Abstract
Background
Hypertension is one of the leading risk factors for cardiovascular diseases in India and Nepal. Socio-economic disparity in these two countries has created wide gap in management of hypertension. However, inequalities in prevalence and management (awareness, treatment, and control) of hypertension is poorly assessed. This study analyzes the risk factors associated with prevalence and management of hypertension in India and Nepal and assesses the wealth-and education-based inequalities in them.
Methods
This study used data from the Demographic and Health Survey; a cross-sectional survey conducted between January 2015 to December 2016 in India and June 2016 to January 2017 in Nepal. A total of 787,713 individuals in India and 14,454 individuals in Nepal aged between 15 and 49 years were included in the study. Respondents were classified as being hypertensive if their systolic blood pressure (SBP) readings were at least 140 mmHg or diastolic blood pressure (DBP) readings were at least 90 mmHg, or if they reported currently taking anti-hypertensive medication. Multilevel logistic regression models with random intercepts at household-and community-levels were used to identify the risk factors associated with prevalence and management of hypertension. For inequality assessment, slope index and relative index of inequalities in prevalence and management of hypertension were estimated.
Results
Overall prevalence of hypertension in India and Nepal were 11.4% (95% confidence interval (CI), 11.4–11.5) and 19.6% (95% CI, 18.9–20.2), respectively. Less than one-third of the hypertensive population received treatment and below 20% among them had their blood pressure controlled. In both countries, wealth-and education-based inequalities in awareness, treatment, and control of hypertension were significantly high in urban and rural areas.
Conclusion
Wealth- and education-based inequalities in prevalence and management of hypertension were high among different socio-economic groups at national and sub-national levels. Tailored strategies are required to effectively manage hypertension in different regions by considering socio-economic and demographic factors.
Keywords: Inequality in management of hypertension, Hypertension, Blood pressure, Non-communicable diseases
Background
Hypertension is one of the major global health risks for cardiovascular diseases (CVDs), kidney disease, and other complications [1, 2]. In 2017, CVDs caused 17.8 million deaths worldwide, accounting for 42% of total mortality due to non-communicable diseases (NCDs); 58% of them had complication of hypertension [3]. Accorinidng to WHO estimate in 2010, almost 1 billion people suffered due to raised blood pressure which was around 40% in low- and middle- income countries (LMICs) and 35% in high-income countires (HICs) [2, 4]. Thus, the Global Action Plan for the Prevention and Control of NCDs was adopted by the World Health Assembly in 2013, targeted to reduce the global prevalence of raised blood pressure (BP) by 25% by 2020 (relative to its 2010 level) [4]. However, despite the global efforts, some studies suggest that prevalence of hypertension among adults is predicted to increase from 26.4% in 2000 to 29.2% in 2025 [5].
Prevalence of hypertension and its related disease burden are notably increasing in most LMICs including southeast Asia, where it affected more than 35% of adults in 2013 [2]. As with other LMICs, hypertension is one of the leading risk factors for health loss including both premature deaths and disabilities in India and Nepal [6, 7]. In 2017, about 7.9 and 6.7% of total disability adjusted life years (DALYs) were attributed to high systolic blood pressure in India and Nepal, respectively with an upward trend since 1990 [8].
Early diagnosis and effective treatment of hypertension are key strategies to reduce disabilities and mortality related to CVDs and other chronic diseases [9, 10]. However, there are no studies that evaluates the availability and affordability of screening and treatment services for hypertension at subnational levels in India and Nepal. It is well known fact that inequality in access to health care services due to socio-demographic and economic factors leads to higher disparity in health outcome [11, 12]. Hence, prevailing health problems cannot be tackled effectively, if disparities in availability and accessibility of health care services are not thoroughly evaluated and intervened within the communities [13]. Therefore, measuring inequalities in prevalence, awareness, treatment, and control of hypertension at national and subnational levels is critical to understand the existing disparities in prevalence and management of hypertension within the communities. Further, this critical assessment will help to formulate tailored strategies and policies to effectively manage hypertension.
Few previous studies demonstrated the inequalities in prevalence and management of hypertension in LMICs [14, 15]. Nonetheless, these studies were mostly based on national-level estimates and did not measure inequalities at sub-national levels, which are more relevant to the needs of policy makers and administrators. Therefore, our study attempts to measure inequalities in prevalence and management of hypertension at national and sub-national levels and assess the risk factors associated with it using a nationally representative sample from Nepal and India.
Method
Sources of data
We used recently available data from the National Family Health Survey 2015–16 (NFHS-4) in India and Nepal Demographic and Health Survey 2015–16 (NDHS) in Nepal to analyze the risk factors and the inequalities in prevalence and management of hypertension. Both surveys were nationally representative population-based cross-sectional household surveys that included participants aged 15–49 years. Due to limited data availability population aged 50 years and above were not included in this study. However, inclusion of population aged 15–49 years emphasizes the burden of hypertension in younger age group in both countries. Data were collected from January 2015 to December 2016 in India and June 2016 to January 2017 in Nepal. NFHS-4 selected 616,346 occupied households and interviewed 601,509 households with response rate of 98.0%. NDHS interviewed 11,203 households out of 11,472 occupied households with response rate of 99.0%. Both surveys used multistage stratified cluster sampling design method to select sample. Out of total population of 1.3 billion in India [16], 687,230 women and 100,483 men aged 15–49 years were included in the study. In Nepal, out of total population of 29.3 million [17], 8488 women and 5966 men aged 15–49 years were included. Further details for data collection are provided in Supplementary Method 1&2, p68. Detailed methodology for each survey is available elsewhere [18, 19].
Outcome variables
Prevalence, awareness, treatment, and control of hypertension were the main outcome variables in this study. Respondents were classified as being hypertensive if their systolic blood pressure (SBP) readings were at least 140 mm Hg (mmHg) or diastolic blood pressure (DBP) readings were at least 90 mmHg, or if they reported currently taking anti-hypertensive medication [20]. SBP and DBP readings were measured three times within five-minute intervals. Management of hypertension includes awareness, treatment, and control of hypertension. Awareness of hypertension was defined as self-reported case of hypertension previously diagnosed by a doctor or other health professionals [20]. Treatment of hypertension was defined as self-reported use of prescribed antihypertensive medication [20], and control of hypertension was defined as receiving antihypertensive medication and having an average SBP below 140 mmHg or DBP below 90 mmHg [20]. All the measurements were taken by the trained field staffs using standardized blood pressure monitors. Details are provided in Supplementary Method 3 p73.
Covariates
We selected predictor variables for the analyses based on previous literatures on hypertension and its management [7, 21]. Covariates were stratified into three levels: individual-, household-, and community-levels. Individual-level variables included were; age, sex, educational status, body mass index (BMI), alcohol and tobacco consumption, and marital status. In both countries, participants aged 15–49 years of age were included in the study. Household-level variables included were availability of iodized salt and household wealth quintile. Community-level variables were region of residence, place of residence, and further stratified by province and states, respectively. Details of covariates are provided in Supplementary Method 3 p73.
Statistical analysis
We used descriptive statistics and frequency distributions to describe participants’ demographic and socio-economic characteristics. Prevalence, awareness, treatment, and control of hypertension were calculated by measuring proportion. To investigate the relationship between covariates and outcome variables, we employed multilevel logistic regression models with random intercept at household-and community-levels [22, 23]. Since NFHS-4 and NDHS used a multi-stage cluster sampling method (described above), the obtained data were nested in multiple categories (for example primary sampling units, states/provinces, and households). Thus, to account for the cluster level effect (within-cluster correlation), multilevel logistic regression was performed in this study [23]. Further, both descriptive and multilevel regression analyses were adjusted to complex survey design using sample weight.
To assess the inequalities in prevalence and management of hypertension, we estimated slope index of inequality (SII), relative index of inequality (RII), concentration index (CIX), and decomposition of concentration index at national and sub-national levels. Inequality analyses were performed based on household wealth index and education level. SII is a weighted measure of inequality that represents the absolute difference in estimated values of a health indicator between the most advantaged and disadvantaged, while taking into consideration all other subgroups using an appropriate regression model. Whereas, RII is a weighted measure of inequality that shows health gradient across multiple subgroups with natural ordering, on a relative scale. It is a ratio of estimated value of a health indicator in the most-advantaged to the most-disadvantaged (or vice-versa) while taking into consideration all other subgroups [24, 25]. Similarly, CIX is a measure of inequality in a health-related variable over distribution of another variable of interest such as household wealth quintile or education. CIX is defined in reference to the concentration curve (CC) which graphs the cumulative proportion of health-related variable against the cumulative proportion of the population ranked by variable of interest. It quantifies the degree of inequality in a specific health variable [9, 26–28]. Further, we decomposed concentration index to see the contribution of other socio-economic and demographic factors towards the concentration of prevalence and management of hypertension [26, 27, 29]. Detail of statistical analyses is provided in Supplementary Methods 4 p76. Statistical analyses were performed using Stata version 15.1/SE.
Results
Sample characteristics
Table 1 shows the sample characteristics of the selected population in India and Nepal. The overall prevalence of hypertension in India and Nepal was 11.4% (95% confidence interval [CI] 11.4–11.5) and 19.6% (18.9–20.2) respectively. Among the hypertensive population, 30.3% (30.0–30.6) in India and 40.0% (38.2–41.8) in Nepal were aware of their condition, 26.4% (26.2–26.7) and 20.2% (18.8–21.7), respectively, were receiving treatment. Only 17.8% (17.5–18.0) in India and 10.4% (9.3–11.6) in Nepal under the treatment had their blood pressure controlled. Detailed statistics are provided in Figs. 1, 2, 3, Supplementary Tables 1–2 p1, and Supplementary Figs. 1–10 p35.
Table 1.
Characteristics of selected participants in India and Nepal, 2016 (number, %)
| Characteristics | India | Nepal | ||
|---|---|---|---|---|
| Female | Male | Female | Male | |
| Sample size | 682,624 (88.6) | 99,217 (11.4) | 8435 (58.2) | 6059 (41.8) |
| Age group | ||||
| 15–24 | 238,367 (34.9) | 33,882 (34.1) | 2436 (28.9) | 1584 (16.1) |
| 25–34 | 206,687 (30.3) | 29,355 (29.6) | 1932 (22.9) | 1089 (18.0) |
| 35–44 | 165,034 (24.2) | 24,894 (25.1) | 1475 (17.5) | 1005 (16.6) |
| 45–49 | 72,536 (10.6) | 11,086 (11.2) | 522 (6.2) | 427 (7.05) |
| Above 49 | NA | NA | 2069 (24.5) | 1953 (32.2) |
| Educational status | ||||
| No formal education | 180,499 (26.5) | 11,098 (11.2) | 4009 (47.6) | 1449 (23.9) |
| Primary education | 91,600 (13.4) | 12,034 (12.2) | 1158 (13.7) | 1231 (20.3) |
| Secondary education | 324,407 (47.6) | 58,228 (58.8) | 2321 (27.5) | 2340 (38.7) |
| Higher education | 84,942 (12.5) | 17,628 (17.8) | 941 (1.2) | 1032 (17.1) |
| Marital status | ||||
| Never married | 153,692 (22.5) | 37,212 (37.5) | 1339 (15.9) | 1369 (22.6) |
| Married | 500,911 (73.4) | 60,785 (61.3) | 6241 (74.0) | 4387 (72.4) |
| Widowed | 20,813 (3.1) | 583 (0.6) | 767 (9.1) | 260 (4.3) |
| Divorced | 2200 (0.3) | 239 (0.2) | 85 (1.0) | 42 (0.7) |
| Not Living together | 4966 (0.7) | 393 (0.4) | NA | NA |
| Tobacco consumption | ||||
| No | 635,761 (93.1) | 54,645 (55.1) | 8148 (96.6) | 4896 (80.8) |
| Yes | 46,862 (6.9) | 44,574 (44.9) | 287 (3.4) | 1163 (19.2) |
| Alcohol consumption | ||||
| No | 73,279 (98.0) | 70,020 (70.6) | 8383 (99.4) | 5903 (97.4) |
| Yes | 1515 (2.0) | 29,197 (29.4) | 52 (0.6) | 155 (2.6) |
| Body mass index | ||||
| Underweight | 152,918 (22.4) | 19,992 (20.2) | 1577 (18.8) | 1079 (17.9) |
| Normal | 389,263 (57.1) | 60,231 (60.8) | 4987 (59.3) | 3939 (65.5) |
| Overweight | 104,808 (15.4) | 15,717 (15.9) | 1420 (16.9) | 869 (14.4) |
| Obese | 34,915 (5.1) | 3108 (3.1) | 415 (4.9) | 130 (2.2) |
| Wealth quintile | ||||
| Q1 (Poorest) | 122,110 (17.9) | 14,809 (14.9) | 1535 (18.2) | 1028 (17.0) |
| Q2 | 134,859 (19.8) | 18,896 (19.1) | 1758 (20.8) | 1208 (20.0) |
| Q3 | 141,047 (20.7) | 21,209 (21.4) | 1831 (21.7) | 1291 (21.3) |
| Q4 | 143,992 (21.1) | 21,870 (22.0) | 1608 (19.1) | 1213 (20.0) |
| Q5 (Richest) | 140,614 (20.6) | 22,431 (22.6) | 1704 (20.2) | 1316 (21.7) |
| Availability of iodine | ||||
| Iodine present | 636,778 (93.4) | 93,097 (93.9) | 7970 (94.6) | 5737 (94.8) |
| No iodine | 43,783 (6.4) | 5703 (5.8) | 409 (4.9) | 272 (4.5) |
| No salt in house | 1392 (0.2) | 318 (0.3) | 49 (0.6) | 43 (0.7) |
| Place of residence | ||||
| Urban | 232,326 (34.0) | 37,053 (37.4) | 5153 (61.1) | 3740 (61.7) |
| Rural | 450,297 (66.0) | 62,163 (62.7) | 3281 (38.9) | 2318 (38.3) |
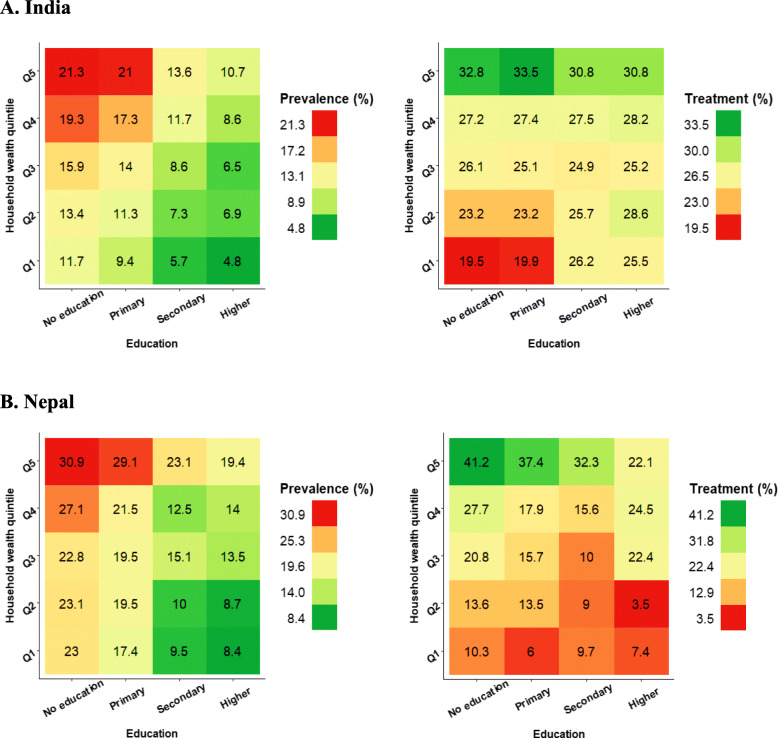
Fig. 1.
Prevalence and treatment of hypertension by household wealth quintile and education in India and Nepal, 2016. * Q1 = Poorest quintile, Q5 = Richest quintile * All the figures were generated in R programming software
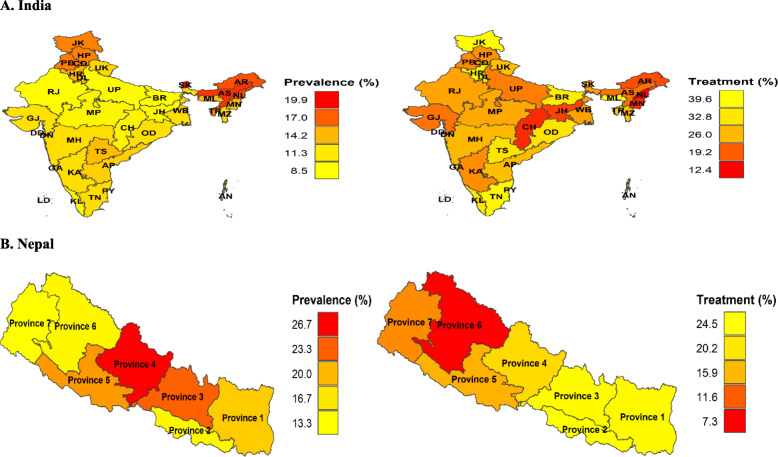
Fig. 2.
Prevalence and treatment of hypertension at subnational levels in India and Nepal, 2016. AN, Andaman and Nicobar Island; AP, Andhra Pradesh; AR, Arunachal Pradesh; AS, Assam; BR, Bihar; CD, Chandigarh; CH, Chhattisgarh; DN, Dadra and Nagar Haveli; DD, Daman and Diu; GA, Goa; GJ, Gujarat; HR, Haryana; HP, Himachal Pradesh; JK, Jammu & Kashmir; JH, Jharkhand; KA, Karnataka; KL, Kerala; LD, Lakshadweep; MP, Madhya Pradesh; MH, Maharashtra; MN, Manipur; ML, Meghalaya; MZ, Mizoram; NL, Nagaland; DL, New Delhi; OD, Odisha; PY, Puducherry; PB, Punjab; RJ, Rajasthan; SK, Sikkim; TN, Tamil Nadu; TR, Tripura; UP, Uttar Pradesh; UK, Uttarakhand; WB, West Bengal; TS, Telangana * All the choropleth maps were generated in R programming software using spatial data from the DHS Spatial Data Repository. Permission to reproduce the map was obtained from DHS Program
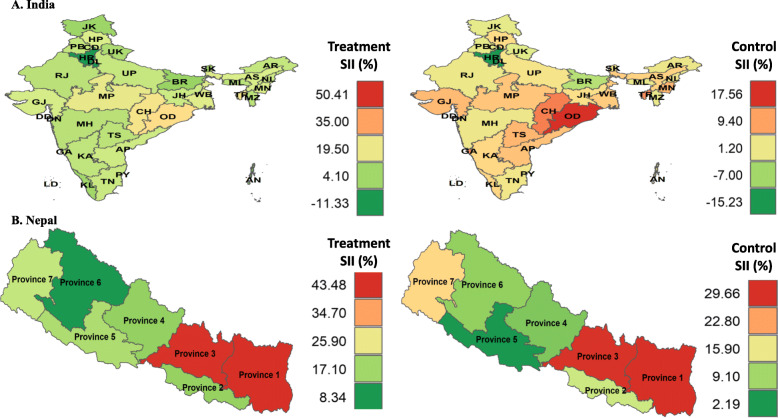
Fig. 3.
Wealth-based SII in treatment and control of hypertension in India and Nepal, 2016. *SII = slope index of inequality; AN, Andaman and Nicobar Island; AP, Andhra Pradesh; AR, Arunachal Pradesh; AS, Assam; BR, Bihar; CD, Chandigarh; CH, Chhattisgarh; DN, Dadra and Nagar Haveli; DD, Daman and Diu; GA, Goa; GJ, Gujarat; HR, Haryana; HP, Himachal Pradesh; JK, Jammu & Kashmir; JH, Jharkhand; KA, Karnataka; KL, Kerala; LD, Lakshadweep; MP, Madhya Pradesh; MH, Maharashtra; MN, Manipur; ML, Meghalaya; MZ, Mizoram; NL, Nagaland; DL, New Delhi; OD, Odisha; PY, Puducherry; PB, Punjab; RJ, Rajasthan; SK, Sikkim; TN, Tamil Nadu; TR, Tripura; UP, Uttar Pradesh; UK, Uttarakhand; WB, West Bengal; TS, Telangana; * All the choropleth maps were generated in R programming software using spatial data from the DHS Spatial Data Repository. Permission to reproduce the map was obtained from DHS Program.
Factors associated with prevalence and management of hypertension
Supplementary Table 3 and Supplementary Table 4 shows the risk factors associated with prevalence, awareness, treatment, and control of hypertension in India and Nepal. After adjusting for covariates, the odds of being hypertensive was higher in men compared to women in both countries (Odds ratio [OR] 1.47, 95% CI, 1.41–1.52 for India and 1.96 (1.59–2.44) for Nepal). However, the odds for awareness, treatment, and control were lower in men compared to women in both countries. In India, the odds of being hypertensive in the wealthy and poorest population were similar, however in case of Nepal these results were not statistically significant. But, the OR for treatment of hypertension were 1.58 (1.41–1.77) and 7.86 (1.92–32.11) and for control were 1.30 (1.14–1.48) and 9.48 (1.11–80.81) in the richest quintile in reference to the poorest quintile in India and Nepal, respectively. In both countries, urban residents had higher odds of being aware and having treatment. In India, odds of having the blood pressure controlled was higher in urban residents compared to the rural residents, however in Nepal this result was not statistically significant.
Wealth-based inequality in prevalence and management of hypertension
Table 2 provides the summary results of wealth-based inequality in prevalence and management of hypertension in India and Nepal. Prevalence of hypertension was 5.2 (95% CI 4.7–5.7) and 7.1 (2.9–11.4) percentage points higher in affluent populations compared to the disadvantaged ones in India and Nepal. Similarly, inequalities in awareness, treatment, and control were substantially high and concentrated towards the wealthy populations in both countries (Fig. 3). Both in urban and rural residences in India, affluent groups had higher percentage points of hypertension prevalence, awareness, treatment, and control than the disadvantaged groups. Unlike in India, absolute inequalities in prevalence, treatment, and control in Nepal were higher in urban residence compared to rural. Wealthy urban population in Nepal had higher prevalence, awareness, treatment, and control than the poorer and poorest population. However, in rural residence, poorest population had higher prevalence of hypertension than the affluent ones.
Table 2.
Wealth based inequalities in prevalence and management of hypertension in India and Nepal, 2016
| Categorization | Mean | SII (95% CI) | RII (95% CI) | CIX*100 (95% CI) | |
|---|---|---|---|---|---|
| Q1 (95% CI) | Q5 (95% CI) | ||||
| India | |||||
| Prevalence (national) | 9.4 (9.3–9.6) | 13.4 (13.2–13.5) | 5.22 (4.77–5.67) | 1.53 (1.48–1.59) | 7.28 (6.75–7.81) |
| Urban | 10.4 (9.7–11.1) | 13.1 (13.0–13.3) | 2.63 (1.74–3.52) | 1.22 (1.14–1.30) | 3.79 (2.71–4.88) |
| Rural | 9.4 (9.2–9.5) | 14.0 (13.7–14.3) | 4.71 (4.27–5.15) | 1.50 (1.45–1.56) | 6.21 (5.67–6.75) |
| Awareness (national) | 19.2 (18.5–19.9) | 37.7 (37.0–38.3) | 20.25 (18.47–22.03) | 1.95 (1.84–2.07) | 11.91 (11.08–12.74) |
| Urban | 19.1 (16.2–21.9) | 37.9 (37.1–38.6) | 12.20 (8.77–15.64) | 1.42 (1.28–1.56) | 8.43 (6.73–10.12) |
| Rural | 19.2 (18.5–19.9) | 37.1 (35.9–38.3) | 18.82 (16.90–20.75) | 1.98 (1.84–2.12) | 10.48 (9.62–11.34) |
| Treatment (national) | 20.8 (20.1–21.5) | 31.2 (30.6–31.8) | 11.68 (10.01–13.35) | 1.55 (1.45–1.64) | 7.25 (6.33–8.18) |
| Urban | 18.0 (15.2–20.7) | 31.9 (31.2–32.6) | 11.24 (8.08–14.40) | 1.47 (1.31–1.63) | 6.29 (4.47–8.12) |
| Rural | 21.0 (20.3–21.7) | 29.5 (28.3–30.6) | 8.88 (7.02–10.74) | 1.42 (1.32–1.52) | 5.37 (4.41–6.34) |
| Control (national) | 16.0 (15.4–16.7) | 19.9 (19.4–20.4) | 6.24 (3.39–9.08) | 1.39 (1.18–1.59) | 3.53 (2.32–4.74) |
| Urban | 14.8 (13.4–16.2) | 18.0 (16.3–19.7) | 1.56 (−16.60–19.72) | 1.09 (0.00–2.18) | 4.73 (2.42–7.04) |
| Rural | 19.6 (18.1–21.1) | 17.8 (17.1–18.5) | 6.80 (−1.05–14.65) | 1.47 (0.82–2.12) | 1.92 (0.65–3.18) |
| Nepal | |||||
| Prevalence (national) | 26.8 (22.8–30.9) | 51.7 (48.1–55.4) | 28.92 (21.27–36.57) | 2.10 (1.67–2.52) | 11.44 (8.48–14.40) |
| Urban | 30.7 (25.4–36.0) | 54.1 (49.8–58.4) | 28.14 (18.12–38.15) | 1.97 (1.48–2.45) | 11.631 (7.87–15.39) |
| Rural | 20.3 (14.3–26.4) | 46.3 (39.7–52.9) | 28.91 (17.27–40.56) | 2.32 (1.51–3.12) | 12.037 (7.51–16.57) |
| Awareness (national) | 9.3 (6.7–12.0) | 33.1 (29.7–36.5) | 30.24 (23.39–37.08) | 4.57 (3.00–6.13) | 23.29 (18.41–28.17) |
| Urban | 12.3 (8.5–16.0) | 35.4 (31.3–39.5) | 30.28 (21.25–39.32) | 3.86 (2.28–5.43) | 23.40 (16.94–29.85) |
| Rural | 4.5 (1.4–7.5) | 27.8 (21.9–33.7) | 27.09 (16.97–37.21) | 5.79 (2.29–9.28) | 21.09 (14.21–27.97) |
| Treatment (national) | 4.2 (2.4–6.0) | 17.7 (14.9–20.5) | 18.32 (12.96–23.69) | 5.33 (2.96–7.70) | 27.41 (19.89–34.93) |
| Urban | 4.7 (2.2–7.1) | 19.5 (16.1–22.9) | 20.01 (13.17–26.85) | 5.27 (2.45–8.09) | 29.86 (19.87–39.85) |
| Rural | 3.4 (0.7–6.1) | 13.5 (9.0–18.0) | 13.97 (5.51–22.44) | 4.81 (1.03–8.60) | 19.90 (9.88–29.92) |
| Control (national) | 14.3 (14.1–14.5) | 9.4 (9.2–9.6) | −6.96 (−7.39– −6.52) | 0.57 (0.54–0.59) | −9.26 (−9.78– −8.74) |
| Urban | 17.3 (16.9–17.7) | 10.1 (9.9–10.4) | −8.56 (−9.50– −7.62) | 0.53 (0.49–0.56) | −10.30 (−11.41– −9.19) |
| Rural | 13.6 (13.4–13.7) | 8.3 (8.0–8.6) | −7.73 (− 8.17– − 7.29) | 0.51 (0.49–0.53) | − 10.70 (− 11.24– −10.16) |
At sub-national levels, India’s North region had highest wealth-based absolute inequality in prevalence of hypertension, where hypertension was more prevalent in richer and richest population than their poorer counterparts. The Northeast and Central part of India had highest absolute inequalities in awareness and treatment. Wealth-based inequality in control of hypertension was highest in the South and Northeast regions. (Fig. 3 and Supplementary Table 8 p18). In Nepal, compared to other provinces, Province 3 had substantially high wealth-based inequalities in prevalence 19.4% (95% CI 9.1–29.9), awareness 43.4% (26.1–60.8), treatment 43.4% (27.7–59.1), and control 29.6% (15.9–43.2) of hypertension followed by Province 6 and 7. Absolute inequalities in prevalence and management of hypertension at sub-national levels were significantly higher in Nepal compared to India. Details are provided in Fig. 3, Supplementary Tables 5–12 p11, and Supplementary Fig. 11,12,15 p45 & 17–24 p51).
Education-based inequality in prevalence and management of hypertension
Prevalence of hypertension in India and Nepal was higher among the population with no formal education than their higher educated counterparts. However, awareness, treatment, and control were higher in educated populations than the uneducated ones in India. In Nepal, awareness and treatment were concentrated in the uneducated population (Supplementary Tables 13–20 p23 and Supplementary Figs. 13–15 p47 & 25–32 p57).
Figure 1 shows the concentration indices for prevalence, awareness, treatment, and control of hypertension in India and Nepal, decomposed by age group, household wealth quintile, body mass index, and education. In both countries, BMI was the major factor that accounted for the pro-rich concentration in prevalence of hypertension. Education didn’t show notable contribution towards the pro-rich concentration in treatment and control of hypertension in both countries.
Discussion
This study provides a concrete evidence regarding wealth-and education-based inequalities in prevalence and management of hypertension at national and subnational levelsin young adults aged 15–49 years, in India and Nepal. It shows that wealth-and education-based inequalities in prevalence and management of hypertension especially treatment and control were significantly high and varied among different regions in India and Nepal.
In this study we found around 11% percent of the young adults aged 15–49 years in India, and almost 20% of young adults in Nepal were hypertensive. More than half of the hypertensive population were unaware of their conditions and almost two-thirds did not receive treatment. Above 80% of the hypertensive population had uncontrolled blood pressure in both countries. These findings were consistent with previous studies [7, 30, 31]. The risk factor analysis showed that the odds of being hypertensive in men were significantly higher than women in both countries. In contrary, odds of being treated and having their blood pressure controlled in women were twice as high as compared to men. A plausible reason includes higher health seeking behavior in women [32, 33]. Odds of being hypertensive, were notably higher among urban residents compared to rural residents. This could be because of unplanned urbanization, environmental factors such as air pollution, high disparities in living standards, and other behavioral risk factors [34, 35]. In both counties, adults aged between 35 and 49 years, with higher BMI had approximately four times higher odds of being hypertensive and were two times less likely to have their blood pressure controlled compared to individuals with normal BMI. The reasons could be low physical activity, long work hours, and sedentary lifestyle [36–38].
Wide regional variability existed in prevalence, awareness, treatment, and control of hypertension in both countries. For instance, some regions in India with disproportionately high prevalence such as the Northeast region, had significantly low awareness, treatment, and control. One of the probable reasons for high prevalence in this region could be unhealthy lifestyles and dietary pattern [38]. Further, low awareness, treatment, and control of hypertension could be due to inadequate knowledge among people about the risk factors of NCDs [39, 40], unaffordable anti-hypertensive medication or lack of treatment services, and distant heath care centers [41]. It was important to note that in both countries, the regions with low prevalence of hypertension, also had low proportion of awareness, treatment, and control which indicates high burden in these regions. Thus, it signifies along with prevalence estimate, estimates for awareness, treatment, and control are important to understand the overall burden of hypertension and ensure effective policy formulation and implementation.
Wealth-and education-based inequalities in awareness, treatment, and control in India and Nepal were remarkably high across all the regions and were highly concentrated in the affluent population. Importantly, wealth-based inequalities in treatment and control were three times higher in Nepal compared to India. This could be due to high disparity in income distribution within different provinces of Nepal [16, 42]. In both countries, some regions for example, East region in India and Province 3 in Nepal had higher levels of awareness, treatment, and control demonstrating better scenarios in hypertension management. However, wealth-and education-based inequality estimates showed that the awareness, treatment, and control of hypertension varied among the subgroups with high concentration towards wealthy and educated population. These results imply the poorest and disadvantaged population were still suffering from high burden of hypertension. Thus, inequality estimates at sub-national levels provided important insight to understand the actual burden of hypertension in different regions and subgroups.
High disparity in prevalence, awareness, treatment, and control of hypertension among different regions entails the importance of thorough intervention at regional levels to tackle the existing problem. Thorough implementation of prevention and treatment strategies recommended by World Health Organization (WHO), the International Society of Hypertension (ISH) and Centers for Disease Control and Prevention (CDC) could be helpful to manage the burden of hypertension [43]. Building better healthcare infrastructure, improving standardized treatment services, and using modern technology such as mobile health applications could help to increase awareness, treatment, and control of hypertension [44, 45].
At present, the governments in both countries are struggling to mitigate the challenges of communicable diseases [46, 47]. The increased risk of hypertension creates a havoc for policy makers and governmental bodies to manage the double burden of diseases. Hence, prioritizing prevention and management of hypertension as a national agenda and thoroughly monitoring the progress at regional level would be urgently needed.
There are several studies conducted to estimate burden of hypertension in low-and middle-income countries including South Asian countries. These studies have shown that the burden of hypertension in low-and middle-income countries is high, particularly in south Asian countries [2, 48]. Most of these studies suggest that hypertension is mostly prevalent in wealthy people. Some studies suggest that in the south Asian countries, burden of hypertension particularly in India and Nepal are in increasing trend with increasing urbanization and sedentary lifestyle [21, 31]. Several studies have estimated the prevalence of hypertension and its management in both countries [7, 31], but none of these studies performed inequality assessment at national and sub-national levels. Therefore, this study provides detailed information on existing inequalities in prevalence and management of hypertension in these two neighboring countries that share similar lifestyle, culture, and religions, yet with differences in demographic and socio-economic characteristics. This study has a few limitations. Firstly, we excluded population aged 49 years and above due to missing data. Hence, this study may not be generalized to population aged 50 years and above. However, this study emphasizes the increasing burden of hypertension in younger adults which is a major issue in many high-income countries [49, 50]. Secondly, this is a cross-sectional study therefore a causal relationship cannot be necessarily established between the covariates and outcomes. Lastly, there could be possibilities of misreporting because of single-day measurements. However, SBP and DBP were measured three times to minimize the possibility of misreporting.
Conclusion
Our study showed that India and Nepal had high inequalities in prevalence and management of hypertension at national and sub-national levels. There was wide gap in awareness, treatment, and control of hypertension among different subgroups within a region. Hence, for effective management of hypertension, tailored strategies are required for specific regions by considering several socio-economic and demographic factors such as socio-economic status, education level, and BMI. More efforts should be put towards awareness campaigns taking SES inequality into consideration. Community-based behavioral interventions such as change in dietary pattern, increase in physical activity, and routine health checkups should be encouraged to manage hypertension in both countries. Effective screening and treatment services should be made easily available and affordable for everyone regardless of their SES. In addition, involvement of the private sector should be encouraged for the sustainable management of hypertension. Further studies are needed to explore the inequality issues and its major factors and the association of hypertension with other comorbidities such as diabetes in India and Nepal.
Supplementary information
Acknowledgements
We thank Peter Ueda and Mr. Md. Rashid Rahman for giving us utmost assistance and valuable suggestions.
Abbreviations
- BP
Blood Pressure
- BMI
Body Mass Index
- CBS
Central Bureau of Statistics
- CC
Concentration Curve
- CDC
Centers for Disease Control and Prevention
- CEBs
Census Enumeration Blocks
- CI
Confidence Interval
- CIX
Concentration Index
- CVDs
Cardiovascular Diseases
- DALYs
Disabilities Adjusted Life Years
- DBP
Diastolic Blood Pressure
- GDP
Gross Domestic Product
- EAs
Enumeration Areas
- HICs
High Income Countries
- ISH
International Society of Hypertension
- LIC
Low Income Countries
- LMICs
Low-and Middle-Income Countries
- MoHFW
Ministry of Health and Family Welfare
- MLM
Multi-level model
- NCDs
Non–communicable Diseases
- NDHS
Nepal Demographic and Health Surveys
- NFHS
National Family Health Survey
- NPHC
National Population and Housing Census
- OOP
Out-of-Pocket
- OR
Odds Ratio
- PSU
Primary Sampling Unit
- RII
Relative Index of Inequality
- SBP
Systolic Blood Pressure
- SDG
Sustainable Development Goals
- SES
Socio-Economic Status
- SII
Slope Index of Inequality
- UHC
Universal Health Coverage
- UN
United Nations
- WB
World Bank
- WHO
World Health Organization
Authors’ contributions
All authors were responsible for the study concept and design. SKR acquired the data. SKR, SR, SN and SKA analyzed and interpreted the data. SKR and MR conducted statistical analysis and drafted the article. KS, SN,MR made critical revision of the manuscript for important intellectual content and gave final approval for the manuscript.
Funding
None.
Availability of data and materials
The datasets analyzed during the study are available in the Demographic and Health Surveys, DHS repository, https://dhsprogram.com/Data/
Ethics approval and consent to participate
Ethical approval certificates were obtained by The Demographic and Health Surveys (DHS).
Ethical Approval for India and Nepal was obtained from Institutional Review Board, ICF International.
India ICF Project Number: 631561.0.000.00.071.01.
Nepal ICF Project Number: 132989.0.000.NP.DHS.01.
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interests exist.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12889-020-09450-6.
References
- 1.Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, Alexander L, Estep K, Hassen Abate K, Akinyemiju TF, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm hg, 1990-2015. JAMA. 2017;317(2):165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 2.A global brief on hypertension [https://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/].
- 3.Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global action plan for the prevention and control of NCDs 2013–2020 [ https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1].
- 5.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farag YMM, Bharati V, Keithi-Reddy SR, Acharya VN, Almeida AF, Anil C, Ballal HS, Gaccione P, Issacs R, Jasuja S. Burden and predictors of hypertension in India: results of SEEK (screening and early evaluation of kidney disease) study. BMC Nephrol. 2014;15(1):42. doi: 10.1186/1471-2369-15-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehata SS N, Mehta R, Vaidya A, Rawal LB, Bhattarai N, Mishra SR. Prevalence, awareness, treatment and control of hypertension in Nepal: data from nationally representative population-based cross-sectional study. J Hypertens. 2018. [DOI] [PubMed]
- 8.Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saito E, Gilmour S, Yoneoka D, Gautam GS, Rahman MM, Shrestha PK, Shibuya K. Inequality and inequity in healthcare utilization in urban Nepal: a cross-sectional observational study. Health Policy Plan. 2016;31(7):817–824. doi: 10.1093/heapol/czv137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 11.Grintsova O, Maier W, Mielck A. Inequalities in health care among patients with type 2 diabetes by individual socio-economic status (SES) and regional deprivation: a systematic literature review. Int J Equity Health. 2014;13(1):43. doi: 10.1186/1475-9276-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Z, Yue X, Wang H, Bao C, Xu W, Chen L, Qi X. Relation of socioeconomic status to hypertension occurrence. Int J Cardiol. 2014;173(3):544–545. doi: 10.1016/j.ijcard.2014.03.082. [DOI] [PubMed] [Google Scholar]
- 13.Niessen LW, Mohan D, Akuoku JK, Mirelman AJ, Ahmed S, Koehlmoos TP, Trujillo A, Khan J, Peters DH. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018. [DOI] [PubMed]
- 14.Almeida G, Sarti FM. Measuring evolution of income-related inequalities in health and health care utilization in selected Latin American and Caribbean countries. Rev Panam Salud Publica. 2013;33(2):83–89. doi: 10.1590/s1020-49892013000200002. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2014;43(1):116–128. doi: 10.1093/ije/dyt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The World Bank Open Data, India, [https://data.worldbank.org/country/India,].
- 17.The World Bank Open Data, Nepal, [https://data.worldbank.org/country/nepal].
- 18.International Institute for Population Science . In: National Family Health Survey (NFHS-4), 2015-2016. Mumbai IIPSI, editor. 2017. [Google Scholar]
- 19.Ministry of Health: Nepal Demographic and Health Survey 2016. In. Edited by Nepal MoH. Kathmandu, Nepal: New ERA and ICF; 2017.
- 20.World Health Organization International Society of Hypertension Writing Group: 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21(11):1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Rahman MM, Gilmour S, Akter S, Abe SK, Saito E, Shibuya K. Prevalence and control of hypertension in Bangladesh: a multilevel analysis of a nationwide population-based survey. J Hypertens. 2015;33(3):465–472. doi: 10.1097/HJH.0000000000000421. [DOI] [PubMed] [Google Scholar]
- 22.Goldstein H, Browne W, Rasbash J. Multilevel modelling of medical data. Stat Med. 2002;21(21):3291–3315. doi: 10.1002/sim.1264. [DOI] [PubMed] [Google Scholar]
- 23.Heck RH, Thomas SL. An introduction to multilevel Modelling techniques. 3. New York: Routledge; 2015. [Google Scholar]
- 24.Schneider MC, Castillo-Salgado C, Bacallao J, Loyola E, Mujica OJ, Vidaurre M, Roca A. Methods for measuring inequalities in health. Revista panamericana de salud publica = Pan Am J Public Health. 2002;12(6):398–414. doi: 10.1590/s1020-49892002001200006. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization . Health Equity Assessment Toolkit (HEAT): software for exploring and comparing health inequalities in countries. Geneva: World Health Organization; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Donnell O, Doorslaer EV, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation. Washington DC: The World Bank; 2008. [Google Scholar]
- 27.Tao Y, Henry K, Zou Q, Zhong X. Methods for measuring horizontal equity in health resource allocation: a comparative study. Heal Econ Rev. 2014;4(1):10. doi: 10.1186/s13561-014-0010-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Costa-Font J, Hernandez-Quevedo C. Measuring inequalities in health: what do we know? What do we need to know? Health Policy. 2012;106(2):195–206. doi: 10.1016/j.healthpol.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 29.Heckley G, Gerdtham UG, Kjellsson G. A general method for decomposing the causes of socioeconomic inequality in health. J Health Econ. 2016;48:89–106. doi: 10.1016/j.jhealeco.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 30.N. K ARK, Pant H, Khan H, Franco OH, Di Angelantonio E, Prabhakaran D. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geldsetzer PM-GJ, Theilmann M, Davies JI, Awasthi A, Vollmer S, Jaacks LM, Barnighausen T, Atun R. Diabetes and hypertension in India: A nationally representative study of 1.3 million adults. JAMA Intern Med. 2018;178(3):363–372. doi: 10.1001/jamainternmed.2017.8094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49(2):147–152. [PubMed] [Google Scholar]
- 33.Fikree FF, Pasha O. Role of gender in health disparity: the south Asian context. BMJ. 2004;328(7443):823–826. doi: 10.1136/bmj.328.7443.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sanidas E, Papadopoulos DP, Grassos H, Velliou M, Tsioufis K, Barbetseas J, Papademetriou V. Air pollution and arterial hypertension. A new risk factor is in the air. J Am Soc Hypertens. 2017;11(11):709–715. doi: 10.1016/j.jash.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Gupta R, Kaur M, Islam S, Mohan V, Mony P, Kumar R, Kutty VR, Iqbal R, Rahman O, Deepa M, et al. Association of Household Wealth Index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am J Hypertens. 2017;30(4):373–381. doi: 10.1093/ajh/hpw169. [DOI] [PubMed] [Google Scholar]
- 36.Chandra A, Neeland IJ, Berry JD, Ayers CR, Rohatgi A, Das SR, Khera A, McGuire DK, de Lemos JA, Turer AT. The relationship of body mass and fat distribution with incident hypertension. Observations Dallas Heart Study. 2014;64(10):997–1002. doi: 10.1016/j.jacc.2014.05.057. [DOI] [PubMed] [Google Scholar]
- 37.Dua S, Bhuker M, Sharma P, Dhall M, Kapoor S. Body mass index relates to blood pressure among adults. N Am J Med Sci. 2014;6(2):89–95. doi: 10.4103/1947-2714.127751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Imamura F, Micha R, Khatibzadeh S, Fahimi S, Shi P, Powles J, Mozaffarian D. Nutrition GBoD, group CDE: dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob Health. 2015;3(3):e132–e142. doi: 10.1016/S2214-109X(14)70381-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vaidya A, Aryal UR, Krettek A. Cardiovascular health knowledge, attitude and practice/behaviour in an urbanising community of Nepal: a population-based cross-sectional study from Jhaukhel-Duwakot health demographic surveillance site. BMJ Open. 2013;3(10):e002976. doi: 10.1136/bmjopen-2013-002976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Choudhary R, Sharma SM, Kumari V, Gautam D. Awareness, treatment adherence and risk predictors of uncontrolled hypertension at a tertiary care teaching hospital in Western India. Indian Heart J. 2016;68(Suppl 2):S251. doi: 10.1016/j.ihj.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, Bahonar A, Chifamba J, Dagenais G, Diaz R, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 42.Ministry of Finance, Government of Nepal . Economic Survey 2017/18. Singh Durbar: MOF; 2018. [Google Scholar]
- 43.Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, Damasceno A, Delles C, Gimenez-Roqueplo A-P, Hering D. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the lancet commission on hypertension. Lancet. 2016;388(10060):2665–2712. doi: 10.1016/S0140-6736(16)31134-5. [DOI] [PubMed] [Google Scholar]
- 44.Vedanthan R, Bernabe-Ortiz A, Herasme OI, Joshi R, Lopez-Jaramillo P, Thrift AG, Webster J, Webster R, Yeates K, Gyamfi J, et al. Innovative approaches to hypertension control in low- and middle-income countries. Cardiol Clin. 2017;35(1):99–115. doi: 10.1016/j.ccl.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Piette JD, Datwani H, Gaudioso S, Foster SM, Westphal J, Perry W, Rodríguez-Saldaña J, Mendoza-Avelares MO, Marinec N. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed J E Health. 2012;18(8):613–620. doi: 10.1089/tmj.2011.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swe KT, Rahman MM, Rahman MS, Saito E, Abe SK, Gilmour S, Shibuya K. Cost and economic burden of illness over 15 years in Nepal: A comparative analysis. PLoS One. 2018;13(4):e0194564. doi: 10.1371/journal.pone.0194564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mills A. Health care systems in low- and middle-income countries. N Engl J Med. 2014;370(6):552–557. doi: 10.1056/NEJMra1110897. [DOI] [PubMed] [Google Scholar]
- 48.Irazola VE, Gutierrez L, Bloomfield G, Carrillo-Larco RM, Dorairaj P, Gaziano T, Levitt NS, Miranda JJ, Ortiz AB, Steyn K, et al. Hypertension prevalence, awareness, treatment, and control in selected LMIC communities: results from the NHLBI/UHG network of centers of excellence for chronic diseases. Glob Heart. 2016;11(1):47–59. doi: 10.1016/j.gheart.2015.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70(4):736–742. doi: 10.1161/HYPERTENSIONAHA.117.09801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Papathanasiou G, Zerva E, Zacharis I, et al. Association of high blood pressure with body mass index, smoking and physical activity in healthy young adults. Open Cardiovasc Med J. 2015;9:5–17. doi: 10.2174/1874192401509010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed during the study are available in the Demographic and Health Surveys, DHS repository, https://dhsprogram.com/Data/