Abstract
Objective
The aim of this study is to assess the prevalence of nonunion in patients with tibia fracture and the association between influencing factors and tibia fracture nonunion.
Method
A database searches of PubMed, the Cochrane Library, EMBASE, China National Knowledge Infrastructure (CNKI), Weipu database, and Wanfang database from inception until June 2019 was conducted. The pooled prevalence, odds ratio (OR), and 95% confidence intervals (CI) were calculated with Stata software.
Results
In this study, 111 studies involving 41,429 subjects were included. In the study of the relationship between influencing factors and tibia fracture nonunion, 15 factors significantly influenced the fracture union, including > 60 years old, male, tobacco smoker, body mass index > 40, diabetes, nonsteroidal anti-inflammatory drugs (NSAIDs) user, opioids user, fracture of middle and distal tibia, high-energy fracture, open fracture, Gustilo-Anderson grade IIIB or IIIC, Müller AO Classification of Fractures C, open reduction, fixation model, and infection.
Conclusion
The prevalence of nonunion in patients with tibia fracture was 0.068 and 15 potential factors were associated with the prevalence. Closed reduction and minimally invasive percutaneous plate osteosynthesis (MIPPO) have the low risks of nonunion for the treatment of tibial fractures.
Keywords: Tibia fracture, Nonunion, Prevalence, Influencing factors, Systematic review
Introduction
Fracture is a common disease that has a great impact on patients’ lives. Take Canada as an example, fractures and dislocations of the lower limb make up 38% of all injury admissions [1]. It is estimated that the disability from traffic accidents (the major cause of fractures) will rank the top three of all causes of disability by 2020 [2].
Fracture nonunion is one of the most common complications of fracture. The rate of fracture nonunion varies greatly in different anatomical locations of the fracture [3], with an average incidence rate of 4.93% [4]. Fracture nonunion is a chronic condition in terms of pain, and functional and psychosocial disability [5]. Nonunion of some fractures can reduce the quality of life and even increase the risk of death [3]. The cost of treatment for fracture nonunion was much more than that of fracture union [6, 7]. Other economic burdens caused by prolonged disability and downtime of job are more difficult to quantify but must be considered [8].
Good blood supply is an important condition for fracture union [1, 9]. Compared to other long bones with abundant blood vessels and soft tissue, the tibia with a longer subcutaneous boundary normally has a poorer blood supply [10]. Therefore, tibial fracture has a higher risk of nonunion due to its special structure and blood supply. The definition of tibia fracture nonunion was no sign of union 9 months after surgical operation or no possibility of union if no further intervention was given assessed by surgeon [11].
Doctors need to know how to predict the risk of fracture nonunion and set up a plan to reduce the rate of fracture nonunion [8, 12]. In 2007, the “diamond concept” was introduced by Giannoudis et al., aiming to define what is required to achieve adequate fracture healing. This concept highlights the importance of three biological factors (osteogenic cells, osteoconductive scaffolds, growth factors) and a fourth factor known as mechanical stabilization. If one or more of these factors are altered, adequate fracture healing will be threatened [9, 13, 14].
Clinical and experimental studies have identified a number of potential factors that may help to predict fracture nonunion [15–18]. These factors include uncontrollable factors (for example, gender, age, underlying diseases, the way of injury) and controllable factors (for example, treatment method) [19, 20]. The uncontrollable factors of tibial nonunion may be similar to those of other anatomic sites. But there are too many influencing factors and even the same influencing factor may lead to different consequences in different anatomical positions [21]. For controllable influencing factors, the treatment of tibial fracture is also controversial [22]. Some doctors believe that intramedullary nailing (IMN) is the gold standard for the treatment of tibial fractures [23, 24]; however, most doctors consider that different treatment options have different advantages [25–28]. The use of non-steroidal anti-inflammatory drugs (NSAIDs) and the fixation of fibular fractures have also been considered as controversial factors for many years [29, 30].
Herein, we conducted a systematic review to explore the prevalence of nonunion in patients with tibia fracture and evaluate the association between influencing factors and tibia fracture nonunion. The study would provide valuable information for future prevention and treatment of tibia fracture nonunion.
Methods
Search strategy
The PubMed, Cochrane Library, EMBASE, CNKI (China National Knowledge Infrastructure), Wanfang database, and Weipu database were systematically searched, from inception to June 2019. The search keywords were “tibia” AND "fracture” AND “union OR nonunion OR disunion.” The manual search was performed through checking the reference lists of key studies and review articles to identify additional studies.
Study selection
An overall literature search was performed and relevant studies were screened independently by two reviewers (Ruifeng Tian, Fang Zheng). Initially, all the titles and abstracts which were identified based on the keywords were screened. Secondly, full texts of articles which were selected from the first phase were reviewed. Finally, the articles which had contents suitable for data extraction were included in the systematic review. Disagreements between the two reviewers were resolved by a third reviewer (Wei Zhao) via discussion and consensus.
Exclusion criteria
Exclusion criteria were as follows: neither English nor Chinese; animal model experiment; patients at the age of < 18; the cases of patients being lower than 10; insufficient information; duplicate publication; and obscure definition, such as delay union or mixed-descriptions of delay union and nonunion.
Data extraction
Relevant data were extracted independently by two reviewers (Ruifeng Tian and Yuhui Zhang). Each of the following information was entered into a pre-designed form: first author’s name, publication year, basic information of patients (including history of medication, unhealthy habits and basic diseases), fracture type, operative information, the number of all tibia fracture patients, and the number of tibia fracture nonunion patients. The information of 19 potentially influencing factors were also exacted for comparison analyses, including age, gender, tobacco smoke, drink, body mass index (BMI), diabetes, nonsteroidal anti-inflammatory drugs (NSAIDs) user, opioids user, osteofascial compartment syndrome, fracture site, injury energy (low or high energy that causes tibia fracture), open fracture, Gustilo-Anderson grade, Müller AO Classification of Fractures (AO), debride time (the time from injury to debride), open reduction, fibula fixation, infection, and fixation models. Disagreements between the two reviewers were resolved by a third reviewer (Jinping Yuan) via discussion and consensus.
Data analysis
Stata software (v12.0, Stata Corp, College Station, TX, USA) was used to assess all statistical analyses and a p < 0.05 was considered statistically significant. First, for exploring the prevalence of nonunion in patients with tibia fracture, the pooled prevalence and its 95% confidence intervals (CI) were calculated by using a random-effect model (p < 0.05, I2 > 50%), otherwise, or a fixed-effect model was selected (p > 0.05, I2 < 50%). When the prevalence rate in the included study was zero, double arcsine was used to deal with the data in case of data exclusion. Second, in the study of the association between potentially influencing factors and nonunion, the odds ratio (OR) and its 95% CI were calculated. To assess sources of heterogeneity, subgroup analyses were conducted, stratified by above 19 potentially influencing factors. Sensitivity analysis was performed by eliminating individual studies one by one. Publication biases were assessed by using the Begg’s test and Egger’s test.
Results
Characteristics of included studies
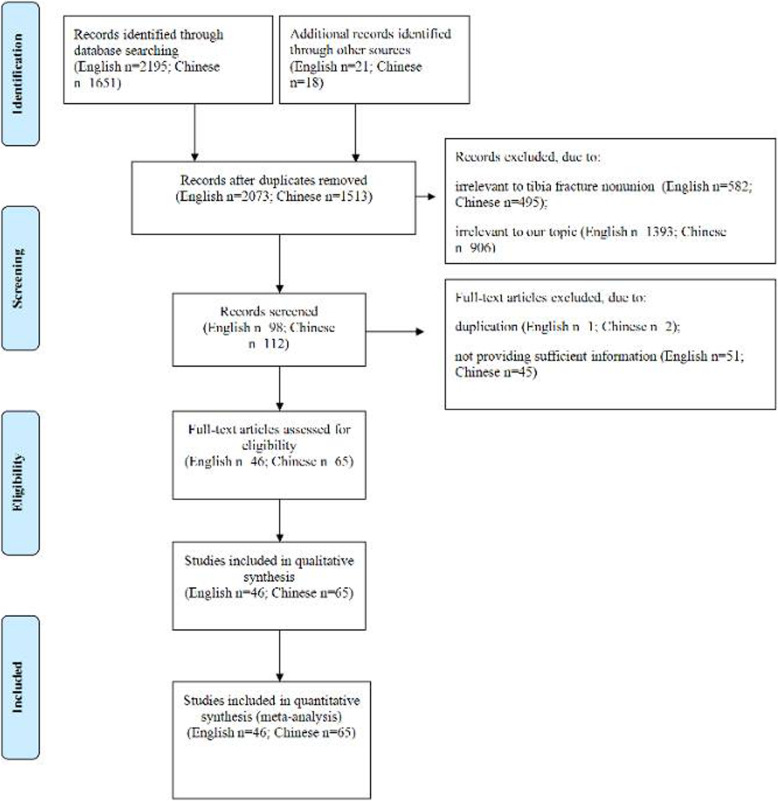
A total of 3846 studies (2195 English and 1651 Chinese) were searched. Following selection process (Fig. 1), 111 studies were included in this systematic review and meta-analysis [6, 15, 16, 19, 31–136].
Fig. 1.
Flow diagram of the study selection process
These studies were published between 1997 and 2019 from USA, China, Australia, Belarus, Canada, Egypt, France, India, Iran, Italy, Japan, Malaysia, Singapore, Turkey, and UK. There were 46 studies written in English and 65 studies in Chinese. The number of patients with tibia fracture ranged from 30 to 14638, and the prevalence of tibia fracture nonunion ranged from 0 to 42.7%. The basic information in all included studies were listed in Table 1.
Table 1.
The basic information and prevalence of tibia fracture nonunion in each included study
| Author | Year | Country | Age | Male | Female | Number of tibia fracture | Number of nonunion | Prevalence |
|---|---|---|---|---|---|---|---|---|
| Su CA [31] | 2018 | USA | 40.4 | 225 | 102 | 284 | 19 | 0.067 |
| Mehta D [32] | 2018 | USA | 35.2 | 29 | 11 | 40 | 4 | 0.100 |
| Milenkovic S [33] | 2018 | USA | 43.5 | 20 | 12 | 32 | 6 | 0.188 |
| Chang BS [34] | 2018 | China | 23-57 | 38 | 26 | 60 | 7 | 0.117 |
| Liu BQ [35] | 2018 | China | 36.1 | 46 | 5 | 51 | 3 | 0.059 |
| Zhang JS [36] | 2018 | China | 49.4 | 60 | 34 | 94 | 5 | 0.053 |
| Zhang QL [37] | 2018 | China | 35 | 50 | 36 | 86 | 0 | 0.000 |
| Yu JQ [38] | 2018 | China | 42.4 | 65 | 39 | 94 | 5 | 0.053 |
| Jin PF [39] | 2018 | China | 57.6 | 90 | 107 | 197 | 26 | 0.132 |
| Ge Y [40] | 2018 | China | 39.3 | 50 | 42 | 92 | 2 | 0.022 |
| Fang YS [41] | 2018 | China | 45.2 | 49 | 13 | 62 | 1 | 0.016 |
| Li J [42] | 2018 | China | 35.5 | 46 | 39 | 70 | 2 | 0.029 |
| Xu DY [43] | 2018 | China | 40.9 | 38 | 26 | 64 | 3 | 0.047 |
| Li ZT [44] | 2018 | China | 52.4 | 48 | 42 | 90 | 1 | 0.011 |
| Dailey HL [45] | 2018 | UK | 739 | 264 | 1003 | 121 | 0.121 | |
| Singh A [46] | 2018 | Singapore | 38.2 | 101 | 2 | 103 | 44 | 0.427 |
| Galal S [47] | 2018 | Egypt | 37.2 | 52 | 8 | 60 | 2 | 0.033 |
| Javdan M[48] | 2017 | USA | 231 | 12 | 0.052 | |||
| Auston DA [49] | 2017 | USA | 42 | 184 | 131 | 315 | 17 | 0.054 |
| Zura R [50] | 2017 | USA | 18-63 | 6273 | 6535 | 12808 | 944 | 0.074 |
| Thakore RV [15] | 2017 | USA | 36 | 364 | 102 | 486 | 56 | 0.115 |
| Chan DS [51] | 2017 | USA | 44 | 82 | 32 | 114 | 24 | 0.211 |
| Xiong SR [52] | 2017 | China | 42.5 | 82 | 66 | 148 | 8 | 0.054 |
| Javdan M [48] | 2017 | Iran | 35.9 | 45 | 4 | 49 | 3 | 0.061 |
| BeytemürÔ [53] | 2017 | Turkey | 40.6 | 52 | 21 | 73 | 1 | 0.014 |
| Daolagupu AK [54] | 2017 | India | 37.14 | 32 | 10 | 42 | 3 | 0.071 |
| Garg S [55] | 2017 | India | 38.9 | 5 | 31 | 36 | 4 | 0.111 |
| Mukherjee S [56] | 2017 | India | 40.3 | 26 | 14 | 40 | 3 | 0.075 |
| Blair JA [57] | 2016 | USA | 42.2 | 156 | 28 | 184 | 16 | 0.087 |
| Burrus MT [16] | 2016 | USA | 8132 | 6506 | 14,638 | 1758 | 0.120 | |
| Avilucea FR [58] | 2016 | USA | 40.6 | 162 | 54 | 216 | 29 | 0.134 |
| O'Halloran K [19] | 2016 | USA | 39.3 | 93 | 289 | 382 | 56 | 0.147 |
| Barcakë [59] | 2016 | USA | 64 | 5 | 0.078 | |||
| Shen J [60] | 2016 | China | 45 | 54 | 71 | 125 | 0 | 0.000 |
| Fang JH [61] | 2016 | China | 36.8 | 40 | 16 | 56 | 2 | 0.036 |
| Hao LS [62] | 2016 | China | 19-67 | 67 | 15 | 82 | 2 | 0.024 |
| Hu H [63] | 2016 | China | 36.7 | 30 | 22 | 52 | 1 | 0.019 |
| Liu JQ [64] | 2016 | China | 43.2 | 44 | 16 | 60 | 1 | 0.017 |
| Rao HR [65] | 2016 | China | 35.7 | 35 | 15 | 50 | 2 | 0.040 |
| Bai T [66] | 2016 | China | 36.8 | 43 | 17 | 60 | 4 | 0.067 |
| Zhao KP [67] | 2016 | China | 35.6 | 41 | 17 | 58 | 1 | 0.017 |
| Uchiyama Y [68] | 2016 | Japan | 41.9 | 77 | 8 | 85 | 3 | 0.035 |
| Gupta P [69] | 2016 | India | 42.7 | 22 | 8 | 30 | 1 | 0.033 |
| Piątkowski K [70] | 2015 | USA | 49.5 | 24 | 17 | 45 | 12 | 0.267 |
| Sun KF [71] | 2015 | China | 43.1 | 32 | 20 | 115 | 7 | 0.061 |
| Sun JQ [72] | 2015 | China | 48 | 35 | 21 | 56 | 7 | 0.125 |
| Ma N [73] | 2015 | China | 45.4 | 334 | 246 | 580 | 82 | 0.141 |
| Huang H [74] | 2015 | China | 17-65 | 52 | 44 | 96 | 5 | 0.052 |
| Huang PZ [75] | 2015 | China | 32 | 43 | 13 | 56 | 1 | 0.018 |
| Zhang YH [76] | 2015 | China | 36.5 | 49 | 21 | 70 | 2 | 0.029 |
| Luo BX [77] | 2015 | China | 38.5 | 47 | 31 | 78 | 1 | 0.013 |
| Wang B [78] | 2015 | China | 41.2 | 39 | 33 | 72 | 2 | 0.028 |
| Cui LH [79] | 2015 | China | 37.5 | 53 | 21 | 74 | 2 | 0.027 |
| Meng YH [80] | 2015 | China | 31.6 | 19 | 35 | 54 | 1 | 0.019 |
| Gong Y [81] | 2015 | China | 16-39 | 38 | 32 | 70 | 11 | 0.157 |
| Lian HK [82] | 2015 | China | 35.1 | 51 | 43 | 94 | 4 | 0.043 |
| Meena RC [83] | 2015 | India | 37.5 | 32 | 12 | 44 | 2 | 0.045 |
| Sathiyakumar V [84] | 2014 | USA | 37.5 | 63 | 30 | 93 | 17 | 0.183 |
| Li Y [85] | 2014 | China. | 43.3 | 116 | 5 | 121 | 2 | 0.017 |
| Dai QH [86] | 2014 | China | 34.5 | 23 | 19 | 42 | 0 | 0.000 |
| Wu ZH [87] | 2014 | China | 48.5 | 32 | 18 | 50 | 1 | 0.020 |
| Li ZZ [88] | 2014 | China | 43.8 | 76 | 44 | 60 | 5 | 0.083 |
| Ren Y [89] | 2014 | China | 34.7 | 49 | 21 | 70 | 4 | 0.057 |
| Luan HX [90] | 2014 | China | 37.1 | 78 | 20 | 98 | 6 | 0.061 |
| Zhang WJ [91] | 2014 | China | 44 | 43 | 25 | 68 | 3 | 0.044 |
| Heng WX [92] | 2014 | China | 18-79 | 45 | 23 | 68 | 4 | 0.059 |
| Yavuz U [93] | 2014 | Turkey | 42 | 32 | 23 | 55 | 3 | 0.055 |
| Lack WD [94] | 2014 | USA | 45 | 92 | 71 | 163 | 13 | 0.080 |
| Berlusconi M [95] | 2014 | Italy | 45 | 42 | 18 | 60 | 5 | 0.083 |
| Antonovaë [6] | 2013 | USA | 52.5 | 378 | 475 | 853 | 99 | 0.116 |
| Huang Q [96] | 2013 | China | 36.9 | 80 | 40 | 120 | 3 | 0.025 |
| Gong M [97] | 2013 | China | 40.3 | 41 | 11 | 52 | 2 | 0.038 |
| Lv YM [98] | 2013 | China | 39.1 | 77 | 34 | 111 | 6 | 0.054 |
| Xu YD [99] | 2013 | China | 39 | 105 | 58 | 163 | 2 | 0.012 |
| Clement ND [100] | 2013 | UK | 77.9 | 63 | 170 | 233 | 23 | 0.099 |
| Sitnik AA [101] | 2013 | Belarus | 43 | 54 | 26 | 80 | 7 | 0.088 |
| Yusof NM [102] | 2013 | Malaysia | 24.5 | 52 | 6 | 58 | 10 | 0.172 |
| Bishop JA [103] | 2012 | USA | 32 | 1 | 0.031 | |||
| Lin ZF [104] | 2012 | China | 36.6 | 222 | 194 | 416 | 33 | 0.079 |
| Zhang H [105] | 2012 | China | 39.6 | 58 | 38 | 96 | 1 | 0.010 |
| Jia QT [106] | 2012 | China | 36 | 61 | 27 | 88 | 4 | 0.045 |
| Zhou JL [107] | 2012 | China | 53 | 43 | 9 | 52 | 10 | 0.192 |
| Rouhani A [108] | 2012 | Iran | 26.4 | 45 | 8 | 54 | 3 | 0.056 |
| Vallier HA [109] | 2011 | USA | 38.3 | 85 | 19 | 114 | 6 | 0.053 |
| Zhu DK [110] | 2011 | China | 18-76 | 53 | 31 | 84 | 3 | 0.036 |
| Zhao DL [111] | 2011 | China | 37.8 | 54 | 26 | 80 | 1 | 0.013 |
| Liu F [112] | 2011 | China | 32.6 | 32 | 14 | 46 | 4 | 0.087 |
| Enninghorst N [113] | 2011 | Australia | 42.4 | 66 | 23 | 89 | 26 | 0.292 |
| Xu JQ [114] | 2009 | China | 36.3 | 121 | 49 | 170 | 8 | 0.047 |
| Li ZG [115] | 2009 | China | 35.8 | 71 | 56 | 127 | 3 | 0.024 |
| Mahmudi N [116] | 2009 | China | 37 | 34 | 10 | 44 | 3 | 0.068 |
| Deng HP [117] | 2009 | China | 40.3 | 51 | 34 | 85 | 4 | 0.047 |
| Dong JH [118] | 2009 | China | 18-74 | 77 | 51 | 128 | 2 | 0.016 |
| Fu KL [119] | 2009 | China | 112 | 11 | 0.098 | |||
| Zhou L [120] | 2009 | China | 37.9 | 52 | 41 | 93 | 5 | 0.054 |
| Lang ZY [121] | 2009 | China | 33.6 | 51 | 16 | 67 | 2 | 0.030 |
| Wu C [122] | 2009 | China | 19-71 | 25 | 12 | 37 | 2 | 0.054 |
| Li QM [123] | 2009 | China | 37.6 | 168 | 51 | 219 | 6 | 0.027 |
| Yokoyama K [124] | 2008 | Japan | 34.6 | 70 | 14 | 84 | 17 | 0.202 |
| Aderinto J [125] | 2008 | UK | 54 | 3 | 0.056 | |||
| Lu HY [126] | 2007 | China | 34.5 | 158 | 98 | 256 | 9 | 0.035 |
| Hu GZ [127] | 2007 | China | 33.4 | 301 | 116 | 396 | 11 | 0.028 |
| Zeng CJ [128] | 2006 | China | 30.7 | 390 | 264 | 541 | 14 | 0.026 |
| Zhang YL [129] | 2006 | China | 35 | 73 | 25 | 98 | 9 | 0.092 |
| Zhao XZ [130] | 2006 | China | 43.8 | 52 | 26 | 78 | 5 | 0.064 |
| Zhu GH [131] | 2005 | China | 34 | 55 | 23 | 78 | 5 | 0.064 |
| Harris I [132] | 2005 | Australia | 34 | 124 | 39 | 163 | 13 | 0.080 |
| Cole PA [133] | 2004 | USA | 89 | 2 | 0.022 | |||
| Bonnevialle P [134] | 2003 | France | 40.8 | 34 | 15 | 49 | 8 | 0.163 |
| Harvey EJ [135] | 2002 | Canada | 110 | 13 | 0.118 | |||
| Keating J [136] | 1997 | USA | 112 | 9 | 0.080 | |||
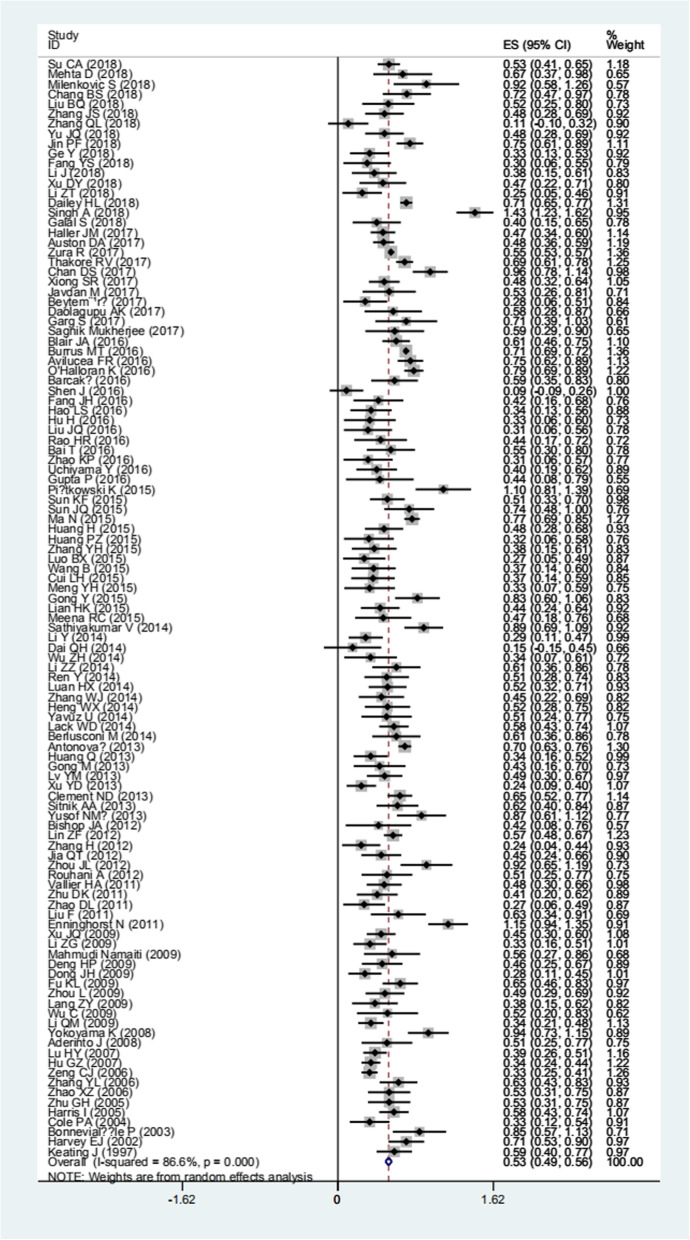
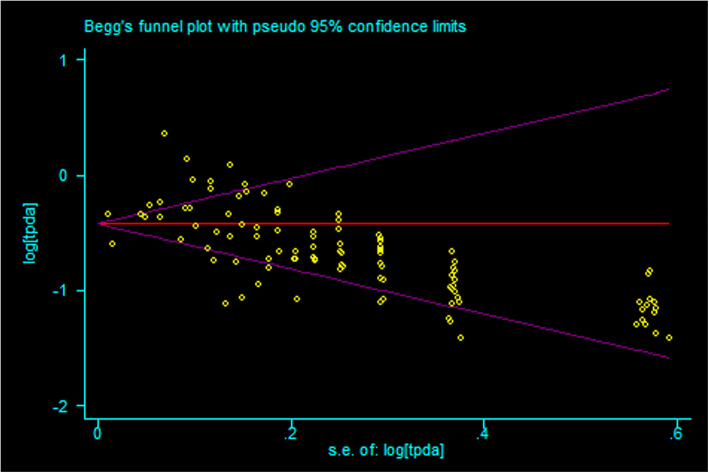
Pooled results, sensitive analysis, publication bias of the prevalence of tibia fracture nonunion
Based on the results of random-effects method (p < 0.05, I2 > 50%), the prevalence of nonunion from tibia fracture patient was 0.068 (95% CI 0.060–0.077) (Fig. 2, Table 2). The sensitive analysis demonstrated that there was no individual studies significantly affected the pooled results. The publication bias were found in pooled results (t = 3.19, p = 0.002) (Fig. 3).
Fig. 2.
The forest plot of prevalence of tibia fracture nonunion
Table 2.
The pooled results and subgroup analysis of prevalence of nonunion from tibia fracture patient
| Number of study | N | n | Prevalence rate | Heterogeneity | Model | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| effect size | lower limit | upper limit | I2 | p | ||||||
| Total | 111 | 41429 | 3817 | 0.068 | 0.060 | 0.077 | 86.60% | < 0.01 | Random | |
| 1. Age (year) | < 60 | 3 | 545 | 60 | 0.125 | 0.060 | 0.189 | 77.50% | 0.012 | Random |
| > 60 | 3 | 316 | 65 | 0.204 | 0.160 | 0.249 | 0.00% | 0.689 | Fixed | |
| 2. Gender | Male | 11 | 8186 | 790 | 0.131 | 0.104 | 0.159 | 77.80% | < 0.01 | Random |
| Female | 11 | 8123 | 618 | 0.118 | 0.085 | 0.150 | 84.50% | < 0.01 | Random | |
| 3. Tobacco smoker | Yes | 8 | 2263 | 299 | 0.173 | 0.119 | 0.226 | 91.80% | < 0.01 | Random |
| No | 8 | 12177 | 888 | 0.111 | 0.072 | 0.150 | 87.30% | < 0.01 | Random | |
| 4. Drink | Yes | 2 | 348 | 42 | 0.136 | 0.036 | 0.235 | 82.50% | 0.017 | Random |
| No | 2 | 12842 | 958 | 0.098 | 0.043 | 0.152 | 86.90% | 0.006 | Random | |
| 5. Body mass index | < 30 | 2 | 24466 | 2257 | 0.091 | 0.049 | 0.133 | 99.30% | < 0.01 | Random |
| > 30 | 2 | 3790 | 451 | 0.119 | 0.109 | 0.129 | 0.00% | 0.557 | Fixed | |
| 30–40 | 2 | 2507 | 236 | 0.094 | 0.083 | 0.105 | 0.00% | 0.441 | Fixed | |
| < 40 | 2 | 26973 | 2493 | 0.091 | 0.053 | 0.128 | 99.20% | < 0.01 | Random | |
| > 40 | 2 | 1283 | 215 | 0.160 | 0.020 | 0.218 | 87.80% | 0.004 | Random | |
| 6. Diabetes | Yes | 4 | 347 | 73 | 0.221 | 0.178 | 0.267 | 8.50% | 0.335 | Fixed |
| No | 4 | 984 | 103 | 0.102 | 0.065 | 0.139 | 67.50% | 0.046 | Random | |
| Yes | 3 | 371 | 58 | 0.153 | 0.116 | 0.189 | 0.00% | 0.420 | Fixed | |
| No | 3 | 1197 | 144 | 0.117 | 0.099 | 0.135 | 59.90% | 0.083 | Random | |
| 8. Opioids user | Yes | 3 | 1035 | 145 | 0.140 | 0.118 | 0.161 | 0.00% | 0.694 | Fixed |
| No | 3 | 522 | 58 | 0.097 | 0.031 | 0.164 | 78.40% | 0.010 | Random | |
| 9. Fracture site | Proximal | 7 | 586 | 30 | 0.043 | 0.027 | 0.06 | 26.50% | 0.254 | Fixed |
| Middle | 7 | 724 | 115 | 0.146 | 0.080 | 0.211 | 84.60% | < 0.01 | Random | |
| Distal | 7 | 614 | 88 | 0.139 | 0.104 | 0.178 | 24.10% | 0.253 | Fixed | |
| 10. Injury energy | High | 4 | 710 | 105 | 0.149 | 0.083 | 0.241 | 83.60% | < 0.01 | Random |
| Low | 4 | 298 | 22 | 0.065 | 0.007 | 0.175 | 87.30% | < 0.01 | Random | |
| 11.Open fracture | Yes | 10 | 14037 | 916 | 0.062 | 0.049 | 0.074 | 56.20% | 0.015 | Random |
| On | 10 | 1985 | 390 | 0.197 | 0.145 | 0.294 | 84.80% | < 0.01 | Random | |
| 12. Gustilo-Anderson gradea | I or II | 9 | 680 | 57 | 0.070 | 0.051 | 0.089 | 31.30% | 0.168 | Fixed |
| IIIA | 9 | 394 | 55 | 0.130 | 0.097 | 0.163 | 0.00% | 0.686 | Fixed | |
| IIIB or IIIC | 9 | 220 | 89 | 0.382 | 0.198 | 0.566 | 88.90% | < 0.01 | random | |
| 13.Müller AO Classification of Fractures (AO) classificationb | A | 7 | 1039 | 69 | 0.059 | 0.027 | 0.090 | 68.90% | 0.004 | Random |
| B | 7 | 600 | 103 | 0.140 | 0.086 | 0.204 | 65.90% | 0.007 | Random | |
| C | 7 | 285 | 54 | 0.158 | 0.078 | 0.260 | 74.50% | 0.001 | Random | |
| 14. Debride time | < 6 h | 2 | 138 | 41 | 0.302 | 0.074 | 0.530 | 89.10% | 0.002 | Random |
| > 6 h | 2 | 49 | 20 | 0.405 | 0.268 | 0.541 | 0.00% | 0.411 | Fixed | |
| 15. Open reduction | Yes | 9 | 573 | 48 | 0.075 | 0.043 | 0.107 | 52.40% | 0.032 | Random |
| No | 9 | 606 | 26 | 0.043 | 0.028 | 0.060 | 42.10% | 0.086 | Fixed | |
| 16. Fixation modec | ORIF | 41 | 6216 | 703 | 0.081 | 0.058 | 0.107 | 82.10% | < 0.01 | Random |
| IMN | 51 | 12642 | 1326 | 0.054 | 0.040 | 0.070 | 77.30% | < 0.01 | Random | |
| MIPPO | 25 | 988 | 18 | 0.023 | 0.015 | 0.032 | 0.00% | 0.835 | Fixed | |
| External fixation | 680 | 33 | 0.055 | 0.023 | 0.098 | 76.90% | < 0.01 | Random | ||
| Conservative treatment | 4 | 116 | 22 | 0.134 | 0.003 | 0.409 | 92.10% | < 0.01 | Random | |
| 17. Fibula fixed | Yes | 7 | 166 | 11 | 0.073 | 0.027 | 0.140 | 53.20% | 0.046 | Random |
| No | 7 | 538 | 69 | 0.122 | 0.094 | 0.149 | < 0.01 | 0.611 | Fixed | |
| 18. Osteofascial compartment syndrome | Yes | 3 | 210 | 31 | 0.134 | 0.088 | 0.179 | 61.90% | 0.072 | Fixed |
| No | 3 | 1359 | 162 | 0.105 | 0.058 | 0.151 | 85.40% | 0.001 | Random | |
| 19. Infection | Yes | 2 | 217 | 84 | 0.510 | 0.155 | 0.866 | 93.80% | < 0.01 | Random |
| No | 2 | 1366 | 119 | 0.076 | 0.022 | 0.129 | 92.80% | < 0.01 | Random | |
aGustilo-Anderson classification: grade I: clean wound < 1 cm in length; grade II: wound 1–10 cm in length without extensive soft-tissue damage, flaps or avulsions; grade III: extensive soft-tissue laceration (>10 cm) or tissue loss/damage or an open segmental fracture; grade IIIa: adequate periosteal coverage of the fracture bone despite the extensive soft-tissue laceration or damage; grade IIIb: extensive soft-tissue loss, periosteal stripping and bone damage, usually associated with massive contamination; grade IIIc: associated with an arterial injury requiring repair, irrespective of degree of soft-tissue injury
bAO classification of tibia fractures with designations of A: simple, B: wedge, C: complex
cORIF open reduction and internal fixation, IMN intramedullary nailing, MIPPO minimally invasive plate osteosynthesis
Fig. 3.
The publication bias of prevalence of tibia fracture nonunion
Subgroup analysis of prevalence of tibia fracture nonunion and comparison results
The prevalence of tibia fracture nonunion in different countries were of various (Tables 2, 3, and 4), for example, USA was 0.094 (95% CI 0.075–0.114), China was 0.047 (95% CI 0.039–0.057), etc.
Table 3.
The comparison results stratified by 19 influencing factors
| Study | Comparison results | Heterogeneity | Model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| p | OR | lower limit | upper limit | I2 | p | ||||
| 1. Age (year) | > 60 vs. < 60 | 3 | < 0.05 | 2.602 | 1.686 | 4.016 | 48.70% | 0.142 | Fixed |
| 2. Gender | Male vs. Female | 11 | < 0.05 | 1.256 | 1.122 | 1.407 | 14.00% | 0.311 | Fixed |
| 3. Tobacco smoker | Yes vs. No | 8 | < 0.05 | 1.692 | 1.458 | 1.964 | 49.30% | 0.055 | Fixed |
| 4. Drink | Yes vs. No | 2 | 0.083 | 1.367 | 0.960 | 1.947 | 0.00% | 0.518 | Fixed |
| 5. Body mass index (BMI) | 30 < BMI < 40 vs. BMI < 30 | 2 | 0.801 | 1.085 | 0.575 | 2.050 | 93.70% | < 0.05 | Random |
| BMI > 40 vs. BMI < 30 | 2 | < 0.05 | 1.874 | 1.607 | 2.185 | 0.00% | 0.660 | Fixed | |
| BMI > 30 vs. BMI < 30 | 2 | 0.189 | 1.351 | 0.862 | 2.119 | 93.00% | < 0.05 | Random | |
| BMI > 40 vs. 30 < BMI < 40 | 2 | 0.045 | 1.773 | 1.014 | 3.102 | 84.30% | 0.012 | Random | |
| BMI > 40 vs. BMI < 40 | 2 | < 0.05 | 1.899 | 1.630 | 2.212 | 0.00% | 0.892 | Fixed | |
| 6. Diabetes | Yes vs. No | 3 | < 0.05 | 2.731 | 1.857 | 4.014 | 32.20% | 0.229 | Fixed |
| 7. Nonsteroidal anti-inflammatory drugs user | Yes vs. No | 3 | 0.018 | 1.536 | 1.076 | 2.194 | 0.00% | 0.384 | Fixed |
| 8. Opioids user | Yes vs. No | 3 | 0.012 | 2.010 | 1.166 | 3.468 | 0.00% | 0.370 | Fixed |
| 9. Fracture site | Middle vs. Proximal | 7 | < 0.05 | 3.152 | 2.019 | 4.922 | 0.00% | 0.788 | Fixed |
| Distal vs. Proximal | 7 | < 0.05 | 2.877 | 1.822 | 4.543 | 0.00% | 0.911 | Fixed | |
| Distal vs. Middle | 7 | 0.670 | 0.932 | 0.673 | 1.290 | 0.00% | 0.650 | Fixed | |
| 10. Injury energy | High vs. Low | 4 | 0.001 | 2.602 | 1.484 | 4.562 | 35.90% | 0.182 | Fixed |
| 11. Open fracture | Yes vs. No | 9 | < 0.05 | 2.846 | 1.700 | 4.202 | 16.50% | 0.296 | Fixed |
| 12. Gustilo-Anderson gradea | IIIA vs. I or II | 9 | 0.005 | 1.831 | 1.204 | 2.784 | 0.00% | 0.847 | Fixed |
| IIIB or IIIC vs. I or II | 9 | < 0.05 | 7.202 | 4.781 | 10.848 | 4.60% | 0.394 | Fixed | |
| IIIB or IIIC vs. IIIA | 9 | < 0.05 | 3.695 | 2.422 | 5.639 | 32.60% | 0.168 | Fixed | |
| 13. Müller AO Classification of Fractures (AO) classificationb | B vs. A | 7 | 0.010 | 2.522 | 1.249 | 5.930 | 54.20% | 0.041 | Random |
| C vs. A | 7 | < 0.05 | 3.685 | 2.405 | 5.648 | 37.00% | 0.160 | Fixed | |
| C vs. B | 7 | < 0.05 | 3.569 | 2.428 | 5.325 | 39.60% | 0.142 | Fixed | |
| 14. Debride time | < 6 h vs. > 6 h | 2 | 0.631 | 1.190 | 0.585 | 2.419 | 0.00% | 0.520 | Fixed |
| 15. Open reduction | Yes vs. No | 9 | < 0.05 | 2.887 | 1.715 | 4.861 | 26.20% | 0.220 | Fixed |
| 16. Fixation modec | IMN vs. MIPPO | 15 | 0.003 | 2.681 | 1.397 | 5.146 | 0.00% | 0.980 | Fixed |
| IMN vs. ORIF | 28 | 0.020 | 1.127 | 1.019 | 1.247 | 54.10% | <0.05 | Random | |
| ORIF vs. MIPPO | 7 | 0.010 | 3.495 | 1.351 | 9.045 | 0.00% | 0.859 | Fixed | |
| External vs. ORIF | 10 | 0.115 | 0.506 | 0.217 | 1.182 | 54.00% | 0.016 | Random | |
| Conservative vs. ORIF | 4 | 0.264 | 1.496 | 0.737 | 3.035 | 64.10% | 0.062 | Fixed | |
| External vs. IMN | 10 | 0.993 | 1.006 | 0.266 | 3.806 | 55.40% | 0.022 | Random | |
| 17. Fibula fixed | Yes vs. No | 7 | 0.435 | 1.317 | 0.659 | 2.634 | 47.60% | 0.075 | Random |
| 18. Osteofascial compartment syndrome | Yes vs. No | 3 | 0.106 | 1.420 | 0.968 | 2.173 | 80.30% | 0.006 | Fixed |
| 19. Infection | Yes vs. No | 2 | < 0.05 | 11.877 | 7.461 | 18.906 | 52.10% | 0.149 | Fixed |
aGustilo-Anderson classification: grade I: clean wound < 1 cm in length; grade II: wound 1–10 cm in length without extensive soft-tissue damage, flaps or avulsions; grade III: extensive soft-tissue laceration (> 10 cm) or tissue loss/damage or an open segmental fracture; grade IIIa: adequate periosteal coverage of the fracture bone despite the extensive soft-tissue laceration or damage; grade IIIb: extensive soft-tissue loss, periosteal stripping and bone damage, usually associated with massive contamination; grade IIIc: associated with an arterial injury requiring repair, irrespective of degree of soft-tissue injury
bAO classification of tibia fractures with designations of A: simple, B: wedge, C: complex
cORIF open reduction and internal fixation, IMN intramedullary nailing, MIPPO minimally invasive plate osteosynthesis
Table 4.
Prevalence of nonunion from tibia fracture in different countries
| Number of study | N | n | Prevalence rate | Heterogeneity | Model | ||||
|---|---|---|---|---|---|---|---|---|---|
| Effect size | Lower limit | Upper limit | I2 | p | |||||
| USA | 19 | 30167 | 3083 | 0.094 | 0.075 | 0.114 | 93.40% | < 0.01 | Random |
| China | 68 | 7550 | 396 | 0.047 | 0.039 | 0.057 | 69.50% | < 0.01 | Random |
| Australia | 2 | 252 | 39 | 0.182 | 0.026 | 0.389 | 93.90% | < 0.01 | Random |
| Belarus | 1 | 80 | 7 | 0.088 | – | – | – | – | – |
| Canada | 1 | 110 | 13 | 0.118 | – | – | – | – | – |
| Charlotte | 1 | 163 | 13 | 0.08 | – | – | – | – | – |
| Egypt | 1 | 60 | 2 | 0.033 | – | – | – | – | – |
| France | 1 | 49 | 8 | 0.162 | – | – | – | – | – |
| India | 5 | 150 | 10 | 0.059 | 0.026 | 0.092 | 0 | 0.73 | Fixed |
| Iran | 3 | 152 | 9 | 0.059 | 0.022 | 0.097 | 0 | 0.99 | Fixed |
| Italy | 1 | 60 | 5 | 0.083 | – | – | – | – | – |
| Japan | 2 | 169 | 20 | 0.114 | 0.049 | 0.278 | 91.70% | 0.001 | Random |
| Malaysia | 1 | 58 | 10 | 0.172 | – | – | – | – | – |
| Singapore | 1 | 103 | 44 | 0.427 | – | – | – | – | – |
| Turkey | 1 | 73 | 1 | 0.014 | – | – | – | – | – |
| UK | 4 | 1042 | 156 | 0.108 | 0.092 | 0.124 | 47.60% | 0.126 | Fixed |
In the following comparisons of influencing factors (Table 3), each of the former prevalence of tibia fracture nonunion was significantly higher than the latter one (p < 0.05), i.e., > 60 years old (0.204) vs. < 60 years old (0.125), male (0.131) vs. female (0.118), tobacco smoker (0.173) vs. non-smoking (0.111), BMI > 40 (0.160) vs. BMI < 40 (0.091), diabetes (0.221) vs. no diabetes (0.102), NSAIDs user (0.153) vs. none NSAIDs user (0.117), opioids user (0.140) vs. none opioids user (0.097), fracture of middle segment (0.146) vs. proximal segment (0.043), fracture of distal segment (0.139) vs. proximal segment (0.043), high-energy injury (0.149) vs. low-energy injury (0.065), open fracture (0.197) vs. close fracture (0.062), Gustilo-Anderson grade I or II (0.070) vs. IIIA (0.130) vs. IIIB and IIIC (0.382), AO Classification A (0.059) vs. B (0.140) vs. C (0.158), open reduction (0.075) vs. close reduction (0.043), infection (0.510) vs. without infection (0.076). No significant difference was found between other comparisons (p > 0.05).
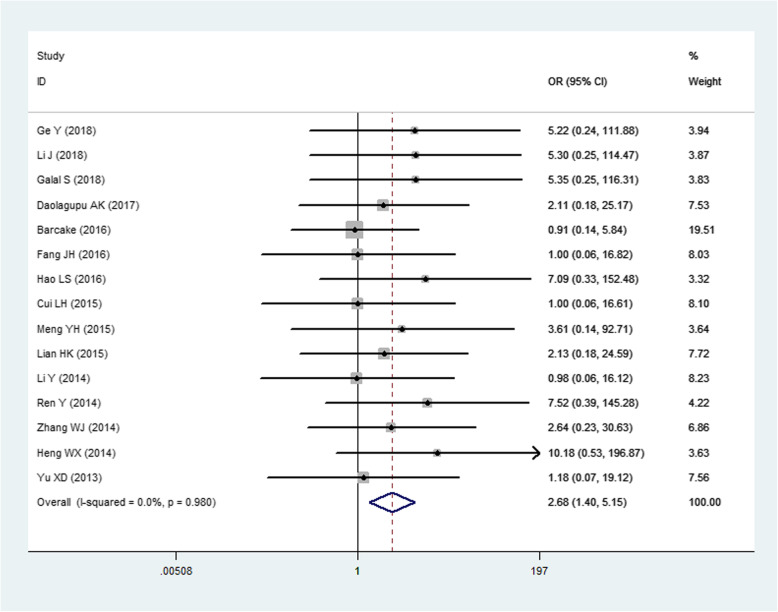
There were 5 fixation models of tibial fractures available, including open reduction and internal fixation (ORIF), intramedullary nailing (IMN), minimally invasive percutaneous plate osteosynthesis (MIPPO), external fixation, and conservative treatment. Significant difference was found between each other comparison of the following 3 fixation models, ORIF (0.081) vs. IMN (0.054) vs. MIPPO (0.023) (p < 0.05) (Fig. 4). No significant difference was found between external and ORIF, conservative and ORIF, or external and IMN (p > 0.05).
Fig. 4.
The comparison of MIPO with IMN
Discussion
To our knowledge, this is the first systematic review and meta-analysis to estimate the prevalence of nonunion in patients with tibia fracture and the relationship between different influence factors and tibia fracture nonunion. The pooled prevalence of tibial fracture nonunion was 0.068. Different countries were in variety of prevalence, indicating a heredity disparity. The lowest prevalence was seen in Turkey (0.014) and next was Egypt (0.033); however, the numbers of included studies were so small that the conclusions were not so robust. There were 68 studies that were conducted in China involving 7550 tibia fracture patients and the prevalence of nonunion was 0.047. However, one study in Singapore, a country that has lots of Chinese population, presented a very high prevalence of tibia fracture nonunion 0.427, indicating other influencing factors other than heredity. In calendar year 2011, an inception cohort study in a large payer database of patients with fracture in the USA was conducted using patient-level health claims for medical and drug expenses compiled for approximately 12,808 patients, and the prevalence of tibial fracture nonunion was reported to be 0.074 [137]. In contrast, the present systematic review involved 30,167 patients in a total of 19 studies conducted in the USA and the prevalence was 0.094. The pooled results enabled a larger sample size and accessed more to the real conclusion.
Some influencing factors contributed to the nonunion of tibial fractures. In 2016, O'Halloran K et al. created a Nonunion Risk Determination Score (NURDS) to predict nonunion risk, based on 7 influencing factors (p < 0.05, OR > 2), including flaps, compartment syndrome, chronic condition(s), open fractures, male gender, grade of American Society of Anesthesiologists Physical Status, and percent cortical contact. While another 2 factors including spiral fractures and low-energy injuries can be predictive of union [19]. In our study, we found more influencing factors, including age > 60 years old, diabetes, opioids user, middle and distal fracture, high-energy injury, open fracture, Gustilo-Anderson grade IIIB and IIIC, and AO Classification C met above criteria (p < 0.05, OR > 2) and can be regarded as predictive indicators. Still, there were some other influencing factors, including male, tobacco smoker, BMI > 40, and NSAIDs user, partially predicated the risks (p < 0.05, OR < 2).
The present study showed that BMI > 40 and diabetes were the influencing factors of nonunion of tibia fractures. With the improvement of quality of life, the negative impact of obesity has gradually become a hot issue of concern. Obesity can lead to vitamin D deficiency, and whether there is a causal relationship between fracture nonunion and vitamin D deficiency is the focus of discussion [138, 139]. But we cannot ignore the fact that diabetes mellitus is closely related to obesity. In our study, the use of NSAIDs was also associated with fracture nonunion. Some experiments have proved that NSAIDs can temporarily inhibit the process of fracture union [140, 141]; however, other studies considered that the pain caused by fracture nonunion of patients led to their resorting to NSAIDs [142].
Our comparison showed that open reduction had a higher rate of fracture nonunion than closed reduction. In surgery, although open reduction can bring good fracture repair, but closed reduction can better protect blood supply and soft tissue. In addition, our study did not find a relationship between fibular fixation and nonunion rates of tibial fractures. However, Strauss EJ and Kumar A’ experiments on cadavers showed that fibular fixation can increase the stability of tibial fractures after surgery [143–145]. So whether it is necessary to fix the fibula for the treatment of tibial fracture accompanied by fibular fracture should be further determined.
The choice of fixation mode is a way to control the nonunion rate of tibial fracture artificially [146, 147]. We compared 5 fixation modes available. The nonunion rate of conservative treatment was the highest one compared with that of surgical treatment. This is obviously different from the lowest rate reported by Li H et al. [148]. This may be related to the insufficient number of articles in conservative treatment. Compared with traditional ORIF, IMN and MIPPO have lower fracture nonunion rate. No significant difference was found between external fixation and ORIF. Ebraheim NA et al. reported that IMN can achieve better healing effect in the treatment of tibial fractures, comparing to ORIF and external fixation [149]. MIPPO had the lowest nonunion rate of all fixation modes. It was proved that MIPPO can maximize the protection of soft tissue and bone marrow around the fracture site [150]. The above 5 fixation modes destroy the necessary conditions of fracture healing to varying degrees. However, it is worth mentioning that different options have different advantages in the treatment of tibial fractures [151, 152]. For example, in distal tibial fractures, more comminuted fractures would rather require open reduction than “simple” type A fractures. So it is unreasonable to only consider the nonunion rate of fracture of operation [148].
The systematic review and meta-analysis had made strict inclusion and exclusion criteria, but still had some limitations and bias which may be unavoidable. Firstly, due to different attentions of individual studies, the influencing factors were only extracted from partial studies with available data and some other influencing factors such as hemoglobin and bone defect were not mentioned. Secondly, different doctors and different hospitals had a variety of surgical technologies and conditions, which may cause unavoidable bias. Thirdly, the number of included studies and the data for meta-analysis were limited which may affect the final results to a certain degree. Fourthly, publication bias was found in the study. Therefore, the data from literature in other languages, more areas, and ongoing studies are required to reflect a more accurate and wide variation. Finally, non-randomized controlled trials (nRCTs) were involved in this systematic review. As a result, subjective factors may affect the result. More rigorous designs and large RCTs are required to make further verification.
In conclusion, the prevalence of nonunion in patients with tibia fracture was 0.068 and 15 potential factors were associated with the prevalence. Closed reduction and MIPPO have low risks of nonunion for the treatment of tibial fractures. A series of factors shed the light which may affect the union rate of tibial fracture for doctors’ reference, and provide the probability of nonunion of tibial fracture under different treatment schemes. The authors hope to help doctors assess the risk of nonunion and propose the most suitable treatment for patients with tibial fractures under different conditions.
Acknowledgements
Not applicable.
Abbreviations
- CNKI
China National Knowledge Infrastructure
- OR
Odds ratio
- CI
Confidence intervals
- NSAIDs
Nonsteroidal anti-inflammatory drugs
- AO
Müller AO Classification of Fractures
- MIPPO
Minimally invasive percutaneous plate osteosynthesis
- IMN
Intramedullary nailing
- NRCTs
Non-randomized controlled trials
Authors’ contributions
An overall literature search was performed and relevant studies were screened by RT; extracted the relevant data. An overall literature search was performed and relevant studies were screened independently by FZ. Disagreements of data were resolved by WZ via discussion and consensus. YZ extracted the relevant data. BZ extracted the relevant data. Disagreements of data extraction were resolved by JY via discussion and consensus. LL: Technical guidance of the writing process. All authors read and approved the final manuscript.
Funding
The study was supported by Liaoning Provincial Natural Science Fund (code 201602837).
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study has obtained ethics approval and consent of the ethics committee in our hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bell A, Templeman D, Weinlein JC. Nonunion of the Femur andTibia: An Update. Orthop Clin North Am. 2016;47(2):365–375. doi: 10.1016/j.ocl.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 2.Lu C, Miclau T, Hu D, et al. Ischemia leads to delayed union duringfracture healing: a mouse model. J Orthop Res. 2007;25(1):51–61. doi: 10.1002/jor.20264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zura R, Braid-Forbes MJ, Jeray K, et al. Bone fracture nonunion ratedecreases with increasing age: A prospective inception cohort study. Bone. 2017;95:26–32. doi: 10.1016/j.bone.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Zura R, Watson JT, Einhorn T, et al. An inception cohort analysis topredict nonunion in tibia and 17 other fracture locations. Injury. 2017;48(6):1194–1203. doi: 10.1016/j.injury.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 5.Lerner RK, Esterhai JL, Jr, Polomano RC, et al. Quality of lifeassessment of patients with posttraumatic fracture nonunion, chronic refractory osteomyelitis, and lower-extremity amputation. Clin Orthop Relat Res. 1993;295:28–36. [PubMed] [Google Scholar]
- 6.Antonova E, Le TK, Burge R, et al. Tibia shaft fractures: costly burden of nonunions. BMC Musculoskelet Disord. 2013;14:42. doi: 10.1186/1471-2474-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekegren CL, Edwards ER, de Steiger R, et al. Incidence, costs and predictors of non-union, delayed union and mal-union following long bone fracture. Int J Environ Res Public Health. 2018;15:12. doi: 10.3390/ijerph15122845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hak DJ, Fitzpatrick D, Bishop JA, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury. 2014;45(2):3–7. doi: 10.1016/j.injury.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: the role of the biological chamber. Injury. 2011;42(11):1191–1193. doi: 10.1016/j.injury.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 10.McMillan TE, Johnstone AJ. Technical considerations to avoid delayed and non-union. Injury. 2017;48(1):64–68. doi: 10.1016/j.injury.2017.04.019. [DOI] [PubMed] [Google Scholar]
- 11.Fong K, Truong V, Foote CJ, et al. Predictors of nonunion and reoperation in patients with fractures of the tibia: an observational study. BMC Musculoskelet Disord. 2013;14:103. doi: 10.1186/1471-2474-14-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zura R, Mehta S, Della Rocca GJ, et al. Biological risk factors for nonunion of bone fracture. JBJS Rev. 2016;4:1. doi: 10.2106/JBJS.RVW.O.00008. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Buitrago AF, Jahangir A. Tibia nonunion. StatPearls. Treasure Island: StatPearls Publishing; 2019. [PubMed] [Google Scholar]
- 14.Giannoudis PV, Einhorn TA, Marsh D. Fracture healing: the diamond concept. Injury. 2007;38(4):3–6. doi: 10.1016/s0020-1383(08)70003-2. [DOI] [PubMed] [Google Scholar]
- 15.Thakore RV, Francois EL, Nwosu SK, et al. The Gustilo-Anderson classification system as predictor of nonunion and infection in open tibia fractures. Eur J Trauma Emerg Surg. 2017;43(5):651–656. doi: 10.1007/s00068-016-0725-y. [DOI] [PubMed] [Google Scholar]
- 16.Burrus MT, Werner BC, Yarboro SR. Obesity is associated with increased postoperative complications after operative management of tibial shaft fractures. Injury. 2016;47(2):465–470. doi: 10.1016/j.injury.2015.10.026. [DOI] [PubMed] [Google Scholar]
- 17.Schmitz MA, Finnegan M, Natarajan R, et al. Effect of smoking on tibial shaft fracture healing. Clin Orthop Relat Res. 1999;365:184–200. doi: 10.1097/00003086-199908000-00024. [DOI] [PubMed] [Google Scholar]
- 18.Kyrö A, Usenius JP, Aarnio M, et al. Are smokers a risk group for delayed healing of tibial shaft fractures? Ann Chir Gynaecol. 1993;82(4):254–262. [PubMed] [Google Scholar]
- 19.O'Halloran K, Coale M, Costales T, et al. Will my tibial fracture heal? Predicting nonunion at the time of definitive fixation based on commonly available variables. Clin Orthop Relat Res. 2016;474(6):1385–1395. doi: 10.1007/s11999-016-4821-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross KA, O'Halloran K, Castillo RC, et al. Prediction of tibial nonunion at the 6-week time point. Injury. 2018;49(11):2075–2082. doi: 10.1016/j.injury.2018.07.033. [DOI] [PubMed] [Google Scholar]
- 21.Lee M, Choi WJ, Han SH, et al. Uncontrolled diabetes as a potential risk factor in tibiotalocalcaneal fusion using a retrograde intramedullary nail. Foot Ankle Surg. 2018;24(6):542–548. doi: 10.1016/j.fas.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 22.Costa ML, Achten J, Hennings S, et al. Intramedullary nail fixation versus locking plate fixation for adults with a fracture of the distal tibia: the UK FixDT RCT. Health Technol Assess. 2018;22(25):1–148. doi: 10.3310/hta22250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manon J, Detrembleur C, Van de Veyver S, et al. Predictors of mechanical complications after intramedullary nailing of tibial fractures. Orthop Traumatol Surg Res. 2019;105(3):523–527. doi: 10.1016/j.otsr.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 24.Caubere A, Demoures T, Choufani C, et al. Use of intramedullary nailing in poor sanitary conditions: French Military Medical Service experience. Orthop Traumatol Surg Res. 2019;105(1):173–177. doi: 10.1016/j.otsr.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Wani IH, Ul Gani N, Yaseen M, et al. Operative management of distal tibial extra-articular fractures—intramedullary nail versus minimally invasive percutaneous plate osteosynthesis. Ortop Traumatol Rehabil. 2017;19(6):537–541. doi: 10.5604/01.3001.0010.8045. [DOI] [PubMed] [Google Scholar]
- 26.Vaienti E, Schiavi P, Ceccarelli F, et al. Treatment of distal tibial fractures: prospective comparative study evaluating two surgical procedures with investigation for predictive factors of unfavourable outcome. Int Orthop. 2018;43(1):201–207. doi: 10.1007/s00264-018-4121-6. [DOI] [PubMed] [Google Scholar]
- 27.Costa ML, Achten GJ, et al. Effect of locking plate fixation vs intramedullary nail fixation on 6-month disability among adults with displaced fracture of the distal tibia: the UK FixDT randomized clinical trial. JAMA. 2017;318(18):1767–1776. doi: 10.1001/jama.2017.16429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mioc ML, Prejbeanu R, Deleanu B, et al. Extra-articular distal tibia fractures-controversies regarding treatment options. A single-centre prospective comparative study. Int Orthop. 2018;42(4):915–919. doi: 10.1007/s00264-018-3775-4. [DOI] [PubMed] [Google Scholar]
- 29.Fader L, Whitaker J, Lopez M, et al. Tibia fractures and NSAIDs. Does it make a difference? A multicenter retrospective study. Injury. 2018;49(12):2290–2294. doi: 10.1016/j.injury.2018.09.024. [DOI] [PubMed] [Google Scholar]
- 30.Pogliacomi F, Schiavi P, Calderazzi F, et al. When is indicated fibular fixation in extra-articular fractures of the distal tibia? Acta Biomed. 2019;89(4):558–563. doi: 10.23750/abm.v89i4.7775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Su CA, Nguyen MP, O’Donnell JA, et al. Outcomes of tibia shaft fractures caused by low energy gunshot wounds. Injury. 2019;49(7):1348–1352. doi: 10.1016/j.injury.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 32.Mehta D, Abdou S, Stranix JT, et al. Comparing radiographic progression of bone healing in Gustilo IIIB open tibia fractures treated with muscle versus fasciocutaneous flaps. J Orthop Trauma. 2018;32(8):381–385. doi: 10.1097/BOT.0000000000001190. [DOI] [PubMed] [Google Scholar]
- 33.Milenkovic S, Mitkovic M, Mitkovic M. External fixation of segmental tibial shaft fractures. Eur J Trauma Emerg Surg. 2018. [DOI] [PubMed]
- 34.Chang BS, Dang L, Song JH, et al. The effect of fibular fixation in the treatment of compound fractures of distal tibia and fibula. J Clin Orthopaed. 2018;21(06):730–733. [Google Scholar]
- 35.Liu BQ, Ding XJ, Che DX, et al. The effect of fibular fracture fixation on the surgical outcome of distal tibial fractur. Chin J Bone Jnt Injury. 2018;33(12):1315–1317. [Google Scholar]
- 36.Zhang JS, Wang YT. Comparative analysis of clinical effects of intramedullary nail and plate internal fixation for distal tibial fracture. China Pract Med. 2018;13(32):77–79. [Google Scholar]
- 37.Zhang QL, Li ZJ. Application effect of distal tibial locking plate and distal tibial intramedullary nail in the treatment of distal tibiofibular fractures. Clin Res Pract. 2018;3(32):82–83. [Google Scholar]
- 38.Yu JK, Wang J. Comparatives study of minimally invasive percutaneous plate internal fixation and open reduction and plate internal fixation in the treatment of tibial Pilon fracture. Chin J Clin. 2018;46(10):1161–1162. [Google Scholar]
- 39.Jin PF, Wang ZQ, Song HP. Rist factors for nonunion of closed tibial shaft fractures. J North China Univ Sci Technol (Health Sciences Edition) 2018;20(5):378–383. [Google Scholar]
- 40.Ge Y. Clinical effect and biomechanical properties of interlocking intramedullary nail and minimally invasive percutaneous plate internal fixation in the treatment of middle and lower tibial fractures. Chin J Convalescent Med. 2018;27(08):840–841. [Google Scholar]
- 41.Fang YS. Percutaneous locking compression titanium plate fixation and interlocking intramedullary nail fixation for distal tibial fractures. Med J Comm. 2018;32(03):226–228. [Google Scholar]
- 42.Li J, Jiang C, Zhu YS. Closed reduction with interlocking intramedullary nail and percutaneous minimally invasive locking compression plate in the treatment of tibial fracture. Chin Remedies Clin. 2018;18(6):1009–1011. [Google Scholar]
- 43.Xu YD, Zhang WX, Zhou MW, et al. Minimally invasive locking plate in the treatment of gustilo type II open tibial fractures. Gansu Med J. 2018;37(6):481–483. [Google Scholar]
- 44.Li ZT, Ma SQ, Zhang HB, et al. Comparison of the efficacy of interlocking intramedullary nail and percutaneous locking plate in the treatment of distal tibial extraarticular fractures. J Modern Med Health. 2018;34(11):1703–1705. [Google Scholar]
- 45.Dailey HL, Wu KA, Wu PS, et al. Tibial fracture nonunion and time to healing after reamed intramedullary nailing: risk factors based on a single-center Review of 1003 patients. J Orthop Trauma. 2018;32(7):263–269. doi: 10.1097/BOT.0000000000001173. [DOI] [PubMed] [Google Scholar]
- 46.Singh A, Jiong Hao JT, Wei DT, et al. Gustilo IIIB open tibial fractures: an analysis of infection and nonunion rates. Indian J Orthop. 2018;52(4):406–410. doi: 10.4103/ortho.IJOrtho_369_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Galal S. Minimally invasive plate osteosynthesis has equal safety to reamed intramedullary nails in treating Gustilo-Anderson type I, II and III-A open tibial shaft fractures. Injury. 2018;49(4):866–870. doi: 10.1016/j.injury.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 48.Javdan M, Tahririan MA, Nouri M. The role of fibular fixation in the treatment of combined distal tibia and fibula fracture: a randomized, control trial. Adv Biomed Res. 2017;6:48. doi: 10.4103/2277-9175.205190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Auston DA, Meiss J, Serrano R, et al. Percutaneous or open reduction of closed tibial shaft fractures during intramedullary nailing does not increase wound complications, infection or nonunion rates. J Orthop Trauma. 2017;31(4):215–219. doi: 10.1097/BOT.0000000000000777. [DOI] [PubMed] [Google Scholar]
- 50.Zura R, Watson JT, Einhorn T, et al. An inception cohort analysis to predict nonunion in tibia and 17 other fracture locations. Injury. 2017;48(6):1194–1203. doi: 10.1016/j.injury.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 51.Chan DS, Balthrop PM, White B, et al. Does a staged posterior approach have a negative effect on OTA 43c fracture outcomes? J Orthop Trauma. 2017;31(2):90–94. doi: 10.1097/BOT.0000000000000728. [DOI] [PubMed] [Google Scholar]
- 52.Xiong SR, Wu YB, Xiong GS, et al. Minimally invasive treatment of middle and lower tibial fractures with interlocking intramedullary nail and locking plate. Fujian Med J. 2017;39(05):94–96. [Google Scholar]
- 53.Beytemür O, Barış A, Albay C, et al. Comparison of intramedullary nailing and minimal invasive plate osteosynthesis in the treatment of simple intra-articular fractures of the distal tibia (AO-OTA type 43 C1-C2) Acta Orthop Traumatol Turc. 2017;51(1):12–16. doi: 10.1016/j.aott.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Daolagupu AK, Mudgal A, Agarwala V, et al. A comparative study of intramedullary interlocking nailing and minimally invasive plate osteosynthesis in extra articular distal tibial fractures. Indian J Orthop. 2017;51(3):292–298. doi: 10.4103/0019-5413.205674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Garg S, Khanna V, Goyal MP, et al. Comparative prospective study between medial and lateral distal tibial locking compression plates for distal third tibial fractures. Chin J Traumatol. 2017;20(3):151–154. doi: 10.1016/j.cjtee.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mukherjee S, Arambam MS, Waikhom S, et al. Interlocking nailing versus plating in tibial shaft fractures in adults: a comparative study. J Clin Diagn Res. 2017;11(4):8–13. doi: 10.7860/JCDR/2017/25577.9746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Blair JA, Stoops TK, Doarn MC, et al. Infection and nonunion after fasciotomy for compartment syndrome associated with tibia fractures: a matched cohort comparison. J Orthop Trauma. 2016;30(7):392–396. doi: 10.1097/BOT.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 58.Avilucea FR, Sathiyakumar V, Greenberg SE, et al. Open distal tibial shaft fractures: a retrospective comparison of medial plate versus nail fixation. Eur J Trauma Emerg Surg. 2016;42(1):101–106. doi: 10.1007/s00068-015-0519-7. [DOI] [PubMed] [Google Scholar]
- 59.Barcak E, Collinge CA, Metaphyseal Distal tibia fractures: a cohort, single-surgeon study comparing outcomes of patients treated with minimally invasive plating versus intramedullary nailing. J Orthop Trauma. 2016;30(5):69–74. doi: 10.1097/BOT.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 60.Shen J, Xu J, Tang MJ, et al. Extra-articular distal tibia facture (AO-43A): A retrospective study comparing modified MIPPO with IMN. Injury. 2016;47(10):2352–2359. doi: 10.1016/j.injury.2016.07.023. [DOI] [PubMed] [Google Scholar]
- 61.Fang JH, Wu YS, Guo XS, et al. Comparison of 3 minimally invasive methods for distal tibia fractures. Orthopedics. 2016;39(4):27–33. doi: 10.3928/01477447-20160606-01. [DOI] [PubMed] [Google Scholar]
- 62.Hao LS, Wang XC, Chen J. A retrospective trial of minimally invasive percutaneous plate osteosynthesis versus open reduction internal fixation for treatment of closed distal tibial fractures. J Trad Chin Orthoped Traumatol. 2016;28(10):14–17. [Google Scholar]
- 63.Hu H, Zhang Z, Li W, et al. Vitiligo: Observation of curative effect of MIPPO technique in treatment of distal tibial fracture. J Clin Med Lit. 2016;3(54):10715–10716. [Google Scholar]
- 64.Liu JQ, Lu L, Chen XP, et al. Clinical study of minimally invasive percutaneous locking plate internal fixation and traditional open reduction and internal fixation for tibial fracture. Jiangxi Med J. 2016;51(02):149–150. [Google Scholar]
- 65.Rao HR, Chen JQ. The clinical observation of minimally invasive percutaneous locking compression plate internal fixation in treatment of distal tibial fractures. J Liaoning Med Univ. 2016;37(02):41–43. [Google Scholar]
- 66.Bai T, Lu L, Gao JJ, et al. Efficacy of second generation tibial intramedullary nail in treatment of distal tibial fracture. Medical J Nat Def Forces Southwest China. 2016;26(10):1119–1121. [Google Scholar]
- 67.Zhao KP, Wang ZH, Li CY. Application of interlocking intramedullary nail and locking plate in middle and lower tibial fracture. Chin J Bone Jnt Injury. 2016;31(10):1096–1097. [Google Scholar]
- 68.Uchiyama Y, Kobayashi Y, Ebihara G. Retrospective comparison of postoperative infection and bone union between late and immediate intramedullary nailing of Gustilo grades I, II, and IIIA open tibial shaft fractures. Trauma Surg Acute Care Open. 2016;1(1):35. doi: 10.1136/tsaco-2016-000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gupta P, Tiwari A, Thora A. Minimally invasive plate osteosynthesis (MIPO) for proximal and distal fractures of the tibia: a biological approach. Malays Orthop J. 2016;10(1):29–37. doi: 10.5704/MOJ.1603.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Piątkowski K, Piekarczyk P, Kwiatkowski K, et al. Comparison of different locking plate fixation methods in distal tibia fractures. Int Orthop. 2015;39(11):2245–2251. doi: 10.1007/s00264-015-2906-4. [DOI] [PubMed] [Google Scholar]
- 71.Sun KF, Feng WW, Yang GZ, et al. A clinical study on comparing result of tibial shaft fractures using reamed intramedullary nail by close reduction versus limited open reduction. J Qiqihar Univ Med. 2015;36(34):5159–5161. [Google Scholar]
- 72.Sun JQ. Minimally invasive percutaneous plate internal fixation for tibial fracture. Chin J Modern Drug Appl. 2015;9(2):133–134. [Google Scholar]
- 73.Ma N, Rao ZT, Zhang JS. Selection of operation mode in treating high energy tibial pilon fractures and analysis of treatment effect related factors. Chin J Gen Pract. 2015;13(01):36–38. [Google Scholar]
- 74.Huang H, Chen Y, Liang Y, et al. A comparative analysis of closed reduction and open reduction interlocking intramedullary nail fixation for tibial shaft fracture. J Youjiang Med Univ Nationalities. 2015;37(01):73–74. [Google Scholar]
- 75.Huang PZ, Huang XY, Yang WD, et al. Application of minimally invasive percutaneous internal fixation for distal tibial extraarticular fractures. Chin J Trad Med Traumatol Orthoped. 2015;23(02):51–52. [Google Scholar]
- 76.Zhang YH. Clinical analysis of two different internal fixation methods for tibial plateau fractures. Henan J Surg. 2015;21(01):103–104. [Google Scholar]
- 77.Luo BX. The effect of minimally invasive internal fixation technology and open reduction plate internal fixation in the treatment of distal tibial fracture. Chin Comm Doctors. 2015;31(5):43–44. [Google Scholar]
- 78.Wang B, Wang ZZ, Zhang F. Comparison of locking compression plate and anatomic plate internal fixation for Pilon fracture. Chin J Tiss Eng Res. 2015;19(13):2091–2095. [Google Scholar]
- 79.Cui LH, Chang ZP. Observation on the effect of interlocking intramedullary nail and MIPPO in the treatment of middle and lower tibial fracture. J Bethune Med Sci. 2015;13(02):176–177. [Google Scholar]
- 80.Meng YH, Huang JQ, Ma P, et al. Treatment of distal tibial shaft fracture with LCP and MIPPO. Chin Orthopaed J Clin Basic Res. 2015;7(2):104–107. [Google Scholar]
- 81.Gong Y. Treatment of distal tibial extraarticular fracture with intramedullary nail and plate internal fixation. Chin J Clin Rational Drug Use. 2015;8(10):128. [Google Scholar]
- 82.Lian HK, Huang JC. Effectiveness comparison of different operative treatment of closed fracture of tibial shaft. Chin J Reparative Reconstructive Surg. 2015;29(9):1067–1071. [PubMed] [Google Scholar]
- 83.Meena RC, Meena UK, Gupta GL. Intramedullary nailing versus proximal plating in the management of closed extra-articular proximal tibial fracture: a randomized controlled trial. J Orthop Traumatol. 2015;16(3):203–208. doi: 10.1007/s10195-014-0332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sathiyakumar V, Thakore RV, Ihejirika RC, et al. Distal tibia fractures and medial plating: factors influencing re-operation. Int Orthop. 2014;38(7):1483–1488. doi: 10.1007/s00264-014-2345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Li Y, Jiang X, Guo Q, et al. Treatment of distal tibial shaft fractures by three different surgical methods: a randomized, prospective study. Int Orthop. 2014;38(6):1261–1267. doi: 10.1007/s00264-014-2294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dai QH. Discussion on the treatment methods and effects of 42 cases of tibial fracture. Contemp Med. 2014;20(29):96–97. [Google Scholar]
- 87.Wu ZH. Clinical value of interlocking intramedullary nail in minimally invasive treatment of tibial shaft fracture. Contemp Med. 2014;20(30):70–71. [Google Scholar]
- 88.Li ZZ. Clinical study of 60 cases of distal tibial comminuted fracture treated with compression plate. Guide China Med. 2014;12(34):119–120. [Google Scholar]
- 89.Ren Y, Hu CN, Chen QK, et al. Selective analysis of the tibia in the lower segment of unstable fractures of two minimally invasive internal fixation Formula. J Pract Orthopaed. 2014;20(8):715–719. [Google Scholar]
- 90.Luan HX, Mao J, Luan FJ. The effect of tourniquet for intramedullary nail in the treatment of tibial shaft fracture. Chin Comm Doctors. 2014;30(18):53–54. [Google Scholar]
- 91.Zhang WJ, Teng Y, Li Q, et al. Minimally invasive percutaneous plate osteosythesis for treatment of tibial shaft fractures. Chin J Bone Jnt Injury. 2014;29(10):1003–1005. [Google Scholar]
- 92.Heng WX, Wang S. Percutaneous minimally invasive plate fixation treatment of tibia fracture clinical observation. J Med Theory Pract. 2014;27(20):2682–2683. [Google Scholar]
- 93.Yavuz U, Sökücü S, Demir B, et al. Comparison of intramedullary nail and plate fixation in distal tibia diaphyseal fractures close to the mortise. Ulus Travma Acil Cerrahi Derg. 2014;20(3):189–193. doi: 10.5505/tjtes.2014.92972. [DOI] [PubMed] [Google Scholar]
- 94.Lack WD, Starman JS, Seymour R, et al. Any cortical bridging predicts healing of tibial shaft fractures. J Bone Joint Surg Am. 2014;96(13):1066–1072. doi: 10.2106/JBJS.M.00385. [DOI] [PubMed] [Google Scholar]
- 95.Berlusconi M, Busnelli L, Chiodini F, et al. To fix or not to fix? The role of fibular fixation in distal shaft fractures of the leg. Injury. 2014;45(2):408–411. doi: 10.1016/j.injury.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 96.Huang Q. Closed reduction and internal fixation with interlocking intramedullary nail for tibial fracture. Asia Pac Trad Med. 2013;9(9):126–127. [Google Scholar]
- 97.Gong M. Clinical observation of 52 cases of lower tibial fracture treated by percutaneous minimally invasive locking compression plate. Seek Med Ask Med. 2013;11(6):149–150. [Google Scholar]
- 98.Lu YM. Analysis of the effect of plate and interlocking intramedullary nail in the treatment of distal tibial fracture. Hebei Med J. 2013;35(8):1183–1184. [Google Scholar]
- 99.Yu XD, Xue F, Chen QB. Comparison of the efficacy of MIPPO and interlocking intramedullary nail in the treatment of distal and middle tibial fractures. J Pract Orthopaed. 2013;19(6):560–562. [Google Scholar]
- 100.Clement ND, Beauchamp NJ, Duckworth AD, et al. The outcome of tibial diaphyseal fractures in the elderly. Bone Joint J. 2013;95(9):1255–1262. doi: 10.1302/0301-620X.95B9.31112. [DOI] [PubMed] [Google Scholar]
- 101.Sitnik AA, Beletsky AV. Minimally invasive percutaneous plate fixation of tibia fractures: results in 80 patients. Clin Orthop Relat Res. 2013;471(9):2783–2789. doi: 10.1007/s11999-013-2841-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yusof NM, Khalid KA, Zulkifly AH, et al. Factors associated with the outcome of open tibial fractures. Malays J Med Sci. 2013;20(5):47–53. [PMC free article] [PubMed] [Google Scholar]
- 103.Bishop JA, Dikos GD, Mickelson D, et al. Open reduction and intramedullary nail fixation of closed tibial fractures. Orthopedics. 2012;35(11):1631–1634. doi: 10.3928/01477447-20121023-21. [DOI] [PubMed] [Google Scholar]
- 104.Lin ZF, Yang YH, Xiong WH. Correlation of union of lower tibial fractures with selection of terapies. Asia Pac Trad Med. 2012;8(7):61–63. [Google Scholar]
- 105.Zhang H, Ye CH, Yu H, et al. Case-control study on different fixation methods for the treatment of tibial fractures in 96 patients. China J Orthop Traumatol. 2012;25(3):198–201. [PubMed] [Google Scholar]
- 106.Jia QT. Comparing limited incision intramedullary nail with locking compression titanium plate in the treatment of tibial fracture. Henan J Surg. 2012;18(2):41–42. [Google Scholar]
- 107.Zhou JL, Pei BY. Comparison of surgical methods for multiple tibial fractures. Shanxi Med J. 2012;41(4):381–383. [Google Scholar]
- 108.Rouhani A, Elmi A, Akbari Aghdam H, et al. The role of fibular fixation in the treatment of tibia diaphysis distal third fractures. Orthop Traumatol Surg Res. 2012;98(8):868–872. doi: 10.1016/j.otsr.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 109.Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma. 2011;25(12):736–741. doi: 10.1097/BOT.0b013e318213f709. [DOI] [PubMed] [Google Scholar]
- 110.Zhu DK. Analysis of the reaming interlocking intramedullary nail for treatment of 84 tibial fractures. Chin Foreign Med Res. 2011;9(7):15–16. [Google Scholar]
- 111.Zhao DL, Zhang W, Zhao HY, et al. Closed reduction, percutaneous locking plate and interlocking intramedullary nail in the treatment of middle and lower tibial shaft fractures. China Modern Doctor. 2011;49(19):42–43. [Google Scholar]
- 112.Liu F, Zhang ZR. Treatment of tibial fracture and analysis of its curative effect. Jilin Med J. 2011;32(36):7753–7754. [Google Scholar]
- 113.Enninghorst N, McDougall D, Hunt JJ, et al. Open tibia fractures: timely debridement leaves injury severity as the only determinant of poor outcome. J Trauma. 2011;70(2):352–356. doi: 10.1097/TA.0b013e31820b4285. [DOI] [PubMed] [Google Scholar]
- 114.Xu JQ, Zhang SM, Chen FW, et al. Delayed union and nonunion of tibial fracture treated with interlocking intramedullary nail. Chin J Misdiagnostics. 2009;9(19):4611–4612. [Google Scholar]
- 115.Li ZG, He SC, Zhu RX. Treatment of 127 cases of distal tibial fracture. Acta Medicinae Sinica. 2009;22(2):272–273. [Google Scholar]
- 116.Mahmudi N. Comparison of open reduction and closed reduction with interlocking intramedullary nail in the treatment of tibiofibular shaft fractures. J Xinjiang Med Univ. 2009;32(10):1496–1497. [Google Scholar]
- 117.Deng HP, Lin GS, Wang ZY, et al. Comparative study of two different methods of reduction and internal fixation for surgical treatment of distal tibial fractures. J Clin Orthopaedic. 2009;12(6):658–660. [Google Scholar]
- 118.Dong JH, Han JM. Surgical treatment of tibia and fibula fracture in 128 cases. Shaanxi Med J. 2009;38(7):845–846. [Google Scholar]
- 119.Fu KL. Treatment of open fracture of middle tibia with steel plate and interlocking intramedullary nail. J Med Forum. 2009;30(9):56–58. [Google Scholar]
- 120.Zhou L, Duan H, Yuan XF, et al. Clinical effect comparison of interlocking intramedullary nail and compression plate in the treatment of tibial fracture. Med Pharm Yunnan. 2009;30(1):74–75. [Google Scholar]
- 121.Lang YZ. Therapeutic effect of two surgical methods for type III A open fracture of tibia and fibula: Shanxi Medical University; 2009.
- 122.Wu C, Tan L, Wang YX. Comparison of percutaneous plate and external fixator for treating the open distal tibial fractures. J Clin Orthopaed. 2009;12(1):43–45. [Google Scholar]
- 123.Li QM, Chen MJ, Deng JT, et al. Clinical observation of three fixation methods for tibial fracture. China J Orthop Traumatol. 2009;21(1):48–49. [PubMed] [Google Scholar]
- 124.Yokoyama K, Itoman M, Uchino M, et al. Immediate versus delayed intramedullary nailing for open fractures of the tibial shaft: a multivariate analysis of factors affecting deep infection and fracture healing. Indian J Orthop. 2008;42(4):410–419. doi: 10.4103/0019-5413.43385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Aderinto J, Keating JF. Intramedullary nailing of fractures of the tibia in diabetics. J Bone Joint Surg (Br) 2008;90(5):638–642. doi: 10.1302/0301-620X.90B5.19854. [DOI] [PubMed] [Google Scholar]
- 126.Lu HY, Shen RQ, Huang CM. Treatment of 256 cases of tibiofibular fracture. J Pract Orthopaed. 2007;10:627–631. [Google Scholar]
- 127.Hu GZ, Jin AM, Liu NF, et al. The curative effect analysis of interlocking intramedullary nail for the treatment of tibia fracture. Chin J Trad Med Traumatol Orthoped. 2007;7:14–16. [Google Scholar]
- 128.Zeng CJ. Therapeutic effect analysis of three treatment methods for tibial fracture. Pract Prev Med. 2006;4:1007–1008. [Google Scholar]
- 129.Zhang YL, Wang YS, Zhang SQ. Comparison of three treatment methods for tibial fracture. Guangdong Med J. 2006;10:1516–1518. [Google Scholar]
- 130.Zhao XZ, Yuan XQ, Feng Q. Treatment experience of 78 cases of tibiofibular diaphyseal fracture. J Yanan Univ (Medical Sciences) 2006;2:37–67. [Google Scholar]
- 131.Zhu GH. Comparison on efficacy of interlocking intramedullary nail and compression plate in treating tibial shaft fractures. J Elinical Res. 2005;10:1418–1420. [Google Scholar]
- 132.Harris I, Lyons M. Reoperation rate in diaphyseal tibia fractures. ANZ J Surg. 2005;75(12):1041–1044. doi: 10.1111/j.1445-2197.2005.03618.x. [DOI] [PubMed] [Google Scholar]
- 133.Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004;18(8):528–535. doi: 10.1097/00005131-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 134.Bonnevialle P, Cariven P, Bonnevialle N, et al. Segmental tibia fractures: a critical retrospective analysis of 49 cases. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(5):423–432. [PubMed] [Google Scholar]
- 135.Harvey EJ, Agel J, Selznick HS, et al. Deleterious effect of smoking on healing of open tibia-shaft fractures. Am J Orthop (Belle Mead NJ) 2002;31(9):518–521. [PubMed] [Google Scholar]
- 136.Keating JF, O'Brien PI, Blachut PA, et al. Reamed interlocking intramedullary nailing of open fractures of the tibia. Clin Orthop Relat Res. 1997;338:182–191. doi: 10.1097/00003086-199705000-00025. [DOI] [PubMed] [Google Scholar]
- 137.Zura R, Xiong Z, Einhorn T, et al. Epidemiology of fracture nonunion in 18 human bones. Jama Surg. 2016;151(11):e162775. doi: 10.1001/jamasurg.2016.2775. [DOI] [PubMed] [Google Scholar]
- 138.Goldner WS, Stoner JA, Thompson J, et al. Prevalence of vitamin D insufficiency and deficiency in morbidly obese patients: a comparison with non-obese controls. Obes Surg. 2008;18(2):145–150. doi: 10.1007/s11695-007-9315-8. [DOI] [PubMed] [Google Scholar]
- 139.Chakkalakal DA. Alcohol-induced bone loss and deficient bone repair. Alcohol Clin Exp Res. 2005;29(12):2077–2090. doi: 10.1097/01.alc.0000192039.21305.55. [DOI] [PubMed] [Google Scholar]
- 140.Simon AM, Manigrasso MB, O'Connor JP. Cyclo-oxygenase 2 function is essential for bone fracture healing. J Bone Miner Res. 2002;17(6):963–976. doi: 10.1359/jbmr.2002.17.6.963. [DOI] [PubMed] [Google Scholar]
- 141.Vuolteenaho K, Moilanen T, Moilanen E, et al. Non-steroidal anti-inflammatory drugs, cyclooxygenase-2 and the bone healing process. Basic Clin Pharmacol Toxicol. 2008;102(1):10–14. doi: 10.1111/j.1742-7843.2007.00149.x. [DOI] [PubMed] [Google Scholar]
- 142.Bhattacharyya T, Levin R, Vrahas MS, et al. Nonsteroidal antiinflammatory drugs and nonunion of humeral shaft fractures. Arthritis Rheum. 2005;53(3):364–367. doi: 10.1002/art.21170. [DOI] [PubMed] [Google Scholar]
- 143.Kumar A, Charlebois SJ, Cain EL, et al. Effect of fibular plate fixation on rotational stability of simulated distal tibial fractures treated with intramedullary nailing. J Bone Joint Surg Am. 2003;85(4):604–608. doi: 10.2106/00004623-200304000-00003. [DOI] [PubMed] [Google Scholar]
- 144.Strauss EJ, Alfonso D, Kummer FJ, et al. The effect of concurrent fibular fracture on the fixation of distal tibia fractures: a laboratory comparison of intramedullary nails with locked plates. J Orthop Trauma. 2007;21(3):172–177. doi: 10.1097/BOT.0b013e3180332dd2. [DOI] [PubMed] [Google Scholar]
- 145.Taylor BC, Hartley BR, Formaini N, et al. Necessity for fibular fixation associated with distal tibia fractures. Injury. 2015;46(12):2438–2442. doi: 10.1016/j.injury.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 146.Pintore E, Maffulli N, Petricciuolo F. Interlocking nailing for fractures of the femur and tibia. Injury. 1992;23(6):381–6. doi: 10.1016/0020-1383(92)90012-h. [DOI] [PubMed] [Google Scholar]
- 147.Sayana MK, Davis BJ, Kapoor B, et al. Fracture strain and stability with additional locking screws in intramedullary nailing: a biomechanical study. J Trauma. 2006;60(5):1053–1057. doi: 10.1097/01.ta.0000197600.46577.37. [DOI] [PubMed] [Google Scholar]
- 148.Li H, Yu D, Wu S, et al. Multiple Comparisons of the Efficacy and Safety for Seven Treatments in Tibia Shaft Fracture Patients. Front Pharmacol. 2019;10:197. doi: 10.3389/fphar.2019.00197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ebraheim NA, Evans B, Liu X, et al. Comparison of intramedullary nail, plate, and external fixation in the treatment of distal tibia nonunions. Int Orthop. 2017;41(9):1925–1934. doi: 10.1007/s00264-017-3432-3. [DOI] [PubMed] [Google Scholar]
- 150.Andalib A, Sheikhbahaei E, Andalib Z, et al. Effectiveness of minimally invasive plate osteosynthesis (MIPO) on comminuted tibial or femoral fractures. Arch Bone Jt Surg. 2017;5(5):290–295. [PMC free article] [PubMed] [Google Scholar]
- 151.Osti L, Del Buono A, Maffulli N. Application of pulsed electromagnetic fields after microfractures to the knee: a mid-term study. Int Orthop. 2015;39(7):1289–1294. doi: 10.1007/s00264-014-2627-0. [DOI] [PubMed] [Google Scholar]
- 152.Gougoulias N, Khanna A, Maffulli N. Open tibial fractures in the paediatric population: a systematic review of the literature. Br Med Bull. 2009;91:75–85. doi: 10.1093/bmb/ldp019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.