted in specialized care (0, 1–2, 3+); prior consultations at ED for any medical condition: prior hospitalizations for any medical condition; and number of interventions in local community health service centers (0, 1–3 and 4+ interventions), i.e. primary care biopsychosocial services.
Statistical analysis
The data were first imputed, showing less than 1% missing data which were replaced by the means [39, 40]. Descriptive analyses were performed including two-way frequency tables for each independent variable, in association with each of the three levels of the dependent variable (no hospitalizations, moderate hospitalizations, and frequent hospitalizations). Bivariate analyses were conducted, and independent variables found significant (p < .05) were included in the multivariable model. Collinearity statistics were also tested using variance inflation factors (VIF) and tolerance tests, with 5 as the maximum level of VIF. Only independent variables found without collinearity were entered in the model. A multivariable hierarchical multinomial logistic regression was run. Needs, predisposing and enabling factors were entered in the model in that order, based on previous studies concerning service use [22, 41–43]. AIC (Akaike’s Information Criterion) and BIC (Bayesian information criterion ) were used as criteria for the selection of the model. A stepwise forward method was also conducted for the estimation of parameters in the multinomial hierarchical logistic regression model. All analyses were performed using SPSS 24.0.
Results
Tables 1, 2 and 3 present sample characteristics. In terms of needs factors for the two years prior to the first 2014–15 ED visit, 67% of study participants had been diagnosed with MD and 15% with SRD. Of those with MD, 40% had common MD (e.g. depressive disorders, anxiety disorders), and 26% serious MD (schizophrenia spectrum and other psychotic disorders, bipolar disorders). Forty percent of patients presented with suicidal behaviors in the ED visit during the index year 2014–15. Approximately one third (31%) were diagnosed with chronic physical illnesses, although severity levels were low in 77% of cases according to the Elixhauser comorbidity index (index 0). The most common co-occurring disorders were MD/chronic physical illnesses (34%) and MD/SRD (18%). Most patients (67%) presented at ED with illness acuity levels of 4 or 5 (less urgent and non-urgent). Regarding predisposing factors, 38% of patients were between 25 and 44 years of age, half of them female (51%). Material deprivation levels varied little among patients. However, 54% lived in the two most socially deprived areas (levels 4–5). Most patients (29%) had consulted a psychiatric ED without medical services. Concerning enabling factors, 49% of patients reported having a family physician (2014–15). In the 12 months prior to their first 2014–15 ED visit, 30 % had not consulted a GP in primary care; 31% had seen one or two physicians, and 39% three or more. Of the 46% who consulted outpatient psychiatrists, 25% made 7+ consultations. Forty-two percent had not consulted a physician in specialized care; 48% had been seen by one or two physicians, and 10% by three or more. Seventy-three percent made prior ED visits, and 22% had prior hospitalizations for any medical condition. The overall number of interventions in local community health service centers was low, with most patients (60%) receiving no intervention at all.
Table 1.
Variables related to needs factors predicting frequency of patient hospitalizations for any medical condition in 2014–15
| Characteristics | Total N (%) |
No hospitalizations (0 times) N (%) |
Moderate hospitalizations (1–2 times) N (%) |
Frequent hospitalizations (3+ times) N (%) |
p |
|---|---|---|---|---|---|
| Overall | 11,367 (100) | 6424 (56.5) | 4192 (36.9) | 751 (6.6) | |
| Needs factors | |||||
| Mental disorders (MD) (2012–2014) | 7624 (67.1) | 4176 (65.0) 2 | 2931 (69.9) 1 | 517 (68.8) | .00 |
| Common MD | 4569 (40.2) | 2484 (38.7) 2 | 1783 (42.5) 1 | 302 (40.2) | .00 |
| Depressive disorders | 1468 (12.9) | 722 (11.2) 2,3 | 636 (15.2) 1 | 110 (14.6) 1 | .00 |
| Anxiety disorders | 3870 (34.0) | 2155 (33.5) | 1462 (34.9) | 253 (33.7) | .36 |
| Adjustment disorders | 3841 (33.8) | 2183 (34.0) | 1415 (33.8) | 243 (32.3) | .67 |
| Serious MD | 3004 (26.4) | 1480 (23.0) 2,3 | 1293 (30.8) 1 | 231 (30.8) 1 | .00 |
| Schizophrenia spectrum and other psychotic disorders | 2144 (18.9) | 1074 (16.7) 2,3 | 905 (21.6) 1 | 165 (22.0) 1 | .00 |
| Bipolar disorders | 1564 (13.8) | 764 (11.9) 2,3 | 683 (16.3) 1 | 117 (15.6) 1 | .00 |
| Personality disorders | 1442 (12.7) | 925 (14.4) 2,3 | 453 (10.8) 1 | 64 (8.5) 1 | .00 |
| Substance-related disorders (SRD) (drug and alcohol) (2012–2014) | 1805 (15.3) | 1036 (15.2) | 657 (15.5) | 112 (14.9) | .86 |
| Alcohol related disorders | 1112 (9.8) | 562 (8.7) 2 | 468 (11.2) 1 | 82 (10.9) | .00 |
| Drug related disorders | 1086 (9.6) | 678 (10.6) 2,3 | 357 (8.5) 1 | 51 (6.8) 1 | .00 |
| Suicidal behaviors in ED visits (2014–2015) | 4512 (39.7) | 2810 (43.7) 2,3 | 1456 (34.7) 1 | 246 (32.8) 1 | .00 |
| Chronic physical illnesses | 3547 (31.2) | 1471 (22.9) 2,3 | 1609 (38.4) 1,3 | 467 (62.2) 1,2 | .00 |
| Elixhauser Comorbidity Index (2012–2014) a | .00 | ||||
| 0 | 8713 (76.7) | 5293 (81.6) 2,3 | 3049 (72.7) 1,3 | 425 (56.6) 1,2 | .00 |
| 1 | 1120 (9.9) | 617 (9.6) | 414 (9.9) | 89 (11.9) | .00 |
| 2 | 635 (5.6) | 278 (4.3) 2,3 | 291 (6.9) 1 | 66 (8.8) 1 | .00 |
| 3+ | 899 (7.9) | 290 (4.5) 2,3 | 438 (10.4) 1,3 | 171 (22.8) 1,2 | .00 |
| Co-occurring MD/SRD | 2084 (18.3) | 726 (11.3) 2,3 | 1054 (25.1) 1,3 | 304 (40.5) 1,2 | .00 |
| Co-occurring MD/chronic physical illnesses | 3843 (33.8) | 1219 (19.0) 2,3 | 2073 (49.5) 1,3 | 551 (73.4) 1,2 | .00 |
| Co-occurring SRD/chronic physical illnesses | 1047 (9.2) | 260 (4.0) 2,3 | 571 (13.6) 1,3 | 216 (28.8) 1,2 | .00 |
| Co-occurring MD/SRD/chronic physical illnesses | 903 (7.9) | 175 (2.7) 2,3 | 522 (12.5) 1,3 | 206 (27.4) 1,2 | .00 |
| Illness acuity b | .00 | ||||
| Levels 1 and 2 (immediate and very urgent) | 1173 (10.3) | 639 (9.9) 2,3 | 482 (11.5) 1,3 | 52 (6.9) 1,2 | |
| Level 3 (urgent) | 2556 (22.5) | 1456 (22.7) 3 | 1003 (23.9) 3 | 94 (12.5) 1,2 | |
| Levels 4 and 5 (less urgent and non-urgent) | 7638 (67.3) | 4326 (67.3) 2,3 | 2707 (64.6) 1,3 | 605 (80.6) 1,2 | |
χ2 Comparisons are produced for each row reporting percentages for categorical variables. Superscript indicates a significant difference at p < .05. For example, the percentage of individuals with MD having no hospitalizations was significantly different than the one having 1–2 hospitalizations. No hospitalizations = column 1, moderate hospitalizations [1, 2]=column 2, and frequent hospitalizations (3+ times) = column 3
aChronic physical illnesses included: chronic pulmonary disease, cardiac arrhythmias, tumor and/or metastasis, renal disease, fluid electrolyte disorders, myocardial infarction, congestive heart failure, metastatic cancer, dementia, stroke, neurological disorders, liver disease, pulmonary circulation disorders, coagulopathy, weight loss, paralysis, AIDS/HIV
bPatients in the study sample had visited ED at least one time in 2014–15 for mental health conditions. For 0 hospitalizations, illness acuity was calculated considering the average of this data for all ED visits in the index year (2014–15); for 1 hospitalization, in the ED visit leading to this hospitalization; and for 2 and 3+ hospitalizations, the average of these data for the ED visits leading to the 2nd and 3rd hospitalizations
Table 2.
Variables related to predisposing factors predicting frequency of patient hospitalizations for any medical condition in 2014–15
| Characteristics | Total N (%) |
No hospitalizations (0 times) N (%) |
Moderate hospitalizations (1–2 times) N (%) |
Frequent hospitalizations (3+ times) N (%) |
p |
|---|---|---|---|---|---|
| Overall | 11,367 (100) | 6424 (56.5) | 4192 (36.9) | 751 (6.6) | |
| Predisposing factors (2014–2015) | |||||
| Age | .00 | ||||
| 12–17 years | 739 (6.5) | 492 (7.7) 2,3 | 190 (4.5) 1,3 | 57 (7.6) 1,2 | |
| 18–24 years | 1953 (17.2) | 1067 (16.6) | 751 (17.9) | 135 (18.0) | |
| 25–44 years | 4330 (38.1) | 2472 (38.5) | 1569 (37.4) | 289 (38.5) | |
| 45–64 years | 3128 (27.5) | 1748 (27.2) | 1185 (28.3) | 195 (26.0) | |
| 65 years+ | 1217 (10.7) | 645 (10.0) 2 | 497 (11.9) 1 | 75 (10.0) | |
| Sex | .92 | ||||
| Male | 5537 (48.7) | 3128 (48.7) | 2038 (48.6) | 371 (49.4) | |
| Female | 5830 (51.3) | 3296 (51.3) | 2154 (51.4) | 380 (50.6) | |
| Deprivation Index: | |||||
| Material | .27 | ||||
| 1: Least deprived | 2402 (21.1) | 1382 (21.5) | 860 (20.5) | 160 (21.3) | |
| 2 | 1747 (15.4) | 985 (15.3) | 647 (15.4) | 115 (15.3) | |
| 3 | 2038 (17.9) | 1153 (17.9) | 761 (18.2) | 124 (16.5) | |
| 4 | 1978 (17.4) | 1134 (17.7) | 721 (17.2) | 123 (16.4) | |
| 5: Most deprived | 2187 (19.2) | 1213 (18.9) | 834 (19.9) | 140 (18.6) | |
| Not assigned a | 1015 (8.9) | 557 (8.7) | 369 (8.8) | 89 (11.9) | |
| Social | .02 | ||||
| 1: Least deprived | 1367 (12.0) | 771 (12.0) | 502 (12.0) | 94 (12.5) | |
| 2 | 1257 (11.1) | 719 (11.2) | 456 (10.9) | 82 (10.9) | |
| 3 | 1540 (13.5) | 907 (14.1) 2 | 532 (12.5) 1 | 110 (14.5) | |
| 4 | 2528 (22.2) | 1445 (22.5) | 924 (22.0) | 159 (21.2) | |
| 5: Most deprived | 3660 (32.2) | 2025 (31.5) 2 | 1418 (33.8) 1,3 | 217 (28.9) 2 | |
| Not assigned a | 1015 (8.9) | 557 (8.7) 3 | 369 (8.8) 3 | 89 (11.9) 1,2 | |
| Type of emergency department (ED) | .00 | ||||
| Psychiatric ED without medical services | 3296 (29.0) | 1829 (28.5) | 1250 (29.8) | 217 (28.9) | |
| Psychiatric ED integrated with a general ED located in a separate site | 2039 (17.9) | 1238 (19.3) 2,3 | 696 (16.6) 1 | 105 (14.0) 1 | |
| General ED without psychiatric services | 2871 (25.3) | 1663 (25.9) | 1041 (24.8) | 167 (22.2) | |
| Psychiatric ED merged with a general ED | 3161 (27.8) | 1694 (26.4) 2,3 | 1205 (28.7) 1,3 | 262 (34.9) 1,2 | |
χ2 Comparisons were produced for each row reporting percentages for categorical variables. Superscript indicates a significant difference at p < .05. For example, the percentage of individuals who were 12–17 years old having no hospitalizations was significantly different than the group with 1–2 or 3+ hospitalizations. No hospitalizations (0 times) = column 1, moderate hospitalizations (1–2 times) = column 2, and frequent hospitalizations (3+ times) = column 3
aThis corresponds to missing address or to residence in an area where index assignment is not available. An index cannot usually be assigned to residents of long-term health care units or homeless individuals
Table 3.
Variables related to enabling factors predicting frequency of patient hospitalizations for any medical condition in 2014–15
| Characteristics | Total N (%) |
No hospitalization (0 times) N (%) |
Moderate hospitalizations (1–2 times) N (%) |
Frequent hospitalizations (3+ times) N (%) |
p |
|---|---|---|---|---|---|
| Overall | 11,367 (100) | 6424 (56.5) | 4192 (36.9) | 751 (6.6) | |
| Enabling factors | |||||
| Having a family physician (2014–15) | 5534 (48.7) | 3157 (49.1) | 2016 (48.1) | 361 (48.1) | .54 |
| Number of consultations for any medical condition with a general practitioner (GP) in private clinics a | .00 | ||||
| 0 visits | 3536 (31.1) | 1779 (27.7) 2,3 | 1461 (34.9) 1,3 | 296 (39.4) 1,2 | |
| 1–3 visits | 4336 (38.1) | 2565 (39.9) 2,3 | 1525 (36.4) 1 | 246 (32.8) 1 | |
| 4+ visits | 3495 (30.7) | 2080 (32.4) 2,3 | 1206 (28.8) 1 | 209 (27.8) 1 | |
| Number of outpatient psychiatrist consultations a | .00 | ||||
| 0 consultations | 6097 (53.6) | 4653 (72.4) 2,3 | 1297 (30.9) 1,3 | 147 (19.6) 1,2 | |
| 1–3 consultations | 1744 (15.3) | 1010 (15.7) 3 | 664 (15.8) 3 | 70 (9.3) 1,2 | |
| 4–6 consultations | 742 (6.5) | 294 (4.6) 2,3 | 387 (9.2) 1 | 61 (8.1) 1 | |
| 7+ consultations | 2784 (24.5) | 467 (7.3) 2,3 | 1844 (44.0) 1,3 | 473 (63.0) 1,2 | |
| Number of GP consulted in primary care a | .00 | ||||
| 0 GPs | 3421 (30.1) | 1866 (29.0) 2 | 1311 (31.3) 1 | 244 (32.5) | |
| 1–2 GPs | 3525 (31.0) | 1897 (29.5) 2 | 1381 (32.9) 1 | 247 (32.9) | |
| 3+ GPs | 4421 (38.9) | 2661 (41.4) 2,3 | 1500 (35.8) 1 | 260 (34.6) 1 | |
| Number of physicians consulted in specialized care a | .00 | ||||
| 0 physicians | 4726 (41.6) | 3833 (59.7) 2,3 | 791 (18.9) 1,3 | 102 (13.6) 1,2 | |
| 1–2 physicians | 5466 (48.1) | 2176 (33.9) 2,3 | 2772 (66.1) 1 | 518 (69.0) 1 | |
| 3+ physicians | 1175 (10.3) | 415 (6.5) 2,3 | 629 (15.0) 1 | 131 (17.4) 1 | |
| Prior consultations at emergency department (ED) for any medical condition a | 8256 (72.6) | 4088 (36.0) 2,3 | 3448 (30.3) 1,3 | 720 (6.3) 1,2 | .00 |
| Prior hospitalizations for any medical condition a | 2461 (21.7) | 1365 (21.2) | 928 (22.1) | 168 (22.1) | .49 |
| Number of overall interventions in local community health service centers a | |||||
| 0 interventions | 6806 (59.9) | 4074 (63.4) 2,3 | 2387 (56.9) 1,3 | 345 (45.9) 1,2 | |
| 1–3 interventions | 1749 (15.4) | 980 (15.3) | 668 (15.9) | 101 (13.4) | |
| 4+ interventions | 2812 (24.7) | 1370 (21.3) 2,3 | 1137 (27.1) 1,3 | 305 (40.6) 1,2 | |
χ2 Comparisons were produced for each row reporting percentages for categorical variables. Superscript indicates a significant difference at p < .05. For example, the percentage of individuals with 0 visits to the GP was significantly different than the one with 1–3 or 4+ visits. No hospitalizations (0 times) = column 1, moderate hospitalizations (1–2 times) = column 2, and frequent hospitalizations (3+ times) = column 3
aMeasured in the 12 months prior to first ED visit in the index year (2014–2015)
Of the 11,367 ED users with MD, most were not hospitalized (56%), while 37% had 1 or 2 (27 and 10% respectively: moderate) hospitalizations, and 7% had 3+ (frequent) hospitalizations. Concerning the principal conditions for hospitalization, 56% were admitted for physical illnesses and 44% for MD, including 9% for SRD. The mean duration of hospital stay per admission was 28.5 days (SD = ±46.1) for those with moderate hospitalizations, and 72.0 days (SD = ±67.5) for those with frequent hospitalizations, who also had 4 hospitalizations on average, ranging from 1 to 28. Among patients hospitalized 2 or 3+ times, 18% were readmitted within 30 days of discharge. Independent variables significantly associated with frequency of hospitalization in the bivariate analyses are presented in Tables 1 to 3.
Table 4 presents results for the hierarchical multinomial logistic regression. Concerning needs factors, patients with the highest risk of both moderate or frequent hospitalization rates, as compared with the index group (no hospitalizations), had more chronic physical illnesses, co-occurring MD/SRD, alcohol related disorders, and depressive disorders. Moreover, only patients with moderate hospitalization rates were more likely to be diagnosed with schizophrenia spectrum and other psychotic disorders, and bipolar disorders. Patients with less risk for both frequent and moderate hospitalization rates, as compared with the index group (no hospitalizations), also had more personality disorders, drug related disorders and suicidal behaviors. Only patients with moderate hospitalization rates were less likely to have illness acuity levels 4–5 than patients with no hospitalizations. Regarding predisposing factors, age groups 18–24, 25–44, 45–64, and 65+ years were associated with moderate hospitalizations only, with the 65+ age group most at risk. Patients with frequent hospitalizations only were less likely to visit psychiatric ED integrated with a general ED located in a separate site or a general ED without psychiatric services as compared with the no hospitalizations group. Patients with moderate hospitalizations only were less likely to visit psychiatric ED integrated with a general ED located in a separate site compared with the no hospitalizations group. Enabling factors associated with both frequent and moderate hospitalization rates included consultations with outpatient psychiatrists, prior consultation at ED for any medical condition and number of physicians consulted in specialized care. Particularly high odds ratios were observed for the group making 7+ consultations with outpatient psychiatrists. Only patients with frequent hospitalizations were likely to have more overall interventions (4+) in local community health service centers as compared with patients with no hospitalizations. The final model explained 44% of the variance (Nagelkerke R2). Enabling factors accounted for 28% of the total variance, needs factors 15%, and predisposing factors 1%. The model had also acceptable goodness of fit (Pearson and chi-square statistics (p > .05)).
Table 4.
Estimations of regression coefficients and odds ratios from the multinomial logistic regression model for frequency of patient hospitalizations for any medical condition in 2014–2015. The model reference group is non-hospitalized patients
| Variables | Moderate hospitalizations: 1–2 times (2014–15) | Frequent hospitalizations: 3+ times (2014–15) | ||||||
|---|---|---|---|---|---|---|---|---|
| Coefficients | P-Value | OR | 95% CI | Coefficients | P-Value | OR | 95% CI | |
| Needs factors | ||||||||
| Mental disorders (MD) (2012–2014) | ||||||||
| Depressive disorders | .31 | .00 | 1.35 | 1.17–1.57 | .34 | .01 | 1.41 | 1.08–1.84 |
| Schizophrenia spectrum and other psychotic disorders | .19 | .00 | 1.21 | 1.06–1.38 | .23 | .05 | 1.26 | 1.00–1.58 |
| Bipolar disorders | .28 | .00 | 1.32 | 1.14–1.52 | .23 | .09 | 1.25 | .96–1.63 |
| Personality disorders | −.41 | .00 | .66 | .57–.77 | −.65 | .00 | .52 | .38–.71 |
| Alcohol related disorders | .33 | .00 | 1.39 | 1.17–1.64 | .41 | .01 | 1.50 | 1.11–2.04 |
| Drug related disorders | −.29 | .00 | .75 | .63–.89 | −.43 | .02 | .65 | .46–.93 |
| Suicidal behaviors in emergency department (ED) visits (2014–2015) | −.24 | .00 | .79 | .72–.87 | −.24 | .01 | .78 | .65–.95 |
| Co-occurring MD/substance related disorders (SRD) | .74 | .00 | 2.09 | 1.85–2.36 | 1.50 | .00 | 4.45 | 3.68–5.44 |
| Chronic physical illnesses (2012–2014) | .70 | .00 | 2.02 | 1.82–2.24 | 1.64 | .00 | 5.15 | 4.30–6.18 |
| Illness acuity (triage priority levels) a, b | ||||||||
| Level 3 (urgent) | −.15 | .09 | .86 | .72–1.03 | .25 | .15 | 1.29 | .91–1.81 |
| Levels 4–5 (less urgent and non-urgent) | −.38 | .00 | .69 | .58–.81 | −.29 | .15 | .75 | .51–1.11 |
| Predisposing factors (2014–15) | ||||||||
| Age b | ||||||||
| 18–24 years | .65 | .00 | 1.91 | 1.52–2.40 | .30 | .14 | 1.35 | .91–1.99 |
| 25–44 years | .52 | .00 | 1.68 | 1.35–2.08 | .17 | .38 | 1.18 | .82–1.17 |
| 45–64 years | .60 | .00 | 1.81 | 1.45–2.26 | .05 | .79 | 1.05 | .72–1.53 |
| 65+ years | .74 | .00 | 2.10 | 1.64–2.69 | .16 | .47 | 1.17 | .76–1.81 |
| Deprivation Index: | ||||||||
| Social | ||||||||
| 2 | −.08 | .41 | .92 | .76–1.12 | −.16 | .38 | .85 | .60–1.21 |
| 3 | −.08 | .36 | .92 | .78–1.09 | .03 | .86 | 1.03 | .77–1.38 |
| 4 | −.03 | .67 | .97 | .81–1.14 | −.14 | .36 | .86 | .64–1.18 |
| 5: Most deprived | .04 | .65 | 1.04 | .88–1.22 | −.15 | .30 | .86 | .64–1.15 |
| Types of ED b | ||||||||
| Psychiatric ED integrated with a general ED located in a separate site | −.14 | .03 | .87 | .76–.99 | −.44 | .00 | .65 | .51–.82 |
| General ED without psychiatric services | .03 | .70 | 1.03 | .88–1.20 | −.25 | .01 | .78 | .58–1.05 |
| Psychiatric ED merged with general ED | .10 | .15 | 1.10 | .97–1.26 | −.17 | .15 | .85 | .67–1.06 |
| Enabling factors c | ||||||||
| Number of consultations for any medical condition with a general practitioner (GP) in medical clinics b | ||||||||
| 1–3 consultations | .03 | .56 | 1.03 | .93–1.15 | −.05 | .63 | .95 | .78–1.16 |
| 4+ consultations | −.00 | .97 | .99 | .88–1.13 | −.12 | .31 | .88 | .71–1.12 |
| Number of outpatient psychiatrist consultations b | ||||||||
| 1–3 consultations | .23 | .00 | 1.26 | 1.09–1.47 | .43 | .02 | 1.54 | 1.06–2.23 |
| 4–6 consultations | .85 | .00 | 2.33 | 1.92–2.83 | 1.42 | .00 | 4.13 | 4.75–6.19 |
| 7+ consultations | 2.02 | .00 | 7.52 | 6.45–8.77 | 3.18 | .00 | 24.00 | 17.52–33.00 |
| Number of physicians consulted in specialized care b | ||||||||
| 1–2 physicians | 1.06 | .00 | 2.88 | 2.50–3.30 | .82 | .00 | 2.27 | 1.53–3.37 |
| 3+ physicians | 1.20 | .00 | 3.31 | 2.74–3.99 | .59 | .00 | 1.78 | 1.28–2.53 |
| Prior consultations at ED for any medical condition | .99 | .00 | 2.71 | 2.42–3.04 | .25 | .00 | 11.94 | 8.16–17.47 |
| Number of interventions in local community service centers b | ||||||||
| 1–3 interventions | .02 | .72 | 1.03 | .90–1.17 | .00 | .99 | .99 | .77–1.30 |
| 4+ interventions | −.02 | .80 | .99 | 88–1.10 | .46 | .00 | 1.58 | 1.30–1.93 |
aFor 0 hospitalizations, illness acuity was calculated considering the average of this data for all ED visits in the index year (2014–15); for 1 hospitalization, in the ED visit leading to this hospitalization; and for 2 and 3+ hospitalizations, the average of these data for the ED visits leading to the 2nd and 3rd hospitalizations
b Reference groups for independent variables with multiple categories were: level 1 and 2 (immediate and very urgent) for illness acuity; 12–17 years for age category; psychiatric ED without medical services within a MH university institute for type of ED; 0 visits for number of consultations for any medical condition with a general practitioner (GP) in medical clinics, number of outpatient psychiatrist consultations, number of physicians consulted in specialized care, and number of interventions in local community health service centers
cMeasured in the 12 months prior to first ED visit in the index year (2014–2015)
Discussion
This study identified risk factors for frequency of hospitalization for any medical condition among patients who visited ED at least once in 2014–15 for MH conditions, based on the Andersen Behavioral Model [22]. Results showed that roughly one third of patients had moderate [1, 2] hospitalizations over the 12-month study period, whereas 7% had frequent hospitalizations (3+). Readmission rates in the index year were slightly higher (39%) in this study compared with rates reported in previous research (30–33%) [32, 44]. This difference is easily explained by the inclusion of hospitalizations for both MH and physical illnesses in this study, the latter conditions being more important.
Findings did not confirm the hypothesis that frequent hospitalizations would be more strongly associated with needs factors. Enabling factors accounted for the largest percentage of total variance explained in the study model and were mainly associated with an increased risk for both moderate and frequent hospitalizations even though several needs factors were identified as risk factors.
The finding that prior ED use was a risk factor for increased hospitalization is consistent with the literature [30, 32, 45]. Interestingly, the frequency of outpatient psychiatrist consultations, even as many as 7+, predicted both moderate and frequent hospitalizations, suggesting that these patients had complex conditions (co-occurring disorders and probably important social problems) requiring more extensive and comprehensive care than could be provided by psychiatrist consultations alone. These patients may also have encountered more episodes of exacerbation related to their illnesses and needing inpatient treatment. These hospitalizations may have been planned and may have been shorter, however; but this was unfortunately not measured in this study. Perhaps specialized treatments were also not always adequate to respond to patients with high needs and prevent hospitalization. Research on adequacy of help confirms the difficulty of treating such patients with co-occurring disorders and complex needs. These patients are often viewed as those with “unmet needs” [46, 47]. Even though a third of patients didn’t consult a GP in the 12 months prior to first 2014–15 ED visit, and more than half reported having no family physician, the number of physician consultations in specialized care was found to be associated with increased risk for moderate and frequent hospitalizations. This result was likely associated with the higher rates of chronic physical illnesses in both groups requiring more specialized care.
The single risk factor for frequent hospitalizations only was a high number (4+) of overall interventions in local community health service centers. These centers have reportedly been designated for the treatment of more vulnerable and deprived populations [48]. Some patients may be homeless [49] or affected by other complex conditions, especially psychosocial problems, that may lead to hospitalization due to difficulties involving access to treatment [50, 51]. Moreover, GP working in these centers are known to treat the largest proportion of patients with MD or SRD with complex needs; they thus have greater experience and are used to working in collaboration with MH services [52]. As GP are employed on a salaried basis, as opposed to fee-for-services in private clinics, they are able to dedicate more time to complex patients. Additionally, these centers employ a variety of staff such as social workers, nurses, and nutritionists offering comprehensive care for more vulnerable populations. Training in crisis management and increased multi-modal clinical approaches for staff in these centers may be helpful in reducing hospitalizations as they are likely to be the primary source of care for these patients [52, 53]. Several studies confirm that psychosocial MH interventions and compliance with follow-up directives may reduce the risk of hospitalization [45, 54, 55]; yet such interventions may be insufficient or poorly integrated with other healthcare services to adequately meet the needs of patients with frequent hospitalizations.
Concerning needs factors, the association between diagnoses of depressive disorders with moderate and frequent hospitalizations mirrored the associations with higher rates of hospital readmission reported in previous studies [11, 56, 57]. High rates of co-occurring disorders [16, 58] and poor health outcomes [59, 60] were also frequent characteristics among these patients. Few services are available for Quebec patients with common mental disorders including depressive disorders, with onerous wait times for free counselling services [48]. Alcohol-related disorders [61], withdrawal [62–64], and co-occurring MD/SRD [65, 66] have been shown to elevate the risk of hospital readmission. Higher hospitalization rates may also be explained by higher rates of physical illnesses in patients with co-occurring MD/SRD [25, 67, 68], such as cardiovascular diseases [69], metabolic syndrome [70, 71], obesity [72] and liver diseases [73].
In fact, patients with both frequent and moderate hospitalizations presented more severe and complex conditions than those not hospitalized; but moderate hospitalizations included patients with more serious MD than those who were frequently hospitalized. Surprisingly, serious psychiatric disorders (schizophrenia spectrum and other psychotic disorders or bipolar disorders) predicted moderate hospitalizations only. It may be that patients with serious MD received more intensive ambulatory biopsychosocial care such as assertive community treatment (ACT) and intensive case management, than other patients, as previous Quebec MH reforms have aimed to consolidate services for these patients in particular. ACT and case management have been found to prevent rehospitalization [74]. Unfortunately, such outpatient services were not measured in this study, as the focus was more on physician services and public primary care psychosocial services. However, illness acuity level 4–5 was less likely to be associated with moderate hospitalizations only, indicating that most patients in the “moderate” group were presenting at ED for urgent medical conditions.
Unlike results of other studies [27, 61], this study identified personality disorders, drug related disorders and suicidal behaviors as negative predictors of hospitalization among patients with moderate or frequent hospitalizations compared with no hospitalizations. This situation may be partially due to stigmatizing attitudes among hospital staff toward patients with personality disorders or drug related disorders, considering them less than optimal candidates for hospitalization [75, 76]. Research also indicates that effective treatment for personality disorders involves sound psychiatric management [77] and effective psychological and psychosocial treatments [78, 79], rather than hospitalization. As well, suggested treatments for drug related disorders include opioid agonist treatment integrated with psychosocial treatment, rather than hospitalization [80–82]. Thus, such patients may more likely have been discharged after an ED visit than hospitalized. Differences in study results may also be a function of service availability and the organization of care in various settings [83]. Moreover, personality disorders are often associated with suicidal behaviors [84, 85]. Patients in this study experienced more suicidal ideation than attempts, which may explain their potentially greater frequency of referrals to outpatient services, including crisis centers, over hospitalization. While some studies have found increased risk of hospitalization following instances of suicidal behaviors [23, 55, 65], others found no such association [86, 87].
Concerning predisposing factors, the fact that visiting a psychiatric ED integrated with a general ED in a separate site was associated with lower risk of moderate and frequent hospitalizations may be explained by better coverage and more integrated care in this type of ED as well as increased access to health services, which may have reduced hospital use. The implementation of new assertive community treatment and intensive case management programs targeted to frequently hospitalized patients, under the MH reform, may have directly contributed to this positive outcome. A lower risk of moderate and frequent hospitalizations was also found for patients who had visited the general ED without psychiatric services. The fact that most patients were hospitalized for physical illnesses only may explain their reduced risk of hospitalization.
The association of all age groups, except the 12–17 group, with moderate hospitalizations speaks to the underutilization of services by youth. Low hospitalization rates in the 12–17 age group have also been identified in other studies [24, 88]. While most MD appear at an early age, they are often diagnosed several years after the first symptoms appear. Outpatient services are favored by this group, as young people view hospitalization as very stigmatizing [89]. However, all age groups were represented among those with frequent hospitalizations in this study. Studies have underlined that youth is a predictor for high ED use [90, 91]. Results related to material and social deprivation were not associated with risk of hospitalization in the final model of this study, which coincided with previous studies that have generally reported mixed results [92, 93]. The study results on material deprivation may be explained by the universal Canadian healthcare system, whereas social deprivation did not seem a sufficient risk factor to influence whether such health conditions would lead to hospitalizations.
This study had several limitations that should be mentioned. First, the data were drawn from administrative databanks that were not primarily developed for clinical investigation, but for financial purposes, suggesting that they be interpreted with caution. Second, the data excluded many key variables not available in the Quebec databanks such as ambulatory services delivered by hospitals not provided by physicians, private services such as psychologists, and community-based services which may have contributed to prevent hospitalization. Data on patient medication consumption and on psychopharmacological treatment adherence were also not unavailable for all patients, precluded their use in this study. It is well known that lack of treatment adherence is a key risk factor for hospitalization [94]. As well, the Quebec databanks did not include key variables, such as homelessness [95], race/ethnicity [32, 96] or MD symptom severity, which may have contributed to hospitalization. Third, the interaction between factors not studied may have had an overall impact on study results. Fourth, while all study participants had visited ED in 2014–15 for MH conditions, the sample was not entirely composed of patients diagnosed with MD-SRD. Finally, the results may not be generalizable to other healthcare systems, particularly those without universal coverage as in Quebec/Canada.
Conclusions
This is the first study to examine risk factors for moderate and frequent hospitalizations compared with no hospitalizations for medical conditions among patients who visited different types of ED for MH conditions in 2014–15, using the Andersen Behavioral Model. Compared with patients who had no hospitalizations or moderate hospitalizations, those with frequent hospitalizations received relatively more interventions overall in local community health service centers, implying that this group consisted of more vulnerable patients with important biopsychosocial problems. Patients with frequent and moderate hospitalizations, compared with no hospitalizations, were also seen more often by outpatient psychiatrists, and had visited more ED previously for medical conditions. Overall, the results suggest that these patients had severe and complex conditions, including co-occurring MD/SRD as well as chronic physical illnesses. Compared with non-hospitalized patients, those with moderate hospitalizations presented more serious MD (schizophrenia spectrum and bipolar disorders), were more than 18 years old, and were less likely to have ED illness acuity levels 4–5. Based on these findings, strategies aimed at reducing frequent hospitalizations need to be provided to these patients, most of whom have co-occurring disorders, with more intensive and diversified biopsychosocial assistance, integrated treatments, and continuous care in response to their multiple needs. For the group with moderate hospitalizations, the focus should be on patients with serious MD, addressing their urgent needs more effectively. Overall, more comprehensive, intensive, and integrated outpatient services for MH-SRD and co-occurring physical illnesses are needed to avoid unnecessary hospitalizations, especially after hospital discharge. Improved access to primary care, both family physicians and local community health service centers, and planning for enhanced outpatient care after discharge are also recommended.
Acknowledgments
We gratefully acknowledge the support of the Canadian Institutes of health Research (CIHR). We would like to thank Judith Sabetti for editorial assistance.
Abbreviations
- BDCU
Banque de données commune des urgences (Quebec emergency databank)
- CI
Confidence interval
- ED
Emergency department
- GP
General practitioner
- MD
Mental disorder
- MED-ECHO
Maintenance et exploitation de données pour l’étude de la clientèle hospitalière (hospitalization/discharge databank)
- MH
Mental health
- SD
Standard deviation
- SRD
Substance related disorder
- SUD
Substance use disorder
- RAMQ
Régie d’Assurance Maladie du Québec (Quebec healthcare insurance)
Authors’ contributions
MJF and LP designed the study with the collaboration of the other authors. LG performed the statistical analysis. LP and GG wrote the first version of the manuscript, which was revised by MJF and YK. All authors have read and approved the final manuscript.
Funding
This study was funded by the Canadian Institutes of Health Research (CIHR), grant number 8400997.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The public health ethics committee of a MH university institute and the Quebec Access to Information Commission evaluated and approved the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Evans LJ, Harris V, Newman L, Beck A. Rapid and frequent psychiatric readmissions: associated factors. Int J Psychiatry Clin Pract. 2017;21(4):271–276. doi: 10.1080/13651501.2017.1324037. [DOI] [PubMed] [Google Scholar]
- 2.Hewlett E, Moran V. Making Mental Health Count: The Social and Economic Costs of Neglecting Mental Health Care [Internet]. OECD; 2014 [cited 2019 Aug 2]. (OECD Health Policy Studies). Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/making-mental-health-count_9789264208445-en.
- 3.Morlino M, Calento A, Schiavone V, Santone G, Picardi A, de Girolamo G. Use of psychiatric inpatient services by heavy users: findings from a national survey in Italy. Eur Psychiatry. 2011;26(4):252–259. doi: 10.1016/j.eurpsy.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Ascher-Svanum H, Zhu B, Faries DE, Salkever D, Slade EP, Peng X, et al. The cost of relapse and the predictors of relapse in the treatment of schizophrenia. BMC Psychiatry. 2010;10(1):2. doi: 10.1186/1471-244X-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pelayo-Terán JM, Gajardo Galán VG, de la Ortiz-García de la Foz V, Martínez-García O, Tabarés-Seisdedos R, Crespo-Facorro B, et al. Rates and predictors of relapse in first-episode non-affective psychosis: a 3-year longitudinal study in a specialized intervention program (PAFIP) Eur Arch Psychiatry Clin Neurosci. 2017;267(4):315–323. doi: 10.1007/s00406-016-0740-3. [DOI] [PubMed] [Google Scholar]
- 6.Kessing LV, Andersen PK. Evidence for clinical progression of unipolar and bipolar disorders. Acta Psychiatr Scand. 2017;135(1):51–64. doi: 10.1111/acps.12667. [DOI] [PubMed] [Google Scholar]
- 7.Richards D. Prevalence and clinical course of depression: a review. Clin Psychol Rev. 2011;31(7):1117–1125. doi: 10.1016/j.cpr.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Salvini R, da Silva DR, Lafer B, Dutra I. A multi-relational model for depression relapse in patients with bipolar disorder. Stud Health Technol Inform. 2015:741–5. [PubMed]
- 9.Kirshenbaum AP, Olsen DM, Bickel WK. A quantitative review of the ubiquitous relapse curve. J Subst Abus Treat. 2009;36(1):8–17. doi: 10.1016/j.jsat.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 11.Hanrahan NP, Bressi S, Marcus SC, Solomon P. Examining the impact of comorbid serious mental illness on rehospitalization among medical and surgical inpatients. Gen Hosp Psychiatry. 2016;42:36–40. doi: 10.1016/j.genhosppsych.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Chwastiak LA, Davydow DS, McKibbin CL, Schur E, Burley M, McDonell MG, et al. The effect of serious mental illness on the risk of Rehospitalization among patients with diabetes. Psychosomatics. 2014;55(2):134–143. doi: 10.1016/j.psym.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmedani BK, Simon GE, Stewart C, Beck A, Waitzfelder BE, Rossom R, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29(6):870–877. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ketterer MW, Draus C, McCord J, Mossallam U, Hudson M. Behavioral factors and hospital admissions/readmissions in patients with CHF. Psychosomatics. 2014;55(1):45–50. doi: 10.1016/j.psym.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 15.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet Lond Engl. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 16.Gunn JM, Ayton DR, Densley K, Pallant JF, Chondros P, Herrman HE, et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):175–184. doi: 10.1007/s00127-010-0330-z. [DOI] [PubMed] [Google Scholar]
- 17.Payne RA, Abel GA, Guthrie B, Mercer SW. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. Can Med Assoc J. 2013;185(5):E221–E228. doi: 10.1503/cmaj.121349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kisely S, Ehrlich C, Kendall E, Lawrence D. Using avoidable admissions to measure quality of Care for Cardiometabolic and Other Physical Comorbidities of psychiatric disorders: a population-based, record-linkage analysis. Can J Psychiatry Rev Can Psychiatr. 2015;60(11):497–506. doi: 10.1177/070674371506001105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pennington M, McCrone P. The cost of relapse in schizophrenia. PharmacoEconomics. 2017;35(9):921–936. doi: 10.1007/s40273-017-0515-3. [DOI] [PubMed] [Google Scholar]
- 20.Stensland M, Watson PR, Grazier KL. An examination of costs, charges, and payments for inpatient psychiatric treatment in community hospitals. Psychiatr Serv. 2012;63(7):666–671. doi: 10.1176/appi.ps.201100402. [DOI] [PubMed] [Google Scholar]
- 21.Trudnak T, Kelley D, Zerzan J, Griffith K, Jiang HJ, Fairbrother GL. Medicaid admissions and readmissions: understanding the prevalence, payment, and Most common diagnoses. Health Aff (Millwood) 2014;33(8):1337–1344. doi: 10.1377/hlthaff.2013.0632. [DOI] [PubMed] [Google Scholar]
- 22.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 23.Hamilton JE, Desai PV, Hoot NR, Gearing RE, Jeong S, Meyer TD, et al. Factors associated with the likelihood of hospitalization following emergency department visits for behavioral health conditions. Acad Emerg Med Off J Soc Acad Emerg Med. 2016;23(11):1257–1266. doi: 10.1111/acem.13044. [DOI] [PubMed] [Google Scholar]
- 24.Fuller RL, Atkinson G, McCullough EC, Hughes JS. Hospital readmission rates: the impacts of age, payer, and mental health diagnoses. J Ambulatory Care Manage. 2013;36(2):147–155. doi: 10.1097/JAC.0b013e3182866c1c. [DOI] [PubMed] [Google Scholar]
- 25.Wu L-T, Zhu H, Ghitza UE. Multicomorbidity of chronic diseases and substance use disorders and their association with hospitalization: Results from electronic health records data. Drug Alcohol Depend. 2018 01;192:316–23. [DOI] [PMC free article] [PubMed]
- 26.Prina AM, Cosco TD, Dening T, Beekman A, Brayne C, Huisman M. The association between depressive symptoms in the community, non-psychiatric hospital admission and hospital outcomes: a systematic review. J Psychosom Res. 2015;78(1):25–33. doi: 10.1016/j.jpsychores.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fok ML-Y, Chang C-K, Broadbent M, Stewart R, Moran P. General hospital admission rates in people diagnosed with personality disorder. Acta Psychiatr Scand. 2019;139(3):248–255. doi: 10.1111/acps.13004. [DOI] [PubMed] [Google Scholar]
- 28.Régie de l’assurance maladie du Québec. Rapport annuel de gestion, 2016-2017. Québec: Régie de l’assurance maladie du Québec; 2017.
- 29.Pampalon R, Hamel D, Gamache P, Raymond G. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29(4):178–191. [PubMed] [Google Scholar]
- 30.Low LL, Liu N, Wang S, Thumboo J, Ong MEH, Lee KH. Predicting frequent hospital admission risk in Singapore: a retrospective cohort study to investigate the impact of comorbidities, acute illness burden and social determinants of health. BMJ Open. 2016 14;6(10):e012705. [DOI] [PMC free article] [PubMed]
- 31.Roick C, Heider D, Kilian R, Angermeyer MC. Heavy users of inpatient psychiatric services. Psychiatr Prax. 2002;29(7):343–349. doi: 10.1055/s-2002-34657. [DOI] [PubMed] [Google Scholar]
- 32.Shafer A. Hospitalization patterns over 30 years across a statewide system of public mental health hospitals: readmission predictors, optimal follow-up period, readmission clusters and individuals with statistically significant high healthcare utilization. Psychiatr Q. 2019;90(2):263–273. doi: 10.1007/s11126-019-9626-7. [DOI] [PubMed] [Google Scholar]
- 33.Quan H, Sundarajan V, Halfon P, Fong A, Burnand B, Luthi J-C, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005:1130–9. [DOI] [PubMed]
- 34.Blais C, Jean S, Sirois C, Rochette L, Plante C, Larocque I, et al. Quebec integrated chronic disease surveillance system (QICDSS), an innovative approach. Chronic Dis Inj Can. 2014;34(4):226–235. [PubMed] [Google Scholar]
- 35.Penninx BWJH, Nolen WA, Lamers F, Zitman FG, Smit JH, Spinhoven P, et al. Two-year course of depressive and anxiety disorders: results from the Netherlands study of depression and anxiety (NESDA) J Affect Disord. 2011;133(1–2):76–85. doi: 10.1016/j.jad.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 36.Jääskeläinen E, Juola P, Hirvonen N, McGrath JJ, Saha S, Isohanni M, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39(6):1296–1306. doi: 10.1093/schbul/sbs130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fleury M-J, Djouini A, Huỳnh C, Tremblay J, Ferland F, Ménard J-M, et al. Remission from substance use disorders: a systematic review and meta-analysis. Drug Alcohol Depend. 2016;168:293–306. doi: 10.1016/j.drugalcdep.2016.08.625. [DOI] [PubMed] [Google Scholar]
- 38.Canadian Association of Emergency Physicians. Canadian Triage acuity scale [Internet]. 2012 [cited 2019 Apr 24]. Available from: https://caep.ca/wp-content/uploads/2017/06/module_I_slides_v2.5_2012.pdf.
- 39.Baraldi AN, Enders CK. An introduction to modern missing data analyses. J Sch Psychol. 2010;48(1):5–37. doi: 10.1016/j.jsp.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 40.Hibbert JD, Liese AD, Lawson A, Porter DE, Puett RC, Standiford D, et al. Evaluating geographic imputation approaches for zip code level data: an application to a study of pediatric diabetes. Int J Health Geogr. 2009;8(1):54. doi: 10.1186/1476-072X-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simo B, Caron J, Bamvita J-M, Grenier G, Fleury M-J. Predictors of number of healthcare professionals consulted by individuals with mental disorders or high psychological distress. Int J Environ Res Public Health. 2019;16(17):3010. doi: 10.3390/ijerph16173010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huynh C, Ferland F, Blanchette-Martin N, Ménard J-M, Fleury M-J. Factors influencing the frequency of emergency department utilization by individuals with substance use disorders. Psychiatr Q. 2016;87(4):713–728. doi: 10.1007/s11126-016-9422-6. [DOI] [PubMed] [Google Scholar]
- 43.McCusker J, Karp I, Cardin S, Durand P, Morin J. Determinants of emergency department visits by older adults: a systematic review. Acad Emerg Med. 2003;10(12):1362–1370. doi: 10.1111/j.1553-2712.2003.tb00011.x. [DOI] [PubMed] [Google Scholar]
- 44.Rieke K, McGeary C, Schmid KK, Watanabe-Galloway S. Risk factors for inpatient psychiatric readmission: are there gender differences? Community Ment Health J. 2016;52(6):675–682. doi: 10.1007/s10597-015-9921-1. [DOI] [PubMed] [Google Scholar]
- 45.Mark TL, Mark T, Tomic KS, Kowlessar N, Chu BC, Vandivort-Warren R, et al. Hospital readmission among medicaid patients with an index hospitalization for mental and/or substance use disorder. J Behav Health Serv Res. 2013;40(2):207–221. doi: 10.1007/s11414-013-9323-5. [DOI] [PubMed] [Google Scholar]
- 46.Paton F, Wright K, Ayre N, Dare C, Johnson S, Lloyd-Evans B, et al. Improving outcomes for people in mental health crisis: a rapid synthesis of the evidence for available models of care. Health Technol Assess [Internet]. 2016 Jan [cited 2020 Jun 21];20(3). Available from: https://openaccess.city.ac.uk/id/eprint/14163/. [DOI] [PMC free article] [PubMed]
- 47.Fleury M-J, Bamvita J-M, Grenier G, Schmitz N, Piat M, Tremblay J. Adequacy of help received by individuals with severe mental disorders after a major healthcare reform in Quebec: predictors and changes at 5-year follow-up. Adm Policy Ment Health Ment Health Serv Res. 2016;43(5):799–812. doi: 10.1007/s10488-015-0695-0. [DOI] [PubMed] [Google Scholar]
- 48.Fleury M, Grenier G. État de situation sur la santé mentale au Québec et réponse du système de santé et de services sociaux. Vol. 2, Rapport d’appréciation de la performance du système de santé et des services sociaux 2012. Commissaire à la Santé et Au Bien-Être; Québec: Gouvernement du Québec. 2012;.
- 49.Ng C-J, Liao P-J, Chang Y-C, Kuan J-T, Chen J-C, Hsu K-H. Predictive factors for hospitalization of nonurgent patients in the emergency department. Medicine (Baltimore) [Internet]. 2016 Jun [cited 2019 Sep 17];95(26). Available from: insights.ovid.com. [DOI] [PMC free article] [PubMed]
- 50.Ayangbayi T, Okunade A, Karakus M, Nianogo T. Characteristics of hospital emergency room visits for mental and substance use disorders. Psychiatr Serv Wash DC. 2017;68(4):408–410. doi: 10.1176/appi.ps.201600125. [DOI] [PubMed] [Google Scholar]
- 51.Nesper AC, Morris BA, Scher LM, Holmes JF. Effect of Decreasing County mental health services on the emergency department. Ann Emerg Med. 2016;67(4):525–530. doi: 10.1016/j.annemergmed.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 52.Fleury M-J, Bamvita J-M, Farand L, Aubé D, Fournier L, Lesage A. GP group profiles and involvement in mental health care. J Eval Clin Pract. 2012;18(2):396–403. doi: 10.1111/j.1365-2753.2010.01597.x. [DOI] [PubMed] [Google Scholar]
- 53.Williams JW, Gerrity M, Holsinger T, Dobscha S, Gaynes B, Dietrich A. Systematic review of multifaceted interventions to improve depression care. Gen Hosp Psychiatry. 2007;29(2):91–116. doi: 10.1016/j.genhosppsych.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 54.Marcus SC, Chuang C-C, Ng-Mak DS, Olfson M. Outpatient follow-up care and risk of hospital readmission in schizophrenia and bipolar disorder. Psychiatr Serv Wash DC. 2017;68(12):1239–1246. doi: 10.1176/appi.ps.201600498. [DOI] [PubMed] [Google Scholar]
- 55.Sfetcu R, Musat S, Haaramo P, Ciutan M, Scintee G, Vladescu C, et al. Overview of post-discharge predictors for psychiatric re-hospitalisations: a systematic review of the literature. BMC Psychiatry. 2017 24;17(1):227. [DOI] [PMC free article] [PubMed]
- 56.Ahmedani BK, Solberg LI, Copeland LA, Fang-Hollingsworth Y, Stewart C, Hu J, et al. Psychiatric comorbidity and 30-day readmissions after hospitalization for heart failure, AMI, and pneumonia. Psychiatr Serv. 2014;66(2):134–140. doi: 10.1176/appi.ps.201300518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pederson JL, Warkentin LM, Majumdar SR, McAlister FA. Depressive symptoms are associated with higher rates of readmission or mortality after medical hospitalization: a systematic review and meta-analysis. J Hosp Med. 2016;11(5):373–380. doi: 10.1002/jhm.2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stubbs B, Vancampfort D, Veronese N, Kahl KG, Mitchell AJ, Lin P-Y, et al. Depression and physical health multimorbidity: primary data and country-wide meta-analysis of population data from 190 593 people across 43 low- and middle-income countries. Psychol Med. 2017;47(12):2107–2117. doi: 10.1017/S0033291717000551. [DOI] [PubMed] [Google Scholar]
- 59.Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014;129(12):1350–1369. doi: 10.1161/CIR.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 60.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 61.Smith MW, Stocks C, Santora PB. Hospital readmission rates and emergency department visits for mental health and substance abuse conditions. Community Ment Health J. 2015;51(2):190–197. doi: 10.1007/s10597-014-9784-x. [DOI] [PubMed] [Google Scholar]
- 62.Clark BJ, Keniston A, Douglas IS, Beresford T, Macht M, Williams A, et al. Healthcare utilization in medical intensive care unit survivors with alcohol withdrawal. Alcohol Clin Exp Res. 2013;37(9):1536–1543. doi: 10.1111/acer.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Husain OM, Lynas PS, Totty JP, Williams K, Waring WS. Unplanned alcohol withdrawal: a survey of consecutive admissions to an acute medical unit in 2010 and 2011. QJM Mon J Assoc Physicians. 2013;106(1):43–49. doi: 10.1093/qjmed/hcs175. [DOI] [PubMed] [Google Scholar]
- 64.Yedlapati SH, Stewart SH. Predictors of alcohol withdrawal readmissions. Alcohol Alcohol Oxf Oxfs. 2018;53(4):448–452. doi: 10.1093/alcalc/agy024. [DOI] [PubMed] [Google Scholar]
- 65.Perlman CM, Hirdes JP, Vigod S. Psychiatric Rehospitalization: Development of a Person-Level Indicator for Care Planning and Quality Assurance. Prim Care Companion CNS Disord. 2015;17(4). [DOI] [PMC free article] [PubMed]
- 66.Tsoutsoulis K, Maxwell A. Menon Tarur Padinjareveettil a, Zivkovic F. Rogers JM Impact of inpatient mental health rehabilitation on psychiatric readmissions: a propensity score matched case control study J Ment Health Abingdon Engl. 2018;27:1–9. doi: 10.1080/09638237.2018.1466049. [DOI] [PubMed] [Google Scholar]
- 67.Han BH, Termine DJ, Moore AA, Sherman SE, Palamar JJ. Medical multimorbidity and drug use among adults in the United States. Prev Med Rep. 2018;12:214–219. doi: 10.1016/j.pmedr.2018.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Onyeka IN, Collier Høegh M, Nåheim Eien EM, Nwaru BI, Melle I. Comorbidity of physical disorders among patients with severe mental illness with and without substance use disorders: a systematic review and meta-analysis. J Dual Diagn. 2019;4:1–15. doi: 10.1080/15504263.2019.1619007. [DOI] [PubMed] [Google Scholar]
- 69.Fan Z, Wu Y, Shen J, Ji T, Zhan R. Schizophrenia and the risk of cardiovascular diseases: a meta-analysis of thirteen cohort studies. J Psychiatr Res. 2013;47(11):1549–1556. doi: 10.1016/j.jpsychires.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 70.Abou Kassm S, Hoertel N, Naja W, McMahon K, Barrière S, Blumenstock Y, et al. Metabolic syndrome among older adults with schizophrenia spectrum disorder: prevalence and associated factors in a multicenter study. Psychiatry Res. 2019;275:238–246. doi: 10.1016/j.psychres.2019.03.036. [DOI] [PubMed] [Google Scholar]
- 71.Li C, Birmaher B, Rooks B, Gill MK, Hower H, Axelson DA, et al. High prevalence of metabolic syndrome among adolescents and young adults with bipolar disorder. J Clin Psychiatry. 2019;30:80(4). doi: 10.4088/JCP.18m12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fezeu LK, Batty GD, Batty DG, Gale CR, Kivimaki M, Hercberg S, et al. Is the relationship between common mental disorder and adiposity bidirectional? Prospective analyses of a UK general population-based study. PLoS One. 2015;10(5):e0119970. doi: 10.1371/journal.pone.0119970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fuller BE, Rodriguez VL, Linke A, Sikirica M, Dirani R, Hauser P. Prevalence of liver disease in veterans with bipolar disorder or schizophrenia. Gen Hosp Psychiatry. 2011;33(3):232–237. doi: 10.1016/j.genhosppsych.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 74.Fleury M-J, Grenier G, Vallée C, Aubé D, Farand L, Bamvita J-M, et al. Implementation of the Quebec mental health reform (2005–2015) BMC Health Serv Res. 2016;16(1):586. doi: 10.1186/s12913-016-1832-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bodner E, Cohen-Fridel S, Mashiah M, Segal M, Grinshpoon A, Fischel T, et al. The attitudes of psychiatric hospital staff toward hospitalization and treatment of patients with borderline personality disorder. BMC Psychiatry. 2015;15:2. doi: 10.1186/s12888-014-0380-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int J Soc Psychiatry. 2015;61(6):539–549. doi: 10.1177/0020764014562051. [DOI] [PubMed] [Google Scholar]
- 77.Links PS, Ross J, Gunderson JG. Promoting good psychiatric Management for Patients with Borderline Personality Disorder. J Clin Psychol. 2015;71(8):753–763. doi: 10.1002/jclp.22203. [DOI] [PubMed] [Google Scholar]
- 78.Bateman AW, Gunderson J, Mulder R. Treatment of personality disorder. Lancet. 2015;385(9969):735–743. doi: 10.1016/S0140-6736(14)61394-5. [DOI] [PubMed] [Google Scholar]
- 79.Choi-Kain LW, Finch EF, Masland SR, Jenkins JA, Unruh BT. What works in the treatment of borderline personality disorder. Curr Behav Neurosci Rep. 2017;4(1):21–30. doi: 10.1007/s40473-017-0103-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bruneau J, Ahamad K, Goyer M-È, Poulin G, Selby P, Fischer B, et al. Management of opioid use disorders: a national clinical practice guideline. CMAJ. 2018;190(9):E247–E257. doi: 10.1503/cmaj.170958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Drake RE, Mueser KT, Brunette MF, McHugo GJ. A review of treatments for people with severe mental illnesses and co-occurring substance use disorders. Psychiatr Rehabil J. 2004;27(4):360–374. doi: 10.2975/27.2004.360.374. [DOI] [PubMed] [Google Scholar]
- 82.Presnall NJ, Wolf DAPS, Brown DS, Beeler-Stinn S, Grucza RA. A comparison of buprenorphine and psychosocial treatment outcomes in psychosocial and medical settings. J Subst Abus Treat. 2019;104:135–143. doi: 10.1016/j.jsat.2019.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Knapp M, Chisholm D, Leese M, Amaddeo F, Tansella M, Schene A, et al. Comparing patterns and costs of schizophrenia care in five European countries: the EPSILON study. Acta Psychiatr Scand. 2002;105(1):42–54. doi: 10.1034/j.1600-0447.2002._10310.x. [DOI] [PubMed] [Google Scholar]
- 84.Bertolote JM, Fleischmann A, De Leo D, Wasserman D. Psychiatric diagnoses and suicide: revisiting the evidence. Crisis. 2004;25(4):147–155. doi: 10.1027/0227-5910.25.4.147. [DOI] [PubMed] [Google Scholar]
- 85.Cavanagh JTO, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 86.Soomro GM, Kakhi S. Deliberate self-harm (and attempted suicide) BMJ Clin Evid. 2015;28:2015. [PMC free article] [PubMed] [Google Scholar]
- 87.Steeg S, Emsley R, Carr M, Cooper J, Kapur N. Routine hospital management of self-harm and risk of further self-harm: propensity score analysis using record-based cohort data. Psychol Med. 2018;48(2):315–326. doi: 10.1017/S0033291717001702. [DOI] [PubMed] [Google Scholar]
- 88.Fleury M-J, Rochette L, Grenier G, Huỳnh C, Vasiliadis H-M, Pelletier É, et al. Factors associated with emergency department use for mental health reasons among low, moderate and high users. Gen Hosp Psychiatry. 2019;60:111–119. doi: 10.1016/j.genhosppsych.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 89.Moses T. Determinants of mental illness stigma for adolescents discharged from psychiatric hospitalization. Soc Sci Med 1982. 2014 May;109:26–34. [DOI] [PubMed]
- 90.Sirotich F, Durbin A, Durbin J. Examining the need profiles of patients with multiple emergency department visits for mental health reasons: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2016;51(5):777–786. doi: 10.1007/s00127-016-1188-5. [DOI] [PubMed] [Google Scholar]
- 91.Ledoux Y, Minner P. Occasional and frequent repeaters in a psychiatric emergency room. Soc Psychiatry Psychiatr Epidemiol. 2006;41(2):115–121. doi: 10.1007/s00127-005-0010-6. [DOI] [PubMed] [Google Scholar]
- 92.Croudace TJ, Kayne R, Jones PB, Harrison GL. Non-linear relationship between an index of social deprivation, psychiatric admission prevalence and the incidence of psychosis. Psychol Med. 2000;30(1):177–185. doi: 10.1017/s0033291799001464. [DOI] [PubMed] [Google Scholar]
- 93.Moran V, Jacobs R, Mason A. Variations in performance of mental health providers in the English NHS: an analysis of the relationship between readmission rates and length-of-stay. Admin Pol Ment Health. 2017;44(2):188–200. doi: 10.1007/s10488-015-0711-4. [DOI] [PubMed] [Google Scholar]
- 94.Hamilton JE, Rhoades H, Galvez J, Allen M, Green C, Aller M, et al. Factors differentially associated with early readmission at a university teaching psychiatric hospital. J Eval Clin Pract. 2015;21(4):572–578. doi: 10.1111/jep.12335. [DOI] [PubMed] [Google Scholar]
- 95.Laliberté V, Stergiopoulos V, Jacob B, Kurdyak P. Homelessness at discharge and its impact on psychiatric readmission and physician follow-up: a population-based cohort study. Epidemiol Psychiatr Sci. 2019;7:1–8. doi: 10.1017/S2045796019000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chen J, Novak P, Barath D, Goldman H, Mortensen K. Local health departments’ promotion of mental health care and reductions in 30-day all-cause readmission rates in Maryland. Med Care. 2018;56(2):153–161. doi: 10.1097/MLR.0000000000000850. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.